Abstract
We have shown that a controlled-flow vacuum-free bottle system (CFVFB) vs. a standard bottle (SB) facilitates overall transfer and rate of milk transfer, and shortens oral feeding duration in very-low-birth-weight (VLBW) infants. We aimed to understand the basis by which this occurs. Thirty infants (19 males; 27 ± 1 weeks gestation) were randomized to a CFVFB or SB. Outcomes monitored at 1−2 and 6−8 oral feedings/day when infants were around 34 and 36 weeks postmenstrual age, respectively, included: overall transfer (% volume taken/volume prescribed), rate of milk transfer (ml/min), sucking stage, frequency of suction (#S/s) and expression (#E/s), suction amplitude (mmHg), and sucking burst duration (s). At both periods we confirmed that infants using a CFVFB vs. SB demonstrated greater overall transfer and rate of milk transfer, along with more mature sucking stages. Suction and expression frequencies were decreased with CFVFB vs. SB at 1−2 oral feeding/day; only that of suction was reduced at 6−8 oral feedings/day. No group differences in suction amplitude and burst duration were observed. We speculate that oral feeding performance improves without significant change in sucking effort with a CFVFB vs. SB. In addition, we have shown that VLBW infants can tolerate faster milk flow than currently presumed. Finally, the use of a CFVFB may reduce energy expenditure as it enhances feeding performance without increasing sucking effort.
Keywords: Bottle feeding, Oral feeding, Suck-swallow-breathe, VLBW, Prematurity, Deglutition, Deglutition disorders
Up to 30% of preterm infants experience difficulty making the transition from tube to oral feeding [1]. This is often due to immaturity in sucking, swallowing, uncoordinated suck-swallow-respiration, inappropriate behavioral states, and/or poor endurance [2-5]. Oral feeding difficulties are associated with delayed attainment of independent oral feeding and hospital discharge [5-7]. In recent years, an estimated 40% of the patients seen in feeding disorders clinics were children born prematurely [7]. Until recently, the difficulty in transitioning from tube to oral feeding has received little attention due to concerns over more immediate life-threatening medical complications, e.g., bronchopulmonary dysplasia, intraventricular hemorrhage, necrotizing enterocolitis. Nevertheless, with the rise in the preterm infant population over the last two decades, there is an urgent need to develop interventions that can safely enhance preterm infants’ oral feeding performance [1, 8-13]. Improving oral feeding skills will not only accelerate attainment of independent oral feeding and shorten hospitalization, but, importantly, reduce medical cost, allow earlier family reunification, and facilitate the development of a more appropriate mother-infant interaction and bonding [14]. Potentially, it may also decrease long-term feeding difficulties/disorders.
To develop efficacious interventions, it is necessary to gain a better understanding of the development of oral feeding skills [5, 15-21]. Safe and successful oral feeding requires not only appropriate sucking, swallowing, and respiration, but also the appropriate coordination of these three functions in order to prevent adverse episodes of apnea, bradycardia, oxygen desaturation, and/or aspiration. Studies have described the maturation of sucking in terms of suction and/or expression, the two components of sucking [16, 19, 22], as well as coarse and fine “structures,” as defined by earlier investigators, e.g., sucking burst duration and suction force/amplitude, respectively [16, 22, 23]. Suction is the negative intraoral pressure exerted by the infant while drawing milk into the mouth; expression is the lingual component implicated in the stripping/compression of the nipple to eject milk. This latter is also implicated in bolus formation, i.e., the oral phase of swallowing [16, 24-27]. In earlier studies [19, 28], we noted that the presence of these two components was not critical for the successful completion of oral feeding as the use of expression alone was sufficient, albeit not as efficient. We descriptively characterized the nutritive sucking pattern of preterm infants using a five-point developmental nutritive sucking scale based on the presence/absence of suction and expression and their rhythmicity [19]. This sucking scale correlated positively with postmenstrual age, overall transfer, and rate of milk transfer. These observations support the notion that maturation of nutritive sucking plays a significant role in improving oral feeding performance. As the stage of nutritive sucking is also reflective of the maturation of suck-swallow-respiration coordination, it is implied that an appropriate development of swallowing, respiration, and suck-swallow-respiration coordination is occurring concurrently. This is supported also with the observation that a mature nonnutritive sucking pattern does not imply mature nutritive sucking and/or successful oral feeding [29].
The use of a controlled-flow vacuum-free bottle system (CFVFB) has been shown to accelerate attainment of independent oral feeding in very-low-birth-weight (VLBW) infants [30]. Namely, it improved their ability to complete more of their feedings in a shorter feeding time and at a faster rate (ml/min) compared to their counterparts’ feeding with a standard bottle (SB). Therefore, it was deemed of interest to gain a better understanding of the basis upon which such improvement occurred. Such information would be of significant value in the development of new intervention(s) to facilitate transition from tube to oral feeding.
In this study we hypothesized that the use of a CFVFB, when compared to that of a SB, will enhance infants’ stage of sucking, along with a greater use of the suction component, greater suction amplitude, and longer sucking burst duration.
Methods
Subjects
Infants were recruited from the Neonatal Intensive Care Unit at Texas Children's Hospital, Houston, Texas, USA. The study was approved by the Institutional Review Board for Human Subjects at Baylor College of Medicine and Affiliated Hospitals. Informed parental consent was obtained following consultation with the attending physicians.
A total of 30 clinically stable preterm infants (19 males, 11 females) participated. Infants were enrolled if they were (1) born between 26 and 29 weeks gestational age (GA) as determined by obstetrical ultrasound and clinical exam; (2) of appropriate size for GA; (3) without congenital anomalies (e.g., oral, cardiac); and (4) without chronic medical conditions, including severe bronchopulmonary dysplasia [31], intraventricular hemorrhages (IVH) grade III or IV [32], periventricular leukomalacia (PVL), or necrotizing enterocolitis (NEC). Infants who had their enteral feeding stopped for greater than 7 consecutive days and/or developed IVH III or IV, PVL, and NEC after recruitment were dropped from the study.
Study Design
Infants were randomly assigned to the CFVFB or SB group. Management of oral feeding, i.e., introduction and advancement, was left to the discretion of the attending physician. Sucking skills were monitored when infants were taking 1−2 and 6−8 oral feedings/day. Infants were not disturbed for at least 30 min prior to each feeding session. The orogastric tube, if present, was removed prior to oral feeding assessment. Because nurses choose the nipples they feel are most appropriate for their patients, the ones used for the study were left to the nurses’ discretion as it was representative of infants’ oral feeding performance in the clinical setting. Caregivers fed the infants in their customary way; no encouragement, e.g., chin and/or cheek support, was provided during these feeding sessions. The duration of the oral feeding session was limited to 20 min as per nursery protocol.
Methodology
The SB used in this study was straight and cylindrical in shape (Fig. 1a). The CFVFB consisted of a nipple-bottle system that delivered milk to the nipple chamber from an open reservoir that was adjusted such that the milk level was maintained continually at the level of the infant's mouth (Fig. 1b). The milk reservoir was held secure on an IV pole and was readily adjusted to the level of the infant's mouth during feeding. Sucking parameters were recorded using a methodology described in previous studies [28, 33]. Briefly, the suction and expression components were monitored via two miniature pressure transducers (Model SPR-524, Millar Instruments, Houston, TX). For suction, one of the transducers was inserted through a polyethylene tubing flush with the tip of the nipple without protruding into the infant's mouth. Expression was monitored via a second transducer connected to a catheter made up of soft silastic tubing connected, in turn, to polyethylene tubing such that the compressible silastic portion was exteriorized along the nipple. To ensure the proper recording of the expression component, the catheter was positioned upward against the hard palate.
Fig. 1.
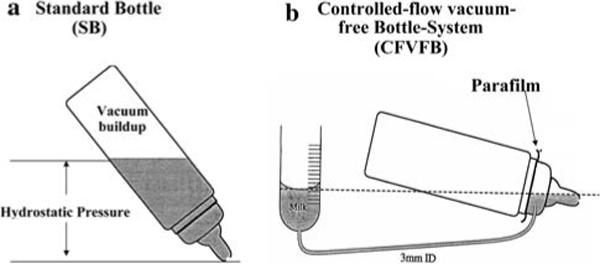
Schematic representation of the regular standard (SB) and controlled-flow vacuum-free (CFVFB) bottles
Study Outcomes
Oral feeding outcomes included overall transfer (percent volume of milk taken over the prescribed volume) and rate of milk transfer (volume transferred per unit time, ml/min). Sucking outcomes consisted of the stages of sucking using a five-point scale (Fig. 2) [19]: frequency of suction (#S/s) and expression (#E/s), suction amplitude (mmHg), and sucking burst duration. Postmenstrual age (PMA, weeks) at 1−2 and 6−8 oral feedings/day, nipple types (standard and premature nipple, ROSS Products, Abbott Laboratories, Columbus, OH, USA), and the number of infants who experienced episodes of apnea (cessation of breathing/20 s), bradycardia (heart rate < 100), and oxygen desatu-ration (<85%) were monitored as potential confounders in data analyses.
Fig. 2.
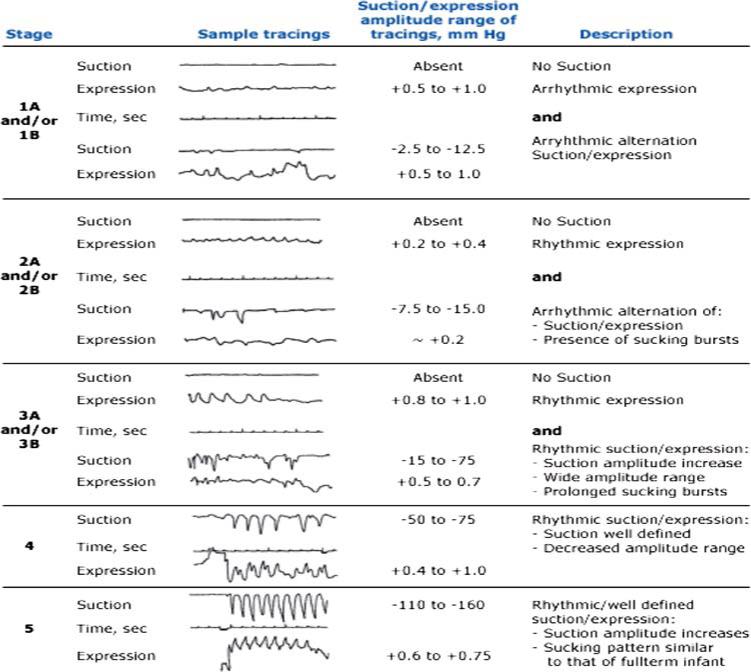
Descriptive scale of sucking stages: This scale comprises five stages based on presence/absence of suction and rhythmicity of suction and expression components during nutritive sucking from a bottle. Sample tracings with corresponding range of amplitudes are presented [from Lau C, Kusnierczyk I, Quantitative evaluation of infant's nonnutritive and nutritive sucking. Dysphagia 2001; 16:58; reproduced with permission from Springer Science and Business Media]
Statistical Analyses
A weighted average was used for the analyses of sucking outcomes. At both time periods (1−2 and 6−8 oral feedings/day), weighted averages were computed from two sucking bursts selected within the first and last 5 min of an oral feeding session. The following formula was used: (T1*B1 + T2*B2)/T1 + T2, with T1, T2 corresponding to the duration (s) of the respective sucking bursts, and B1, B2 relating to the average value of a particular sucking outcome. Sucking bursts were delineated by periods of pauses of 1.5 s or longer. The two sucking bursts analyzed were selected so that their sucking stage and duration were closest to the respective averages computed from all the sucking bursts during the first and last 5 min of the monitored sessions.
Independent t tests and paired t tests were used for continuous variables to compare between and within groups at 1−2 and 6−8 oral feedings/day, respectively. The χ2 test was used to assess differences in categorical variables. Based on an average rate of milk transfer of 1.6 ± 1.1 ml/min for infants born earlier than 30 weeks gestation, measured in an earlier study [30], an estimated sample size of 30 was calculated with an α level of 0.05, using a type 1 error of 0.05 and a power of 0.80. In order to detect a difference of 1.5 ml/min, 9 infants per group were estimated. Six additional participants per group were recruited for potential outliers.
Results
Subjects’ characteristics are summarized in Table 1. Both groups were comparable for GA, birth weight, gender distribution, and PMA at 1−2 and 6−8 oral feedings/day. Table 2 shows that at both periods the types of nipple used and number of infants experiencing episodes of apnea/bradycardia or oxygen desaturation were comparable between groups.
Table 1.
Subjects' characteristics
| SBa (n = 15) | CFVFBa (n = 15) | p* | |
|---|---|---|---|
| Gestational age (GA, weeks) | 27.7 ± 1.2 (26−29) | 27.9 ± 1.0 (26−29) | 0.738 |
| GA distribution | |||
| 26−27 weeks | 6 | 6 | 1.000** |
| 28−29 weeks | 9 | 9 | |
| Birth weight (g) | 956 ± 276 (560−1300) | 1037 ± 200 (727−1310) | 0.365 |
| Gender distribution | |||
| Male | 9 | 10 | 0.705** |
| Female | 6 | 5 | |
| Postmenstrual age (PMA, weeks) | |||
| 1−2 oral feedings/day | 34.3 ± 1.0 (33−37) | 34.2 ± 0.8 (33−36) | 0.695 |
| 6−8 oral feedings/day | 36.3 ± 1.5 (34−39) | 36.8 ± 2.0 (34−42) | 0.425 |
Values are mean ± sd (range)
Independent t test
χ2
Table 2.
Potential confounders
| 1−2 oral feedings/day |
6−8 oral feedings/day |
|||
|---|---|---|---|---|
| SB | CFVFB | SB | CFVFB | |
| Nipple type distribution | ||||
| Number of standard nipples used | 2 | 5 | 12 | 14 |
| Number of premature nipples used | 13 | 10 | 3 | 1 |
| Number of infants experiencing episode(s) of apnea/bradycardia | 2 | 4 | 2 | 3 |
| Number of infants experiencing episode(s) of oxygen desaturations | 2 | 4 | 3 | 2 |
Overall intake was significantly greater in infants feeding with a CFVFB as opposed to a SB at both monitored periods (p ≤ 0.007) (Fig. 3). It is of note that at 1−2 and 6−8 oral feedings/day, the percent overall transfer was similar for the CFVFB infants (p = 0.469), whereas it increased in the SB group (p = 0.016). The percentage of infants who completed their feeding was significantly different (p < 0.001) for the CFVFB vs. SB group. They were 80 vs. 13% and 93 vs. 47% at 1−2 and 6−8 oral feedings/day, respectively. Rate of milk transfer (Fig. 4) was significantly greater in the CFVFB vs. the SB group at both times (p < 0.001) and improved over time for both groups of infants (p ≤ 0.002). Feeding durations were significantly shorter in the CFVFB group than in the SB group at both periods (p ≤ 0.025, Table 3). Stages of sucking, on the other hand, were consistently more mature in infants using the CFVFB vs. SB (p < 0.05) (Fig. 5). Stages of sucking matured as both groups of infants advanced in oral feeding (p ≤ 0.003). Suction frequency (Fig. 6) decreased in CFVFB infants at 1−2 and 6−8 oral feedings/day compared to their SB counterparts (p ≤ 0.017) and increased over time only in the SB group (p = 0.022). Expression frequency (Fig. 6) decreased in CFVFB vs. SB infants at 1−2 oral feedings/day (p = 0.003) and increased over time only in the CFVFB infants (p = 0.002). Suction amplitude and sucking burst duration were similar in the two groups at both periods (Table 3).
Fig. 3.
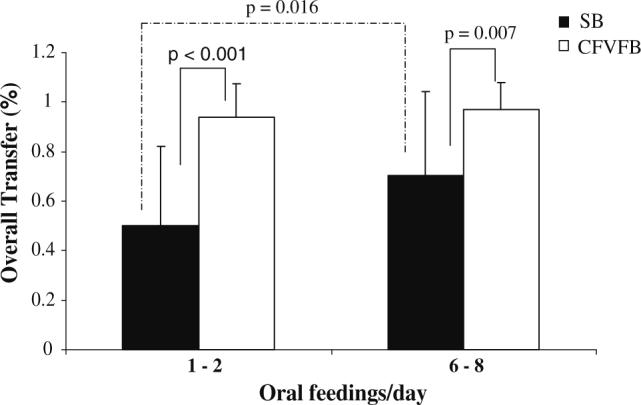
Percent overall transfer (percent volume taken over volume to be taken) at 1−2 and 6−8 oral feedings per day
Fig. 4.
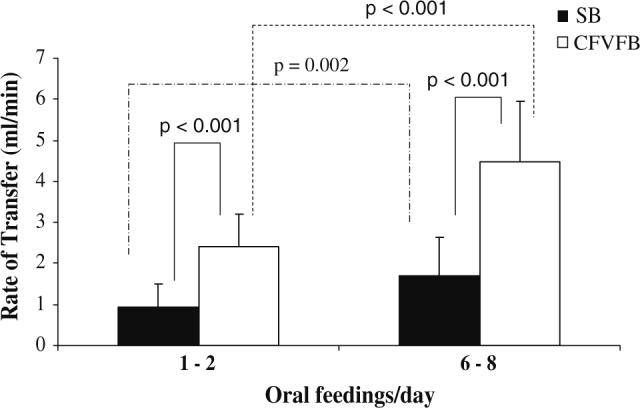
Rate of milk transfer (ml/min) at 1−2 and 6−8 oral feedings per day
Table 3.
Feeding outcomes
| SBa | CFVFBa | p* | |
|---|---|---|---|
| Feeding duration (min) | |||
| 1−2 oral feedings/day | 17.7 ± 4.7 | 14.1 ± 3.5§ | 0.025 |
| 6−8 oral feedings/day | 18.9 ± 3.4 | 12.3 ± 4.7 | <0.001 |
| Suction amplitude (mmHg) | |||
| 1−2 oral feedings/day | −26.2 ± 19.8 | −35.8 ± 21.2 | 0.257 |
| 6−8 oral feedings/day | −35.7 ± 25.7 | −52.0 ± 47.3 | 0.266 |
| Sucking burst duration (s) | |||
| 1−2 oral feedings/day | 16.2 ± 16.2 | 12.8 ± 7.6 | 0.449 |
| 6−8 oral feedings/day | 13.4 ± 7.6 | 16.1 ± 11.3 | 0.464 |
Values are mean ± sd
Independent t test
Fig. 5.
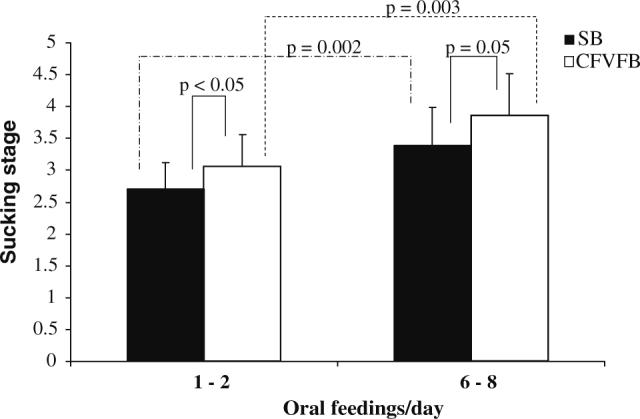
Stages of sucking at 1−2 and 6−8 oral feedings per day
Fig. 6.
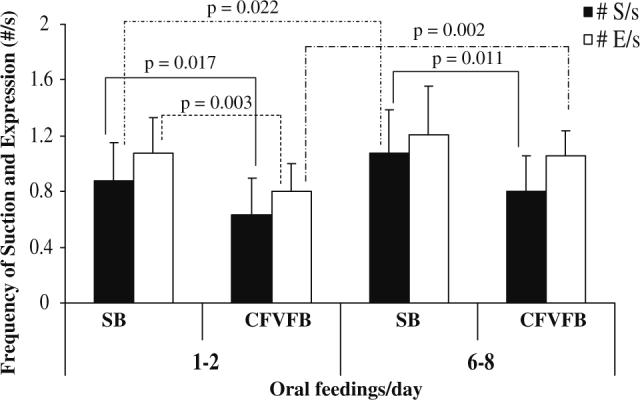
Frequency of suction (#S/s) and expression (#E/s) at 1−2 and 6−8 oral feedings per day
Discussion
With the increased survival of preterm infants, awareness of oral feeding difficulties in this population is growing. Development of safe interventions is needed to facilitate the transition of preterm infants from tube to oral feeding [8, 12, 13]. The use of a CFVFB is one such intervention. In the present study we confirmed our earlier observation that the use of a CFVFB, when compared to that of a SB, improves oral feeding performance in infants born between 26 and 29 weeks gestation, i.e., greater overall intake, rate of milk transfer, shorter feeding duration, with a greater number of these infants completing their feedings at both monitored periods. The present results confirm our hypothesis that infants offered a CFVFB demonstrate a more mature stage of sucking. However, they do not support the greater use of the suction component, greater suction amplitude, and longer sucking burst duration.
Two equally important considerations come into play when interpreting these results: first, the physical properties within standard bottles resulting from the physics of fluid mechanics as a feed progresses, and second, the level of maturation achieved by preterm infants at particular times in their advancement toward full oral feeding. These two conditions, although independent of each other, need to interact “fittingly” in order for infants to feed safely and efficiently by mouth.
Physical properties of baby bottles
With the use of a SB, vacuum builds up within the bottle as an infant withdraws milk [29]. As a feed progresses, this negative pressure/force increases, opposing the suction exerted by the infant, until the nipple seal is broken to allow equilibration inside and outside the bottle. For the infant, this situation leads to difficulty in generating suction and/or results in a net decrease in suction amplitude, hence, a decrease in the rate of milk flow. Consequently, the elimination of vacuum build-up offered by a CFVFB mechanically would be expected to increase suction efficiency and thus improve oral feeding performance as demonstrated in our results. In addition, the elimination of the hydrostatic pressure within the bottle, further offered by a CFVFB, allows the infant to control intake, as milk would flow only when sucking occurs and thus enhances safety.
Maturation level of preterm infants’ oral feeding skills
Nutritive sucking in clinically stable preterm infants matures as they progress toward full oral feeding [19]. However, as mentioned earlier, this functional development is the result not only of their sucking skill but also of their swallowing and respiratory competence, along with the adequate coordination of these three functions [20]. These factors, individually or combined, limit the rate of milk transfer that infants can generate and tolerate at a particular time in their progression toward full oral feeding [29, 34, 35].
With the advantages offered by a CFVFB and the functional limitations of preterm infants’ oral feeding skills, we conclude that the observed enhanced oral feeding performance resulted from the use of a more mature nutritive sucking pattern, likely the rhythmicity of sucking, along with increased sucking efficacy. The latter may result from infants generating faster rates of milk flow without significant changes in sucking parameters, i.e., no increased use of suction and suction amplitude. From this observation we advance that VLBW infants can tolerate faster milk flow than currently presumed, i.e., the rate of milk transfer being 2.5 to 3 times faster with a CFVFB than with a SB. In an earlier study [35], we advanced that infants can regulate their sucking skills so as to obtain a flow rate they can tolerate based on their level of suck-swallow-respiration coordination. This aptitude is indirectly confirmed by two observations made in this study: (1) Infants did not increase the use of suction or suction amplitude when the elimination of vacuum in the bottle would have readily facilitated such a response. (2) Infants using the CFVFB showed an increase in expression but not suction frequency between 1−2 and 6−8 oral feedings per day, whereas their counterparts using a SB demonstrated an increase in suction but not expression frequency. It should be remembered that expression is less efficient than suction [19, 28]. Finally, we speculate that the use of a CFVFB system may reduce energy expenditure as it enhances feeding performance without increasing sucking effort.
Sucking burst duration has been used as an index of oral feeding performance: the longer the sucking burst, the greater the expected intake [5, 36]. However, this may not be necessarily valid if the sucking pattern and amplitude change. With a more efficient sucking pattern due to maturation or facilitated by a particular intervention, as is the case in this study, burst durations need not increase.
In summary, this study provides a clearer understanding of the basis that allowed improved oral feeding performance with the use of a CFVFB. It demonstrates that (1) by eliminating the resistance to flow engendered by the vacuum buildup normally occurring in a standard bottle, oral feeding performance is improved with no significant change in sucking effort, (2) developmentally, VLBW infants can tolerate faster milk flow than currently presumed, and (3) use of a CFVFB may offer an additional advantage as reduced sucking effort would lead to energy conservation.
Acknowledgments
The authors thank C. Scheel, MD, for his assistance in data collection, and E. O. Smith, PhD, and K. Fraley for their assistance in statistics. This project was supported by the National Institute of Child Health and Human Development (R01-HD28140; R01-HD044469) and the Fonds de la Recherche en Santé du Québec for a graduate student scholarship (SF). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
Contributor Information
Richard J Schanler, Schneider Children's Hospital at North Shore, Manhasset, NY 11023, USA.
Chantal Lau, Department of Pediatrics/Neonatology, Baylor College of Medicine, One Baylor Plaza, BCM 320, Houston, TX 77030, USA.
References
- 1.Hawdon JM, Beauregard N, Slattery J, Kennedy G. Identification of neonates at risk of developing feeding problems in infancy. Dev Med Child Neurol. 2000;42:235–9. doi: 10.1017/s0012162200000402. [DOI] [PubMed] [Google Scholar]
- 2.Comrie JD, Helm JM. Common feeding problems in the intensive care nursery: maturation, organization, evaluation, and management strategies. Semin Speech Lang. 1997;18:239–60. doi: 10.1055/s-2008-1064075. [DOI] [PubMed] [Google Scholar]
- 3.Gardner SL, Hagedorn MI. Physiologic sequelae of prematurity: the nurse practitioner's role. Part V. Feeding difficulties and growth failure (pathophysiology, cause, and data collection. J Pediatr Health Care. 1991;5:122–134. doi: 10.1016/0891-5245(91)90022-i. [DOI] [PubMed] [Google Scholar]
- 4.VandenBerg KA. Nippling management of the sick neonate in the NICU: the disorganized feeder. Neonatal Netw. 1990;9:9–16. [PubMed] [Google Scholar]
- 5.Lau C, Hurst N. Oral feeding in infants. Curr Probl Pediatr. 1999;29:105–24. doi: 10.1016/s0045-9380(99)80052-8. [DOI] [PubMed] [Google Scholar]
- 6.Schanler RJ, Shulman RJ, Lau C, Smith EO, Heitkemper MM. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics. 1999;103:434–9. doi: 10.1542/peds.103.2.434. [see comments].
- 7.Burklow KA, Phelps AN, Schultz JR, McConnell K, Rudolph C. Classifying complex pediatric feeding disorders. J Pediatr Gastroenterol Nutr. 1998;27:143–7. doi: 10.1097/00005176-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Burklow KA, McGrath AM, Kaul A. Management and prevention of feeding problems in young children with prematurity and very low birth weight. Inf Young Children. 2002;14:19–30. [Google Scholar]
- 9.Harris M. Oral-motor management of the hight-risk neonate. Phys Occup Ther Pediatr. 1986;6:231–53. [Google Scholar]
- 10.Bazyk S. Factors associated with the transition to oral feeding in infants fed by nasogastric tubes. Am J Occup Ther. 1990;44:1070–8. doi: 10.5014/ajot.44.12.1070. [DOI] [PubMed] [Google Scholar]
- 11.McGrath JM, Braescu AV. State of the science: feeding readiness in the preterm infant. J Perinat Neonatal Nurs. 2004;18:353–68. doi: 10.1097/00005237-200410000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Thoyre SM. Developmental transition from gavage to oral feeding in the preterm infant. Annu Rev Nurs Res. 2003;21:61–92. [PubMed] [Google Scholar]
- 13.Shaker CS, Woida AM. An evidence-based approach to nipple feeding in a level III NICU: nurse autonomy, developmental care, and teamwork. Neonatal Netw. 2007;26:77–83. doi: 10.1891/0730-0832.26.2.77. [DOI] [PubMed] [Google Scholar]
- 14.Lau C. Effects of stress on lactation. Pediatr Clin North Am. 2001;48:221–34. doi: 10.1016/s0031-3955(05)70296-0. [DOI] [PubMed] [Google Scholar]
- 15.Wolff PH. The serial organization of sucking in the young infant. Pediatrics. 1968;42:943–56. [PubMed] [Google Scholar]
- 16.Sameroff AJ. The components of sucking in the human newborn. J Exp Child Psychol. 1968;6:607–23. doi: 10.1016/0022-0965(68)90106-9. [DOI] [PubMed] [Google Scholar]
- 17.Buchholz DW, Bosma JF, Donner MW. Adaptation, compensation, and decompensation of the pharyngeal swallow. Gastrointest Radiol. 1985;10:235–9. doi: 10.1007/BF01893106. [DOI] [PubMed] [Google Scholar]
- 18.Bu'Lock F, Woolridge MW, Baum JD. Development of co-ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Dev Med Child Neurol. 1990;32:669–78. doi: 10.1111/j.1469-8749.1990.tb08427.x. [DOI] [PubMed] [Google Scholar]
- 19.Lau C, Alagugurusamy R, Schanler RJ, Smith EO, Shulman RJ. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatr. 2000;89:846–52. [PubMed] [Google Scholar]
- 20.Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92:721–7. [PubMed] [Google Scholar]
- 21.Gewolb IH, Vice FL. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev Med Child Neurol. 2006;48:589–94. doi: 10.1017/S001216220600123X. [DOI] [PubMed] [Google Scholar]
- 22.Kaye H. Infant sucking behavior and its modification. In: Lipsitt LP, Spiker CC, editors. Advances in child development and behavior. Vol. 3. Academic Press; New York: 1967. pp. 1–52. [Google Scholar]
- 23.Crook CK. Taste and the temporal organization of neonatal sucking—The genesis of sweet preference. In: Weiffenbach JM, editor. Taste and development. Department of HEW, NIH; Bethesda, MD: 1977. pp. 146–60. DHEW Publ No. (NIH) 77−1068
- 24.Colley JRT, Creamer B. Sucking and swallowing in infants. Br Med J. 1958;2:422–4. doi: 10.1136/bmj.2.5093.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ardran GM, Kemp FH, Lind J. A cineradiographic study of bottle feeding. Br J Radiol. 1958;31:11–22. doi: 10.1259/0007-1285-31-361-11. [DOI] [PubMed] [Google Scholar]
- 26.Ardran GM, Kemp FH, Lind JA. Cineradiographic study of breast feeding. Br J Radiol. 1958;31:156–62. doi: 10.1259/0007-1285-31-363-156. [DOI] [PubMed] [Google Scholar]
- 27.Adverson JC, Lefton-Greif MA. A professional manual with caregiver guidelines. Communication Skill Builders; San Antonio, TX: 1998. Pediatric videofluoroscopic swallow studies. [Google Scholar]
- 28.Lau C, Sheena HR, Shulman RJ, Schanler RJ. Oral feeding in low birth weight infants. J Pediatr. 1997;130:561–9. doi: 10.1016/s0022-3476(97)70240-3. [DOI] [PubMed] [Google Scholar]
- 29.Lau C, Kusnierczyk I. Quantitative evaluation of infants nonnutritive and nutritive sucking. Dysphagia. 2001;16:58–67. doi: 10.1007/s004550000043. [DOI] [PubMed] [Google Scholar]
- 30.Lau C, Schanler RJ. Oral feeding in premature infants: advantage of a self-paced milk flow. Acta Paediatr. 2000;89:453–9. doi: 10.1080/080352500750028186. [DOI] [PubMed] [Google Scholar]
- 31.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 32.Papile L, Burnstein J, Burnstein R, Kuffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 grams. J Pediatr. 1978;92:529–34. doi: 10.1016/s0022-3476(78)80282-0. [DOI] [PubMed] [Google Scholar]
- 33.Fucile S, Gisel E, Lau C. Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. J Pediatr. 2002;141:230–6. doi: 10.1067/mpd.2002.125731. [DOI] [PubMed] [Google Scholar]
- 34.Mathew OP. Breathing patterns of preterm infants during bottle feeding: role of milk flow. J Pediatr. 1991;119:960–5. doi: 10.1016/s0022-3476(05)83056-2. [DOI] [PubMed] [Google Scholar]
- 35.Scheel CE, Schanler RJ, Lau C. Does the choice of bottle nipple affect oral feeding performance of very-low-birth-weight (VLBW) infants? Acta Paediatr. 2005;94:1–8. doi: 10.1080/08035250510027255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medoff-Cooper B, Verklan T, Carlson S. The development of sucking patterns and physiologic correlates in very-low-birth-weight infants. Nurs Res. 1993;42:100–5. [PubMed] [Google Scholar]


