SYNOPSIS
Objectives
Pediatric obesity is increasing at epidemic rates in industrialized nations. It is recommended that pediatricians screen all children annually with the use of body mass index (BMI). However, it is unclear whether this recommendation is followed. This study sought to (1) determine the proportion of children screened for obesity with BMI, and (2) test whether attending physicians are more likely than resident physicians to document and plot BMI.
Methods
We conducted a systematic review of medical records in an urban academic pediatric practice. Participants were children aged 5 to 11 years presenting for health care in 2004. We measured the proportion of subjects with documented and plotted BMI and compared results for attending and resident physicians. We used logistic regression analysis to determine factors associated with documentation of BMI.
Results
Of 397 medical records reviewed, 59.7% contained the 2000 Centers for Disease Control and Prevention growth curve with BMI for age; 5.5% documented BMI, and 4.3% plotted BMI. Resident physicians were more likely to document (13.0% vs. 3.0%, p=0.0008) and plot (9.0% vs. 2.7%, p=0.0260) BMI compared with attending physicians. Children with a BMI ≥95% for age were more likely to have their BMI documented (odds ratio [OR] = 10.7, 95% confidence interval [CI] 3.7, 31.5) and plotted (OR=7.1, 95% CI 2.3, 21.6).
Conclusion
We found the use of BMI to screen for childhood obesity very poor in this academic pediatric practice. Resident physicians were more likely to document and plot BMI than attending physicians.
Childhood obesity is increasing at epidemic rates in the United States and other industrialized nations.1–5 The most recent National Health and Nutrition Examination Survey (NHANES) data (2003–2006) revealed that 17.0% of children aged 6 to 11 years are obese and 33.3% are considered overweight.2 Furthermore, pediatric obesity is known to be associated with adverse health consequences such as type 2 diabetes mellitus, metabolic syndrome, hyperlipidemia, hypertension, depression, and obstructive sleep apnea.5,6 Identifying children at risk for obesity is a critical component of any prevention strategy.7 National guidelines recommend that physicians measure and document the body mass index (BMI) of all school-age children annually.4,8 It is known that provider identification of children as overweight is associated with higher rates of screening for comorbidities.9 Likewise, inadequate screening for pediatric obesity translates into missed opportunities for treatment of obesity and evaluation of weight-related health consequences.
Despite recommendations for routine screening, the percentage of children screened for obesity with BMI at routine health maintenance visits is not known. Previous studies have provided varying estimates of provider adherence to these recommendations. Surveys have estimated that approximately 10% to 50% of pediatric providers routinely screen for pediatric obesity with the use of BMI.10,11 Additionally, at least three retrospective reviews have evaluated the diagnosis and management of obesity.12–14 These studies showed that among children who are overweight or obese, the diagnosis is recognized 20% to 50% of the time, with the children in the obese category being recognized significantly more often than those in the overweight category.12–16 Only a few studies have reported the frequency of documentation and plotting of BMI in a primary care setting. However, this was not the primary aim of these studies.13,16
To our knowledge, no studies have tested whether resident and attending physicians differ in their use of BMI as a screening tool for gauging pediatric overweight. Furthermore, we believe it is important to learn about provider practices and potential differences in documentation and plotting of BMI. This information will help inform decisions about educational interventions, particularly regarding the adequacy of current residency training and the need for additional education of attending physicians regarding the use of BMI as a screening tool for pediatric obesity.
The main objectives of this study were to (1) determine the proportion of children screened for obesity with the use of BMI (documentation and plotting), and (2) determine whether level of physician training was associated with the documentation and plotting of BMI. We hypothesized that attending physicians were more likely to document and plot BMI than resident physicians, based on the idea that attending physicians are more experienced in diagnosing and treating childhood obesity, less rushed because of improved efficiency, and more systematic regarding basic screening procedures. A secondary objective was to identify patient characteristics (e.g., race, gender, and insurance status) that predict documentation and plotting of BMI. Additional outcomes of interest included provider patterns of diagnostic testing, follow-up, referral, and treatment recommendations.
METHODS
Overview
This study was a retrospective review of the medical records in a large academic internal medicine-pediatrics practice. This hospital-based setting is unique in that attending physicians work alongside resident physicians in a group practice, with a total of 42 providers—28 resident physicians and 14 attending physicians. The practice is located in an urban area in the midwestern United States and serves a racially and socioeconomically diverse population of children and adults.
We chose to focus our study on children aged 5 to 11 years, as this is the group with the most rapidly increasing rates of pediatric obesity based on the NHANES data.3 In addition, determination of overweight status for children in this age range can be visually challenging and deceptive.17,18 The Institutional Review Board of the University of Cincinnati approved this study.
Subjects
A computerized billing program identified 741 patient records for children aged 5 to 11 years seen in the office from January 1 through December 31, 2004. Due to staff limitations, we selected a convenience sample of 500 of the 741 subjects for review. One researcher started from the beginning of the alphabetized list of subjects, two researchers started from points in the middle, and a fourth researcher started from the end until we reached a total of 500 subjects. For each patient record, we defined the index visit as the most recent patient encounter with a height and weight recorded. We excluded patients who were seen only for ill visits during 2004 without a documented height from the analysis (n=103). This sampling strategy yielded a total of 397 subjects.
Clinic procedures
At the time of this study, a medical assistant measured the weight, height, and vital signs of patients in this practice, and then escorted the patients to an examination room. Plotting of height, weight, and BMI is the physician's responsibility. Growth charts remain part of the medical record for return patients, and are added to the chart for new patients.
Measures
Four researchers systematically collected data using a standardized chart abstraction tool. We collected demographic information such as age, gender, race, and insurance status. Then we recorded height (inches or centimeters) and weight (pounds or kilograms) as documented on the chart and later converted them to meters and kilograms to calculate BMI. We also recorded the reason for the index visit (routine health maintenance vs. ill visit).
An attending physician supervised all patients seen by a resident physician; a portion of the patients were seen only by an attending physician. We documented the provider's level of training as “resident” if a resident physician saw the patient and as attending if the patient was seen only by the attending physician. We did not record the individual provider's identity. Because we derived our sample from a query of all children seen during a calendar year, we accounted for provider vacations and other clinic absences and ensured representation of all providers in the practice. Two researchers reviewed 5% of the charts to validate the findings.
We defined documentation of BMI as the mention of BMI or writing of BMI on any part of the progress note from the visit. We noted the presence or absence of plotting of BMI for age for the index visit by reviewing the growth curve. The presence of the correct growth curve on the chart required the updated Centers for Disease Control and Prevention (CDC) 2000 growth curve that includes the BMI for age curve.
We noted all existing diagnoses or medical problems as documented by physicians in the “Problem List” of the medical record. We collected specific information regarding weight-management advice as documented in the progress note. In addition, we collected information on whether a referral was made, along with the type of referral. Lastly, we collected information on diagnostic testing and follow-up recommendations from documentation in the provider's progress note.
Analysis
We categorized BMI percentile using CDC recommendations of normal weight (<85% BMI for age and gender), overweight (≥85% and <95% BMI for age and gender), and obese (≥95% BMI for age and gender).7,19 We calculated BMI percentiles based on CDC age- and gender-specific standards,20 using publicly available programs.21 We assessed differences in documentation and plotting of BMI, referral, and diagnostic evaluation by provider level of training using Chi-square tests. Using multivariable logistic regression, we identified factors independently associated with the plotting and documentation of BMI. All analyses were performed using SAS© version 9.1.22
RESULTS
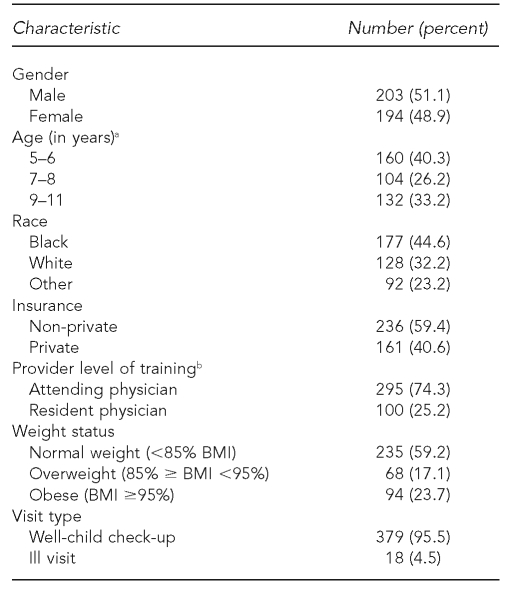
A description of the study population is outlined in Table 1. Of the 397 subjects, 51.1% were male, 44.6% were black, and 40.6% had private insurance, with the remaining either self-pay or Medicaid insured. The patients' mean age was 7.8 years. An attending physician saw approximately 74.3% of patients, with the remainder being seen by a resident physician. We recorded about 59.2% of the patients as normal weight (BMI for age <85%), 17.1% as overweight (85%≤ BMI <95%), and 23.7% as obese (BMI ≥95%).
Table 1.
Descriptive characteristics of a sample of patients in a large academic internal medicine-pediatrics practice in the Midwest (n=397)
aAge data were unknown for one record.
bProvider level of training was unknown for two records.
BMI = body mass index
Documentation and plotting of BMI
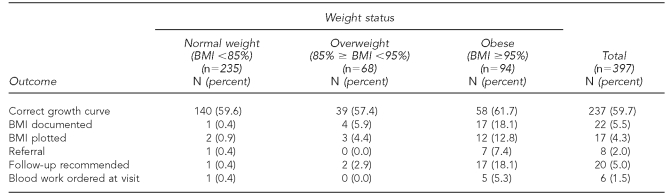
Only 59.7% of the medical records contained the recommended 2000 CDC growth curve. Only 5.5% (22/397) of patients had BMI documented, and 4.3% (17/397) of patients had BMI for age plotted on the growth curve (Table 2). Stratification by weight status revealed a greater likelihood of patients who were overweight or obese to have their BMI documented or plotted. Among the patients who were overweight, 5.9% (4/68) had their BMI documented, and 4.4% (3/68) had their BMI plotted. Among the patients who were obese, 18.1% (17/94) had their BMI documented, and 12.8% (12/94) had their BMI plotted. While a larger portion of the children in the overweight and obese categories had their BMI documented and plotted, a large number of overweight and obese children still were not screened for obesity.
Table 2.
A sample of patients in a large academic internal medicine-pediatrics practice in the Midwest with the outcome of interest by weight status
BMI = body mass index
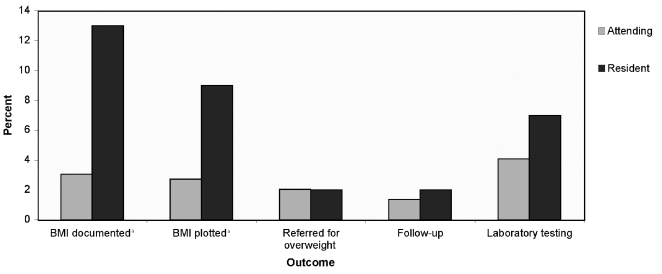
Provider's level of training
The Figure shows differences in outcomes by the provider's level of training. Attending physicians provided the care for a greater number of patients (295) than did resident physicians (100). We found no differences in the degree of obesity among patients seen by attending and resident physicians. Level of training was significantly associated with BMI documentation. Comparing documentation and plotting of BMI by provider's level of training using Chi-square analysis revealed a greater likelihood of resident physicians vs. attending physicians documenting (p<0.001) and plotting (p<0.050) BMI for age. While we found small differences in referral rates, follow-up recommendations, and diagnostic testing by level of training, these differences were not statistically significant.
Figure.
Proportion of charts with outcome of interest by provider level of training for a sample of patients in a large academic internal medicine-pediatrics practice in the Midwest
ap<0.05 for Chi-square analysis
BMI = body mass index
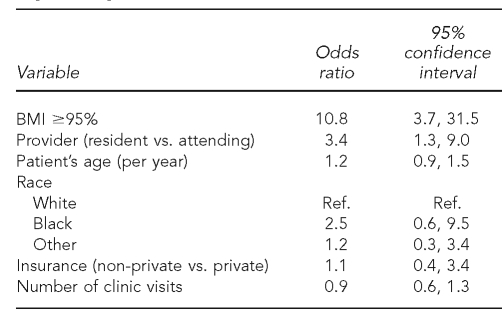
Multivariable logistic regression
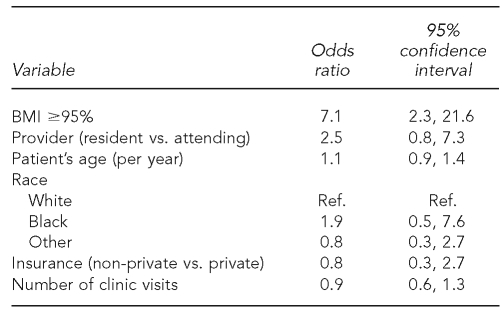
After controlling for age, race, type of insurance, and number of clinic visits, logistic regression analysis revealed the child's status as obese (BMI ≥95% for age) (odds ratio [OR] = 10.8) as the strongest predictor of provider documentation of BMI (Table 3). Provider level of training as a resident physician compared with an attending physician also predicted documentation of BMI (OR=3.4). For plotting of BMI for age, the child's status as obese was the only significant predictor (OR=7.1) (Table 4). Provider level of training was not a significant predictor of physician plotting of BMI for age.
Table 3.
Factors associated with documentation of BMI for a sample of patients in a large academic internal medicine-pediatrics practice in the Midwest: logistic regression model
BMI = body mass index
Ref. = reference group
Table 4.
Factors associated with plotting BMI for a sample of patients in a large academic internal medicine-pediatrics practice in the Midwest: logistic regression model
BMI = body mass index
Ref. = reference group
Treatment for obesity
Only a minority of children either overweight or obese had specific recommendations for referral, follow-up, or diagnostic evaluation. None of the patients who were overweight were referred for further management, and only 2.9% (2/68) received a recommendation for follow-up with their primary care provider regarding their weight. Only 7.4% (7/94) of patients who were obese were referred for management of their obesity, while 18.1% (17/94) of the obese children had recommended follow-up with their primary care provider. Among those who were obese, 5.3% (5/94) had blood work ordered at their visit.
DISCUSSION
Despite a relatively high prevalence of pediatric obesity (40.8% overweight or obese), providers in this academic pediatric practice did not routinely screen children with documentation and plotting of BMI for age. We found the child's status as being obese (BMI ≥95% for age) to be the strongest predictor of documentation and plotting of BMI for age, but significant numbers of these obese children did not have their BMI documented or plotted. Increased level of training did not impact provider documentation or plotting of BMI. In fact, resident physicians were more likely than attending physicians to document and plot BMI. In addition, among overweight children, less than 3.0% were referred, had recommended follow-up, or had additional diagnostic evaluation. Among those obese children, less than 10.0% received a referral, less than 20.0% had recommended follow-up, and only 5.0% had additional diagnostic evaluation.
The prevalence of pediatric obesity in this population is similar to that of other studies. Our rates of documentation and plotting of BMI are higher but still comparable to those found by Dorsey et al., who noted documentation of BMI in 0.5% of reviewed medical records.13 However, their study did not focus primarily on determining rates of BMI documentation. Compared with studies that have used surveys of pediatric providers to estimate rates of documentation and plotting of BMI, our findings were significantly lower.10,11 This is not surprising because surveys may tend to overestimate the degree of adherence to recommended screening practices, particularly if the provider is aware of the recommendations. In addition, providers who participate in surveys may not be representative of the general population of pediatric providers. Alternatively, the retrospective review relies heavily on the provider's written documentation, and it may not completely reflect the encounter with the patient.
Our finding that resident physicians were more likely to document and plot BMI than attending physicians has not been previously reported. An earlier study found an association between increased years of training among resident physicians and improved diagnosis of pediatric obesity.14 Another study comparing rates of diagnosis of pediatric obesity among general pediatricians, pediatric endocrinologists, and pediatric gastroenterologists found general pediatricians to be the most likely to diagnose pediatric overweight and pediatric gastroenterologists as the least likely to make the same diagnosis.12 Our findings may be explained by the fact that attending physicians may have completed their training prior to the recommendations for widespread use of BMI among pediatricians.
Another unique aspect of the current study is that we conducted it in a combined internal medicine and pediatrics practice. To our knowledge, no other study has evaluated a similar group. Many would argue that internal medicine and pediatric trained physicians would be highly sensitive to the topic of obesity, due to knowledge of and exposure to the long-term consequences of obesity in adults. Because of this unique perspective, one might hypothesize that these physicians would demonstrate higher rates of screening for pediatric obesity compared with pediatric trained physicians. Although we found slightly higher rates of screening with BMI than Dorsey et al.13 (0.5% vs. our study's rate of 5.5%), both rates were so low that it is not accurate to imply that type of training makes a considerable impact on screening rates for childhood obesity.
Previous retrospective reviews have evaluated physician documentation and diagnosis of overweight.9,12–16 These studies generally showed low rates of diagnosis of pediatric overweight among pediatric providers (less than 50.0%). Our study suggests that this may be related to a failure to use BMI to assess overweight status. A recent study by Barlow et al.16 assessed the frequency of overweight and obesity identification and its association with use of the BMI curve. They found that pediatricians identified overweight or obesity in 27.0% of children with a BMI in the overweight category, and 86.0% of children in the obese category. Furthermore, they found an association between BMI plotting and higher rates of recognition of overweight or obesity among the children in the overweight category (≥85% and <95% BMI for age and gender). This increased recognition with the use of the BMI curve was not seen in those children in the obese category (BMI for age ≥95% for age and gender).16
To further highlight the importance of the use of BMI, particularly in younger children, Robbins et al. demonstrated that BMI percentile was the strongest predictor of incident obesity in a cohort of children aged 3 to 7 years. In addition, the authors reported a 50.0% increase in odds of becoming overweight for each 10-unit increase in BMI percentile.23 Additional factors may explain the low rates of diagnosis of pediatric overweight, but it seems plausible that improved screening with BMI at routine visits and increased knowledge regarding interpretation of BMI may lead to greater rates of diagnosis.
We were unable to evaluate why pediatric providers do not use BMI. A recent study by Flower et al. explored barriers and facilitators to using BMI in primary care settings using focus groups.24 They reported lack of familiarity and agreement with BMI screening recommendations, skepticism about treatment effectiveness, and practice-level issues (e.g., lack of access to BMI charts and accurate height and weight data) as barriers to the use of BMI.24 It has been suggested that electronic medical records may aid in the calculation, documentation, and plotting of BMI and, ultimately, in pediatric obesity screening. However, pediatric providers will still be required to accurately interpret and monitor BMI at routine health maintenance visits.
Limitations
This study had some limitations. The retrospective nature of our study was a primary limitation. Our study's cross-sectional nature allowed us to evaluate provider practices at one point in time. Therefore, it is unclear how these practices may have changed over time. In addition, we relied on written physician documentation at the time of the visit. This could have resulted in an underestimation of physician use of BMI and treatment of pediatric overweight. Because we reviewed only a sample of the 741 patients meeting the study criteria, our results could misrepresent the use of BMI in this practice. However, documentation rates were so low that it is unlikely that reviewing the remaining medical records would have significantly affected our results. Lastly, the unique nature of a combined resident-attending practice may limit the generalizability of our findings. However, it allowed us to compare rates of documentation and plotting of BMI by provider level of training. In addition, generalizability was limited by the fact that we evaluated only one practice.
CONCLUSION
The findings of our study are particularly important in emphasizing a lack of screening with the use of BMI for pediatric obesity among children aged 5 to 11 years. We have shown that those children who visually appear to be obese are more likely to have their BMI documented and plotted. While this may be helpful, the most valuable use of plotting BMI is to detect those children that are crossing percentiles on the BMI for age growth curve, or those in the overweight category.
Visual screening is an imprecise and inadequate tool to identify overweight children. Routine screening of all children is required to identify overweight and obese children. Although attending physicians in this study could have trained and educated pediatricians, they were less likely than trainees to document and plot BMI. Widespread training of practicing pediatricians regarding the use of BMI as a screening tool for pediatric obesity is needed. While the resident physicians in the study showed higher rates of screening for obesity with BMI, their overall use of BMI was low. It is likely that with improved training of attending physicians, there will be increased use of BMI by trainees and, ultimately, by all physicians. Improved screening for obesity will result in earlier and improved identification of children with obesity. As Barlow et al. have shown, the use of BMI is particularly helpful in identifying those in the overweight category.16 This group of children may benefit from intervention if we can prevent the progression from overweight to obese status.
REFERENCES
- 1.Speiser PW, Rudolf MC, Anhalt H, Camacho-Hubner C, Chiarelli F, Eliakim A, et al. Obesity Consensus Working Group. Childhood obesity. J Clin Endocrinol Metab. 2005;90:1871–87. doi: 10.1210/jc.2004-1389. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–44. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 5.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 6.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518–25. [PubMed] [Google Scholar]
- 7.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics. 1998;102:E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 8.Krebs NF, Jacobson MS American Academy of Pediatrics Committee on Nutrition. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 9.Dilley KJ, Martin LA, Sullivan C, Seshadri R, Binns HJ Pediatric Practice Research Group. Identification of overweight status is associated with higher rates of screening for comorbidities of overweight in pediatric primary care. Pediatrics. 2007;119:e148–55. doi: 10.1542/peds.2005-2867. [DOI] [PubMed] [Google Scholar]
- 10.Perrin EM, Flower KB, Ammerman AS. Body mass index charts: useful yet underused. J Pediatr. 2004;144:455–60. doi: 10.1016/j.jpeds.2004.01.047. [DOI] [PubMed] [Google Scholar]
- 11.Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dieticians. Pediatrics. 2002;110(1 Pt 2):222–8. [PubMed] [Google Scholar]
- 12.Riley MR, Bass MN, Rosenthal P, Merriman RB. Underdiagnosis of pediatric obesity and underscreening for fatty liver disease and metabolic syndrome by pediatricians and pediatric subspecialists. J Pediatr. 2005;147:839–42. doi: 10.1016/j.jpeds.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Dorsey KB, Wells C, Krumholz HM, Concato J. Diagnosis, evaluation, and treatment of childhood obesity in pediatric practice. Arch Pediatr Adolesc Med. 2005;159:632–8. doi: 10.1001/archpedi.159.7.632. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton JL, James FW, Bazargan M. Provider practice, overweight and associated risk variables among children from a multi-ethnic underserved community. J Natl Med Assoc. 2003;95:441–8. [PMC free article] [PubMed] [Google Scholar]
- 15.O'Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:e154–9. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 16.Barlow SE, Bobra SR, Elliot MB, Brownson RC, Haire-Joshu D. Recognition of childhood overweight during health supervision visits: does BMI help pediatricians? Obesity (Silver Spring) 2007;15:225–32. doi: 10.1038/oby.2007.535. [DOI] [PubMed] [Google Scholar]
- 17.Caccamese SM, Kolodner K, Wright SM. Comparing patient and physician perception of weight status with body mass index. Am J Med. 2002;112:662–6. doi: 10.1016/s0002-9343(02)01104-x. [DOI] [PubMed] [Google Scholar]
- 18.Eck LH, Ray JW, Klesges RC, Relyea GE, Hackett-Renner C. Physicians' diagnosis of obesity status in NHANES II. Int J Obes Relat Metab Disord. 1994;18:704–8. [PubMed] [Google Scholar]
- 19.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 20.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (US) Growth chart training: a SAS program for the CDC growth charts [cited 2009 Feb 27] Available from: URL: http://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/sas.htm.
- 22.SAS Institute Inc. SAS®: Version 9.1. Cary (NC): SAS Institute Inc; 2005. [Google Scholar]
- 23.Robbins JM, Kahn KS, Lisi LM, Robbins SW, Michel SH, Torcato BR. Overweight among young children in the Philadelphia health care centers: incidence and prevalence. Arch Pediatr Adolesc Med. 2007;161:17–20. doi: 10.1001/archpedi.161.1.17. [DOI] [PubMed] [Google Scholar]
- 24.Flower KB, Perrin EM, Viadro CI, Ammerman AS. Using body mass index to identify overweight children: barriers and facilitators in primary care. Ambul Pediatr. 2007;7:38–44. doi: 10.1016/j.ambp.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]