Abstract
Objectives
To describe self-reported advance care planning, health care preferences, use of advance directives, and health perceptions in a very elderly community-dwelling sample.
Methods
Surviving participants of the original cohort of the Framingham Heart Study who were cognitively intact and attended a routine research exam between February 2004 and October 2005. Participants were queried about discussions about end of life care, preferences for care, documentation of advance directives, and health perceptions.
Results
Among 220 community-dwelling respondents, 67% were women with a mean age of 88 years (range 84-100). Overall 69% discussed their wishes for medical care at the end of life with someone, but only 17% discussed their wishes with a physician or health care provider. Two-thirds had a health care proxy, 55% had a living will, and 41% had both. Most (80%) respondents preferred comfort care over life-extending care, and 71% preferred to die at home; however, substantially fewer respondents said they would rather die than receive specific life-prolonging interventions [chronic ventilator (63%) or feeding tube (64%)]. Many were willing to endure distressing health states, with less than half indicating that they would rather die than live out their life in a great deal of pain (46%) or be confused/forgetful (45%) all of the time.
Conclusions
Although the vast majority of very elderly community-dwellers in this sample appear to prefer comfort measures at the end of life, many said they were willing to endure specific life-prolonging interventions and distressing health states to avoid death. Our results highlight the need for physicians better understand patients’ preferences and goals of care to help them make informed decisions at the end of life.
Keywords: advance directives, geriatrics, end of life care, patient centered care, decision-making
INTRODUCTION
Advance care planning is one key element to achieving patient autonomy by allowing patients’ to participate in decisions about their medical care (1, 2). However, many patients near the end of life lose decision-making capacity or become too ill to participate in such decisions (1). When this happens, patients’ loved ones and physicians must make these difficult decisions, even though they may be unaware of or disagree with patient’s preferences for care (3, 4). Advance care planning is based on the premise that ongoing discussions about end of life issues accompanied by written advance directives are valuable to help loved ones, physicians, and other providers better understand and make treatment decisions consistent with patients’ wishes, if the patient becomes incapacitated (5-7). Experts recommend that advance care planning discussions be held before patients face an acute health crisis and that the process continue as patients age or their clinical situation changes (3, 7). However, little is known about the extent to which advance care planning is happening among very elderly community-dwellers (8-11).
We surveyed surviving community-dwelling participants of the original cohort of the Framingham Heart Study, all of whom are over age 80, about advance care planning, use of advance directives, and preferences for health care. The Framingham Heart Study is a natural place to further our understanding of very elderly adults who have been followed closely for almost 60 years, and who are now approaching the end of their natural lifespan. The original cohort participants have been followed extensively across adulthood to collect detailed medical and social information, with very little loss to follow-up. In this context, we examined the extent to which these very elderly community-dwelling adults report advance care planning; describe their preferences for care and reported use of advance directives; and examined how these factors relate to social support, illness burden, physical functioning, cognitive functioning, depressive symptoms, health perceptions, and previous health care use.
METHODS
Data Collection
The Framingham Heart Study (FHS) is a prospective observational cohort study that began in 1948 to investigate risk factors for cardiovascular disease and other health conditions. The original cohort consisted of 5,209 participants (55% women) aged 30 to 62 at entry from Framingham, Massachusetts (12). Since study inception, participants have returned every two years for a routine research examination, which include a physician-administered medical history, a medical assessment, and questionnaires administered by trained interviewers. Written informed consent was obtained from participants and the Institutional Review Board at Boston Medical Center approved the examination content.
Study Sample
Surviving original cohort participants who attended their 28th biennial examination were eligible for this study if they were cognitively intact and community-dwelling. All examinations occurred between February 4, 2004 and October 26, 2005. Overall 253 community-dwelling participants attended exam 28. however 17 participants fulfilled criteria for significant cognitive impairment or dementia after review by the FHS Dementia Study investigators (13); and therefore were ineligible to answer questions related to advance care planning and health care preferences. Of the 236 eligible participants, 220 (93%) agreed to answer these questions. Overall, 60% of examinations for eligible participants occurred in the FHS clinic. The remainder occurred at offsite locations (e.g., private residences) often because of distance.
Advance Care Planning and Care Preferences
Twelve items were administered to assess advance care planning and preferences for care; 11 of which were administered in the SUPPORT/HELP Project and utilized in several published reports (14-16). Participants were asked whether they have talked to anyone about their wishes for medical care toward the end of life; had filled out a living will, and; completed a health care proxy. Those reporting a health care proxy were asked to identify that individual. Participants were asked whether they prefer a treatment plan focused on extending life as much as possible, even if it meant more pain and discomfort, or one focused on relieving pain and discomfort as much as possible, even if it means not living as long. Participants reported their willingness to endure certain health states including whether they would rather die. The hypothetical health states included being 1) in a great deal of pain all the time even with medications; 2) attached to a ventilator or respirator all the time; 3) fed through a tube all the time; 4) unconscious or in a coma all the time, and; 5) confused or forgetting all the time. Lastly, participants were asked where they would prefer to die.
Participants were queried about their perceptions of their own longevity and future physical functioning, factors that may influence advance care planning and care preferences. Specifically, they were asked “What do you think the chances are that you would live 12 months or more?” and “What are the chances that you will be able to take care of yourself 12 months from now?”.
Due to concerns about participant burden and the potential emotional content of the questions, the interviewer assessed participants’ willingness to respond to the questions and external behavior immediately following these questions. Interviewers documented whether the participant 1) stopped the interview; 2) was visibly upset or bothered by any question(s), and; 3) had difficulty understanding any question(s).
Potential Correlates
Factors previously shown to correlate with advance care planning and preferences for care in seriously ill populations are collected routinely during biennial examinations. Sociodemographic characteristics included age, sex, place of residence, and education (obtained from baseline interview). Social support was assessed by marital status, living situation, and two Berkman (17) Social Network questionnaire items, which assessed whether participants had someone to listen to them and provide emotional support.
Perceived health was assessed by “In general, how is your health now?”. Self-reported physical functioning was assessed by ability to perform activities of daily living (ADL) (eating, dressing, bathing, transferring, toileting, and walking about 50 yards) without human assistance (18) and ability to walk a half mile without help (19). Cognitive functioning was assessed using the Mini-mental State Exam (MMSE) [scores ≥24 indicate no cognitive impairment] (20). Presence of depressive symptoms was assessed using the Center for Epidemiologic Studies Depression Scale (CES-D) [ scores ≥ 16 indicate significant depressive symptoms] (21). Use of health care services included hospitalizations, illness visit to doctor, check up by doctor, and nursing home or skilled nursing facility admission in previous 2 years. Comorbid illness was assessed by a documented history of diabetes, coronary heart disease, stroke, congestive heart failure, intermittent claudication, cancer, and hip fracture. These conditions were documented by chart review and validated by a panel of FHS investigators. Diabetes was defined by a causal blood sugar > 200 mg/dL or self-reported use of oral hypoglycemic medications or insulin.
Statistical Analysis
All statistical analyses used SAS version 9.1 (SAS Institute, Cary, NC). We conducted bivariable analyses to describe the sample and identify differences in advance care planning and health care preferences between men and women, and to identify factors associated with self-reported use of advance directives (having a health care proxy and living will). We used multivariable logistic regression to identify factors independently associated with advanced directives after adjusting for age and sex. Because advanced directives were relatively common (>10%), we derived adjusted prevalence ratios (aPR) and 95% confidence intervals using a log binomial regression model (22).
RESULTS
Among the 220 community-dwelling respondents, 3 (1.3%) stopped before completing questions on advance care planning and preferences, and 12 (5.5%) appeared upset or bothered by one or more questions. The average age of respondents was 88 years, 67% were women, 64% were widowed, three-quarters achieved a high school education or higher, and nearly all reported a routine check-up within the past 2 years. Compared with men, women were less often married and more often living alone (Table 1). Men were more likely to have one or more comorbid conditions and to have been hospitalized than women.
Table 1.
Characteristics of Community-Dwelling Participants of the Framingham Heart Study by Sex (n=220)
| Women (n=147) n (%) |
Men (n=73) n (%) |
p-value | |
|---|---|---|---|
| Demographic Characteristics | |||
| Age at interview, mean ± SD | 88.3 ± 3.4 | 87.8 ± 3.1 | .277 |
| Education | |||
| Less than high school graduate | 32 (22) | 19 (26) | |
| High school graduate | 64 (44) | 29 (40) | |
| More than high school | 48 (33) | 26 (34) | .789 |
| Place of residence | |||
| Private residence | 111 (76) | 58 (79) | |
| Other (e.g. assisted living) | 36 (24) | 15 (21) | .514 |
| Social Support | |||
| Marital status | |||
| Married | 21 (14) | 41 (58) | |
| Widow | 111 (76) | 29 (41) | |
| Other | 15 (10) | 1 (1) | <.001 |
| Living situation | |||
| Lives alone | 87 (60) | 22 (31) | |
| Lives with someone | 59 (40) | 50 (69) | <.001 |
| Has someone to listen | |||
| None of the time | 7 (5) | 1 (2) | |
| Some of the time | 43 (30) | 22 (32) | |
| All of the time | 91 (65) | 45 (66) | .536 |
| Has someone to provide emotional support and help make difficult decisions |
|||
| None of the time | 6 (4) | 3 (4) | |
| Some of the time | 20 (14) | 15 (22) | |
| All of the time | 114 (81) | 52 (74) | .353 |
| Clinical Characteristics | |||
| History of | |||
| Cancer | 39 (27) | 26 (36) | .164 |
| Coronary heart disease | 38 (26) | 29 (40) | .035 |
| Stroke | 10 (7) | 17 (23) | <.001 |
| Intermittent claudication | 12 (9) | 12 (16) | .095 |
| Congestive heart failure | 14 (10) | 9 (12) | .522 |
| Diabetes | 18 (12) | 11 (15) | .560 |
| Hip fracture | 17 (12) | 2 (3) | .039 |
| Number of comorbid illnesses | |||
| None | 56 (38) | 13 (18) | |
| 1 | 48 (33) | 26 (36) | |
| 2 | 29 (20) | 23 (31) | |
| 3 or more | 14 (9) | 11 (15) | .002 |
| Perceived health | |||
| Excellent | 25 (17) | 12 (17) | |
| Good | 95 (66) | 45 (62) | |
| Fair/poor | 24 (17) | 15 (21) | .571 |
| Perceived chance of taking care of self in 12 months |
|||
| 90% or better | 81 (55) | 39 (54) | |
| about 75% | 19 (13) | 19 (26) | |
| 50% or worse | 37 (26) | 12 (17) | |
| Unsure | 9 (6) | 2 (3) | .053 |
| Perceived chance of living 12 months or longer |
|||
| 90% or better | 85 (55) | 43 (60) | |
| about 75% | 11 (7) | 11 (15) | |
| 50% or worse | 39( 27) | 13 (18) | |
| Unsure | 12 (8) | 5 (7) | .211 |
| CES-D* Score ≥ 16, indicating significant depressive symptoms |
|||
| No | 119 (82) | 64 (89) | |
| Yes | 27 (18) | 8 (11) | .176 |
| Cognitive status, MMSE Score†† | |||
| < 24 | 132 (90) | 66 (90) | |
| ≥ 24 | 15 (10) | 7 (10) | .886 |
| ADL† dependencies | |||
| None | 128 (87) | 65 (89) | |
| 1 or more | 19 (13) | 8 (11) | ..676 |
| Uses assistive device to perform ADL† |
|||
| No | 49 (33) | 32 (44) | |
| Yes | 98 (67) | 41 (56) | .120 |
| Ability to walk a half mile without help |
57 (39) | 20 (28) | |
| Able | 63 (44) | 43 (60) | |
| Unable | 25 (17) | 9 (12) | .078 |
| Doesn’t do | |||
| Health care use since last exam | |||
| Had check up by doctor | 141 (97) | 70 (96) | 1.00 |
| Illness visit to doctor | |||
| No visit | 96 (65) | 39 (53) | |
| 1 | 29 (20) | 24 (33) | |
| 2 or more | 22 (15) | 10 (14) | .314 |
| Hospitalization | |||
| None | 97 (66) | 35 (48) | |
| 1 | 28 (19) | 24 (33) | |
| 2 or more | 22 (15) | 14 (19) | .041 |
| Had nursing home stay | 18 (12) | 9 (12) | .986 |
CES-D = Center for Epidemiologic Studies Depression Scale.
MMSE = Mini-Mental Status Exam
ADL = Activities of daily living.
Number of observations with missing data — education (n=3); marital status (n=2); living alone (n=2); having someone to listen to you (n=11); having someone to provide emotional support and help make difficult decisions (n=10); perceived ability to take care of self (n=2); perception of living 12 months or longer (n=1); CES-D (n=2); ADLs (n=1); ability to walk a half mile without help (n=3); Interim check up by doctor (n=1).
We observed no difference in advance care planning and health care preferences between men and women (Table 2). Overall, 69% of respondents reported discussing their wishes for medical care at the end of life with someone, but only 17% of these respondents discussed their wishes with a physician or other health care provider. Among those who discussed their wishes for care, the vast majority talked with a family member. Almost two-thirds reported having a health care proxy, 55% a living will, 70% had either, and 41% had both. Although 80% preferred comfort over life-extending care, a greater proportion of men reported that they prefer life-extending care. Most respondents preferred to die at home.
Table 2.
Advance Care Planning and Health Care Preferences among Community-Dwelling Elders (n=220)
| All Participants† n (%) |
Women (n=147) n (%) |
Men (n=73) n (%) |
|
|---|---|---|---|
| Discussed wishes for end of life care | |||
| No | 69 (31) | 42 (29) | 27 (37) |
| Yes | 151 (69) | 105 (71) | 46 (63) |
| Among those who have discussed wishes, percent who discussed with |
[n=151] | [n=105] | [n=46] |
| Family member | 138 (91) | 96 (91) | 42 (91) |
| Physician/health care provider | 25 (17) | 17 (16) | 8 (17) |
| Attorney | 25 (17) | 15 (14) | 10 (21) |
| Friend | 17 (11) | 15 (14) | 2 (4) |
| Clergy | 5 (3) | 3 (3) | 2 (4) |
| Other | 5 (3) | 5 (5) | 0 (0) |
| Completed advance directives (has health care proxy and living will) |
91 (41) | 60 (41) | 31 (43) |
| Has heath care proxy | 136 (66) | 92 (67) | 44 (62) |
| Has Living Will | 116 (55) | 75 (54) | 41 (57) |
| Preferences for Goals of Care | |||
| Extend life as much as possible | 18 (8) | 8 (5) | 10 (14) |
| Focused on comfort/pain relief | 174 (80) | 122 (84) | 52 (72) |
| Unsure | 26 (12) | 16 (11) | 10 (14) |
| Preference for Place of Death | |||
| Home | 139 (71) | 93 (69) | 46 (75) |
| Hospital | 23 (12) | 16 (12) | 7 (12) |
| Hospice | 14 (7) | 12 (9) | 2 (3) |
| Nursing home | 2 (1) | 2 (2) | 0 (0) |
| Other | 17 (9) | 11 (8) | 6 (10) |
There were no statistically significant differences by sex. Number of observations with missing data — health care proxy (n=12); living will (n=8); preference for goals of care (n=2); preference for place of death (n=25).
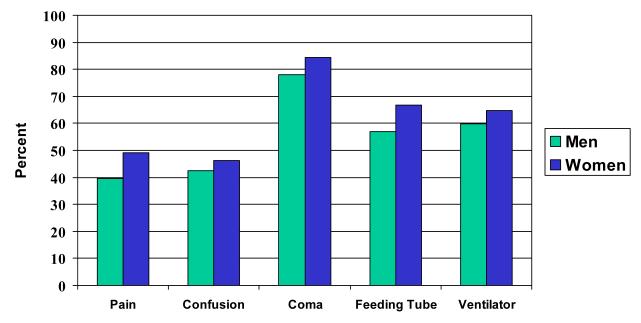
For each health state, a greater proportion of women than men reported that they would rather die than live out their life in a particular state (Figure 1). Although 4 out of 5 respondents preferred comfort care, fewer respondents preferred death over living out their life attached to a ventilator (63%), or fed through a tube (64%) all the time. Respondents were more willing to endure symptoms of pain and confusion, with less than half indicating that they would rather die than live out their life in a great deal of pain (46%) or be forgetful or confused (45%) all of the time. In contrast, being unconscious or in a coma all the time was undesirable to most respondents, with 82% indicating that they would rather die.
Figure 1.
Preferences for Future Health States among Community-Dwelling Elders (n = 220) Respondent would rather die than spend all of the time in:
Table 3 presents the proportion of respondents reporting advance directives across different factors. Having advanced directives was associated with higher education, living in a non-private residence, having someone to listen, and not having depressive symptoms. After adjusting for age and sex, only education and goals of care remained associated with having advance directives. Compared to participants with less than a high school education, those with a high school education (aPR=1.63, 95% CI [0.94, 2.81]) and more than a high school education [aPR=2.40, 95% CI (1.41, 4.07)] were more likely to have advance directives, although the former did not achieve statistical significance. Compared to participants who preferred comfort care, those preferring life-extending care were substantially less likely to have advance directives [aPR=0.32, (0.11, 0.90)], whereas participants who were unsure about their preference were indistinguishable [aPR=0.72, (0.40, 1.27)].
Table 3.
Proportion of Community-Dwelling Elders with Advance Directives Across Selected Characteristics (n=220)
| Number with Characteristic (n) |
% with Advance Directives* |
|
|---|---|---|
| Demographic Characteristics | ||
| Sex | ||
| Female | 147 | 40.8 |
| Male | 73 | 42.5 |
| Education† | ||
| Less than high school graduate | 51 | 23.5 |
| High school graduate | 93 | 40.9 |
| More than high school | 73 | 54.8 |
| Place of residence† | ||
| Private residence | 169 | 37.9 |
| Other (e.g. assisted living) | 51 | 52.9 |
| Social Support | ||
| Marital status | ||
| Married | 62 | 46.8 |
| Widow | 140 | 41.4 |
| Other | 16 | 25.0 |
| Lives situation | ||
| Lives alone | 109 | 45.0 |
| Lives with someone | 109 | 36.7 |
| Has someone to listen† | ||
| None of the time | 8 | 12.5 |
| Some of the time | 65 | 32.3 |
| All of the time | 136 | 49.3 |
| Has someone to provide emotional support and help make difficult decisions |
||
| None of the time | 9 | 22.2 |
| Some of the time | 35 | 34.3 |
| All of the time | 166 | 45.2 |
| Clinical Characteristics | ||
| Number of comorbid illnesses | ||
| None | 69 | 44.9 |
| 1 | 74 | 39.2 |
| 2 | 52 | 42.3 |
| 3 or more | 25 | 36.0 |
| Perceived health status | ||
| Excellent | 37 | 43.2 |
| Good | 140 | 41.4 |
| Fair/poor | 39 | 41.0 |
| Perceived chance of living 12 months or longer | ||
| 90% or better | 128 | 45.3 |
| about 75% | 22 | 31.8 |
| 50% or worse | 52 | 36.5 |
| Unsure | 17 | 41.2 |
| Perceived chance of taking care of self in 12 months |
||
| 90% or better | 120 | 48.3 |
| about 75% | 38 | 36.8 |
| 50% or worse | 49 | 28.6 |
| Unsure | 11 | 36.4 |
| CES-D+ Score ≥ 16, indicating significant depressive symptoms† |
||
| No | 183 | 44.8 |
| Yes | 35 | 25.7 |
| Cognitive status, MMSE Score†† | ||
| < 24 | 198 | 42.4 |
| ≥ 24 | 22 | 31.8 |
| ADL§ dependencies | ||
| None | 193 | 43.0 |
| 1 or more | 27 | 29.6 |
| Uses assistive device to perform ADL§ | ||
| No | 81 | 45.7 |
| Yes | 139 | 38.9 |
| Ability to walk a half mile without help | ||
| Able | 106 | 49.0 |
| Unable | 77 | 33.8 |
| Doesn’t do | 34 | 32.3 |
| Health care use since last exam | ||
| Check up by doctor | ||
| No | 8 | 37.5 |
| Yes | 211 | 41.7 |
| Illness visit to doctor | ||
| No visit | 135 | 37.8 |
| 1 | 53 | 52.8 |
| 2 or more | 12 | 37.5 |
| Hospitalization | ||
| None | 132 | 42.4 |
| 1 | 52 | 36.5 |
| 2 or more | 36 | 44.4 |
| Nursing home stay | ||
| No | 193 | 43.5 |
| Yes | 27 | 25.9 |
Percentages refer to proportion of participants with a particular characteristic who had an advance directive.
p-value <0.05.
CES-D = Center for Epidemiologic Studies Depression Scale.
MMSE = Mini-Mental Status Exam
ADL = Activities of daily living.
Number of observations with missing data — education (n=3); marital status (n=2); perceived health (n=4); living alone (n=2); having someone to listen to you (n=11); having someone to provide emotional support and help make difficult decisions (n=10); perceived health status (n=4); perceived ability to take care of self (n=13); perception of living 12 months or longer (n=18); CES-D (n=2); ADLs (n=1); Interim check up by doctor (n=1).
DISCUSSION
We studied advance care planning and health care preferences of community-dwelling participants of the Framingham Heart Study original cohort. These men and women, now aged 84 to 100 years, have been followed for over 60 years, and have made substantial contributions to our understanding of many disease processes, most notably cardiovascular disease (23). With the current study, this cohort provides important insight into our understanding of advance care planning and health care preferences of very elderly community-dwellers who are still cognitively intact and thus able to participate in discussions regarding their goals for care. The majority of respondents reported that they preferred comfort measures at the end of life and to die at home. However, in spite of the cohort’s advanced age and overwhelming preference for comfort measures, when presented with specific clinical scenarios many respondents said they were willing to endure specific life-prolonging interventions (chronic ventilator and feeding tube) to avoid death. Moreover, more than half of respondents said they were willing to live out their life in a great deal of pain or being forgetful or confused rather than die.
There are several possible clinically relevant explanations for this finding. First, the framing of the questions about goals of care and hypothetical health states is very important. Patients likely do not fully understand what comfort care entails or the implications of specific life-prolonging interventions, and may not view these concepts as mutually exclusive. Moreover, patients’ lack of knowledge and experience with specific medical interventions and hypothetical scenarios has been shown to cloud the relationship between goals of care and preferences for life-prolonging interventions (24). A recent study found that using video images to depict a patient living with advanced dementia had a significant impact on subjects’ preferences for care by improving their understanding and ability to imagine themselves having advanced dementia (25). Prior to seeing the video, 50% of subjects preferred comfort care and 21% preferred life-prolonging care. However, after seeing the video almost 90% indicated they desired comfort care and none chose life-prolonging care. In our study, most respondents chose death over living the rest of their life in a coma or unconscious, possibly because this is a tangible state that is more readily understood. Finally, qualitative data suggest that when faced with hypothetical choices, patients place more emphasis on the outcome of an intervention (in this instance avoiding death) rather than the intervention itself (26). Nevertheless, given the inconsistency observed between reported goals of care and preferences for life-prolonging interventions and distressing health states, it is concerning that few of these very elderly respondents have discussed their wishes for end of life care with a health care provider.
More than 15 years ago, Lo and colleagues recommended that physicians talk to their elderly patients about their wishes for care (27). Most physicians believe that it is their professional responsibility to help patients with advance care planning, with over 80% of physicians reporting that they should initiate end-of-life discussions with patients (28). Therefore, it is troubling that in this very elderly cohort where nearly all respondents reported having a recent routine check-up, only 12% of all respondents reported discussing their preferences with a physician or health care provider. Yet these findings are consistent with studies suggesting that discussions with physicians about end of life care were uncommon (10, 11, 29). We did find it encouraging that the vast majority of respondents had someone to provide emotional support, help make difficult decisions, and listen to them, and many reported that they had discussed their wishes for care with family members. Nonetheless, our findings highlight the need for physicians to have these discussions with very elderly patients in order to help their patients make informed decisions rooted in their values.
Our findings were remarkably consistent with those of seriously ill hospitalized patients aged 80 and older enrolled in the Hospitalized Elderly Longitudinal Project (HELP) (15). Using the same set of questions asked in our study, HELP found that 73-78% of very elderly adults preferred comfort care within 3 to 6 months prior to death. HELP also found that fewer patients would choose death rather than endure a lifetime of pain (48%) and confusion (35%) or be attached to a ventilator (70%) or feeding tube (50%) (15).
Few studies have actually examined advance care planning among community-dwelling elders (8-11). We found that two-thirds of very elderly community-dwellers reported having a health care proxy and about half had a living will. In contrast, a study of managed care patients age 80 and older found that only 27% had been asked about their end of life preferences and that only 46% had advance directives documented in their chart (10). In a multi-ethnic sample of younger community-dwelling elders, Morrison and Meier found that only 35% had a health care proxy (8).
There is some evidence that discussions about end of life care are helpful to patients. Patients who discussed end of life care with their physicians reported less fear and anxiety, a better understanding of their options for care, and a greater ability to make decisions and influence their medical care (30, 31). Data suggest that completion of advance directives were associated with greater satisfaction (30, 32), greater hospice use, and fewer concerns about communication (33). Despite national trends toward shared-decision making, one-third of the general adult population moderately or strongly agreed that they would prefer to leave decision-making to their physician, with older adults and those in poorer health less likely to want to participate in decision-making (34, 35). Moreover, few desire tight control over medical decisions if unable to make their own decisions (36), and many community-dwelling elders trust that physicians would make the right care decisions should they become very sick (8).
Because many very elderly patients are clinically complex, advance care planning should not wait until patients face an acute medical crisis such as being hospitalized with life-threatening illness (4, 7). Studies show that patients are open and willing to discuss advance care planning, but generally they would prefer that their physician raise the topic (8, 37). Even though most physicians believe it is their responsibility to have end of life discussions (28), some may be reluctant since a potentially time-consuming discussion may take away from other pressing clinical matters (38). Ideally, providers should begin talking to their elderly patients about advance care planning early and have ongoing discussions, especially with changes in health status (3). This will introduce concepts of end of life care while elderly patients are able to participate in the decision-making process and allow patients to re-evaluate their values as they age or experience changes in their clinical situation.
Advance directives assume that patients can anticipate their preferences for care for hypothetical future heath states (8, 39). However, there is little evidence that decisions patients make when relatively healthy can predict treatment choices when death is imminent (39). Although the vast majority of very elderly participants in our study could state their health care preferences and were not emotionally upset by the end-of-life content, some had difficulty. We found that higher education was strongly associated with advanced directives in the very elderly. Because an estimated 27% of older adults have below basic document literacy (40), health literacy may be an important and unrecognized barrier to completing advance directives. Moreover, treatment preferences appear to be only moderately stable over time, but preferences to refuse life-prolonging treatment tend to be more stable than preferences to receive life-prolonging treatment (41). Given the advanced age of our sample and that the majority preferred comfort measures — it is likely that their goals of care would be relatively stable, but it is unclear how their preferences for specific life-prolonging interventions and distressing health states would change.
Our findings should be interpreted within the context of important limitations. These findings reflect views of non-Hispanic White community-dwelling elders, most of whom still reside in the Northeast, and may not be representative of elders from racial and ethnic minority groups or other geographic regions. In particular, studies have consistently shown that African American patients are more likely to undergo aggressive care, to prefer life-sustaining treatment, to want cardiopulmonary resuscitation, and to die in a hospital (11, 32, 42-48). African Americans are less likely to have discussions about life-sustaining treatments with physicians (49) and are much less accepting of advanced care planning. African Americans and Hispanic Americans have advanced directives less often than their White counterparts (44, 50-53). In addition, frail older ethnic minorities are less likely to self-express their own health care choices than their White counterparts (54) Next, we were unable to look in-depth at any one topic or explore reasons why few very elderly community-dwellers discuss wishes for care with their providers. Finally, we relied on participants’ self-report. It is possible that providers have addressed end of life issues with some participants, but participants did not recall or perceived the discussion differently. Although such information is subject to recall bias and participants’ perceptions, perhaps it speaks to the quality of the patient-provider communication.
In summary, many very elderly adults still reside in community settings and are capable of making treatment decisions near the end of life. Most elders were able to state their preferences, and few appeared upset or bothered when asked about end of life care. Although the majority of participants prefer comfort measures at the end of life, many indicated that they would endure life-prolonging interventions and distressing health states to avoid death. The reasons for this discrepancy are likely to be multifaceted. Yet, very few respondents reported having discussed their preferences with their providers. Future research should develop and test interventions to improve rates of end of life discussions in very elderly community-dwelling populations. These efforts should involve family members whenever possible. Discussions among the physician-patient-family triad may facilitate unified decision-making that is informed and rooted in patients’ values. Increased family involvement may help bridge outpatient and inpatient settings so that patients receive care that is consistent with their preferences.
Acknowledgements
The authors thank Sidney and Dorothy Stogel for providing funding for this study and acknowledge the support of Richard A. Parker, MD and Russell S. Phillips, MD. The National Heart, Lung, and Blood Institute’s (NHLBI) Framingham Heart Study is supported by contract number N01-HC-25195. Dr. Kelly-Hayes was also supported by grants from the National Institute on Aging (R01 AG08122, Epidemiology of Dementia in the Framingham Study) and National Institute of Neurological Disorders and Stroke (R01 NS17950, Precursors of Stroke Incidence and Prognosis). The funding agency had no role in the design, methods, subject recruitment, data collection, analysis or preparation of the manuscript.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
This paper was presented in part at the annual meeting of the Society of General Internal Medicine, New Orleans, Lousiana, May 2005.
REFERENCES
- 1.Field M, Cassel CK, editors. Approaching Death: Improving Care at the End of Life. National Academy Press; Washington DC: 1997. [PubMed] [Google Scholar]
- 2.AGS Ethics Committee The care of dying patients: A position statement from the American Geriatrics Society. J Am Geriatr Soc. 1995;43:577–8. doi: 10.1111/j.1532-5415.1995.tb06109.x. [DOI] [PubMed] [Google Scholar]
- 3.Wenger NS, Rosenfeld K. Quality indicators for end-of-life care in vulnerable elders. Ann Intern Med. 2001;135(8 Pt 2):677–85. doi: 10.7326/0003-4819-135-8_part_2-200110161-00006. [DOI] [PubMed] [Google Scholar]
- 4.Emanuel LL, von Gunten CF, Ferris FD. Advance care planning. Arch Fam Med. 2000;9(10):1181–7. doi: 10.1001/archfami.9.10.1181. [DOI] [PubMed] [Google Scholar]
- 5.Emanuel LL, Danis M, Pearlman RA, Singer PA. Advance care planning as a process: structuring the discussions in practice. J Am Geriatr Soc. 1995;43(4):440–6. doi: 10.1111/j.1532-5415.1995.tb05821.x. [DOI] [PubMed] [Google Scholar]
- 6.Gillick MR. Advance care planning. N Engl J Med. 2004;350(1):7–8. doi: 10.1056/NEJMp038202. [DOI] [PubMed] [Google Scholar]
- 7.Teno JM, Lynn J. Putting advance-care planning into action. J Clin Ethics. 1996;7(3):205–13. [PubMed] [Google Scholar]
- 8.Morrison RS, Meier DE. High rates of advance care planning in New York City’s elderly population. Arch Intern Med. 2004;164(22):2421–6. doi: 10.1001/archinte.164.22.2421. [DOI] [PubMed] [Google Scholar]
- 9.Hopp FP. Preferences for surrogate decision makers, informal communication, and advance directives among community-dwelling elders: results from a national study. Gerontologist. 2000;40(4):449–57. doi: 10.1093/geront/40.4.449. [DOI] [PubMed] [Google Scholar]
- 10.Gordon NP, Shade SB. Advance directives are more likely among seniors asked about end-of-life care preferences. Arch Intern Med. 1999;159(7):701–4. doi: 10.1001/archinte.159.7.701. [DOI] [PubMed] [Google Scholar]
- 11.Hanson LC, Earp JA, Garrett J, Menon M, Danis M. Community physicians who provide terminal care. Arch Intern Med. 1999;159(10):1133–8. doi: 10.1001/archinte.159.10.1133. [DOI] [PubMed] [Google Scholar]
- 12.Dawber T. The Framingham Study: The Epidemiology of Atherosclerotic Disease. Harvard University Press; Cambridge, MA: 1980. [Google Scholar]
- 13.Seshadri S, Wolf PA, Beiser A, et al. Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham Study. Neurology. 1997;49(6):1498–504. doi: 10.1212/wnl.49.6.1498. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy EP, Phillips RS, Zhong Z, Drews RE, Lynn J. Dying with cancer: patients’ function, symptoms, and care preferences as death approaches. J Am Geriatr Soc. 2000;48(5 Suppl):S110–21. doi: 10.1111/j.1532-5415.2000.tb03120.x. [DOI] [PubMed] [Google Scholar]
- 15.Somogyi-Zalud E, Zhong Z, Lynn J, Hamel MB. Elderly persons’ last six months of life: findings from the Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc. 2000;48(5 Suppl):S131–9. doi: 10.1111/j.1532-5415.2000.tb03122.x. [DOI] [PubMed] [Google Scholar]
- 16.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–14. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 17.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 18.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. the Index of Adl: a Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 19.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21(4):556–9. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 23.Framingham Heart Study [Accessed January 8, 2008]; http://www.framinghamheartstudy.org/biblio/index.html.
- 24.Brett AS. Limitations of listing specific medical interventions in advance directives. JAMA. 1991;266(6):825–8. [PubMed] [Google Scholar]
- 25.Volandes AE, Lehmann LS, Cook EF, Shaykevich S, Abbo ED, Gillick MR. Using video images of dementia in advance care planning. Arch Intern Med. 2007;167(8):828–33. doi: 10.1001/archinte.167.8.828. [DOI] [PubMed] [Google Scholar]
- 26.Rosenfeld KE, Wenger NS, Kagawa-Singer M. End-of-life decision making: a qualitative study of elderly individuals. J Gen Intern Med. 2000;15(9):620–5. doi: 10.1046/j.1525-1497.2000.06289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo B, Rouse F, Dornbrand L. Family decision making on trial. Who decides for incompetent patients? N Engl J Med. 1990;322(17):1228–32. doi: 10.1056/NEJM199004263221711. [DOI] [PubMed] [Google Scholar]
- 28.Markson L, Clark J, Glantz L, Lamberton V, Kern D, Stollerman G. The doctor’s role in discussing advance preferences for end-of-life care: perceptions of physicians practicing in the VA. J Am Geriatr Soc. 1997;45(4):399–406. doi: 10.1111/j.1532-5415.1997.tb05162.x. [DOI] [PubMed] [Google Scholar]
- 29.McDonald DD, Deloge JA, Joslin N, et al. Communicating end-of-life preferences. West J Nurs Res. 2003;25(6):652–66. doi: 10.1177/0193945903254062. discussion 667-75. [DOI] [PubMed] [Google Scholar]
- 30.Smucker WD, Ditto PH, Moore KA, Druley JA, Danks JH, Townsend A. Elderly outpatients respond favorably to a physician-initiated advance directive discussion. J Am Board Fam Pract. 1993;6(5):473–82. [PubMed] [Google Scholar]
- 31.Ditto PH, Danks JH, Smucker WD, et al. Advance directives as acts of communication: a randomized controlled trial. Arch Intern Med. 2001;161(3):421–30. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- 32.Tierney WM, Dexter PR, Gramelspacher GP, Perkins AJ, Zhou XH, Wolinsky FD. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16(1):32–40. doi: 10.1111/j.1525-1497.2001.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–94. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 34.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20(6):531–5. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Demoratz MJ. Advance directives: getting patients to complete them before they need them. Case Manager. 2005;16(1):61–3. doi: 10.1016/j.casemgr.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 36.Hawkins NA, Ditto PH, Danks JH, Smucker WD. Micromanaging death: process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45(1):107–17. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- 37.Emanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ. Advance directives for medical care--a case for greater use. N Engl J Med. 1991;324(13):889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 38.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277–83. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 39.Meier DE, Morrison RS. Autonomy reconsidered. N Engl J Med. 2002;346(14):1087–9. doi: 10.1056/NEJM200204043461413. [DOI] [PubMed] [Google Scholar]
- 40.Marcus EN. The silent epidemic--the health effects of illiteracy. N Engl J Med. 2006;355(4):339–41. doi: 10.1056/NEJMp058328. [DOI] [PubMed] [Google Scholar]
- 41.Ditto PH, Smucker WD, Danks JH, et al. Stability of older adults’ preferences for life-sustaining medical treatment. Health Psychol. 2003;22(6):605–15. doi: 10.1037/0278-6133.22.6.605. [DOI] [PubMed] [Google Scholar]
- 42.Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14(1):15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. J Gen Intern Med. 1996;11(11):651–6. doi: 10.1007/BF02600155. [DOI] [PubMed] [Google Scholar]
- 44.Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48(12):1779–89. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 45.Phillips RS, Wenger NS, Teno J, et al. Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Am J Med. 1996;100(2):128–37. doi: 10.1016/s0002-9343(97)89450-8. [DOI] [PubMed] [Google Scholar]
- 46.Rosenfeld KE, Wenger NS, Phillips RS, et al. Factors associated with change in resuscitation preference of seriously ill patients. The SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Arch Intern Med. 1996;156(14):1558–64. [PubMed] [Google Scholar]
- 47.Goodlin SJ, Zhong Z, Lynn J, et al. Factors associated with use of cardiopulmonary resuscitation in seriously ill hospitalized adults. JAMA. 1999;282(24):2333–9. doi: 10.1001/jama.282.24.2333. [DOI] [PubMed] [Google Scholar]
- 48.Eleazer GP, Hornung CA, Egbert CB, et al. The relationship between ethnicity and advance directives in a frail older population. J Am Geriatr Soc. 1996;44(8):938–43. doi: 10.1111/j.1532-5415.1996.tb01864.x. [DOI] [PubMed] [Google Scholar]
- 49.Haas JS, Weissman JS, Cleary PD, et al. Discussion of preferences for life-sustaining care by persons with AIDS. Predictors of failure in patient-physician communication. Arch Intern Med. 1993;153(10):1241–8. [PubMed] [Google Scholar]
- 50.Morrison RS, Zayas LH, Mulvihill M, Baskin SA, Meier DE. Barriers to completion of health care proxies: an examination of ethnic differences. Arch Intern Med. 1998;158(22):2493–7. doi: 10.1001/archinte.158.22.2493. [DOI] [PubMed] [Google Scholar]
- 51.Degenholtz HB, Arnold RA, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. J Am Geriatr Soc. 2002;50(2):378–81. doi: 10.1046/j.1532-5415.2002.50073.x. [DOI] [PubMed] [Google Scholar]
- 52.Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med. 2003;31(5 Suppl):S373–8. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- 53.Kiely DK, Mitchell SL, Marlow A, Murphy KM, Morris JN. Racial and state differences in the designation of advance directives in nursing home residents. J Am Geriatr Soc. 2001;49(10):1346–52. doi: 10.1046/j.1532-5415.2001.49263.x. [DOI] [PubMed] [Google Scholar]
- 54.Hornung CA, Eleazer GP, Strothers HS, 3rd, et al. Ethnicity and decision-makers in a group of frail older people. J Am Geriatr Soc. 1998;46(3):280–6. doi: 10.1111/j.1532-5415.1998.tb01038.x. [DOI] [PubMed] [Google Scholar]