Abstract
Background
Studies of injection drug use cessation have largely sampled adults in drug treatment settings. Little is known about injection cessation and relapse among young injection drug users (IDU) in the community.
Methods
A total of 365 HCV-negative IDU under age 30 years were recruited by street outreach and interviewed quarterly for a prospective cohort between January 2000 and February 2008. Participants were followed for a total of 638 person-years and 1996 visits. We used survival analysis techniques to identify correlates of injection cessation (≥3 months) and relapse to injection.
Results
67% of subjects were male, median age was 22 years (interquartile range (IQR) 20 - 26) and median years injecting was 3.6 (IQR 1.3 – 6.5). 28.8% ceased injecting during the follow-up period. Among those that ceased injecting, nearly one-half resumed drug injection on subsequent visits, one-quarter maintained injecting cessation, and one-quarter were lost to follow-up. Participating in a drug treatment program in the last 3 months and injecting less than 30 times per month were associated with injection cessation. Injecting heroin or heroin mixed with other drugs, injecting the residue from previously used drug preparation equipment, drinking alcohol, and using benzodiazepines were negatively associated with cessation. Younger age was associated with relapse to injection.
Conclusion
These results suggest that factors associated with stopping injecting involve multiple areas of intervention, including access to drug treatment and behavioral approaches to reduce injection and sustain cessation. The higher incidence of relapse in the younger subjects in this cohort underscores the need for earlier detection and treatment programs targeted to adolescents and transition-age youth.
Keywords: Injection drug use, Cessation, Relapse, Youth
1. Introduction
There are approximately 16 million injection drug users (IDU) in 148 countries worldwide (Mathers et al., 2008). Injection drug use is associated with considerable morbidity and mortality and poses significant economic and social costs. In developed countries, injection drug use accounts for a majority of hepatitis C virus (HCV) infections, and a significant proportion of hepatitis B virus (HBV) and HIV infections (Alter, 2002; Dore et al., 2003). In the United States, up to 60% of HCV, 17% of HBV, and 32% of HIV infections are attributed to injection drug use (National Institute on Drug Abuse, 2000; Office of National Drug Control Policy, 2004). In developing countries, fewer data are available for these infections, but injection drug use has been associated with explosive HIV epidemics in Thailand and Russia and accounts for a high proportion of infections in Vietnam and China (Aceijas et al., 2004). In 2002, the health care-related costs for these blood-borne infections and other medical conditions associated with illicit drug use in the U. S. were estimated at 15.8 billion dollars annually, and costs associated with losses to productivity including premature death, drug-related illnesses, and incarceration were estimated to be 180 billion annually (Office of National Drug Control Policy, 2004).
Previous studies of the natural history of injection drug use have described various trajectories of injection behavior including: long-term injection, cessation of injection, and multiple transitions in and out of injection (Galai et al., 2003; Murphy et al., 2008). Longitudinal studies from the Netherlands conducted in adult treatment settings have found injection cessation to be associated with increases in methadone dose, lower frequency of injecting, obtaining fewer needles from needle exchange and the presence of an AIDS diagnosis (Langendam et al., 2000; van Ameijden and Coutinho, 2001).
Such studies based on treatment samples, however, are limited in generalizability since IDUs in treatment are unlikely to be representative of the larger population of community-based IDUs. Treatment-based samples are less likely to include street-based IDU, those without insurance, and younger IDU (Schutz et al., 1994; Shah et al., 2000).
Moreover, self-reported behavior in treatment settings may be affected by social desirability bias (Bowling, 2005). This is especially true if the interview is being conducted by staff associated with the treatment program.
Younger IDU are ideal candidates for injecting cessation as early intervention plays a key role in preventing (or delaying) HIV and HCV acquisition (Doherty et al., 2000; Garfein et al., 1998). However, few studies have reported on injection drug use cessation among young IDU. Studies among IDU in Baltimore and Montreal (Shah et al., 2006; Steensma et al., 2005) have observed cessation to be associated with younger age, fewer years injecting, stable housing, employment, lower frequency of drug use, injecting fewer types of drugs, and HIV infection.
We examined injection cessation and relapse in young street-based IDU in San Francisco, CA to determine the incidence of injection drug use cessation and relapse and the effect of socio-demographic factors, drug use frequency, and drug injection behaviors on injection drug use cessation and relapse.
2. Methods
From January 2000 through February 2008 IDUs under the age of 30 were recruited using street outreach methods to participate in the UFO Study (‘U Find Out’). Participants were recruited to study HIV and viral hepatitis during two waves of enrollment, the first between 2000 and 2001, and the second from 2003 through February 2008. The rationale, design and methods of the UFO cohort study have been described previously (Hahn et al., 2002). Briefly, at baseline screening participants were interviewed anonymously, counseled and tested for antibodies to HCV (anti-HCV) and HCV RNA. Subjects screened in years 2000-2002 also were tested for markers of HBV infection and immunization, and antibody to HIV. Participants were encouraged to return for test results, post-test counseling, and medical and social service referrals. All participants gave informed consent and were remunerated $10 for the screening visit and $20 when they returned for serological results one week later. Those who were HCV RNA or anti-HCV negative were invited to enroll in the cohort and scheduled for a structured interview and blood testing on a quarterly schedule.
The study was approved by the Committee on Human Research at the University of California, San Francisco.
2.1. Instrument
Structured questionnaires were administered during a 30 to 45 minute interview. Interview topics included socio-demographic characteristics, injection and non-injection drug use, injection risk behaviors, and sexual behaviors.
Socio-demographic variables included age, gender, race/ethnicity, education level, and main source of income. Structural predictors of interest included history of and recent drug treatment, history of and recent incarceration, and housing status in the past three months. Main source of income was categorized as income from jobs and government assistance (supplemental security income, general assistance, unemployment benefits) vs. other sources (family, friends, panhandling, stealing, selling drugs, or selling sex). Drug treatment in the prior 3 months included drug detoxification (“detox”), residential treatment, methadone maintenance, and 12-step programs. Participants who reported living the majority of time in the past three months in an apartment, home of parents, friends, or relatives, or half-way house or foster home were categorized as housed and those who reported living on the street, in a shelter, drug treatment facility, jail or prison were categorized as marginally housed or homeless.
Behavioral variables included both lifetime and recent behavior occurring in the last three months. Injection-related behavioral variables were needle borrowing, sharing of drug preparation equipment (cottons or cookers), injecting the residue from previously used drug preparation equipment (“doing a rinse”), pooling money with other IDU to buy drugs, and overdose. Sex risk behavior variables included number of sexual partners, unprotected anal or vaginal sex, sex in exchange for money or drugs, and having a sex partner who was also an IDU. Both injection and non-injection drug behavior information was elicited for ever use, last 3 months, and last 30 days. Variables included: years injecting, use of heroin, cocaine, methamphetamine, crack, or heroin mixed with methamphetamine or cocaine. Participants were also asked about the number of injection events and days injected in the prior month. Non-injection drug use included smoking or snorting cocaine, crack, or heroin, as well as the use of benzodiazepines, prescription opiates, marijuana, and alcohol.
The primary outcomes of interest for this analysis were injection drug use cessation and relapse to injection. Injection cessation was defined as having stopped injecting (self-reported) for three months or more at any time point during the follow-up period. Relapse to injection was defined as any injection drug use in the past three months occurring subsequent to a period of injection cessation and continuing for at least 1 day in the past month.
2.2. Statistical analysis
Cox regression models with both time-dependent and fixed covariates were used to identify predictors of injection cessation and relapse. Time to injection cessation was defined as time from initiation of injection to first observed episode of cessation. Since subjects were current IDU at the start of the study data were left-truncated. Subjects entered into analysis at the baseline visit and remained until the first day of the episode of cessation or were censored at the last visit date. Time to relapse was defined as time from initiation of injection cessation to date of first relapse to injection. Stata 9.0 was used for all analyses.
In order to examine the effect of behaviors that preceded injection cessation, all behavioral variables were lagged by one quarterly visit. By taking the behavioral information from the prior quarterly interview, we were able to identify behaviors that occurred in the three months prior to cessation rather than behaviors that occurred concurrently with or as the result of cessation.
Variable selection for inclusion in the models was based on the following: a priori hypotheses generated from previous studies (Langendam et al., 2000; Shah et al., 2006; Steensma et al., 2005; van Ameijden and Coutinho, 2001), including injection frequency, housing status and drug treatment attendance; other variables of significance (having a p-value < 0.10) identified from bivariate analyses. Age, race/ethnicity, and gender were explored as potential confounders. Multivariate models were constructed in an iterative process employing a backward selection procedure in which all variables that met the criteria above were included in a model and removed one at a time. We verified that hazards were proportional for time-dependent covariates by testing the interaction of visit time with each covariate and using episode splitting techniques. The final model included only variables that had a p-value less than 0.05. We analyzed Schoenfeld residuals to assess the proportionality assumption and evaluated goodness of fit using the likelihood ratio test.
3. Results
Of 1216 subjects screened, 798 (66%) tested anti-HCV and/or HCV RNA negative and were eligible for the prospective cohort study. 537 (67%) of those subsequently enrolled in the cohort. Eligible participants who did not enroll included those who did not return for test results and those who were not planning to remain in San Francisco for more than 1 month. Of the 537 enrolled, 365 (68%) returned for at least one quarterly follow-up visit. All 365 enrollees completing at least one follow-up visit were included in these analyses. Enrolled participants who were followed did not differ from those with no follow-up with respect to age, years injecting, gender, education or race/ethnicity. Followed individuals were less likely to be homeless (64% vs. 74%, p = 0.02), and more likely to inject drugs daily (33% vs. 24%, p = 0.04).
At baseline, the median age of the 365 participants in this analysis was 22 years (Range 15 – 30 years), 67% were male and 76% were white (Table 1). The median years injecting was 3.6 (Interquartile Range (IQR) 1.3-6.5) and 33% injected every day in the past month. 63% injected heroin or heroin mixed with cocaine or methamphetamine on most days in the past month and 32% injected methamphetamine on most days.
Table 1.
Selected baseline socio-demographic and behavioral characteristics of young IDU in the UFO Cohort Study, San Francisco, CA, 2000-2008 (N=365)
| Baseline characteristics | Median (IQR) |
|---|---|
| Age (per year) | 22 (20 – 26) |
| Duration of injection (per year) | 3.6 (1.3 – 6.5) |
| N (%) | |
| Injection cessation for >=3 months during follow-up | 105 (28.8) |
| Male sex | 244 (66.9) |
| Non-white race/ethnicity | 88 (24.3) |
| Less than high school education | 196 (54.8) |
| History of drug treatment | 130 (36.0) |
| History of mental health treatment | 258 (70.7) |
| History of incarceration | 300 (82.4) |
| Homeless or marginally housed, last 3 mo. | 233 (63.8) |
| Income from job or government assistance | 111 (30.4) |
| Drug treatment, last 3 mo. | 56 (15.4) |
| Mental health treatment, last 3 mo. | 91 (24.9) |
| Incarceration, last 3 mo. | 99 (27.2) |
| Syringe exchange, last mo. | 288 (79.1) |
| Traveled outside of San Francisco, last 3 mo. | 193 (52.9) |
| Injection behavior | |
| Drug injected most days, last mo. | |
| Heroin/Heroin mixed | 225 (63.4) |
| Methamphetamine | 113 (31.8) |
| Cocaine | 9 (2.5) |
| Other | 8 (2.3) |
| Daily injection, last mo. | 119 (32.6) |
| Less than 30 injection events, last mo. | 149 (40.9) |
| Injected heroin or heroin mixed with another drug, last 3 mo. | 287 (78.6) |
| Injected methamphetamine, last 3 mo. | 220 (60.6) |
| Injected cocaine, last 3 mo. | 117 (32.1) |
| Used a shared cooker, last 3 mo. | 214 (58.6) |
| Borrowed used needle, last 3 mo. | 133 36.5) |
| Injected someone's rinse, last 3 mo. | 139 (38.1) |
| Pooled money to buy drugs, last 3 mo. | 299 (82.1) |
| Overdosed, last 3 mo. | 53 (15.6) |
| Non-injection drug use | |
| Drank alcohol, last mo. | 281 (77.2) |
| Used marijuana last 3 mo. | 255 (83.3) |
| Smoked or snorted heroin, last 3 mo. | 71 (19.4) |
| Smoked or snorted crack, last 3 mo. | 162 (44.5) |
| Smoked or snorted cocaine, last 3 mo. | 107 (29.3) |
| Smoked or snorted methamphetamine, last 3 mo. | 215 (58.9) |
| Used opiate pills, last 3 mo. | 211 (57.8) |
| Used benzodiazepine pills, last 3 mo. | 171 (47.0) |
| Sexual behavior | |
| Any sex partner, last 3 mo. | 302 (82.7) |
| Sex in exchange for money or drugs, last 3 mo. | 32 (8.8) |
| IDU sex partner, last 3 mo. | 208 (57.0) |
| Any unprotected sex, last 3 mo. | 234 (77.2) |
The total observation time was 638 person-years. One hundred five (29%) reported at least one episode of injection cessation with a median time from study entry to cessation of 10.9 months (IQR 7.0 – 22.0) and a cessation incidence of 16.4 (95% CI: 13.6 – 19.9) per 100 person-years. Participants had been injecting for a median of 4.6 years (IQR 1.4 – 8.5) before ceasing injection.
3.1. Patterns of injection cessation
Subsequent to the first reported episode of cessation, 49 (47%) resumed injecting drugs. The median time to relapse was 6.0 months (IQR 3.0 – 12.8). Over one-quarter maintained injecting cessation (n=30); and were followed for a median of 5.4 months (IQR 3.2 – 15.7) post-cessation. One-quarter were lost to follow-up (n=26). (Figure 1).
Figure 1.
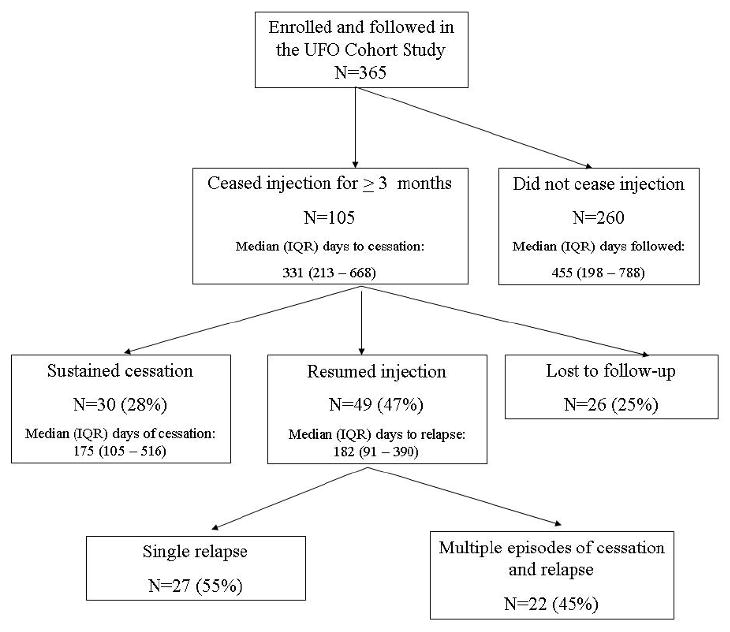
Longitudinal patterns of drug injection and cessation behavior among young IDU in the UFO Cohort Study, San Francisco, CA 2000-2008
3.2. Factors associated with injection cessation
Crude hazard ratios of socio-demographic and behavioral factors associated with injection cessation are presented in Table 2. Injection cessation was associated with having a job or government assistance as the main source of income (Hazard Ratio (HR) = 2.22) and inversely associated with a history of incarceration (HR = 0.41). Injection cessation was not significantly associated with age, housing status, duration of injection, gender, race/ethnicity, or education level. We found associations between both drug treatment and mental health treatment in the last 3 months and injection cessation (HR = 2.03 and 1.60) respectively. Use of syringe exchange in the past 30 days (time-lagged) was inversely associated with injection cessation (HR = 0.42).
Table 2.
Crude hazard ratios for injection cessation and relapse in young IDU in the UFO Cohort Study, San Francisco, CA, 2000-2008
| Injection cessation N=365 |
Relapse to injection N=79 |
|||
|---|---|---|---|---|
| Fixed characteristics | HR | (95% CI) | HR | (95% CI) |
| Age (per year) | 1.05 | (0.99 – 1.11) | 0.93 | (0.86 – 1.00) |
| Duration of injection (per year) | 1.00 | (0.86 – 1.15) | 1.05 | (0.98 – 1.13) |
| Male sex | 1.07 | (0.70 – 1.65) | 1.03 | (0.56 – 1.90) |
| Non-white race/ethnicity | 1.36 | (0.89 – 2.08) | 1.45 | (0.79 – 2.66) |
| Less than high school education | 1.15 | (0.77 – 1.70) | 0.89 | (0.50 – 1.57) |
| History of drug treatment | 0.88 | (0.58 – 1.35) | 0.85 | (0.47 – 1.54) |
| History of mental health treatment | 1.55 | (0.98 – 2.45) | 1.30 | (0.63 – 2.70) |
| History of incarceration | 0.41 | (0.25 – 0.65)** | 1.20 | (0.58 – 2.49) |
| Lagged time-dependent covariates† | ||||
| Homeless or marginally housed, last 3 mo. | 1.20 | (0.80 – 1.79) | 0.88 | (0.48 – 1.59) |
| Income from job or government assistance | 2.22 | (1.48 – 3.32)** | 0.73 | (0.40 – 1.35) |
| Drug treatment, last 3 mo. | 2.03 | (1.34 – 3.09)** | 0.79 | (0.44 – 1.44) |
| Mental health treatment, last 3 mo. | 1.60 | (1.05 – 2.44)* | 0.94 | (0.52 – 1.71) |
| Incarceration, last 3 mo. | 0.84 | (0.54 – 1.30) | 1.67 | (0.86 – 3.25) |
| Syringe exchange, last mo. | 0.42 | (0.28 – 0.62)** | NA | |
| Traveled outside of San Francisco, last 3 mo. | 0.74 | (0.49 – 1.11) | 0.65 | (0.33 – 1.29) |
| Lagged time-dependent injection behavior | ||||
| Drug injected most days, last mo. | ||||
| Heroin/Heroin mixed | Ref | |||
| Methamphetamine | 1.37 | (0.88 – 2.11) | NA | |
| Cocaine | 1.30 | (0.40 – 4.19) | ||
| Daily injection, last mo. | 0.43 | (0.26 – 0.70)** | NA | |
| Less than 30 injection events, last mo. | 3.56 | (2.32 – 5.47)** | NA | |
| Injected heroin or heroin mixed with another drug, last 3 mo. | 0.31 | (0.21 – 0.47)** | NA | |
| Injected methamphetamine, last 3 mo. | 0.73 | (0.49 – 1.08) | NA | |
| Injected cocaine, last 3 mo. | 0.56 | (0.35 – 0.89)* | NA | |
| Used a shared cooker, last 3 mo. | 0.41 | (0.27 – 0.62)** | NA | |
| Borrowed used needle, last 3 mo. | 0.29 | (0.16 – 0.53)** | NA | |
| Injected someone's rinse, last 3 mo. | 0.23 | (0.13 – 0.42)** | NA | |
| Pooled money to buy drugs, last 3 mo. | 0.40 | (0.27 – 0.60)** | NA | |
| Overdosed, last 3 mo. | 0.24 | (0.07 – 0.77)* | NA | |
| Lagged time-dependent non-injection drug use | ||||
| Drank alcohol, last mo. | 0.55 | (0.37 – 0.81)** | 0.74 | (0.40 – 1.35) |
| Used marijuana last 3 mo. | 0.86 | (0.51 – 1.45) | 0.71 | (0.36 – 1.40) |
| Smoked or snorted heroin, last 3 mo. | 0.78 | (0.44 – 1.37) | 1.86 | (0.23 – 14.83) |
| Smoked or snorted crack, last 3 mo. | 0.97 | (0.66 – 1.44) | 1.27 | (0.62 – 2.56) |
| Smoked or snorted cocaine, last 3 mo. | 0.62 | (0.36 – 1.08) | 0.88 | (0.40 – 1.98) |
| Smoked or snorted methamphetamine, last 3 mo. | 1.05 | (0.71 – 1.56) | 1.44 | (0.71 – 2.93) |
| Used opiate pills, last 3 mo. | 0.65 | (0.44 – 0.96) | 0.56 | (0.25 – 1.26) |
| Used benzodiazepine pills, last 3 mo. | 0.44 | (0.27 – 0.70)** | 1.60 | (0.90 – 2.85) |
| Lagged time-dependent sexual behavior | ||||
| Any sex partner, last 3 mo. | 0.73 | (0.47 – 1.13) | 1.11 | (0.60 – 2.07) |
| Sex in exchange for money or drugs, last 3 mo. | 1.28 | (0.66 – 2.47) | 1.36 | (0.33 – 5.65) |
| IDU sex partner, last 3 mo. | 0.65 | (0.46 – 0.96)* | 0.74 | (0.34 – 1.58) |
| Any unprotected sex, last 3 mo. | 1.46 | (0.81 – 2.64) | 0.95 | (0.36 – 2.52) |
p-value < 0.01
p-value < 0.05
behavioral variables were time-lagged by one quarterly visit in order to identify behaviors that occurred in the three months prior to cessation rather than behaviors that were occurring concurrently with (or as the result of) cessation.
In analyses of time-lagged IDU and related behaviors, those reporting less than 30 injection events in the month prior to the period examined for cessation were more likely to report injection cessation (HR = 3.56). We found injection cessation to be inversely associated with injecting daily (HR = 0.43), injecting heroin or heroin mixed with other drugs (HR = 0.31), injecting cocaine (HR = 0.56), borrowing a used needle (HR = 0.29), sharing a cooker (HR = 0.41), injecting someone else's rinse (HR = 0.23), and experiencing an overdose (HR = 0.24).
Among non-injection drug use behaviors, we found inverse associations with drinking alcohol (HR = 0.55) and benzodiazepine use in the past 3 months (HR = 0.33) and injection cessation. We did not find associations with marijuana use, smoking or snorting heroin, crack, or methamphetamine.
We examined social characteristics, such as having a sex partner who is an IDU, pooling money to buy drugs, and exchanging sex for money. Pooling money to buy drugs in the past 3 months (HR = 0.40) and having an IDU sex partner (HR = 0.65) were inversely associated with cessation. Exchanging sex for money was not associated with cessation.
Table 3 shows results of multivariate analysis. Factors independently associated with injection cessation included injecting <30 times per month (Adjusted Hazard Ratio (AHR) = 2.31), injecting heroin or heroin mixed with other drugs (AHR = 0.53), alcohol use (AHR = 0.61), benzodiazepine use in the prior 3 months (AHR = 0.57), injecting the residue from a used cotton or cooker (AHR = 0.40), participation in recent drug treatment (AHR = 2.08), and a history of incarceration (AHR = 0.48). The model met the proportional hazards assumption (p = 0.55) and the likelihood ratio test for the addition of time interacted variables was not significant (p = 1.00).
Table 3.
Adjusted hazard ratios for injection cessation in young IDU in the UFO Cohort Study, San Francisco, CA, 2000-2008 (N=362).
| Characteristic | Adj HR |
(95% CI) |
|---|---|---|
| History of incarceration | 0.48 | (0.29 – 0.78)** |
| Drug treatment, last 3 mo. | 2.08 | (1.31 – 3.29)** |
| Less than 30 injection events, last mo. | 2.31 | (1.45 – 3.69)** |
| Injected heroin or heroin mixed with other drugs, last 3 mo. | 0.53 | (0.33 – 0.85)** |
| Injected someone's rinse, last 3 mo. | 0.40 | (0.21 – 0.75)** |
| Drank alcohol, last month | 0.61 | (0.41 – 0.92)* |
| Used benzodiazepine pills, last 3 mo. | 0.57 | (0.34 – 0.94)* |
p-value < 0.01
p-value < 0.05
3.3. Relapse to injection
Forty-nine of the seventy-nine (62%) subjects that ceased injection and who had follow-up visits after cessation relapsed to injection. The incidence of relapse was 55.5 (95% CI: 41.9 – 73.4) per 100 person-years overall, but dropped to 30.2 (16.2 – 56.1) per 100 person-years among those aged 27 and older at date of cessation (p = 0.02, data not shown). Twenty-seven participants reported a single relapse episode and 22 reported multiple episodes of relapse and cessation. Of the 22 participants who reported multiple episodes of relapse and cessation, 16 reported no drug injection in the last 3 months on their last visit.
Crude and adjusted hazard ratios for associations with relapse to injection are shown in Tables 2 and 4. Younger age at cessation was the only factor independently associated with relapse to injection (AHR = 2.30). The model met the proportional hazards assumption (p = 0.59) and did not contain time varying effects.
Table 4.
Adjusted hazard ratios for relapse to injection among injection ceasers in the UFO Cohort Study, San Francisco, CA, 2000-2008 (N=79).
| Characteristic | AHR | (95% CI) |
|---|---|---|
| Age at cessation < 27 years | 2.30 | (1.15 – 4.62)* |
p-value < 0.05
4. Discussion
Over one-quarter (29%) of young IDU followed prospectively in the UFO Study reported ceasing injection for three or more months. Of those followed after cessation approximately one-third maintained injection cessation while the majority (two-thirds) relapsed to injection. These findings are consistent with longitudinal patterns of drug injection behavior reported among IDU in the ALIVE cohort in Baltimore, MD by Galai et al. who found 20% ceased injection, 14% relapsed once, 37% had multiple transitions, and 29% never ceased injecting (Galai et al., 2003).
Drug use and injection-related behaviors inversely associated with ceasing injection were injecting heroin mixed with methamphetamine or cocaine, injecting the residue from a cooker (rinses), use of benzodiazepines, and drinking alcohol. Injecting drug mixes and injecting rinses can be indicative of a more severe drug habit which may make cessation more difficult (Bruneau et al., 2004). Benzodiazepine use among IDUs is associated with poorer health and psychosocial functioning (Darke, 1994; Darke et al., 1992; Fry and Bruno, 2002). Injection cessation was over three times as likely to occur among those who reported less than 30 injection events in the month prior to cessation compared to those reporting 30 or more injections. Daily drug injection, especially to prevent withdrawal symptoms among opiate users, is yet another marker of increased addiction severity. Unfortunately, younger drug users are often assumed to be too young to have lengthy injection careers or severe drug dependence. They may receive short-term detoxification and counseling but traditionally are denied access to effective opioid agonist maintenance treatment with methadone or buprenorphine (Woody et al., 2008).
We found an independent, inverse association between history of incarceration and injection cessation. IDU with a history of incarceration are more likely to be homeless and to report high risk-injecting behavior, and are less likely to enroll in drug treatment programs (Kittikraisak et al., 2006; Shah et al., 2000). Our findings are consistent with studies reporting higher rates of cessation among those currently employed (Steensma et al., 2005) and lower rates among those with a history of incarceration or involved in illicit or marginal activities (Bruneau et al., 2004; Galai et al., 2003; Joe et al., 1991; Warner et al., 2004).
Recent entry into drug treatment was independently associated with injection cessation, which is consistent with the findings of other studies (Galai et al., 2003; Goldstein et al., 2000; Henderson et al., 2003; Latkin et al., 1999; Shah et al., 2006). Type of drug treatment program was not collected throughout all waves of data collection. As a result, we did not have sufficient statistical power to examine potential differences in cessation and relapse by drug treatment modality.
Some limitations of the study were that initiation and length of drug use cessation and relapse could not be measured in those lost to follow-up or missing quarterly interviews, potentially biasing the estimates of the rates of cessation and relapse. We did not record cessation episodes that occurred prior to study enrollment, thus cessation episodes were potentially undercounted. Assuming that cessation of injection was related to loss to follow-up after study enrollment, actual incidence of cessation could be as high as 35% if all subjects lost to follow-up had ceased injection. Theorizing that loss to follow-up after cessation represents continued abstinence, we calculated a hypothetical incidence of relapse giving all 26 who were lost to follow-up a person-time equal to the median number of days of cessation for injectors who sustained cessation and were followed (median 175 days). Under this scenario, the incidence of relapse would change from 55.5 per 100 person-years to 51.7 per 100 person-years. Likewise, if we were to assume subjects lost to follow-up after cessation had resumed injection, incidence of relapse would be 79.2 per 100 person-years.
Another limitation to our findings is that self-reported behavioral information potentially introduced social desirability bias. Underreporting of risk behavior information would have a conservative effect on the measures of association. To minimize this, all interviews in our study were conducted at a neutral setting and all staff were well-trained to conduct a non-judgmental interview.
Our study provides important information on the incidence of injection cessation and relapse in a longitudinal community sample of young adult IDU and identifies several predictors of injection cessation and relapse. We observed a higher incidence of relapse in the younger subjects in this cohort, supporting the call for earlier detection and treatment through screening, brief intervention, referral and treatment programs for adolescents and transition-age youth (Clark, 2008). Indeed, the nonmedical use of prescription-type pain relievers, tranquilizers, stimulants, and sedatives surpassed marijuana for the first time as the most common illicit drug used in the past month by youths aged 12-13 years (Substance Abuse and Mental Health Services Administration, 2007), and all indicators suggest that the prevalence of prescription opioid use among adolescents is increasing and serving as an expanded pathway to heroin injection and addiction (Compton et al., 2005; Siegal et al., 2003). School-based programs or family-centered prevention programs may be useful early detection strategies. More effective treatment interventions than brief detoxification and group or individual counseling are needed for younger IDU who are at higher risk of relapse.
In addition, because drug treatment was one of the few factors associated with injection cessation in study subjects of all ages, increased opportunities for drug treatment are essential. While these may take the form of treatment-on-demand initiatives that deliver easy access to those who are ready for treatment or materialize as publicly-funded drug treatment in lieu of incarceration for non-violent offenders, more research is needed to identify which forms of drug treatment are associated with longer episodes of injecting cessation. The most effective treatments for opioid dependence are maintenance opioid against therapy (National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998); however equally effective pharmacotherapies for stimulant dependence have yet to be identified.
In conclusion, young IDU remain at high risk of blood-borne infections and other negative health outcomes. Understanding of longitudinal patterns of injection drug use cessation and relapse and their determinants is critical for guiding public health interventions to reduce morbidity and mortality.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aceijas C, Stimson GV, Hickman M, Rhodes T. Global overview of injecting drug use and HIV infection among injecting drug users. Aids. 2004;18:2295–2303. doi: 10.1097/00002030-200411190-00010. [DOI] [PubMed] [Google Scholar]
- Alter MJ. Prevention of spread of hepatitis C. Hepatology. 2002;36:S93–98. doi: 10.1053/jhep.2002.36389. [DOI] [PubMed] [Google Scholar]
- Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf) 2005;27:281–291. doi: 10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
- Bruneau J, Brogly SB, Tyndall MW, Lamothe F, Franco EL. Intensity of drug injection as a determinant of sustained injection cessation among chronic drug users: the interface with social factors and service utilization. Addiction. 2004;99:727–737. doi: 10.1111/j.1360-0443.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- Clark W. Plenary Session - SBIRT: Adolescents and Transition Age Youth; Substance Abuse: Current Trends, Current Solutions, 32nd Annual National Conference of the Association for Medical Education and Research in Substance Abuse; Washington, D.C.. 2008. [Google Scholar]
- Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Darke S. The use of benzodiazepines among injecting drug users. Drug Alcohol Rev. 1994;13:63–69. doi: 10.1080/09595239400185741. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Ross M, Wodak A. Benzodiazepine use and HIV risk-taking behaviour among injecting drug users. Drug Alcohol Depend. 1992;31:31–36. doi: 10.1016/0376-8716(92)90005-w. [DOI] [PubMed] [Google Scholar]
- Doherty MC, Garfein RS, Monterroso E, Brown D, Vlahov D. Correlates of HIV infection among young adult short-term injection drug users. Aids. 2000;14:717–726. doi: 10.1097/00002030-200004140-00011. [DOI] [PubMed] [Google Scholar]
- Dore GJ, Law M, MacDonald M, Kaldor JM. Epidemiology of hepatitis C virus infection in Australia. J Clin Virol. 2003;26:171–184. doi: 10.1016/s1386-6532(02)00116-6. [DOI] [PubMed] [Google Scholar]
- Fry CL, Bruno RB. Recent trends in benzodiazepine use by injecting drug users in Victoria and Tasmania. Drug Alcohol Rev. 2002;21:363–367. doi: 10.1080/0959523021000023225. [DOI] [PubMed] [Google Scholar]
- Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano DD. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort, 1988-2000: description and determinants. Am J Epidemiol. 2003;158:695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Doherty MC, Monterroso ER, Thomas DL, Nelson KE, Vlahov D. Prevalence and incidence of hepatitis C virus infection among young adult injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18 1:S11–19. doi: 10.1097/00042560-199802001-00004. [DOI] [PubMed] [Google Scholar]
- Goldstein MF, Deren S, Magura S, Kayman DJ, Beardsley M, Tortu S. Cessation of drug use: impact of time in treatment. J Psychoactive Drugs. 2000;32:305–310. doi: 10.1080/02791072.2000.10400454. [DOI] [PubMed] [Google Scholar]
- Hahn JA, Page-Shafer K, Lum PJ, Bourgois P, Stein E, Evans JL, Busch MP, Tobler LH, Phelps B, Moss AR. Hepatitis C virus seroconversion among young injection drug users: relationships and risks. J Infect Dis. 2002;186:1558–1564. doi: 10.1086/345554. [DOI] [PubMed] [Google Scholar]
- Henderson LA, Vlahov D, Celentano DD, Strathdee SA. Readiness for cessation of drug use among recent attenders and nonattenders of a needle exchange program. J Acquir Immune Defic Syndr. 2003;32:229–237. doi: 10.1097/00126334-200302010-00017. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD, Hubbard RL. Treatment predictors of tenure in methadone maintenance. J Subst Abuse. 1991;3:73–84. doi: 10.1016/s0899-3289(05)80007-0. [DOI] [PubMed] [Google Scholar]
- Kittikraisak W, Davidson PJ, Hahn JA, Lum PJ, Evans JL, Moss AR, Page-Shafer K. Incarceration among young injectors in San Francisco: associations with risk for hepatitis C virus infection. Journal of Substance Use. 2006;11:271–281. [Google Scholar]
- Langendam MW, van Brussel GH, Coutinho RA, van Ameijden EJ. Methadone maintenance and cessation of injecting drug use: results from the Amsterdam Cohort Study. Addiction. 2000;95:591–600. doi: 10.1046/j.1360-0443.2000.95459110.x. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Knowlton AR, Hoover D, Mandell W. Drug network characteristics as a predictor of cessation of drug use among adult injection drug users: a prospective study. Am J Drug Alcohol Abuse. 1999;25:463–473. doi: 10.1081/ada-100101873. [DOI] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008:372. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Brecht ML, Herbeck D, Evans E, Huang D, Hser YI. Longitudinal HIV Risk Behavior Among the Drug Abuse Treatment Outcome Studies (DATOS) Adult Sample. Eval Rev. 2008;32:83–112. doi: 10.1177/0193841X07307411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. Effective medical treatment of opiate addiction. Jama. 1998;280:1936–1943. [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Hepatitis C Community Drug Alert Bulletin. [10.17.08];2000 Available: http://www.drugabuse.gov/HepatitisAlert/HepatitisAlert.html.
- Office of National Drug Control Policy. The Economic Costs of Drug Abuse in the United States, 1992-2002. Washington, DC: Executive Office of the President; 2004. Publication No. 207303. [Google Scholar]
- Schutz CG, Rapiti E, Vlahov D, Anthony JC. Suspected determinants of enrollment into detoxification and methadone maintenance treatment among injecting drug users. Drug Alcohol Depend. 1994;36:129–138. doi: 10.1016/0376-8716(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Shah NG, Celentano DD, Vlahov D, Stambolis V, Johnson L, Nelson KE, Strathdee SA. Correlates of enrollment in methadone maintenance treatment programs differ by HIV-serostatus. Aids. 2000;14:2035–2043. doi: 10.1097/00002030-200009080-00020. [DOI] [PubMed] [Google Scholar]
- Shah NG, Galai N, Celentano DD, Vlahov D, Strathdee SA. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988-2000. Drug Alcohol Depend. 2006;83:147–156. doi: 10.1016/j.drugalcdep.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Siegal HA, Carlson RG, Kenne DR, Swora MG. Probable relationship between opioid abuse and heroin use. Am Fam Physician. 2003;67:942–945. [PubMed] [Google Scholar]
- Steensma C, Boivin JF, Blais L, Roy E. Cessation of injecting drug use among street-based youth. J Urban Health. 2005;82:622–637. doi: 10.1093/jurban/jti121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings, Rep No NSDUH Series H-34 DHHS Publication No SMA 08-4343. Rockville, MD: 2008b. [Google Scholar]
- van Ameijden EJ, Coutinho RA. Large decline in injecting drug use in Amsterdam, 1986-1998: explanatory mechanisms and determinants of injecting transitions. J Epidemiol Community Health. 2001;55:356–363. doi: 10.1136/jech.55.5.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner LA, Alegria M, Canino G. Remission from drug dependence symptoms and drug use cessation among women drug users in Puerto Rico. Arch Gen Psychiatry. 2004;61:1034–1041. doi: 10.1001/archpsyc.61.10.1034. [DOI] [PubMed] [Google Scholar]
- Woody GE, Poole SA, Subramaniam G, Dugosh K, Bogenschutz M, Abbott P, Patkar A, Publicker M, McCain K, Potter JS, Forman R, Vetter V, McNicholas L, Blaine J, Lynch KG, Fudala P. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. Jama. 2008;300:2003–2011. doi: 10.1001/jama.2008.574. [DOI] [PMC free article] [PubMed] [Google Scholar]


