Abstract
Objective. We evaluated the efficacy of a brief, clinic-based, safer sex program administered by a lay health adviser for young heterosexual African American men newly diagnosed with a sexually transmitted disease (STD).
Methods. Subsequent to STD diagnosis, eligible men (N = 266; aged 18–29 years) were randomized to either a personalized, single-session intervention (delivered by a lay health adviser) or standard of care. We conducted behavioral assessments at baseline and 3 months postintervention (retention was 74.1%). We also conducted a 6-month clinic record review.
Results. Compared to men randomized to the control condition, those receiving the intervention were significantly less likely to acquire subsequent STDs (50.4% vs 31.9%; P = .002) and more likely to report using condoms during last sexual intercourse (72.4% vs 53.9%; P = .008). They also reported fewer sexual partners (mean 2.06 vs 4.15; P < .001) and fewer acts of unprotected sex (mean 12.3 vs 29.4; P = .045). Based on a 9-point rating scale, men in the intervention group had higher proficiency scores for condom application skills (mean difference = 3.17; P < .001).
Conclusion. A brief clinic-based intervention delivered by a lay health adviser may be an efficacious strategy to reduce incident STDs among young heterosexual African American men.
In the United States, AIDS case rates are approximately 8 times higher among African American men than among White men.1,2 African American men have the highest prevalence and incidence rates of AIDS of all demographic classifications of US residents. Particularly in the South,3–5 African American men are also disproportionately affected by sexually transmitted diseases (STDs).6 Given these disparities, an important public health imperative is to develop and test interventions designed to reduce the risk of HIV or other STD acquisition among African American men—especially young African American men, who are at the greatest risk of infection.7,8 The imperative applies to both African American men who have sex with men and those who have sex with women. In general, however, heterosexual men of all racial/ethnic origins have been largely neglected with respect to the development and evaluation of HIV prevention interventions.9–11
Few studies have specifically investigated clinic-based approaches to reducing HIV or other STDs among young African American men who have sex with women. For example, in a recent review of effective behavioral interventions for HIV infection, Lyles et al. identified 18 programs that met established methodological criteria.12 Of these 18, 14 were designed for persons who were not knowingly HIV positive, and of these 14, none was designed for heterosexual African American men. The Centers for Disease Control and Prevention currently endorses a brief (60-minute) clinic-based program delivered in a small-group format designed to promote safer sex among African American and Hispanic men of all ages.13 To evaluate program efficacy, investigators used a clinic record review (mean of 17 months) to monitor subsequent STDs. Men randomized to the intervention (22.5%) were less likely to acquire a subsequent STD than were men in the routine-care group (26.8%).14
Although organizing groups of 3 to 8 men demonstrates efficacy, this may be problematic in many STD clinics from an operational perspective. In a multicenter randomized controlled trial, a one-to-one tailored counseling intervention was evaluated among STD clinic patients.15 Patients randomized to the enhanced counseling and the brief counseling conditions were less likely to acquire subsequent STDs over a 6-month follow-up (estimated odds ratio [OR] = 0.69 and 0.71, respectively). The trial had a low participation rate (44%) and high attrition (49%). Although the trial demonstrated a treatment advantage, there was a marginal treatment effect for the primary behavioral outcome, unprotected vaginal sex. Subsequent reanalysis of the data indicated that intervention effects were not uniform across age groups. For example, among adolescents younger than 20 years, the 12-month STD incidence was 17.2% in the enhanced (intervention) group versus 26.6% in the control group. However, among young adults aged 20 to 25 years, intervention effects were markedly smaller (13.1% vs 14.8%).16
In another study, a single-session clinic-based intervention produced significant effects in a subset analysis of young men (aged 20–30 years) and African American men over a 6- to 9-month follow-up period,17 whereas in a 6-session, video-based intervention, reductions were observed in self-reported unprotected vaginal sex among African American men recruited from an urban STD clinic.18 Unfortunately, the former study was not designed specifically for African American men and was evaluated using a nonrandomized design, whereas the latter study used a small-group intervention format, which limits its utility for clinic-based implementation, and did not assess subsequent STD acquisition. Finally, a clinic-based study using a 1-month (3-session) intervention format failed to observe significant differences in STD acquisition.19
We sought to test the efficacy of a clinic-based, safer sex program specifically designed for young heterosexual African American men newly diagnosed with an STD and residing in the southern United States. The trial tested the hypothesis that men randomized to the intervention group would be significantly less likely than would be controls to acquire a subsequent STD and to engage in unprotected sex. Hypotheses pertaining to fewer sexual partners and greater condom application skills for men receiving the intervention were also tested.
METHODS
Participants
The study was conducted September 2004 through May 2006. Men were recruited from a public STD clinic located in a southern US city. Recruitment occurred following diagnosis and treatment for STDs. Nurses assessed potential eligibility by determining whether men (1) were newly diagnosed with an STD, (2) self-identified as African American, and (3) were aged 18 to 29 years. Potentially eligible men were asked if they would be interested in volunteering for a study. Those indicating any level of interest (N = 306) were escorted to the project's lay health adviser (in an adjacent office), who further screened men for eligibility by determining whether men were English speaking and by asking 2 questions: (1) Are you knowingly HIV positive? and (2) Have you used a male condom at least once in the past 3 months for sexual intercourse (defined as “penis in the vagina”) with a woman?
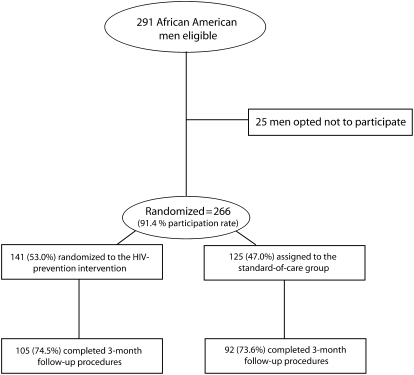
Of the 306 potentially eligible men screened by the lay health adviser, 15 were deemed ineligible based on their responses to the second set of eligibility criteria. These inclusion criteria were important because the brief nature of the intervention was designed specifically to improve the quality and consistency of condom use among men reporting recent experience with condom use. Of the 291 men deemed eligible, 266 (91.4%) were randomized to the 2 trial conditions (Figure 1).
FIGURE 1.
Allocation of study participants in a randomized, controlled trial of a brief, clinic-based intervention to promote STD protective behaviors: Southern United States, September 2004 Through May 2006.
Note. STD = sexually transmitted disease.
Study Design
In a 2-arm randomized control trial, we used concealment of allocation techniques to minimize allocation bias.20 Before implementing the trial, a random sequence was determined, and envelopes containing allocation cards (coded for intervention or control) were sealed, randomly sequenced, and piled; the top envelope on the pile was always used to determine assignment to group. The trial was conducted using a 3-month follow-up assessment and a 6-month medical-records review to assess intervention efficacy.
Intervention Methods
Based on recent evidence suggesting that young African American men experience multiple difficulties with condoms,21,22 we designed the intervention to promote men's quality, correctness, and consistency of condom use. A 1-year formative phase was used to develop the intervention. In an initial elicitation study (that used the same inclusion criteria as the trial), we collected qualitative data pertaining to men's barriers in achieving correct and consistent condom use.21 We used the findings to develop the brief (approximately 45–50 minutes long) intervention, which we then tested and revised based on identified gaps.
The program (named Focus on the Future) was based on a lay health adviser model. Evidence suggests that lay health advisors are instrumental in achieving intervention success among various populations of African Americans across a broad range of health behaviors.23 The essence of the model is that the most effective change agents are people who come from the community for which the intervention program is intended. This goes beyond the concept of “matching” by race, age, and gender.24
A young African American male who had grown up and resided in the main catchment area served by the clinic was selected, hired, and trained to implement the intervention. His everyday experiences and communication style were indeed no different from those of the men participating in the intervention. The lay health adviser was selected based on his ability to effectively discuss sex and condom use with men in a nonjudgmental manner. Part of this ability included being adept at quickly establishing rapport with men by finding common ground between them. Once selected, he attended a 3-day training seminar designed to provide him the skills and information needed to deliver the single-session intervention.
The single session was predicated on the information, motivation, and behavioral skills model.25 Information directly relevant to the quality of condom use was provided. For example, men learned that condoms come in a variety of sizes and shapes, and they learned about the value of periodically adding water-based lubricants to condoms during sexual intercourse. Men learned, by demonstration from the lay health adviser, that oil-based lubricants can quickly erode latex condoms. Enhancing men's motivation to use condoms was an integral component of the session. Throughout the session, the advisor encouraged men to feel good about using condoms, to experience condoms as being compatible with sexual pleasure, and to actively protect themselves from future STD acquisition. The lay health adviser constantly attempted to equate condom use with an investment in the men's future.
The participants were also motivated to personally respond to the AIDS epidemic through our use of large posters illustrating the disproportionate HIV/AIDS burden experienced by African American men. An equally important, but implicit, objective was to have the advisor be responsive to men's questions, problems, and concerns regarding safer sex with their female partners. Men were prompted to think about ways they could initiate condom use with existing partners. Skill acquisition was also emphasized. Correct condom and lubrication use were demonstrated and practiced by men until they expressed a sense of mastery. Men were encouraged to use condoms they felt fit them comfortably and provided them with a sense of security. Based on formative work,21 we decided to provide men with pocket-size vials of water-based lubricants as well as 12 or more condoms of their choice from a broad selection of brands and sizes.
All men enrolled in the study received nurse-delivered messages regarding condom use per Centers for Disease Control and Prevention guidelines.26 These messages were typically delivered in only a few minutes and essentially informed men that condoms are an effective means of preventing subsequent STD acquisition when used consistently. As patients of the clinic, all men were allowed to take up to 12 condoms—with only 1 size and brand available—from the clinic as they exited. In addition to the disease-specific diagnosis and treatment the men received, these procedures comprised clinical standard of care. Men randomized to the control group received only this standard of care, whereas men randomized to the intervention group received this standard of care and participated in the Focus on the Future program.
Data Collection
Immediately following diagnosis and study enrollment, men completed a self-administered questionnaire that the lay health advisor gave them. To avoid problems associated with low literacy, questions were recorded onto a compact disc that men could play using a portable headset. Next, men completed a directly observed condom-application skills assessment. The same procedures were repeated at the follow-up assessment. Men were compensated $40 for the first assessment and $60 for the second.
Primary Outcome Measure
Subsequent diagnosis of an STD constituted the primary outcome. Because this publicly funded clinic was the only low-cost option for men in the entire urban catchment area, a medical-records review was used to assess this outcome.
Other Outcome Measures
Four behavioral outcomes were assessed: (1) number of female sexual partners in the past 3 months, (2) condom use during the last act of penetrative (penile–vaginal or penile–anal) sexual intercourse with a female partner, (3) frequency of unprotected penetrative sexual intercourse with a female partner in the past 3 months, and (4) proficiency in using condoms as determined through direct observation of men's ability to apply condoms to a stationary, life-size, rubber penile model. For the fourth behavioral outcome, a 9-item checklist was refined based on previous research conducted by R. J. D.27 This checklist comprised “yes” versus “no” indicators completed by the lay health adviser as men demonstrated the task of condom application.
Statistical Analyses
Demographic and baseline attributes among intervention and control participants were compared via the 2-sample t test with unrestricted variances for quantitative variables and the χ2 test for dichotomous variables. Demographic and baseline attributes among participants who dropped out of the study and participants who remained in the study were compared similarly.
The outcomes of reinfection at any time within the 6 months and condom use at the last sexual act preceding the 3-month follow-up were analyzed via logistic regression. Remaining outcomes were analyzed via linear regression. Univariate analyses used only intervention or control status as a predictor, and multivariable analyses used intervention or control status and several covariates.
First, a dichotomized version of monthly income was used as a covariate. Monthly income served as a proxy indicator of socioeconomic status. Despite the relatively low average income of the sample, we suspected that socioeconomic status may nonetheless be an important determinant of safer sex practices and reinfection. Second, whether men were diagnosed as having 1 versus multiple STDs at baseline served as a covariate; this provided an objective marker of past sexual risk behavior among this sample of high-risk men. Given the strong predictive power of past behavior to predict future behavior, we determined that this measure was an important covariate. Third, the corresponding baseline measure of the outcome variable (except for reinfection) was always included as a covariate. Fourth, the outcome of reinfection was considered to be confounded by condom use and condom use skills; thus, follow-up values for these 2 variables were included as covariates.
Because outcome variables (except reinfection) had missing values because of attrition, the primary data analyses (described in the previous paragraph) were performed twice: first with only complete cases (participants for whom there were no missing values) and then with multiple imputation28 as implemented in the MI and MIANALYZE procedures of SAS version 9.1 (SAS Institute, Cary, North Carolina).
Finally, because there were some extreme outlying observations with respect to the first and third behavioral outcomes, sensitivity analyses were performed to complement the primary analyses. One set of sensitivity analyses entailed the removal of records with extreme outlying values, and the other involved logarithmic transformations to mitigate the outliers’ influence. All analyses were conducted in SAS version 9.1.
RESULTS
Baseline Comparability of Groups
We assessed differences between men randomized to the intervention and control conditions for demographic and other key variables at baseline (Table 1). The only significant difference observed was demonstrated condom application skills, with men in the control condition scoring lower than men in the intervention condition.
TABLE 1.
Demographic and Other Baseline Attributes of Enrollees in a Risk-Reduction Intervention Evaluation of African American Men Aged 18 to 29 Years Newly Diagnosed With an STD, by Group Assignament: Southern United States, September 2004 Through May 2006
| Intervention (n = 141), Mean ±SD or No. (%) | Control (n = 125), Mean ±SD or No. (%) | P | |
| Age, y | 23.1 ± 3.4 | 23.4 ± 3.1 | .49 |
| Net monthly income > $1000 | 38 (27.0) | 42 (33.9)a | .22 |
| Current relationship is monogamous | 68 (48.6)b | 60 (48.0) | .92 |
| Current relationship is not monogamous | 59 (42.1)b | 54 (43.2) | .86 |
| Previously taught how to use condoms | 127 (90.1) | 110 (88.7)a | .72 |
| Multiple STDs diagnosed at baseline | 41 (29.3)b | 27 (22.1)a | .19 |
| Baseline diagnosis included chlamydia | 55 (39.0) | 50 (40.3)a | .83 |
| Baseline diagnosis included gonorrhea | 87 (61.7) | 76 (61.3)a | .94 |
| Demonstrated condom use skills | 3.83 ± 2.24c | 2.60 ± 1.67d | <.001 |
| Number of female sexual partners, past 3 monthsf | 2.91 ± 2.73 | 3.08 ± 2.43 | .60 |
| Unprotected acts of sexual intercourse, past 3 monthsg | 16.0 ± 47.3h | 14.3 ± 21.0i | .72 |
| Used condoms last time sexual intercourse occurred | 74 (52.5) | 53 (42.4) | .10 |
Note. STD = sexually transmitted disease. All results pertain to men who self-identified as heterosexual.
Out of 124 participants with data for variable for which not all participants had data.
Out of 140 participants with data for variable for which not all participants had data.
Out of 131 participants with data for variable for which not all participants had data.
Out of 112 participants with data for variable for which not all participants had data.
eMedian and interquartile range were 3.0 and 1.0, respectively, for the control group and 2.0 and 1.0, respectively, for the intervention group. Excluding 4 participants in the control group and 3 in the intervention group who claimed more than 100 unprotected acts of sexual intercourse at baseline or follow-up or who claimed more than 25 partners at baseline or follow-up, mean and standard deviation are 3.02 and 2.29 for the control group and 2.70 and 1.71 for the intervention group.
Median and interquartile range were 6.5 and 18.0, respectively, for the control group and 4.0 and 13.0, respectively, for the intervention group. Excluding 4 participants in the control group and 3 in the intervention group who claimed more than 100 unprotected acts of sexual intercourse at baseline or follow-up or who claimed more than 25 partners at baseline or follow-up, mean and standard deviation are 13.51 and 18.08 for the control group and 11.75 and 19.44 for the intervention group.
Out of 123 participants with data for variable for which not all participants had data.
Out of 114 participants with data for variable for which not all participants had data.
Attrition
Among the 266 participants, 69 (25.9%) did not return to complete the 3-month follow-up assessment (Figure 1). However, we were still able to determine if these men acquired a subsequent STD. Comparing the 197 participants who remained in the study with the 69 who dropped out, there were no significant differences in sociodemographics or baseline attributes (Table 2). Further, the proportions of men dropping out were not significantly different between the 2 groups (intervention or control). Finally, men dropping out were not significantly different from men completing the study with respect to STD reinfection rates.
TABLE 2.
Differences Between Men Completing Follow-up Assessments and Those Not Completing Follow-up Assessments in a Risk-Reduction Intervention Evaluation of African American Men Aged 18 to 29 Years Newly Diagnosed With an STD: Southern United States, September 2004 Through May 2006
| Stayed in (n = 197), Mean ±SD or No. (%) | Dropped out (n = 69), Mean ±SD or No. (%) | P | |
| Age, y | 23.4 ± 3.3 | 23.0 ± 3.3 | .47 |
| Net monthly income > $1000 | 61 (31.1)a | 19 (27.5) | .58 |
| Current relationship is monogamous | 88 (44.9)a | 40 (58.0) | .06 |
| Current relationship is not monogamous | 88 (44.9)a | 25 (36.2) | .21 |
| Previously taught how to use condoms | 179 (91.3)a | 58 (84.1) | .09 |
| Multiple STDs diagnosed at baseline | 52 (26.7)b | 16 (23.9)c | .65 |
| Baseline diagnosis included chlamydia | 73 (37.2)a | 32 (46.4) | .18 |
| Baseline diagnosis included gonorrhea | 122 (62.2)a | 41 (59.4) | .68 |
| Demonstrated condom use skills | 3.39 ± 2.16d | 2.90 ± 1.84e | .09 |
| Number of female sexual partners, past 3 months | 3.13 ± 2.81 | 2.61 ± 1.78 | .08 |
| Unprotected acts of sexual intercourse, past 3 months | 16.6 ± 42.0f | 11.6 ± 17.9g | .21 |
| Used condoms last time sexual intercourse occurred | 90 (45.7) | 37 (53.6) | .26 |
| Assigned to intervention group | 105 (53.3) | 36 (52.2) | .87 |
| Reinfection | 78 (39.6) | 30 (43.5) | .57 |
Note. STD = sexually transmitted disease. All results pertain to men who self-identified as heterosexual.
Out of 196 participants with data for variable for which not all participants had data.
Out of 195 participants with data for variable for which not all participants had data.
Out of 67 participants with data for variable for which not all participants had data.
Out of 181 participants with data for variable for which not all participants had data.
Out of 62 participants with data for variable for which not all participants had data.
Out of 171 participants with data for variable for which not all participants had data.
Out of 66 participants with data for variable for which not all participants had data.
Effects of the Intervention
With 1 exception, the 5 outcome measures achieved univariate significance in both the complete case and multiple imputation analyses (Table 3). We used the complete case analysis to compare men in the control group and found that those in the intervention group were significantly less likely to acquire a subsequent STD within the 6-month follow-up interval (50.4% vs 31.9%; univariate OR estimate = 0.46; 95% confidence interval [CI] = 0.28, 0.76). Men in the intervention scored higher on the condom application skills assessment (mean difference estimate = 3.17; 95% CI = 2.81, 3.53; relative difference = +145%). Also, men in the intervention reported significantly fewer sexual partners (2.06 vs 4.15, mean difference estimate = –2.10; 95% CI = –3.22, −0.98; relative difference = –51%), significantly fewer acts of unprotected sex (12.3 vs 29.4; mean difference estimate = –17.1; 95% CI = –33.6, −0.5; relative difference = –58%) and were significantly more likely to report using condoms during their last episode of sexual intercourse (72.4% vs 53.9%; univariate OR estimate = 2.25; 95% CI = 1.24, 4.07). Of note, these results remained relatively unchanged with multiple imputation, with the exception of unprotected sex, which narrowly missed significance.
TABLE 3.
Intervention Versus Control Group Outcomes Assessed 3 Months Postintervention in a Risk-Reduction Intervention Evaluation of African American Men Aged 18 to 29 Years Newly Diagnosed With an STD: Southern United States, September 2004 Through May 2006
| Univariate Measure of Effect |
Multivariable Measure of Effect |
|||||
| Intervention (n = 141), No. (%) Mean ±SD (No.) | Control (n = 125), No. (%) Mean ±SD (No.) | OR Estimate (95% CI) | P | AOR Estimate (95% CI) | P | |
| Reinfectiona | 45 (31.9) | 63 (50.4) | 0.46 (0.28, 0.76) | .002 | 0.32 (0.12, 0.86) | .02 |
| Condom use skillsbc | 5.35 ± 1.21 (104) | 2.18 ± 1.30 (84) | 3.17 (2.81, 3.53) | <.001 | 3.21 (2.80, 3.63) | <.001 |
| Condom use skillsbd | 3.17 (2.79, 3.54) | <.001 | 3.19 (2.81, 3.56) | <.001 | ||
| Partners in past 3 monthscef | 2.06 ± 1.65 (105) | 4.15 ± 5.59 (91) | −2.10 (−3.22, −0.98) | <.001 | −2.09 (−3.18, −0.99) | <.001 |
| Partners in past 3 monthsdf | −1.85 (−2.97, −0.74) | .002 | −1.87 (−2.96, −0.79) | .001 | ||
| Unprotected acts of sexual intercourse, past 3 monthscgh | 12.3 ± 25.8 (99) | 29.4 ± 79.3 (84) | −17.1 (−33.6, −0.5) | .045 | −13.4 (−35.6, 8.8) | .23 |
| Unprotected acts of sexual intercourse, past 3 monthsdh | −14.9 (−31.0, 1.3) | .07 | −11.9 (−31.3, 7.5) | .21 | ||
| Condom used at last act of sexual intercourseci | 76 (72.4) | 49 (53.9) | 2.25 (1.24, 4.07) | .008 | 2.20 (1.08, 4.48) | .03 |
| Condom used at last act of sexual intercoursedi | 2.27 (1.23, 4.19) | .009 | 2.06 (1.07, 3.96) | .03 | ||
Note. STD = sexually transmitted infection. For quantitative variables, the measure of effect is a mean difference (expected score for intervention participant minus expected score for control participant, adjusted in the multivariable analyses for covariates specified below) and was estimated by linear regression. For dichotomous variables, the measure of effect is an odds ratio (odds in favor for intervention participant divided by odds in favor for control participant, adjusted in the multivariable analyses for covariates specified below) and was estimated by logistic regression. Complete case analyses used only those participants for whom there were no missing values on variables in the regression model. Multiple imputation analyses used all participants. All results pertain to men who self-identified as heterosexual. For variables on which not all participants had data, the numbers in parentheses identify how many participants did have data.
Multivariable analysis controls for monthly income level, having 1 vs 2 or more STDs diagnosed at study enrollment (mixed STDs), follow-up values for condom skills, and follow-up values for condom use at last act of sexual intercourse.
Multivariable analysis controls for income, mixed STDs, and the baseline value of condom skills.
Complete case analysis.
Multiple imputation.
Median and interquartile range are 2.0 and 3.0, respectively, for the control group and 2.0 and 2.0, respectively, for the intervention group. Excluding 4 participants in the control group and 3 in the intervention group who claimed more than 100 unprotected acts of sexual intercourse at baseline or follow-up or who claimed more than 25 partners at baseline or follow-up, mean and standard deviation are 3.52 and 4.04 for the control group and 2.00 and 1.47 for the intervention group.
Multivariable analysis controls for income, mixed STDs, and the baseline value for number of female sexual partners in the past 3 months.
Median and interquartile range are 4.5 and 21.0, respectively, for the control group and 1.0 and 11.0, respectively, for the intervention group. Excluding 4 participants in the control group and 3 in the intervention group who claimed more than 100 unprotected acts of sexual intercourse at baseline or follow-up or who claimed more than 25 partners at baseline or follow-up, mean and standard deviation are 17.24 and 28.77 for the control group and 11.12 and 21.96 for the intervention group.
Multivariable analysis controls for income, mixed STDs, and baseline values for skill, unprotected sex, and condom use at last act of sexual intercourse.
Multivariable analysis controls for income, mixed STDs, and the baseline values for skills and condom use at last act of sexual intercourse.
Multivariable analysis yielded more robust intervention effects on subsequent STD acquisition (Table 3). Men randomized to the intervention had about 68% lower odds of acquiring a subsequent STD (adjusted OR estimate = 0.32; 95% CI = 0.12, 0.86). Furthermore, findings from the multiple imputation analyses indicated that men in the intervention group had a higher score on the condom application assessment (mean difference estimate = 3.19; 95% CI = 2.81, 3.56), had fewer female sexual partners (mean difference estimate = –1.87; 95% CI = –2.96, −0.79), and were more likely to report condom use at last sexual episode (adjusted OR estimate = 2.06; 95% CI = 1.07, 3.96). One outcome did not achieve statistical significance in multivariable analyses, namely, number of episodes of unprotected sex in the past 90 days (mean difference estimate = –11.9; 95% CI = –31.3, 7.5).
Both sets of sensitivity analyses preserved the conclusions from the primary analyses that men in the intervention had significantly fewer female sexual partners than did men in the control group (Table 4). The sensitivity analyses involving logarithmically transformed number of unprotected acts preserved the mixed conclusions from the primary analyses, in particular statistical significance with univariate complete cases but lack thereof with multivariable multiple imputation. The sensitivity analyses entailing removal of records disagreed with the primary analyses only in that statistical significance was not achieved with univariate complete cases.
TABLE 4.
Results of Sensitivity Analyses for Selected Outcomes Measures Used to Compare Men Randomized to the Intervention Versus Control Groups in a Risk-Reduction Intervention Evaluation of African American Men Aged 18 to 29 Years Newly Diagnosed With an STD: Southern United States, September 2004 Through May 2006
| Univariate |
Multivariable |
|||
| Measure of Effect, Estimate (95% CI) | P | Measure of Effect, Estimate (95% CI) | P | |
| Observations with extreme outlying values excludeda | ||||
| Partners in past 3 monthscd | −1.52 (−2.37, −0.67) | <.001 | −1.37 (−2.18, −0.55) | .001 |
| Partners in past 3 monthsc,e | −1.28 (−2.14, −0.43) | .004 | −1.19 (−2.01, −0.36) | .006 |
| Unprotected acts of sexual intercourse, past 3 monthsc,f | −6.1 (−13.7, 1.4) | .11 | −1.0 (−9.8, 7.9) | .83 |
| Unprotected acts of sexual intercourse, past 3 monthsd,f | −4.6 (−12.0, 2.8) | .21 | −3.3 (−11.9, 5.4) | .43 |
| Response variable transformed logarithmically to reduce the impact of outlying valuesb | ||||
| Partners in past 3 monthsc,d | −0.33 (−0.49, −0.17) | <.001 | −0.32 (−0.47, −0.17) | <.001 |
| Partners in past 3 monthsc,e | −0.29 (−0.48, −0.10) | .004 | −0.29 (−0.48, −0.11) | .004 |
| Unprotected acts of sexual intercourse, past 3 monthsc,f | −0.53 (−1.00, −0.07) | .03 | −0.32 (−0.88, 0.24) | .26 |
| Unprotected acts of sexual intercourse, past 3 monthsd,f | −0.50 (−0.99, 0.00) | .051 | −0.42 (−1.00, 0.17) | .15 |
Note. STD = sexually transmitted disease.
Four participants in the control group and 3 participants in the intervention group were excluded who claimed more than 100 unprotected acts at baseline or follow-up or who claimed more than 25 partners at baseline or follow-up.
The transformed value is the natural logarithm of 1 plus the original value. Point and 95% confidence interval estimates for measures of effect are not directly comparable to those obtained in the absence of a logarithmic transformation; the main feature of interest is whether the P value is in qualitative agreement with the corresponding P value in Table 2 (i.e., both < .05 or both > .05).
Multivariable analysis controls for income, mixed STDs, and the baseline value for number of female sexual partners in the past 3 months.
Multivariable analysis controls for income, mixed STDs, and baseline values for skill, unprotected sexual intercourse, and condom use at last act of sexual intercourse.
DISCUSSION
The findings of our study clearly show the efficacy of this brief clinic-based intervention for young heterosexual African American men at risk of STD or HIV acquisition in terms of lower rates of subsequent STD acquisition, reduction in STD- or HIV-associated sexual behaviors, and improvement in condom application skills. The practical value of the findings is paramount, because they demonstrate marked reductions in STD incidence without the use of lengthy, resource-intensive programs. Moreover, the reduction in incidence over the 6-month postintervention period produced a larger effect size than did those observed in previous trials of brief, clinic-based interventions for African American men.14–19,29 The observed protective value relative to subsequent infection was also greater than that derived from a recent meta-analysis of clinic-based STD prevention programs (effect size: .32 vs .85).29 The treatment advantage may be attributable to multiple factors, such as tailoring to a relatively homogeneous population of men, intervening only with men who reported previous experience in using condoms, and the use of a lay health adviser model. The effect may also be partially explained by the observation that men randomized to the intervention group reported significantly fewer sexual partners at follow-up (an unexpected finding).
In an era when the Centers for Disease Control and Prevention has stated, “In the United States, the HIV/AIDS epidemic is a health crisis for African Americans,”30 the findings offer one approach to addressing this marked racial disparity. The findings also suggest a protective benefit for men's female sexual partners, who are typically African American. Because power imbalances in heterosexual relationships may favor males, intervention with African American men may also protect African American women against HIV or other STD acquisition.31 Indirect effects may also occur by lowering the prevalence of STDs within African American women's sexual networks.32 In turn, reductions in STD prevalence and incidence among African American men and women may mitigate the racial disparity in HIV/AIDS prevalence and incidence by removing STDs as a cofactor.33–36
The brief nature of the intervention also warrants comment. Implementation of small-group interventions or multisession interventions may not be optimally efficient in STD clinics. Because clinics are designed to provide patients with a series of one-to-one interactions with clinical staff, triaging young African American men newly diagnosed with an STD into an additional one-to-one session with a lay health adviser is a relatively simple expansion of the existing clinical paradigm. In addition, the use of a lay health adviser to implement the intervention may be a cost-effective strategy. The relative ease of implementation and higher cost-effectiveness may address the problem of effectively translating evidence-based research into practice.37–40
Limitations
There are a number of limitations to the study. First, as is true for all sexuality research, findings are limited by the validity of retrospective self-report, although this limitation is somewhat mitigated by the medical-records review findings pertaining to STD reinfection. Further, as is typically true for STD or HIV behavioral randomized trials, the use of a nonprobability sample limits the ability to generalize the findings to young heterosexual African American men newly diagnosed with an STD in other clinics of the United States. Another concern was the attrition rate. That 26% of the enrolled men did not return for the follow-up assessment (despite potential compensation of $60 and lack of employment) suggests that these men may experience instability in their daily lives, perhaps as a consequence of poverty and discrimination. However, differences between dropouts and men completing the study were not observed, and attrition was not a problem relative to the primary study outcome, because we were able to collect these data by medical record review.
Although urine-based polymerase chain reaction testing for subsequent STD acquisition may have been a more rigorous approach, the use of archival data is not uncommon, even in large-scale trials that employ polymerase chain reaction testing.41 Although we could not ascertain whether men were diagnosed with subsequent STD infections elsewhere with this study design, options for alternative sources of clinical care were limited and most likely would be comparably distributed between study groups. The relatively short duration of the follow-up period pertaining to behavioral outcomes is also a limitation, given that maintenance of intervention effects could not be assessed over longer periods. Also noteworthy is that the program was specifically designed to improve the quality, correctness, and frequency of use among men recently using condoms, thereby excluding those entirely rejecting condom use. This planning decision was made based on our awareness that a 40-minute intervention is unlikely to change behaviors of men who never use condoms. However, a complete lack of condom use (“never use”) among young African American men is not the norm; nationally representative data indicate that fewer than 1 of every 6 young African American men reported never using condoms during a 12-month recall period.42
It must also be acknowledged that the use of multiple raters would have allowed us to establish intrarater reliability for the measure of demonstrated condom application skills; this limitation should be considered in the larger context of the study findings (that is, the “skills variable” was only 1 of several supporting outcomes). Finally, the study design cannot determine what portion of the observed effect was attributable to the provision of condoms to men in a variety of sizes and brands. This is less a limitation than a product of the intervention's purpose of increasing men's pleasure in using condoms by providing a range of options.
Conclusions
The weight of evidence suggests that a brief, clinic-based intervention may be efficacious in reducing subsequent acquisition of STDs among young heterosexual African American men newly diagnosed with an STD. The use of a lay health advisor may help keep intervention costs low, thereby enabling program dissemination in resource-poor environments. As the United States40 and other countries43 implement clinic-based counseling in settings that provide STD screening, the option of postdiagnostic counseling conducted by a lay health adviser may prove useful. Adaptation and application of the program in geographic areas (domestically and globally) experiencing epidemics of STD or HIV may be worth pursuing in future studies.
Acknowledgments
Support for this project was provided by a grant from the National Institute of Mental Health (R21 MH066682-01A1). We gratefully acknowledge the assistance of the clinic director Deborah Snow and the clinic staff members. We also acknowledge the assistance from William Yarber, Stephanie Sanders, and Cindy Graham (the Kinsey Institute for Research in Sex, Gender, and Reproduction) relative to intervention development. Finally, we wish to acknowledge members of the data safety monitoring board, William Yarber, Willard Cates, and Lee Warner.
Human Participant Protection
Study procedures were approved by the Office of Research Integrity at the University of Kentucky. The trial was registered with the clinicaltrials.gov protocol registration system (No. NCT00314028) and monitored by a data safety monitoring board.
References
- 1.Centers for Disease Control and Prevention HIV/AIDS Surveillance, 2004 [year-end edition] Atlanta, GA: Centers for Disease Control and Prevention; 2004 [Google Scholar]
- 2.Centers for Disease Control and Prevention African Americans and AIDS. Atlanta, GA: Centers for Disease Control and Prevention; 2006 [Google Scholar]
- 3.Centers for Disease Control and Prevention HIV/AIDS Among African Americans. Fact Sheet. Available at: http://www.cdc.gov/hiv/topics/aa/resources/factsheets/aa.htm. Accessed May 19, 2008
- 4.Centers for Disease Control and Prevention Health Disparities Experienced by Black or African Americans, United States. MMWR Morb Mortal Wkly Rep. 2005;54:1–3 [PubMed] [Google Scholar]
- 5.Southern States AIDS/STD Directors Work Group Southern States Manifesto: HIV/AIDS & STDs in the South—A Call to Action. Available at: http://www.southernaidscoalition.org/FinalSouthernStatesManifesto.pdf. Accessed May 19, 2008
- 6.Centers for Disease Control and Prevention Sexually Transmitted Disease Surveillance, 2003. Atlanta, GA: Centers for Disease Control and Prevention; 2004 [Google Scholar]
- 7.Ruiz MS, Gable AR, Kaplan EH, Soto MA, Fienberg HV, Russell J. No Time to Lose: Getting More From HIV Prevention. Washington, DC: National Academies Press; 2001 [PubMed] [Google Scholar]
- 8.National Institutes of Health NIH fiscal year 2007 plan for HIV-related research. Available at: http://www.oar.nih.gov/public/pubs/fy2007/Overview.pdf. Accessed May 19, 2006
- 9.Seal DW, Ehrhardt AA. HIV-prevention-related sexual health promotion for heterosexual men in the United States: pitfalls and recommendations. Arch Sex Behav. 2004;33:211–212 [DOI] [PubMed] [Google Scholar]
- 10.Seal DW, Exner TM, Ehrhardt AA. HIV sexual risk reduction intervention with heterosexual men. Arch Intern Med. 2003;163:738–739 [PubMed] [Google Scholar]
- 11.Elway AR, Hart GJ, Hawkes S, Petticrew M. Effectiveness of interventions to prevent sexually transmitted infections and human immunodeficiency virus in heterosexual men: a systematic review. Arch Intern Med. 2002;162:1818–1830 [DOI] [PubMed] [Google Scholar]
- 12.Lyles CM, Kay LS, Crepaz N, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007;97:133–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Compendium of HIV prevention interventions with evidence of effectiveness. Available at: http://www.cdc.gov/hiv/resources/reports/hiv_compendium/organize.htm. Accessed May 19, 2008
- 14.O'Donnell CR, O'Donnell L, San Doval A, Duran R, Labes K. Reductions in STD infections subsequent to an STD clinic visit: using video-based patient education to supplement provider interactions. Sex Transm Dis. 1998;25:161–168 [DOI] [PubMed] [Google Scholar]
- 15.Kamb ML, Fishbein M, Douglas JM, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. JAMA. 1998;280:1161–1167 [DOI] [PubMed] [Google Scholar]
- 16.Bolu OO, Lindsey C, Kamb M, et al. Is HIV/Sexually transmitted disease prevention counseling effective among vulnerable populations? A subset analysis of data collected for a randomized controlled trail evaluating counseling efficacy (Project RESPECT). Sex Transm Dis. 2004;31:469–474 [DOI] [PubMed] [Google Scholar]
- 17.Cohen DA, Dent C, MacKinnon D, Hahn G. Condoms for men, not women: results of a brief promotion program. Sex Transm Dis. 1992;19:245–251 [DOI] [PubMed] [Google Scholar]
- 18.Kalichman SC, Cherry C, Browne-Sperling F. Effectiveness of a video-based motivational skills-building HIV risk reduction intervention for inner-city African American men. J Consult Clin Psychol. 1999;67:959–966 [DOI] [PubMed] [Google Scholar]
- 19.Maher JE, Peterman TA, Osewe PL, et al. Evaluation of a community based organization's intervention to reduce the incidence of sexually transmitted diseases: a randomized controlled trial. South Med J. 2003;96:248–253 [DOI] [PubMed] [Google Scholar]
- 20.Schulz KF. Subverting randomization in controlled trials. JAMA. 1995;274:1456–1458 [PubMed] [Google Scholar]
- 21.Crosby RA, Graham CA, Yarber WL, Sanders SA. If the condom fits, wear it: a qualitative study of young African American men. Sex Transm Infect. 2004;80:306–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crosby RA, Yarber WL, Sanders SA, et al. Men with broken condoms: who and why? Sex Transm Infect. 2007;83:71–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eng E, Parker E. Natural helper models to enhance a community's health and competence. : DiClemente RJ, Crosby RA, Kegler M, Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass Wiley; 2002: 126–156 [Google Scholar]
- 24.Jemmott JB III, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized, controlled trial. JAMA. 1998;279:1529–1536 [DOI] [PubMed] [Google Scholar]
- 25.Fisher J, Fisher W. The information-motivation-behavioral skills model. : DiClemente RJ, Crosby RA, Kegler M, Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass; 2002:40–70 [Google Scholar]
- 26.Centers for Disease Control and Prevention Sexually transmitted diseases treatment guidelines, 2002. MMWR Morb Mortal Wkly Rep. 2002;51:1–60 [Google Scholar]
- 27.DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent females: a randomized controlled trial. JAMA. 2004;292:171–179 [DOI] [PubMed] [Google Scholar]
- 28.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd ed Hoboken, NJ: Wiley; 2002 [Google Scholar]
- 29.Crepaz N, Horn AK, Rama SM, et al. The efficacy of behavioral interventions in reducing HIV risk sex behaviors and incident sexually transmitted diseases in Black and Hispanic sexually transmitted disease clinic patients in the United States: a meta-analytic review. Sex Transm Dis. 2007;34:319–332 [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention A heightened national response to the HIV/AIDS crisis among African Americans. Atlanta, GA: Department of Health and Human Services; 2007 [Google Scholar]
- 31.Puri CP, Balaiah D, Iyer KS. Increased male responsibility and participation: the key to improving reproductive health. Icmr Bull. 1999;29:59–70 [PubMed] [Google Scholar]
- 32.Pourbohloul B, Brunham RC. Network models and transmission of sexually transmitted diseases. Sex Transm Dis. 2004;31:388–390 [DOI] [PubMed] [Google Scholar]
- 33.Laga M, Monoka A, Kivuvu M, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS. 1993;7:95–101 [DOI] [PubMed] [Google Scholar]
- 34.Sorvillo F, Kernott P. Trichomonas vaginalis and amplification of HIV-1 transmission. Lancet. 1998;351:213–214 [DOI] [PubMed] [Google Scholar]
- 35.Wasserheit JN. Epidemiological synergy: interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19:61–72 [PubMed] [Google Scholar]
- 36.Grosskurth H, Mosha F, Todd J, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: a randomized controlled trial. Lancet. 1995;346:53–536 [DOI] [PubMed] [Google Scholar]
- 37.Kerner J, Rimer B, Emmons K. Dissemination research and research dissemination: how can we close the gap? Health Psychol. 2005;24:443–446 [DOI] [PubMed] [Google Scholar]
- 38.Glasgow RE, Lichtenstein E, Marcus AC. Why don't we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93:1261–1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glasgow RE. The future of health behavior change research: what is needed to implement translation research into health promotion practice. Ann Behav Med. 2004;27:3. [DOI] [PubMed] [Google Scholar]
- 40.Rietmeijer CA. Risk reduction counseling for prevention of sexually transmitted infections: how it works and how to make it work. Sex Transm Infect. 2007;83:2–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The National Institutes of Mental Health (NIMH) Multisite HIV Prevention Trial Group The NIMH Multisite HIV Prevention Trial: reducing HIV sexual risk behavior. Science. 1998;280:1889–1894 [DOI] [PubMed] [Google Scholar]
- 42.Udry R, Mullen Harris K, Elder GH. The National Longitudinal Study of Adolescent Health. Available at: http://www.cpc.unc.edu/addhealth/data. Accessed July 9, 2007
- 43.Ward H. One-to-one counseling for STI prevention: not so much whether as how. Sex Transm Infect. 2007;83:1. [PMC free article] [PubMed] [Google Scholar]