Abstract
Objective
Autoimmune lymphoproliferative syndrome (ALPS) is a disorder of apoptosis, often presenting in childhood. Similarly, MRL/lpr−/− mice homozygous for Fas mutations develop an ALPS-like disease with autoimmunity, lymphadenopathy, splenomegaly, and expansion of double negative T (DNT) cells. Currently, there are no proven therapies with adequate safety margins for sustained abolition of the lymphoproliferation associated with ALPS. We sought to test the ability of valproic acid (VPA), a histone deacetylase inhibitor, to induce apoptosis and inhibit lymphoproliferation.
Methods
Human peripheral blood mononuclear cells (PBMCs) from patients with ALPS and normal controls were tested in vitro to determine the efficacy of VPA at inducing cell death. VPA was used in vivo to control lymphoproliferation in MRL/lpr−/− mice, a model for ALPS.
Results
VPA induced cell death in vitro, and was partially inhibited by the pan caspase inhibitor, Z-VAD-FMK. MRL/lpr−/− mice treated with VPA for 8 weeks showed significant reductions in spleen and lymph node weights and cellularity compared to controls. A concomitant decrease in DNT cells was observed in the spleen, lymph nodes, and peripheral blood. Serum levels of VPA peaked 1 hour after injection, and a 2.5 fold increase in histone acetylation was observed in the spleen at 4 hours after injection.
Conclusion
Based on our data, VPA is effective at reducing lymphoproliferation in mice, and is currently being studied in a clinical trial as a lympholytic agent in patients with ALPS.
Keywords: ALPS, valproic acid, histone deacetylase inhibitor, lymphadenopathy, splenomegaly, MRL/lpr mice
Introduction
Autoimmune lymphoproliferative syndrome (ALPS) is a disorder of defective Fas-mediated apoptosis that typically presents early in life and persists for many years[1]. ALPS is characterized by lymphadenopathy, splenomegaly, hypergammaglobulinemia, elevated IL-10 levels[2], autoimmunity, and accumulation of double negative T (DNT) cells[3], which are virtually pathognomonic of ALPS[4]. Mutations in the Fas gene account for approximately 70% of all ALPS-cases and patients with these mutations are classified as ALPS type Ia. Other cases of ALPS have been associated with mutations in Fas ligand (FasL; ALPS type Ib), caspase genes (ALPS type II), N-RAS (type IV), or in as yet unidentified genes affecting apoptosis (ALPS type III)[5–8]. More recently, patients with somatic mutations in the Fas gene affecting the DNT cells have been described [9] and are classified as ALPS type Ia somatic.
The role of Fas in maintaining lymphocyte homeostasis and peripheral immune tolerance was first elucidated by studies using Fas-deficient MRL/LpJ-Tnfrsf6lpr (MRL/lpr−/−) mice[10]. These mice have a similar phenotype as humans with ALPS, including massive lymphadenopathy, splenomegaly, hypergammaglobulinemia, autoimmunity, and accumulation of DNT cells. Although MRL/lpr−/− mice develop severe glomerulonephritis and vasculitis, as opposed to the autoimmune multilineage cytopenias often observed in ALPS patients, they have frequently been used as a model to test potential therapeutics[11–16].
Immunosuppressive drugs have shown beneficial effects in the treatment of ALPS-associated autoimmune diseases, but have a limited effect on lymphoproliferation as their prolonged use is fraught with complications. Our goal has been to find a relatively safe drug with a history of clinical use, since the majority of ALPS patients are relatively stable notwithstanding their enlarged lymph nodes and spleen. Since approximately 50% of children with ALPS have refractory autoimmune cytopenias and undergo splenectomy, placing them at increased risk of life-threatening pneumococcal and meningococcal bacteremia, we sought a safe and effective medication to control lymphoproliferation and hypersplenism. Several histone deacetylase (HDAC) inhibitors, including apicidin[17, 18], sodium butyrate[19], and psammaplin A[20] induce apoptosis of various tumor cells. Two HDAC inhibitors, trichostatin A (TSA) and suberonylanilide hydroxamic acid (SAHA) have been used to treat MRL/lpr−/− mice. Mice treated with TSA or SAHA had reduced splenomegaly and lessened kidney disease compared with animals given vehicle alone[21, 22].
We explored the efficacy of two other HDAC inhibitors, romidepsin (depsipeptide) and valproic acid (VPA), in vitro and in the MRL/lpr−/− mouse. Both romidepsin[23–28] and VPA[29–35] induce apoptosis of tumor cells in vitro. Although VPA induces apoptosis of selected cell types, it has also been shown to protect neurons from apoptosis[36–39]. VPA exerts its apoptotic effects through both caspase-dependent and caspase-independent pathways[40, 41]. Romidepsin is under evaluation in clinical trials for the treatment of leukemia, T cell lymphoma, renal carcinoma, and other tumors (www.clinicaltrials.gov). VPA is commonly used in children and adults to prevent seizures, and is also currently being tested in patients with cancer[42]. Preliminary data in one ALPS patient showed that the dose used to treat seizures was effective at inhibiting histone acetylation.
Here we show that VPA induces cell death in PBMCs from healthy blood donors and from patients with ALPS in vitro. VPA-induced cell death was partially blocked by the pan-caspase inhibitor Z-VAD-FMK. Romidepsin and VPA reduced the number of lymphocytes and DNT cells in MRL/lpr−/− mice. While a short course of romidepsin in older mice was effective, it was also associated with reduced bone marrow cellularity; in contrast, VPA did not affect the bone marrow. Further studies in MRL/lpr−/− mice showed that serum levels of VPA peaked one-hour post-injection, while histone acetylation levels in the spleen peaked four hours post-injection. Our results indicate that valproic acid reduces accumulation of DNT cells in the lymphoid tissue and blood of MLR/lpr−/− mice and may have a role in the treatment of patients with ALPS.
Materials and Methods
In vitro cell death studies
Studies to confirm whether and how valproic acid induces apoptosis were conducted with cryopreserved human peripheral blood mononuclear cells (PBMCs) obtained after written informed consent under National Institutes of Health (NIH) institutional review board (IRB)-approved protocols for ALPS patients (93-I-0063) with defined functional Fas mutations (Type 1a) and from normal control subjects, as previously described[14]. Briefly, normal and ALPS type Ia PBMCs were thawed, washed and cultured at 106 cells/mL in complete RPMI-1640 with 10% fetal bovine serum and phytohemaglutinin-L (PHA-L, 0.5 ug/ml; Sigma, St. Louis, MO) for 48 hours at 37°C. Cells were then washed and incubated with 300U/mL of recombinant human interleukin 2 (IL-2) for 4 days. IL-2 stimulated human PBMCs were transferred to 96-well flat bottom plates (2×105 cells/well) and incubated for 48 hours in duplicate or triplicate wells with valproic acid at 0, 0.05, 1, 2 and 4 mM. Following drug exposure, cells were harvested and analyzed by fixed-time flow cytometry, as previously described[3]. Briefly, cells were washed and labeled with 7AAD and annexin V (BD Pharmingen, San Diego, CA) and run on a FACS Caliber (BD Pharmingen) for a fixed amount of time. Cell death is given as a percent of detected cells from control wells. To determine whether valproic acid induced lymphocyte apoptosis through a caspase-dependent pathway, 0 or 50 uM of the pan-caspase inhibitor Z-VAD-FMK (BD Pharmingen) or DMSO only was added to IL-2 stimulated PBMC cultures at the same time as drug. Cells were incubated in duplicate with inhibitor for 48 hours and the media (containing fresh pan-caspase inhibitor and valproic acid) was replaced at 24 hours. After 48 hours, cells were harvested and analyzed by fixed-time flow cytometry.
MRL/LpJ-Tnfrsf6lpr mouse studies
Eight-week old female MRL/LpJ-Tnfrsf6lpr (MRL/lpr−/−) mice (Jackson Laboratories, Bar Harbor, ME) were injected intaperitoneally (i.p.) 5 times per week in four independent experiments (30 mice per group total) with 500 mg/kg of valproic acid dissolved in PBS or PBS alone for 8 weeks. The 500 mg/kg dose was used based on preliminary dose escalation studies starting at 250 mg/kg based on the published literature. Mice were treated as above at 250, 350 or 500 mg/kg VPA and sacrificed. The 500 mg/kg dose yielded the greatest clinical benefit and showed histone acetylation levels comparable to those observed in one ALPS patient treated with the standard clinical dose for seizures. Alternatively, 18-week old female MRL/LpJ-Tnfrsf6lpr (MRL/lpr−/−) mice (Jackson Laboratories) received three injections of romidepsin (depsipeptide) at 2 mg/kg or vehicle intravenously (i.v.) every 4 days over 2 weeks (n = 8/group). Romidepsin was used as a proof of concept for this class of drug and was given for a short course due to sclerosing of the tail vein following repeated i.v. administration. Mice were sacrificed to quantify spleen weights; cellularity of the spleen, lymph nodes, and bone marrow; lymphocyte subsets in spleen, lymph node and peripheral blood. MRL/lpr−/− mice injected with vehicle (PBS) served as controls. Spleen, lymph node and bone marrow cellularity were assessed by isolating single cell suspensions and counting live cells by trypan blue exclusion. Lymphocyte subsets were determined by flow cytometry of single cell suspensions, using PE-labeled anti-CD3 (145-2C11), PerCp-labeled anti-CD4 (L3T4), FITC-labeled anti-CD8 (Ly-2) and APC-labeled anti-CD45R (B220, RA3-6B2) anti-murine antibodies (BD Pharmingen, San Diego, CA.). B cells were identified as CD45R+CD3−. Total CD3+ cells include the CD4+, CD8+ and DNT cell subsets. Single positive T cells were CD3+CD4+CD8−CD45R− or CD3+CD4−CD8+CD45R−. DNT cells were identified as being CD3+CD45R+CD4−CD8−. Samples were run on a FacsCaliber (BD Pharmingen). Flow cytometry data was analyzed using FloJo 8.6.
VPA serum levels
Serum levels of VPA were performed by a competitive binding assay using a Fluorescence Polarization Immunoassay run on an Abbott AxSYM analyzer (Abbott Laboratories, Abbott Park). The run-to-run precision was 4.8 % at 74.2 mg/L and the within run precision was 3.4 % at 78.6 mg/L. The lower limit of detection was 4.0 mg/L. Cross reactivity of the major metabolite of VPA (3-keto-valproic acid) was less than 10% and cross reactivity of the minor metabolites (3-hydroxy, or 4 hydroxy, or 4-en, or 2-propyl-glutarate, 5-hydroxy) was below the limit of detection.
Acetylation
Spleen cell lysate was added to loading buffer (1:1 guanidine thiocyanate/PBS). Samples were serially diluted 1:2 six times. Dilutions were loaded into a 96 well vacuum manifold (Bio-Rad, Hercules, CA) with 2 nitrocellulose membranes (Protran; Whatman, North America) and vacuum was applied slowly. The membrane was then removed, washed twice in Tris buffered saline before incubation with mouse antibody to GAPDH at a 1:500 dilution (American Research Products, Belmont, MA), followed by hybridization with anti-mouse Horseradish peroxidase antibody at a 1:1000 dilution (Amersham, Piscataway, NJ). The blot was imaged using enhanced chemiluminescence (Amersham). The membrane was then stripped using ReBlot Plus Mild Antibody Striping Solution (Millipore, Temecula, CA) for 10 min, incubated with anti-acetyl histone H3 rabbit antibody at a 1:2200 dilution, incubated with anti-rabbit horseradish peroxidase antibody at a 1:1000 dilution (Amersham), and imaged using enhanced chemiluminescence. Densitometry was performed using IPLab gel software.
Statistical analysis
Data was analyzed using JMP 5.0.1a software for 2-way Student T-tests and one-way ANOVA with post-hoc tests.
Results
Valproic acid induces cell death in vitro in a caspase-dependent and caspase–independent manner
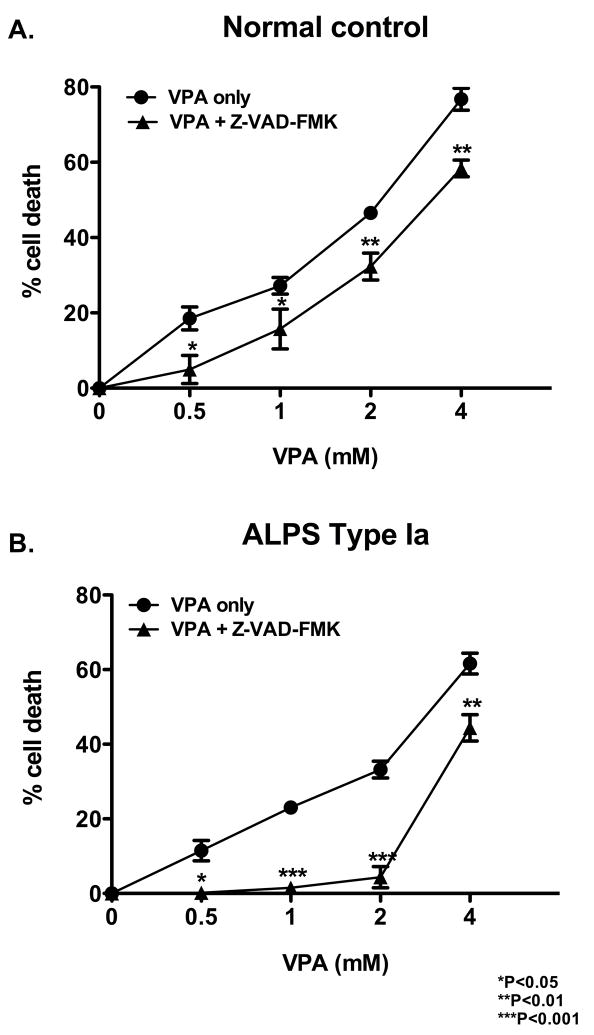
PBMCs from healthy persons (controls) and patients with ALPS Type 1a were stimulated with PHA-L and expanded in media containing IL-2 for 4 days, followed by incubation with varying concentrations of VPA for 48 hours in the presence or absence of the pan-caspase inhibitor, Z-VAD-FMK (50 uM). Background cell death with Z-VAD-FMK alone was approximately 40% greater than DMSO alone or media alone in both normal control (9.4% vs 5.5% vs 6.2%, respectively) and ALPS (15.1% vs 8.2% vs 7.7%, respectively) PBMC cultures. These values were accounted for in that all data were based on the control wells containing no VPA, which included Z-VAD-FMK, DMSO or media only. Control PBMCs showed a high degree of cell death induced by VPA, and only modest protection with Z-VAD-FMK (Fig. 1A). In contrast, PBMCs from patients with ALPS Type 1a showed a high degree of cell death induced by VPA, and increased protection from apoptosis by caspase inhibition compared to control PBMCs (Fig. 1B). Thus, valproic acid induced cell death through both caspase-dependent and caspase–independent mechanisms in PBMCs from patients with ALPS type Ia in vitro.
Figure 1. Valproic acid induces cell death in vitro.
PBMCs were incubated with valproic acid (VPA) for 48 hours in the presence or absence of the caspase inhibitor, Z-VAD-FMK (50uM). A. Normal control (N=2). B. Patient with type 1a ALPS (N=2).
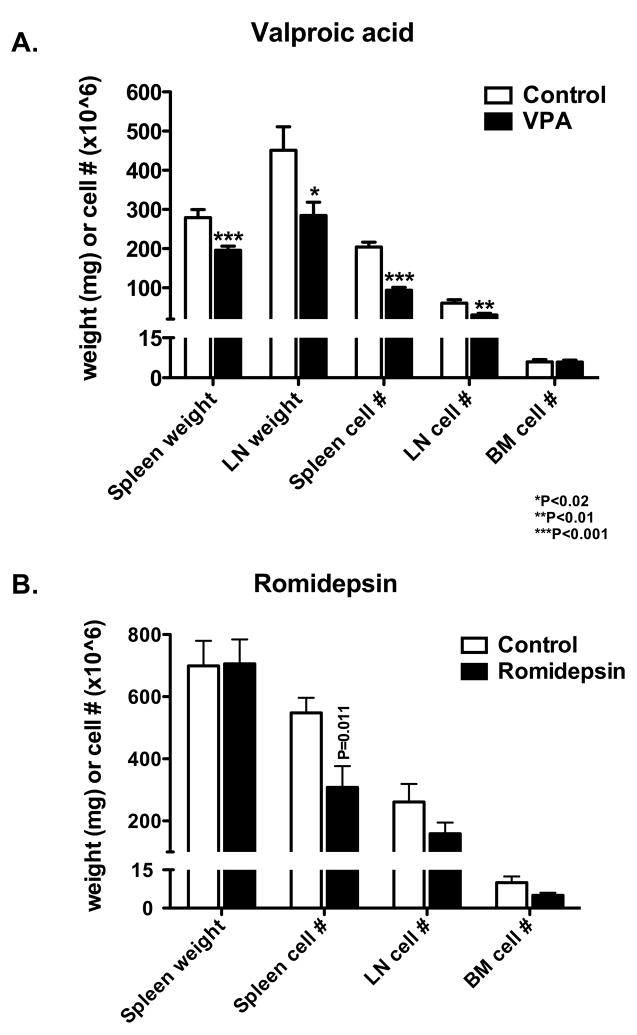
Lymphoid organ weight and cellularity are reduced with VPA treatment
Although observed differences were not as robust as can be expected following a standard chemotherapy regimen, weights of the spleen and lymph nodes (pooled inguinal, axillary, and brachial nodes) were significantly lower in mice treated with VPA compared with vehicle alone (Fig. 2A). Single cell suspensions prepared from inguinal lymph nodes and spleens showed that the cellularity of the lymph nodes and spleen were significantly reduced in mice treated with VPA versus vehicle alone (Fig. 2A). Mice receiving three i.v. doses of romidepsin as a control HDAC (histone deacetylase) inhbitor at 2 mg/kg showed reductions in the cellularity of the spleen, lymph nodes and bone marrow compared to animals that received vehicle alone (Fig. 2B). It should also be noted that the spleen weight and cellularity do not always correlate as tightly, in a predictable fashion, due to fatty deposits and necrosis in some spleens. Thus, VPA, in contrast to romidepsin, did not affect bone marrow cellularity while reducing lymphoid organ weight and cellularity.
Figure 2. Lymphoid organ weights and cellularity are reduced with valproic acid or romidepsin.
(A). Thirty mice in each group received 500 mg/kg valproic acid (VPA) or vehicle only (control) intraperitoneally 5 times per week for 8 weeks. Lymph node (LN) weight was the sum of inguinal, axillary, and brachial lymph nodes; lymph node cellularity was based on inguinal nodes only. (B) Eight mice in each group received three doses of 2 mg/kg romidepsin or vehicle i.v. Spleen weight, and spleen, lymph node, and bone marrow cellularity were determined.
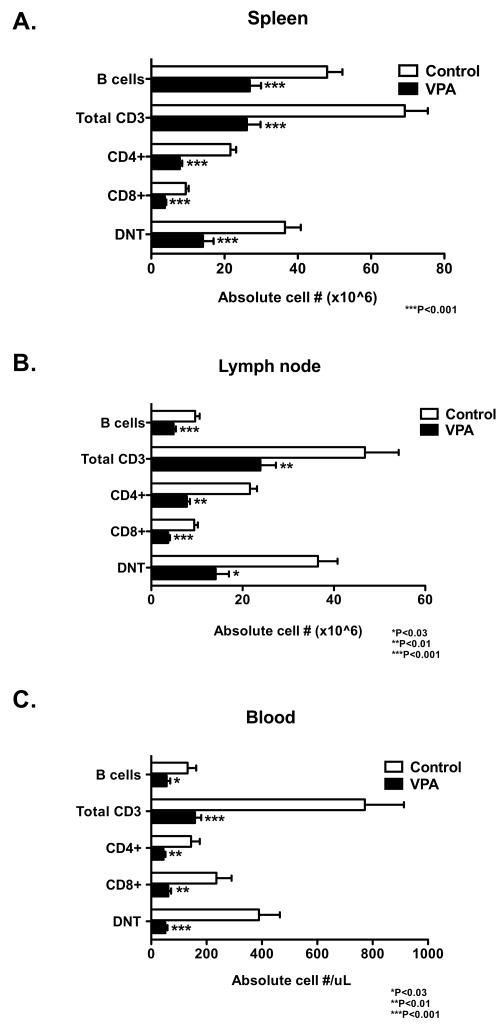
Double negative T cells are reduced with VPA treatment
Single cell suspensions were prepared from the spleen, lymph nodes, and peripheral blood of mice treated with VPA or vehicle alone. Mice treated with VPA had significantly lower numbers of B and T lymphocytes, specifically, CD3+, CD4+, CD8+, and DNT cells in the spleen (Fig. 3A), lymph nodes (Fig. 3B) and blood (Fig. 3C) compared to animals that received vehicle alone. The percent of DNT cells in the spleen (23.1±4.7 vs 55.7±2.7; P<0.001), lymph nodes (55.2±4.6 vs 66.7±1.3; P<0.02), and peripheral blood (31.8±2.8 vs 66.1±1.2; P<0.001) were also significantly reduced in mice treated with 2 mg/kg romidepsin compared with animals receiving vehicle alone. Although all lymphocyte types were reduced in number in spleen, lymph nodes and blood of mice treated with VPA, the observation that DNT cells were the lymphocyte type that showed the most significant reduction in the peripheral blood suggests that DNT cells may be more sensitive than other cell types to valproic acid.
Figure 3. Double-negative T cells are reduced with valproic acid treatment.
Absolute cell numbers in the (A) spleen and (A) inguinal lymph nodes were determined based on cell number per organ and percentages based on flow cytometry. The absolute lymphocyte types in the (C) blood was based on flow cytometry percentage and peripheral blood lymphocyte absolute numbers. Flow cytometry analysis of cells stained with antibodies to CD3, CD4, CD8 and CD45R (B220). N=30/group for spleen and lymph node values and 17–19/group for blood.
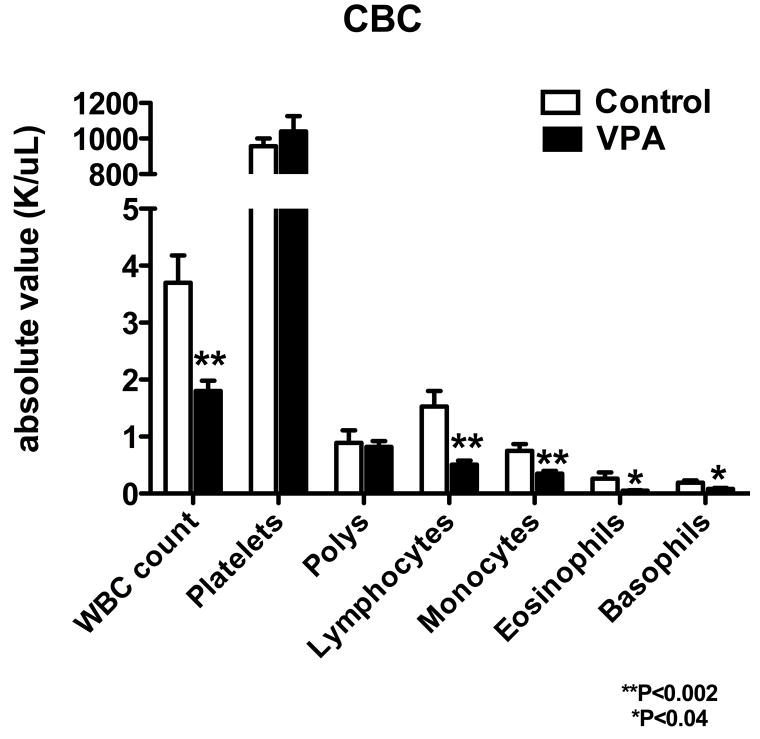
White blood cell, lymphocyte, and monocyte counts are reduced in the peripheral blood of mice treated with VPA
Mice receiving 500 mg/kg VPA for 8 weeks showed a lower total white blood cell count in the peripheral blood and significantly reduced numbers of lymphocytes, monocytes, eosinophils and basophils compared with animals receiving vehicle alone (Fig. 4). The greatest reduction (nearly 3-fold) was observed in the lymphocyte counts, and much of this reduction was attributable to the loss of DNT cells in the peripheral blood based on the flow cytometric data above.
Figure 4. Differential blood counts of mice treated with valproic acid.
Mice received 500 mg/kg valproic acid (VPA) or vehicle only (control) intraperitoneally 5 times per week for 8 weeks. N=17–19/group.
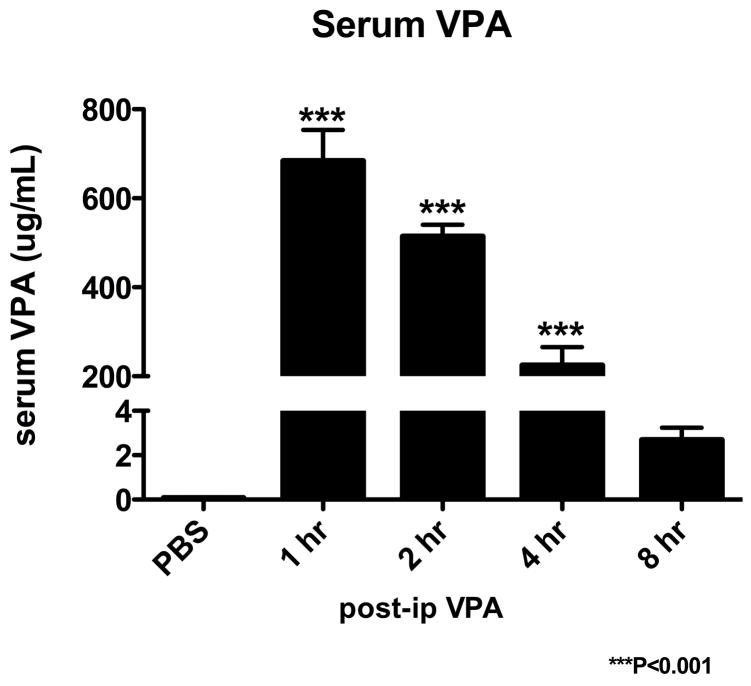
Correlation of serum levels of VPA and acetylation of histone 3 in the spleen following administration of VPA to mice
Mice were injected i.p. with a single dose of valproic acid at 500 mg/kg and sacrificed 1, 2, 4 and 8 hours later. VPA levels peaked at one hour after i.p. injection and declined thereafter, reaching levels that were not statistically different from pre-treatment levels by 8 hours (Fig. 5).
Figure 5. Serum levels peak at one hour after valproic acid treatment.
Eight to 10 mice in each group received a single injection of 500 mg/kg valproic acid (VPA) intraperitoneally and were sacrificed at given time points post injection. PBS shows mice that received phosphate buffered saline only. Serum valproic acid levels were determined.
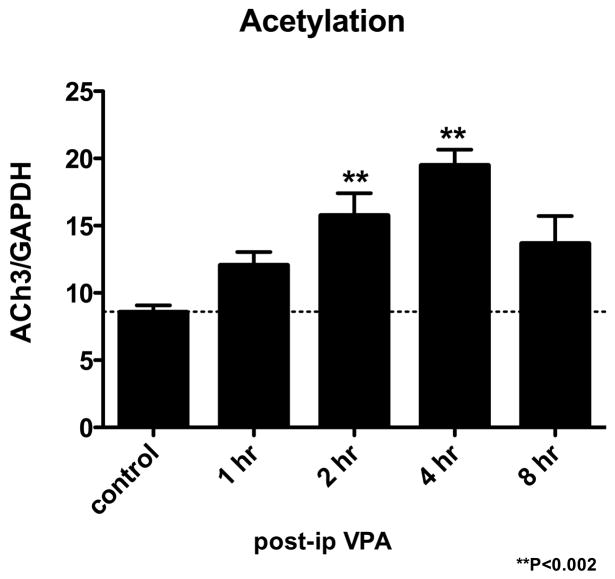
Dot blot assays were performed on splenocytes from mice injected i.p. to determine the level of acetylation of histone H3. Acetylation peaked to approximately 2.5-fold over pre-treatment levels at four hours after a single i.p. dose of VPA and then fell to 1.6-fold over baseline at 8 hrs (Fig. 6). Thus, while serum levels of VPA peaked at 1 hr after an i.p. dose and then rapidly declined, acetylation of histone 3 in the spleen peaked later and remained elevated for at least 8 hrs after the medication was given.
Figure 6. Histone acetylation peaks at four hours after valproic acid treatment.
Two mice for each time point received a single injection of 500 mg/kg valproic acid (VPA) and were sacrificed at given times after injection. Control shows mice that received vehicle only (PBS). Splenocytes were used to determine acetylation of histone 3 by dot blot assay. Acetylated histone 3 (ACh3)/GAPDH ratios are plotted against time.
Discussion
Here we show that the HDAC inhibitor VPA induces cell death of PBMCs from healthy persons and from patients with ALPS. We found that VPA induces both caspase-dependent and caspase-independent death of PBMCs isolated from healthy persons and patients with ALPS in vitro. Although there was greater cell death in the normal control at higher doses, the clinical equivalent of 0.5 to 1 mM VPA showed similar values. The effects of caspase inhibition appeared to be greater in PBMCs from patients with ALPS than from normal control subjects, suggesting that the PBMCs from the ALPS patients may be more sensitive to stimuli that induce apoptosis, other than Fas. It should be noted that these effects may be more pronounced in activated lymphocytes, as opposed to naïve circulating lymphocytes. VPA induces a large number of changes in cellular gene and protein expression related to apoptosis including an increased expression of Fas and Fas ligand resulting in activation of caspase-8[29]; increasing caspase-3 activation[32]; sensitizing cells to TRAIL[33]; down-regulating bcl-XL, while up-regulating bax[35]; and activation of p21 and suppression of c-Myc[34], as well as affecting Notch signaling[43]. In addition, VPA reduces the level of bcl-2 resulting in loss of mitochondrial membrane potential and release of cytochrome c from the mitochondria[29, 35, 40, 44]. Thus, the observation that VPA induces apoptosis at least partially through the intracellular mitochondrial pathway is consistent with our findings that VPA induces apoptosis of PBMCs from patients with ALPS who have a defect in their Fas signalling pathway.
VPA reduced the cellularity of spleen and lymph nodes and reduced the number of CD3+CD4−CD8− T cells in the spleen, lymph nodes and blood; however, VPA did not affect the cellularity in the bone marrow of MRL/lpr−/− mice compared with untreated mice. Lymphodepletion is not a common side effect of VPA in humans or mice, therefore, the relative lymphopenia observed in MRL/lpr−/− mice may be specific to these animals. This may be the result of the relatively high dose MRL/lpr−/− mice received, approximately ten times the human dose. However, it is unclear how the mice metabolize VPA compared to humans, and many drugs are used at higher dose in mice to achieve comparable results. In addition, although a high dose was given once a day for five days a week to achieve clinical reduction in lymphoproliferation, a lower dose may be as effective if given twice per day, seven days per week, as in humans. Alternatively, VPA treatment of MRL/lpr−/− mice may simply inhibit further lymphoproliferation making it appear as a relative reduction when compared to control mice that continue to accumulate lymphoid mass. In contrast, we found that a short course of romidepsin in MRL/lpr−/− mice reduced the cellularity in the bone marrow as well as in the spleen and lymph nodes. Thus, the lack of observed myelosuppression with VPA may be an asset in children with ALPS who likely require long-term therapy. However, romidepsin may also prove to be a more potent HDAC inhibitor that can be used at lower doses and less frequently to maintain reduced lymphocyte numbers in ALPS.
While we found a reduction in vasculitis of the kidney with VPA, the overall renal pathology score was increased (data not shown). This may rather be the result of the route rather of administration, since renal impairment is not a known side effect of VPA when given to humans. Studies are ongoing to determine the oral dose required in mice to achieve similar serum levels observed with i.p. VPA. Further studies would also be warranted in other lupus prone strains, such as NZB/W, to determine if increased renal disease is a general phenomena of VPA given i.p. In contrast to our study, Mishra et al.[21] and Reilly et al.[22] demonstrated that treatment of MRL/lpr−/− mice subcutaneously with trichostatin and parenterally with SAHA resulted in reduced overall kidney pathology, respectively. Trichostatin A decreased levels of interferon (IFN)-gamma, IL-12p40, IL-6, IL-10 proteins in splenocytes from MRL/lpr−/− mice in vitro[21]. These cytokines have the potential to contribute to inflammation and pathologic changes in the kidney. While VPA is an HDAC inhibitor like SAHA or trichostatin, VPA may also have different effects on autoimmunity in MRL/lpr−/− mice. Additional studies are ongoing to explore the impact of VPA on autoimmunity by looking at kidney/liver enzymes, cytokines and autoantibody production.
We found that treatment of MRL/lpr−/− mice with VPA induced histone acetylation in splenocytes that persisted longer than the serum levels of VPA. Previous experiments showed that treatment of splenocytes isolated from MRL/lpr−/− mice with trichostatin or SAHA resulted in accumulation of acetylated histone H3 and H4[21]. A more recent study from the same authors showed site-specific hypoacetylation of H3 and H4 in splenocytes from MRL/lpr−/− mice compared to control wild-type MRL mice, and increased site-specific acetylation of H3 and H4 to normal levels and attenuation of disease when animals were treated with trichostatin[45]. Thus, VPA yields similar changes in histone acetylation to trichostatin and SAHA, but given its wider clinical experience in children, makes it an attractive potential therapy in ALPS. We hypothesize that HDAC inhibitors may be more effective in ALPS patients due to their lack of a fully functional extrinsic apoptosis pathway, making them more susceptible and sensitive to activation of the intrinsic pathway or reactive oxygen species. Perhaps there are more fundamental epigenetic differences that have yet to be determined between ALPS patients and normal individuals. Further studies are required to explore mechanistic questions and gain further insights into this class of drugs.
In summary, we found that VPA reduced lymphoproliferation in MRL/lpr−/− mice, which suggests that VPA might be useful in patients with ALPS as a lympholytic agent in combination with another agent(s) that can reduce autoimmune complications. Mycophenolate mofetil is currently being used in patients with ALPS for the treatment of autoimmune disease, but the drug has little effect on lymphoproliferation in these patients (Rao et al., unpublished data). Thus, the combination of mycophenolate mofetil and VPA might be useful for treating both the autoimmunity and lymphoproliferation associated with ALPS. While not robustly ablative, VPA did reduce lymph node and spleen weights, but the sizes of these organs were still increased relative to wild-type mice of the same age. However, these data may not necessarily correlate to the human response, which may be even better when given long-term. Valproic acid at lower doses may also decrease the threshold required for apoptosis to occur thus allowing a second drug given in combination to be more effective. Additionally, VPA might be used as a corticosteroid sparing agent either to reduce ongoing lymphoproliferation, or perhaps more effectively, to keep lymphadenopathy from recurring in persons treated with corticosteroids so that the latter medication can be tapered and discontinued while avoiding a splenectomy in the long run. We also speculate that by decreasing accumulation of abnormal lymphocytes we may be able to decrease the relative risk of developing secondary malignancies. A preliminary trial using VPA in one patient with ALPS at standard oral doses used for seizure disorders showed that the drug increased histone acetylation by 2.5 to 3.5 fold, which was similar to the increase observed in mice. We are currently enrolling patients with ALPS in a clinical trial to determine the efficacy of VPA in controlling lymphoproliferation.
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, NIAID, Bethesda, MD 20892.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sneller MC, Straus SE, Jaffe ES, et al. A novel lymphoproliferative/autoimmune syndrome resembling murine lpr/gld disease. J Clin Invest. 1992;90:334–341. doi: 10.1172/JCI115867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopatin U, Yao X, Williams RK, et al. Increases in circulating and lymphoid tissue interleukin-10 in autoimmune lymphoproliferative syndrome are associated with disease expression. Blood. 2001;97:3161–3170. doi: 10.1182/blood.v97.10.3161. [DOI] [PubMed] [Google Scholar]
- 3.Sneller MC, Wang J, Dale JK, et al. Clincal, immunologic, and genetic features of an autoimmune lymphoproliferative syndrome associated with abnormal lymphocyte apoptosis. Blood. 1997;89:1341–1348. [PubMed] [Google Scholar]
- 4.Rao VK. Taking ALPS down a Notch. Blood. 2008;111:477. [Google Scholar]
- 5.Avila NA, Dwyer AJ, Dale JK, et al. Autoimmune lymphoproliferative syndrome: a syndrome associated with inherited genetic defects that impair lymphocytic apoptosis--CT and US features. Radiology. 1999;212:257–263. doi: 10.1148/radiology.212.1.r99jl40257. [DOI] [PubMed] [Google Scholar]
- 6.Lim MS, Straus SE, Dale JK, et al. Pathological findings in human autoimmune lymphoproliferative syndrome. Am J Path. 1998;153:1541–1550. doi: 10.1016/S0002-9440(10)65742-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliveira JB, Bidere N, Niemela JE, et al. NRAS mutation causes a human autoimmune lymphoproliferative syndrome. Proc Natl Acad Sci U S A. 2007;104:8953–8958. doi: 10.1073/pnas.0702975104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Werff ten Bosch J, Otten J, Thielemans K. Autoimmune lymphoproliferative syndrome type III, an indefinite disorder. Leuk Lymphoma. 2001;41:501–511. doi: 10.3109/10428190109060341. [DOI] [PubMed] [Google Scholar]
- 9.Holzelova E, Vonarbourg C, Stolzenberg MC, et al. Autoimmune lymphoproliferative syndrome with somatic Fas mutations. N Engl J Med. 2004;351:1409–1418. doi: 10.1056/NEJMoa040036. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe-Fukunaga R, Brannan CI, Copeland NG, Jenkins NA, Nagata S. Lymphoproliferation disorder in mice explained by defects in Fas antigen that mediates apoptosis. Nature. 1992;356:314–317. doi: 10.1038/356314a0. [DOI] [PubMed] [Google Scholar]
- 11.Bobe P, Bonardelle D, Benihoud K, Opolon P, Chelbi-Alix MK. Arsenic trioxide: A promising novel therapeutic agent for lymphoproliferative and autoimmune syndromes in MRL/lpr mice. Blood. 2006;108:3967–3975. doi: 10.1182/blood-2006-04-020610. [DOI] [PubMed] [Google Scholar]
- 12.Choi Y, Ramnath VR, Eaton AS, et al. Expression in transgenic mice of dominant interfering Fas mutations: a model for human autoimmune lymphoproliferative syndrome. Clin Immunol. 1999;93:34–45. doi: 10.1006/clim.1999.4767. [DOI] [PubMed] [Google Scholar]
- 13.Federzoni E, Gordon G, Muller S, Schmid I, Simon HU, Yousefi S. Expression of CD95 on mature leukocytes of MRL/lpr mice after transplantation of genetically modified bone marrow stem cells. Immunol Lett. 2008;117:45–49. doi: 10.1016/j.imlet.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Rao VK, Dowdell KC, Dale JK, et al. Pyrimethamine treatment does not ameliorate lymphoproliferation or autoimmune disease in MRL/lpr−/− mice or in patients with autoimmune lymphoproliferative syndrome. Am J Hematol. 2007;82:1049–1055. doi: 10.1002/ajh.21007. [DOI] [PubMed] [Google Scholar]
- 15.Teachey DT, Seif AE, Brown VI, et al. Targeting Notch signaling in autoimmune and lymphoproliferative disease. Blood. 2008;111:705–714. doi: 10.1182/blood-2007-05-087353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teachey DT, Obzut DA, Axsom K, et al. Rapamycin improves lymphoproliferative disease in murine autoimmune lymphoproliferative syndrome (ALPS) Blood. 2006;108:1965–1971. doi: 10.1182/blood-2006-01-010124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Im JY, Park H, Kang KW, Choi WS, Kim HS. Modulation of cell cycles and apoptosis by apicidin in estrogen receptor (ER)-positive and-negative human breast cancer cells. Chem Biol Interact. 2008;172:235–244. doi: 10.1016/j.cbi.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Park H, Im JY, Kim J, Choi WS, Kim HS. Effects of apicidin, a histone deacetylase inhibitor, on the regulation of apoptosis in H-ras-transformed breast epithelial cells. Int J Mol Med. 2008;21:325–333. [PubMed] [Google Scholar]
- 19.Mohana Kumar B, Song HJ, Cho SK, Balasubramanian S, Choe SY, Rho GJ. Effect of histone acetylation modification with sodium butyrate, a histone deacetylase inhibitor, on cell cycle, apoptosis, ploidy and gene expression in porcine fetal fibroblasts. J Reprod Dev. 2007;53:903–913. doi: 10.1262/jrd.18180. [DOI] [PubMed] [Google Scholar]
- 20.Ahn MY, Jung JH, Na YJ, Kim HS. A natural histone deacetylase inhibitor, Psammaplin A, induces cell cycle arrest and apoptosis in human endometrial cancer cells. Gynecol Oncol. 2008;108:27–33. doi: 10.1016/j.ygyno.2007.08.098. [DOI] [PubMed] [Google Scholar]
- 21.Mishra N, Reilly CM, Brown DR, Ruiz P, Gilkeson GS. Histone deacetylase inhibitors modulate renal disease in the MRL-lpr/lpr mouse. J Clin Invest. 2003;111:539–552. doi: 10.1172/JCI16153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reilly CM, Mishra N, Miller JM, et al. Modulation of renal disease in MRL/lpr mice by suberoylanilide hydroxamic acid. J Immunol. 2004;173:4171–4178. doi: 10.4049/jimmunol.173.6.4171. [DOI] [PubMed] [Google Scholar]
- 23.Roychowdhury S, Baiocchi RA, Vourganti S, et al. Selective efficacy of depsipeptide in a xenograft model of Epstein-Barr virus-positive lymphoproliferative disorder. J Natl Cancer Inst. 2004;96:1447–1457. doi: 10.1093/jnci/djh271. [DOI] [PubMed] [Google Scholar]
- 24.Vinodhkumar R, Song YS, Devaki T. Romidepsin (depsipeptide) induced cell cycle arrest, apoptosis and histone hyperacetylation in lung carcinoma cells (A549) are associated with increase in p21 and hypophosphorylated retinoblastoma proteins expression. Biomed Pharmacother. 2008;62:85–93. doi: 10.1016/j.biopha.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Sato N, Ohta T, Kitagawa H, et al. FR901228, a novel histone deacetylase inhibitor, induces cell cycle arrest and subsequent apoptosis in refractory human pancreatic cancer cells. Int J Oncol. 2004;24:679–685. [PubMed] [Google Scholar]
- 26.Doi S, Soda H, Oka M, et al. The histone deacetylase inhibitor FR901228 induces caspase-dependent apoptosis via the mitochondrial pathway in small cell lung cancer cells. Mol Cancer Ther. 2004;3:1397–1402. [PubMed] [Google Scholar]
- 27.Kobayashi Y, Ohtsuki M, Murakami T, et al. Histone deacetylase inhibitor FK228 suppresses the Ras-MAP kinase signaling pathway by upregulating Rap1 and induces apoptosis in malignant melanoma. Oncogene. 2006;25:512–524. doi: 10.1038/sj.onc.1209072. [DOI] [PubMed] [Google Scholar]
- 28.Hoshino I, Matsubara H, Hanari N, et al. Histone deacetylase inhibitor FK228 activates tumor suppressor Prdx1 with apoptosis induction in esophageal cancer cells. Clin Cancer Res. 2005;11:7945–7952. doi: 10.1158/1078-0432.CCR-05-0840. [DOI] [PubMed] [Google Scholar]
- 29.Angelucci A, Valentini A, Millimaggi D, et al. Valproic acid induces apoptosis in prostate carcinoma cell lines by activation of multiple death pathways. Anticancer Drugs. 2006;17:1141–1150. doi: 10.1097/01.cad.0000236302.89843.fc. [DOI] [PubMed] [Google Scholar]
- 30.Bokelmann I, Mahlknecht U. Valproic acid sensitizes chronic lymphocytic leukemia cells to apoptosis and restores the balance between pro- and antiapoptotic proteins. Mol Med. 2008;14:20–27. doi: 10.2119/2007-00084.Bokelmann. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Catalano MG, Poli R, Pugliese M, Fortunati N, Boccuzzi G. Valproic acid enhances tubulin acetylation and apoptotic activity of paclitaxel on anaplastic thyroid cancer cell lines. Endocr Relat Cancer. 2007;14:839–845. doi: 10.1677/ERC-07-0096. [DOI] [PubMed] [Google Scholar]
- 32.Dragunow M, Greenwood JM, Cameron RE, et al. Valproic acid induces caspase 3-mediated apoptosis in microglial cells. Neuroscience. 2006;140:1149–1156. doi: 10.1016/j.neuroscience.2006.02.065. [DOI] [PubMed] [Google Scholar]
- 33.Lagneaux L, Gillet N, Stamatopoulos B, et al. Valproic acid induces apoptosis in chronic lymphocytic leukemia cells through activation of the death receptor pathway and potentiates TRAIL response. Exp Hematol. 2007;35:1527–1537. doi: 10.1016/j.exphem.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 34.Li XN, Shu Q, Su JM, Perlaky L, Blaney SM, Lau CC. Valproic acid induces growth arrest, apoptosis, and senescence in medulloblastomas by increasing histone hyperacetylation and regulating expression of p21Cip1, CDK4, and CMYC. Mol Cancer Ther. 2005;4:1912–1922. doi: 10.1158/1535-7163.MCT-05-0184. [DOI] [PubMed] [Google Scholar]
- 35.Shen WT, Wong TS, Chung WY, et al. Valproic acid inhibits growth, induces apoptosis, and modulates apoptosis-regulatory and differentiation gene expression in human thyroid cancer cells. Surgery. 2005;138:979–984. doi: 10.1016/j.surg.2005.09.019. discussion 984–975. [DOI] [PubMed] [Google Scholar]
- 36.Morland C, Boldingh KA, Iversen EG, Hassel B. Valproate is neuroprotective against malonate toxicity in rat striatum: an association with augmentation of high-affinity glutamate uptake. J Cereb Blood Flow Metab. 2004;24:1226–1234. doi: 10.1097/01.WCB.0000138666.25305.A7. [DOI] [PubMed] [Google Scholar]
- 37.Jeong MR, Hashimoto R, Senatorov VV, et al. Valproic acid, a mood stabilizer and anticonvulsant, protects rat cerebral cortical neurons from spontaneous cell death: a role of histone deacetylase inhibition. FEBS Lett. 2003;542:74–78. doi: 10.1016/s0014-5793(03)00350-8. [DOI] [PubMed] [Google Scholar]
- 38.Sinn DI, Kim SJ, Chu K, et al. Valproic acid-mediated neuroprotection in intracerebral hemorrhage via histone deacetylase inhibition and transcriptional activation. Neurobiol Dis. 2007;26:464–472. doi: 10.1016/j.nbd.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 39.Pan T, Li X, Xie W, Jankovic J, Le W. Valproic acid-mediated Hsp70 induction and anti-apoptotic neuroprotection in SH-SY5Y cells. FEBS Lett. 2005;579:6716–6720. doi: 10.1016/j.febslet.2005.10.067. [DOI] [PubMed] [Google Scholar]
- 40.Kawagoe R, Kawagoe H, Sano K. Valproic acid induces apoptosis in human leukemia cells by stimulating both caspase-dependent and -independent apoptotic signaling pathways. Leuk Res. 2002;26:495–502. doi: 10.1016/s0145-2126(01)00151-5. [DOI] [PubMed] [Google Scholar]
- 41.Schwartz C, Palissot V, Aouali N, et al. Valproic acid induces non-apoptotic cell death mechanisms in multiple myeloma cell lines. Int J Oncol. 2007;30:573–582. [PubMed] [Google Scholar]
- 42.Atmaca A, Al-Batran SE, Maurer A, et al. Valproic acid (VPA) in patients with refractory advanced cancer: a dose escalating phase I clinical trial. Br J Cancer. 2007;97:177–182. doi: 10.1038/sj.bjc.6603851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stockhausen MT, Sjolund J, Manetopoulos C, Axelson H. Effects of the histone deacetylase inhibitor valproic acid on Notch signalling in human neuroblastoma cells. Br J Cancer. 2005;92:751–759. doi: 10.1038/sj.bjc.6602309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Takai N, Desmond JC, Kumagai T, et al. Histone deacetylase inhibitors have a profound antigrowth activity in endometrial cancer cells. Clin Cancer Res. 2004;10:1141–1149. doi: 10.1158/1078-0432.ccr-03-0100. [DOI] [PubMed] [Google Scholar]
- 45.Garcia BA, Busby SA, Shabanowitz J, Hunt DF, Mishra N. Resetting the epigenetic histone code in the MRL-lpr/lpr mouse model of lupus by histone deacetylase inhibition. J Proteome Res. 2005;4:2032–2042. doi: 10.1021/pr050188r. [DOI] [PubMed] [Google Scholar]