Abstract
Although popular diets focus on weight loss and their favorable biochemical and physiological effects, fewer investigations have evaluated the biological impact of these diets during weight maintenance. To study this issue, three popular diets, Atkins, South Beach and Ornish were tested in a randomized and counterbalanced, crossover study between January and December 2006. Participants completed each of the three 4-week isocaloric dietary intervention phases followed by a 4-week washout period. They were weighed weekly and caloric adjustments made if weight change exceeded 1 kg. At the completion of each dietary phase, 3-day food records were analyzed, fasting blood sampled and brachial artery reactivity testing (BART) performed.
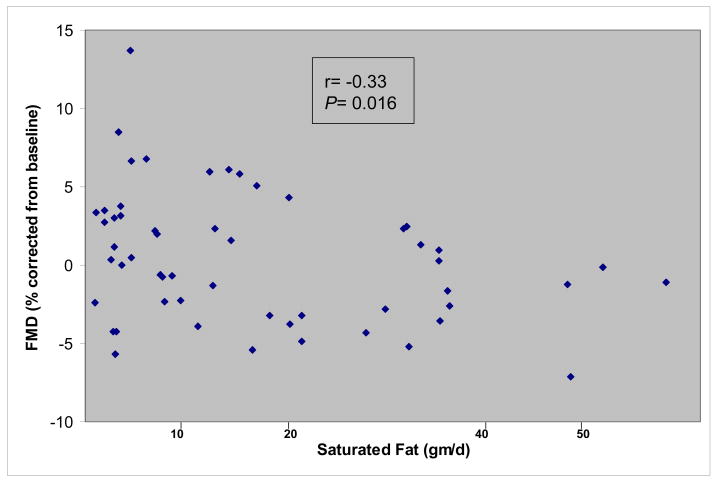
Eighteen adults completed all 3 isocaloric dietary phases. During the South Beach and Ornish maintenance phase there were significant reductions in low density lipoprotein cholesterol (LDL-C) (11.8% [P=0.01], 16.6% [P=0.0006], respectively) compared to pre-diet baseline. Moreover, in contrast to the Atkins maintenance phase, significant reductions in LDL-C and apolipoprotein B levels were observed after the South Beach (P=0.003, P=0.05, repeated measures ANOVA) and Ornish maintenance phase (P=0.0004, P=0.006, repeated measures ANOVA). Brachial artery testing revealed an inverse correlation between flow-mediated vasodilatation and intake of saturated fat (r=−0.33; p=0.016). These data suggest that during weight maintenance, less favorable biological effects are observed during a simulated, high fat Atkins diet when compared to the South Beach and Ornish diet. The findings support additional study in subjects with visceral obesity and the metabolic syndrome, in whom an increased risk of coronary disease at baseline may be accentuated with chronic consumption of a diet that exhibits unfavorable effects on lipids and endothelial function.
Keywords: Atkins, Ornish, South Beach, diet, lipids, endothelial function
Introduction
Popular diets designed to induce acute weight reduction represent a multibillion dollar a year industry (1). While numerous studies have evaluated the effectiveness of weight reduction and the extent to which weight loss is associated with improvement in a variety of metabolic parameters (e.g., glucose, lipids, blood pressure), considerably less information is available with regard to the effect of these parameters during weight maintenance. This is an important area to investigate because weight maintenance often represents the chronic phase prescribed after acute weight reduction has been achieved. Yet, surprisingly few data are available in the assessment of popular diets during weight maintenance. Because coronary heart disease (CHD) remains the leading cause of death in the United States and dietary factors contribute to the development and acceleration of atherothrombosis (2), the present study was designed to evaluate the impact of biochemical and physiological parameters affecting CHD risk during weight maintenance. If saturated fat is associated with low density lipoprotein (LDL) receptor downregulation (3) and endothelial dysfunction (4), two potential mechanisms accounting for elevated CHD risk (5), then popular diets that advocate high saturated fat intake (i.e., Atkins) may exhibit unfavorable effects on lipids and endothelial function compared to lower saturated fat intake during the weight maintenance phase.
Subjects and Methods
Subjects
A total of 26 adults responded to a posted advertisement seeking healthy adults aged 20 years and older. Because the study was not designed to investigate weight loss, inclusion criteria consisted of body mass index less than 30 kg/m2 and with no history of metabolic, hepatic, renal or systemic disease. They were comprised predominantly of medical students, residents and hospital employees. The participants were asked not to use herbal remedies, fish oils or anti-inflammatory medications. Alcohol use was permitted provided that intake was regular and that no more than 1 ounce was consumed daily. None of the volunteers were taking lipid-lowering or antihypertensive agents. Patients taking vasoactive medications (e.g., cetrizine) were asked not to take the medication the evening prior to brachial artery reactivity testing (BART). Volunteers were asked to maintain the same level of physical activity throughout the study. All studies were performed after an overnight fast of at least 12 hours, which included restriction of caffeine and alcohol. The protocol was approved by the Institutional Review Board and all subjects provided written informed consent.
Study Methods
This was a randomized crossover study of 3, 4-week dietary interventions with a 4-week washout period between each dietary phase for a total study period of 6 months for each participant. At the end of each 4-week interval, subjects returned for fasting blood measurements and BART testing. The study was undertaken between January and December, 2006.
Dietary Phases
The outpatient dietary interventions were based on 3 popular diets, the high fat, low carbohydrate Atkins diet (6), the Mediterranean South Beach diet (7) and the high carbohydrate, low fat Ornish diet (8). Dietary assignment was randomized and counterbalanced. At baseline, each volunteer provided 72-hour food records for analysis by a registered dietitian (RD) that served as the template for teaching participants how to record food items and quantity consumed during the trial. Subjects were informed at the outset that the study was not aimed at weight reduction but rather weight maintenance (e.g., within 1–2% of body weight) throughout the 6-month trial. Therefore, volunteers were weighed at weekly intervals and if weight alterations exceeded 1 kg, the RD adjusted caloric and nutrient intake accordingly. A total of 6 volunteers had dietary adjustments made during their 4-week dietary phase in order to maintain their weight within the designated range. At the conclusion of each 4-week dietary phase and 4-week washout phase, subjects presented after a 12-hour fast for blood drawing and endothelial testing. In all, there were 6 different phases; baseline, 1st diet, washout, 2nd diet, washout and 3rd diet for a total of 20-weeks from baseline to study completion.
Laboratory Methods
Lipoprotein and Biochemical Analysis
Following an overnight fast and signed consent, 30 mL of blood were collected by venipuncture into 2 tubes containing ethylenediaminetetraacetic acid centrifuged within 30 minutes at 4°C to separate plasma. Total cholesterol (TC) and triglycerides (TG) were measured using a Hitachi 704 clinical chemistry analyzer (Boehringer Mannheim Diagnostics, Indianapolis, IN) and high density lipoprotein cholesterol (HDL-C) was measured following precipitation of apolipoprotein B (ApoB) containing lipoproteins as previously described (9). Apolipoproteins A-I (apoA-1) and B were measured using a nephelometer (Behring Diagnostics, Inc., Westwood, MA) with reagents supplied by the manufacturer. Electrolytes, hepatic function and high sensitivity C-reactive protein (CRP) were measured by Quest Diagnostics (Van Nuys, CA).
Brachial Artery Flow Mediated Vasodilation
Brachial artery flow mediated (endothelial dependent) vasodilation (FMD) was measured using an 11-5 MHz broadband linear-array transducer and baseline images were acquired after a 15-minute supine equilibration period as previously described (10). Post-stimulus images were acquired 1 minute ± 15 seconds following the release of a 5-minute upper-arm occlusion. Baseline measurements were performed prior to each 4-week dietary phase and represented the average of 3 measurements that were analyzed by an experienced investigator blinded to subject’s identity and study phase.
Statistics
Sample-size calculations determined that 18 subjects would be required to detect a 15% reduction in TC between the high and low fat dietary phases with a standard deviation of 27 mg/dL, power 90% and α=0.05. Following each dietary phase, 72-hour food records were analyzed by a registered dietitian (CD) using the Nutri Base® V Personal Plus edition (version 5.19, 2005, CyberSoft, Inc, Phoenix, AZ). Participants were asked to record the amount of each item consumed; one RD reviewed the food records for completion and a second RD checked all entries to verify accuracy. Differences in energy intake, lipids (including log transformation for TG analysis), lipoproteins and other biochemical measurements before and after each dietary phase were analyzed using STATA Statistical Data Analysis software (version 8.2, January 2003, Statacorp, College Station, TX) and SAS (version 9.13, Cary NC). Repeated measures ANOVA (SAS proc Mixed, with a repeated statement and compound symmetric covariance structure) was used to estimate the mean within-person (post –pre value) change and standard error (SE) of the within person changes in metabolic parameters. A two-tailed P ≤ 0.05 was considered significant. For the brachial artery studies, FMD was quantified as the percent diameter change of the post-occlusion arterial diameter measurement relative to baseline and end-diastolic frames. Pearson’s correlation analysis was used to evaluate the association of change between saturated fat intake and FMD.
Results and Discussion
Of the 24 participants who enrolled in the study, 18 subjects (9 men and 9 women) completed the study; 8 withdrew due to logistical reasons or inability to continue with a specified dietary phase. Mean age was 30.6 ± 9.6 years, and mean body mass index was 22.6 ± 3 kg/m2. Mean fasting lipids and lipoproteins included TC of 184.9 ± 48.3 mg/dL, TG of 78.1 ± 32.7 mg/dL, LDL-C of 107.2 ± 48.3 mg/dL and HDL-C of 62.2 ± 17.0 mg/dL.
Baseline dietary composition was most consistent with a Mediterranean-like diet with mean total fat intake of 30 ± 10%. Dietary intake estimates of 72-hour food records demonstrated no appreciable change in energy intake between the Atkins (7216 ± 1844 kJ/d), South Beach (6732 ± 1338 kJ/d) and Ornish (6869 ± 1380 kJ/d) phases consistent with the absence of weight loss. However, the Atkins diet was associated with a greater intake of dietary cholesterol compared to South Beach or Ornish (567 ± 267 versus 202 ± 186 and 114 ± 89 mg/d; P < 0.05) as well as higher total fat (58 ± 9 versus 31 ± 11 and 9 ± 3; P < 0.001) and saturated fat content (30 ± 8 versus 14 ± 7 and 3 ± 1; P < 0.001) compared to the other 2 dietary phases. Table 1 outlines pre-dietary phase baseline after the 4 week washout phase and the respective post dietary changes following each assigned 4 week phase. There were no appreciable differences between baseline levels of lipids, lipoproteins or apolipoproteins in the 3 pre-dietary phases. However, TC and LDL-C were reduced after the South Beach and Ornish phases whereas TG, apoB and apoA1 were only reduced after Ornish. When comparing the 3 dietary phases, the Atkins diet evidenced greater increases in TC and LDL-C compared to either South Beach (P=0.007, P=0.003) or Ornish (P<0.0001, P=0.0004). In contrast, the Ornish diet was associated with reduced HDL-C and apoA-1 compared to either Atkins (P =0.01, P =0.0007) or South Beach (P =0.01, P =0.001) and lower levels of CRP (P =0.04) compared to Atkins dietary phase.
Table 1.
The effect of 3 popular diets on lipids, lipoproteins, apolipoproteins A1 and B (mg/dL) and C-Reactive Protein (mg/L) before and after completion of each 4-week dietary phase of the crossover study a,b.
| Pre (sd) | ChangeSE | 95% CI | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| within diet | between dietsd | ||||||||
| AS | AO | SO | |||||||
| TC | Atkins | 183.8 (44.0) | 9.2 | 4.7 | 0.0 to 18.3 | 0.06 | 0.007 | <0.0001 | 0.06 |
| South Beach | 182.6 (47.6) | −9.8 | 4.7 | −19.0 to 0.7 | 0.04 | ||||
| Ornish | 191.7 (51.2) | −22.7 | 4.7 | −31.8 to −13.5 | <0.001 | ||||
| TG | Atkins | 83.3 (29.7) | −3.7 | 7.9 | −19.1 to 11.8 | 0.65. | 0.95 | 0.08 | 0.07 |
| South Beach | 94.9 (47.6) | −4.3 | 7.9 | −19.8 to 11.1 | 0.59 | ||||
| Ornish | 86.1 (41.3) | 16.2 | 7.9 | 0.7 to 31.6 | |||||
| TGc | Atkins | 4.37(0.34) | −0.08 | 0.08 | −0.23 to 0.08 | 0.35 | 0.56 | 0.03 | 0.10 |
| South Beach | 4.44(0.50) | −0.01 | 0.08 | −0.16 to 0.15 | 0.91 | ||||
| Ornish | 4.35(0.47) | 0.18 | 0.08 | 0.02 to 0.33 | 0.03 | ||||
| HDL | Atkins | 62.9 (18.0) | 1.2 | 2.6 | −3.9 to 6.4 | 0.64 | 0.98 | 0.01 | 0.01 |
| South Beach | 62.0 (15.3) | 1.1 | 2.6 | −4.0 to 6.3 | 0.67 | ||||
| Ornish | 64.3 (14.7) | −8.7 | 2.6 | −3.6 to 13.9 | 0.002 | ||||
| LDL | Atkins | 96.1 (24.8) | 8.1 | 4.4 | −0.4 to 16.7 | 0.07 | 0.003 | 0.0004 | 0.44 |
| South Beach | 93.1 (48.4) | −11.8 | 4.4 | −20.4 to −3.3 | 0.01 | ||||
| Ornish | 102.2(37.1) | −16.6 | 4.4 | −25.2 to −8.1 | 0.0006 | ||||
| APOA1 | Atkins | 168.4(35.7) | 3.0 | 4.0 | −4.7 to 10.7 | 0.45 | 0.83 | 0.0007 | 0.001 |
| South Beach | 170.2(29.3) | 1.8 | 4.0 | −6.1 to 9.6 | 0.67 | ||||
| Ornish | 171.9(29.8) | −17.8 | 4.0 | −10.1 to −25.6 | 0.0001 | ||||
| APOB | Atkins | 81.7 (28.9) | 4.8 | 2.7 | −0.45 to 10.0 | 0.08 | 0.05 | 0.006 | 0.37 |
| South Beach | 77.9 (26.8) | −2.9 | 2.7 | −8.3 to 2.4 | 0.29 | ||||
| Ornish | 83.4 (31.0) | −6.4 | 2.7 | −1.2 to −11.6 | 0.02 | ||||
| CRP | Atkins | 0.39 (0.31) | 0.18 | 0.11 | −0.04 to 0.41 | 0.12 | 0.13 | 0.04 | 0.63 |
| South Beach | 0.64 (0.65) | −0.09 | 0.13 | −0.33 to 0.16 | 0.50 | ||||
| Ornish | 0.60 (0.51) | −0.17 | 0.12 | −0.4 to 0.06 | 0.16 | ||||
Pre= pre-dietary phase baseline
SD= standard deviation
SE= standard error
CI= confidence interval
TC= total cholesterol; TG= triglyceride; HDL=high density lipoprotein; LDL=low density lipoprotein
APOA1=apolipoprotein A1; APOB=apolipoprotein B; CRP=C-reactive protein
n=18
Repeated measures of analysis of variance using general linear modeling for each variable.
Log- transformed analysis
AS, AO, SO (differences between Atkins and South Beach, Atkins and Ornish and South Beach and Ornish Diets)
Baseline measurements of brachial artery FMD were similar in the Atkins (3.18 ± 0.59 mm), South Beach (3.16 ± 0.58 mm) and Ornish (3.18 ± 0.64 mm) diets. However, after the assigned dietary period, the Ornish diet was associated with higher FMD compared to Atkins and a non-significant increased FMD was also observed after the South Beach diet compared to Atkins. An inverse correlation between on-treatment FMD and saturated fat intake is illustrated in Figure 1 and inverse trend observed between FMD and total fat intake (r= −0.22; p=0.12).
Figure 1.
Inverse Correlation Between Saturated Fat Intake (gms/d) & Flow Mediated Vasodilation after correcting for baseline values
The most noteworthy finding in the present study was that during weight maintenance, the Atkins diet was associated with higher TC and LDL-C compared to the South Beach and Ornish dietary phases and reduced endothelial vasoreactivity compared to the Ornish phase. Moreover, saturated fat intake correlated inversely with endothelial function as assessed by BART. Previous isocaloric studies have demonstrated that a low fat, high carbohydrate diet is associated with elevation in TG and reductions in LDL-C and HDL –C compared to higher total and saturated fat intake (11, 12). Surprisingly however, there have been minimal isocaloric comparative evaluations of lipids and endothelial function. One study compared a diet high in carbohydrates (18% fat) to high saturated fat (37% fat), monounsaturated fat (37% fat) and polyunsaturated fat (36% fat) each for a 2-week intervention period. Significant reductions in brachial FMD were observed during the high saturated fat diet phase (4) although the short testing interval and lack of adjustment for covariates (13–15) may have impacted the modest effects observed. Because most dietary studies are relatively short term (i.e., less than 1 year) and focus on weight reduction efficacy, considerably less information is available regarding the potential clinical impact of popular diets after weight has been stabilized (i.e., long-term maintenance). The results of the present study suggest that a diet that exhibits unfavorable effects on lipids and endothelial function during the maintenance phase may be less advantageous compared with diets associated with improvement in these parameters. This is particularly noteworthy in subjects at increased risk of CHD (e.g., metabolic syndrome) (16), for whom long term dietary recommendations are often required.
There are several limitations associated with the present study. First, the study was not designed to compare the weight losing effects of popular diets but rather to evaluate the biological effects that occur during weight maintenance in apparently metabolically healthy, non-obese men and women. Therefore, the study results are neither generalizable to obese subjects or to those enrolled in the weight loss induction phase of these diets. Secondly, although lipid and endothelial related differences between the dietary phases were discernible despite a relatively small size, CRP measurements displayed greater variability suggesting that a larger sample size would be required to better delineate whether differences between the groups during the maintenance phase. A third limitation relates to the verification of adherence to dietary therapy. Specifically, it is recognized that weight monitoring and dietary food records, the primary tools used in the present study are less sensitive when compared with more reliable methods such as having assigned dietary meals prepared in a metabolic kitchen.
Conclusions
High saturated fat intake may adversely impact lipids and endothelial function during weight maintenance. As such, popular diets such as Atkins may be less advantageous for CHD risk reduction when compared to the Ornish and South Beach diets once weight loss has been achieved. The findings support additional study, especially in subjects with or at increased risk of CHD, in order to further explore the potential clinical implications of popular diets during long term maintenance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Malik VS, Hu FB. Popular weight-loss diets: from evidence to practice. Nat Clin Pract Cardiovasc Med. 2007;4:34–41. doi: 10.1038/ncpcardio0726. [DOI] [PubMed] [Google Scholar]
- 2.Brousseau ME, Schaefer EJ. Diet and coronary heart disease: clinical trials. Curr Atheroscler Rep. 2000;2:487–493. doi: 10.1007/s11883-000-0048-6. [DOI] [PubMed] [Google Scholar]
- 3.Dietschy JM. Dietary fatty acids and the regulation of plasma low-density lipoprotein cholesterol concentrations. J Nutr. 1998;128:444S–448S. doi: 10.1093/jn/128.2.444S. [DOI] [PubMed] [Google Scholar]
- 4.Keogh JB, Grieger JA, Noakes M, Clifton PM. Flow-mediated dilatation is impaired by a high-saturated fat diet but not by a high-carbohydrate diet. Arterioscler Thromb Vasc Biol. 2005;25:1274–1279. doi: 10.1161/01.ATV.0000163185.28245.a1. [DOI] [PubMed] [Google Scholar]
- 5.Robinson SD, Harding SA, Cummins P, et al. Functional interplay between platelet activation and endothelial dysfunction in patients with coronary heart disease. Platelets. 2006;17:158–62. doi: 10.1080/17476930500454514. [DOI] [PubMed] [Google Scholar]
- 6.Atkins RC. Dr. Atkin’s New Diet Revolution, Revised. Avon Books; NY: 1998. [Google Scholar]
- 7.Agatston A. The South Beach Diet. Rodale Press; Erasmus, PA: 2003. [Google Scholar]
- 8.Ornish D. Eat More, Weigh Less: Dr. Dean Ornish’s Life Choice Program for Losing Weight Safely While Eating Abundantly. HarperCollins Publishers; New York: 1993. [Google Scholar]
- 9.Miller M, Bachorik PS, McCrindle B, Kwiterovich PO. Effect of gemfibrozil in men with primary isolated hypoalphalipoproteinemia: A randomized, double-blind, placebo-controlled, crossover study. Am J Med. 1993;94:7–12. doi: 10.1016/0002-9343(93)90113-4. [DOI] [PubMed] [Google Scholar]
- 10.Vogel RA, Corretti MC, Plotnick GD. Changes in flow-mediated brachial artery vasoactivity with lowering of desirable cholesterol levels in healthy middle-aged men. Am J Cardiol. 1996;77:37–40. doi: 10.1016/s0002-9149(97)89131-x. [DOI] [PubMed] [Google Scholar]
- 11.Lichtenstein AH, Ausman LM, Carrasco W, Jenner JL, Ordovas JM, Schaefer EJ. Hypercholesterolemic effect of dietary cholesterol in diets enriched in polyunsaturated and saturated fat. Dietary cholesterol, fat saturation, and plasma lipids. Arterioscler Thromb. 1994;14:168–175. doi: 10.1161/01.atv.14.1.168. [DOI] [PubMed] [Google Scholar]
- 12.Grundy SM. Comparison of monounsaturated fatty acids and carbohydrates for lowering plasma cholesterol. N Engl J Med. 1986;314:745–748. doi: 10.1056/NEJM198603203141204. [DOI] [PubMed] [Google Scholar]
- 13.Williams MR, Westerman RA, Kingwell BA, Paige J, Blombery PA, Sudhir K, Komesaroff PA. Variations in endothelial function and arterial compliance during the menstrual cycle. J Clin Endocrinol Metab. 2001;86:5389–5395. doi: 10.1210/jcem.86.11.8013. [DOI] [PubMed] [Google Scholar]
- 14.Vogel RA, Corretti MC, Plotnick GD. Effect of a single high-fat meal on endothelial function in healthy subjects. Am J Cardiol. 1997;79:350–354. doi: 10.1016/s0002-9149(96)00760-6. [DOI] [PubMed] [Google Scholar]
- 15.Mori TA, Beilin LJ. Omega-3 fatty acids and inflammation. Curr Atheroscler Rep. 2004;6:461–7. doi: 10.1007/s11883-004-0087-5. [DOI] [PubMed] [Google Scholar]
- 16.Sarti C, Gallagher J. The metabolic syndrome: prevalence, CHD risk, and treatment. J Diabetes Complications. 2006;20:121–32. doi: 10.1016/j.jdiacomp.2005.06.014. [DOI] [PubMed] [Google Scholar]