It has been widely accepted for over 10 years that secondhand smoke causes heart disease (Taylor et al. 1992; California Environmental Protection Agency 1997; California Environmental Protection Agency 2005; U.S. Department of Health and Human Services 2006), with about a 30% increase in risk associated with long-term living or working with smokers. (Newer evidence assessing exposure using the biomarker cotinine suggests that the risk could be twice as large (Whincup et al. 2004).) This relatively large increase in risk compared to the effects of active smoking is due to the rapid and substantial effects that secondhand smoke has on the cardiovascular system, particularly platelet activation and endothelial function (Glantz et al. 1991; Law et al. 1997; Barnoya et al. 2004; Pechacek et al. 2004; Raupach et al. 2006).
Since these effects play important roles in both the long-term development of atherosclerotic lesions, and the triggering of acute coronary events, it was not all that surprising when Sargent, et al. (Sargent et al. 2004) reported a significant drop in hospital admissions for acute myocardial infarction (AMI; ICD-9 code 410) while a 100% smokefree law was in effect in Helena, Montana. In addition, when enforcement of the ordinance was suspended, AMI admissions inside Helena rebounded. Sargent, et al, also examined admissions to the hospital from people living in the surrounding area (not covered by the ordinance) and found no change in AMI admissions from these people while the ordinance was in effect. Helena’s small size yielded a small study sample size and the confidence interval for the point estimate was correspondingly broad (Table 1). In addition, the size of the effect was surprisingly large: a 40% drop in admissions (RR=0.60, 95% CI 0.21, 0.99). While providing evidence that the elimination of secondhand smoke exposure caused the drop in hospital admissions, this result called out for independent validation.
Table 1.
Effects of clean indoor air ordinances on community hospital discharge rates
| Location/Study | Dates of Study Period | Number of cases in each study | Relative Risk | 95% CI | End Points |
|---|---|---|---|---|---|
| Helena, Montana Sargent, et al, (2004) | June through November (the months the law was in effect) from 1998 to 2003 | 304 | 0.60 | 0.21, 0.99 | Acute myocardial infarction (ICD-9 410) |
| Pueblo, Colorado Bartecchi, et al, (2006) | January 2002 through December 2004 | 2794 | 0.73 | 0.63, 0.85 | Acute myocardial infarction (ICD-9 410) |
| Piedmont, Italy Barone-Adesi, et al, (2006) | January 2001 through June 2005 | 4213 | 0.89 | 0.81, 0.98 | Acute myocardial infarction (ICD-9 410) in persons under 60 |
| Bowling Green, Ohio Khuder, et al, (2007) | January 1999 through June 2005 (beginning 6 months after law went into effect) | 1109 | 0.61 | 0.55, 0.67 | Ischemic heart disease (ICD-9 410–414) and heart failure (ICD-9 428) |
| Pooled Estimate (random effects model) | 0.73 | 0.56, 0.89 |
Since then, there have been two larger studies of AMI, one in Pueblo, Colorado (Bartecchi et al. 2006) and another in the Piedmont region of Italy (Barone-Adesi et al. 2006). These studies also found significant reductions in AMI admissions associated with implementation of smokefree laws (Table 1). Bartecchi, et al (Bartecchi et al. 2006) also examined AMI admissions in Colorado Springs, Colorado, a community similar to Pueblo without a smokefree ordinance, and found no significant change in admissions in Colorado Springs during the time that the Pueblo ordinance was in effect.
In this issue of Preventive Medicine, Khuder, et al. (Khuder et al. In press) provide another such independent validation of the fact that smokefree laws are associated with a rapid reduction in acute cardiovascular events. They found that hospital admissions for ischemic cardiovascular disease (ICD-9 codes 410-414) and heart failure (ICD-9 code 428) fell by 39% (RR=0.61, CI 0.55, 0.67) after Bowling Green, Ohio implemented a smokefree law. They also examined hospital admission patterns in Kent, Ohio, a matched control community with no such law, and found no changes in admissions patterns during the time that the Bowling Green law went into effect.
The fact that the Bowling Green study, like the other two U.S. studies, employed matched control communities without smokefree laws in which no change in risk was reported during the time that the risk reduction was found in the communities with these laws is a major strength of all three studies.
A notable methodological difference between the Bowling Green study and the three earlier studies is that the Bowling Green study included a broader range of cardiac diagnoses (all ischemic heart disease and heart failure rather than just AMI). Despite this difference, there are three reasons that it is reasonable to interpret findings from Khuder, et al. as comparable to the three prior studies. First, the rates of AMI are a relatively stable portion of all coronary heart disease (CHD), about 44% (ICD-9 410 compared to ICD-9 410-414 (Centers for Disease Control 2001)). If this is true, and if risk for AMI and risk for CHD due to secondhand smoke are similar, then AMI and CHD will have similar relative risks associated with secondhand smoke. Including this larger range of diagnoses would reduce the estimated variance for the study by Khuder, et al. because of a larger sample size than had they only included AMI. Second, our understanding of the biology is that secondhand smoke is a risk factor for CHD in general, not just AMI (Glantz et al. 1995), suggesting that it is reasonable to combine risks for AMI and CHD in a single meta-analysis. Third, previous estimates of risk for CHD due to secondhand smoke exposure is about the same size as the estimated risk for AMI (Glantz et al. 1991).
The Bowling Green study, unlike the others, considered the first six months of the smokefree ordinance’s implementation as part of the “non-intervention” period. Khuder et al. argue that delays in implementation and acceptance of the ordinance would produce a lagged effect. This analytic lag means that to the extent that there was an immediate effect on heart disease admissions, the Bowling Green study would underestimate the effect of the ordinance. This six-month lag also means that the study cannot assess the immediacy of the effect found in all three prior studies; conversely, it means that, to the extent that all communities experience some lag in effect, that the prior studies also underestimated the effect.
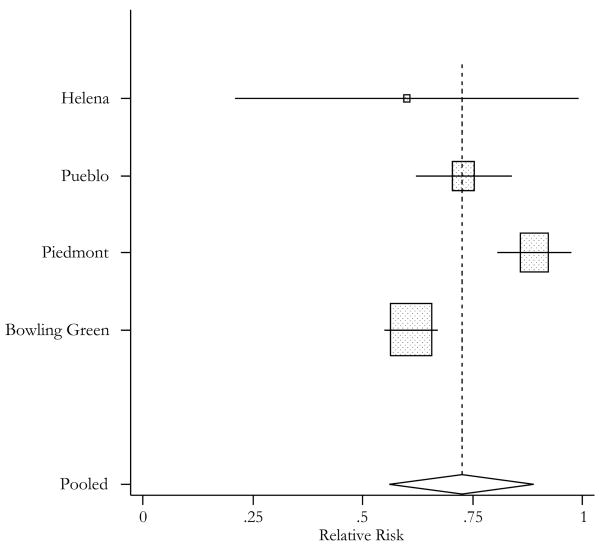
Now that there 4 similar studies, it is possible to pool them to obtain an overall estimate of the effects of smokefree ordinances on hospital admissions for coronary heart disease. The effect size estimates for the different studies are heterogeneous (Qd.f.=3=28.30, p<0.001), so we used a random effects meta-analysis using the meta package for Stata version 9.2. Overall, these four studies indicate that smokefree laws were associated with a 27% reduction (RR .73; CI 0.56, 0.89) in heart disease hospital admissions (Table 1 and Figure 1).
Figure 1.
Estimates of relative risk of hospital discharge following implementation of smokefree air ordnances presented for acute myocardial infarction (Helena, Pueblo, and Piedmont) or ischemic heart disease (Bowling Green) with 95% confidence band. Box size is inversely proportional to the variance of each study’s estimate. Diamond width indicates estimated 95% confidence band for the pooled risk.
As of January 2007, over half the U.S. population was covered by smokefree laws (American Nonsmokers’ Rights Foundation 2007), and such laws were spreading around the world. Besides immediately improving indoor air quality and reducing long-term risk of cardiovascular (and cancer and other diseases) (California Environmental Protection Agency 2005; U.S. Department of Health and Human Services 2006), these laws immediately and substantially (27%) reduce the risk of acute myocardial infarction and other cardiovascular events. The large, consistent, and immediate effect of these laws on health further strengthens the case for passing, fully implementing and enforcing them.
Acknowledgments
This work was funded by grants from the National Cancer Institute (CA-113710 and CA-61021). The funding agency had no role in the conduct of the research or preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Alexis Dinno, Postdoctoral Fellow, Center for Tobacco Control Research and Education, University of California, San Francisco, 530 Parnassus Ave, Suite 366, San Francisco, CA 94143-1390, Phone: (415) 476-3652, Fax: (415) 514-9345, alexis.dinno@ucsf.edu
Stanton Glantz, Professor of Medicine (Cardiology), Director, Center for Tobacco Control Research and Education, Cardiovascular Research Institute, University of California San Francisco, 530 Parnassus Ave, Suite 366, San Francisco, CA 94143-1390, Phone: (415) 476-3893, Fax: (415) 514-9345, glantz@medicine.ucsf.edu
References
- Percent of U.S. State Populations Covered by Local or State 100% Smokefree Air Laws, American Nonsmokers’ Rights foundation 2007 American Nonsmokers’ Rights Foundation. [Google Scholar]
- Barnoya J, and Glantz SA. Cardiovascular effects of secondhand smoke: nearly as large as smoking. 2004 doi: 10.1161/CIRCULATIONAHA.104.492215. submitted to Circulation. [DOI] [PubMed] [Google Scholar]
- Barone-Adesi F, Vizzini L, et al. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. European Heart Journal. 2006;27(20):2468. doi: 10.1093/eurheartj/ehl201. [DOI] [PubMed] [Google Scholar]
- Bartecchi C, Alsever RN, et al. Reduction in the Incidence of Acute Myocardial Infarction Associated With a Citywide Smoking Ordinance. Circulation. 2006;114(14):1490–1496. doi: 10.1161/CIRCULATIONAHA.106.615245. [DOI] [PubMed] [Google Scholar]
- Health Effects of Exposure to Environmental Tobacco Smoke. Final Report 1997 California Environmental Protection Agency. [Google Scholar]
- Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant 2005 California Environmental Protection Agency. [Google Scholar]
- Centers for Disease Control. Mortality From Coronary Heart Disease and Acute Myocardial Infarction -- United States, 1998. Morbidity and Mortality Weekly Report. 2001;50(6):90–93. [PubMed] [Google Scholar]
- Glantz SA, Parmley WW. Passive smoking and heart disease. Circulation. 1991;83(1):1–12. doi: 10.1161/01.cir.83.1.1. [DOI] [PubMed] [Google Scholar]
- Glantz SA, Parmley WW. Passive smoking and heart disease. Mechanisms and risk. JAMA. 1995;273(13):1047–1053. [PubMed] [Google Scholar]
- Khuder SA, Milz S, et al. The Impact of a Smoking Ban on Hospital Admissions for Coronary Heart Disease. Preventive Medicine. doi: 10.1016/j.ypmed.2007.03.011. In press. [DOI] [PubMed] [Google Scholar]
- Law M, Morris J, et al. Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. British Medical Journal. 1997;315(7114):973–980. doi: 10.1136/bmj.315.7114.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechacek TF, Babb S. How acute and reversible are the cardiovascular risks of secondhand smoke? Bmj. 2004;328(7446):980–3. doi: 10.1136/bmj.328.7446.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raupach T, Schafer K, et al. Secondhand smoke as an acute threat for the cardiovascular system: a change in paradigm. Eur Heart J. 2006;27(4):386–92. doi: 10.1093/eurheartj/ehi601. [DOI] [PubMed] [Google Scholar]
- Sargent RP, Shepard RM, et al. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. British Medical Journal. 2004;328(7446):977–980. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AE, Johnson CE, et al. Environmental tobacco smoke and cardiovascular disease. A position paper from the Council on Cardiopulmonary and Critical Care, American Heart Association. Circulation. 1992;86:699–702. doi: 10.1161/01.cir.86.2.699. [DOI] [PubMed] [Google Scholar]
- The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. 2006 U.S. Department of Health and Human Services. [PubMed] [Google Scholar]
- Whincup PH, Gilg JA, et al. Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement. Bmj. 2004;329(7459):200–5. doi: 10.1136/bmj.38146.427188.55. [DOI] [PMC free article] [PubMed] [Google Scholar]