Abstract
Objective
Although prior research has demonstrated that frequent placement changes can negatively impact outcomes of children in foster care, it is equally possible that a child's baseline attributes may impact both their capacity to achieve placement stability and their subsequent well-being. The goal of this study was to disentangle the effect of a child's baseline problems at entry into foster care on subsequent placement stability and behavioral outcomes in order to separate out the direct impact of placement stability on behavioral problems of children in foster care.
Design/Methods
Using a sample of 729 children who entered continuous foster care in the National Survey of Child & Adolescent Well-Being (NSCAW), placement stability over the first 18 months in out-of-home placement was categorized as: early stability (permanency or stable placement within 45 days); late stability (permanency or stable placement beyond 45 days); and unstable (never achieving permanency or stability). A propensity score predicting a child's likelihood of placement instability based on their baseline attributes was divided into categories identifying each child as low, medium, or high-risk for placement instability. These risk categories were then added to a logistic regression model to examine the independent association between placement stability and behavioral well-being using the Child Behavioral Checklist (CBCL) and Temperament Scores from the National Longitudinal Survey of Youth.
Results
Weighted analyses revealed that half (52%) of the children achieved early stability; 19% achieved later stability; and 28% remained unstable. Early stabilizers were more likely to be young (p=0.02), have normal baseline behavior (p=0.07), have no prior history with Child Protective Services (p=0.03), and have birth parents that did not have serious mental or behavioral problems (p=0.09). After accounting for baseline attributes, stability remained an important predictor of well-being at 18 months. Children with unstable placements were more likely to have behavior problems than children who achieved early stability across every level of risk for instability. Among the low risk group, the probability of behavioral problems among early stabilizers was 22%, compared to 36% among unstable children, showing a 63% increase in behavior problems due to instability alone. (p<0.05)
Conclusions
Children in foster care experience placement instability unrelated to their baseline problems, and this instability has a significant impact on their behavioral well-being. This finding presents an opportunity for intervention to improve both placement stability and outcomes among youth entering care.
Responding to evidence that children were languishing in foster care, the Adoption and Safe Families Act of 1997 (ASFA, Public Law 105−89) marked a turning point in child welfare policy, making permanency and adoption as important a priority for children in foster care as the traditional mission of ensuring safety and security for these children. However, despite this renewed focus on permanency and the resulting increase in adoptions since 1997, 1 nearly half of children continue to reside in foster care for more than 18 months, and many, for years.2 The experience for many of these children is often one of instability, as 1 in 3 will fail to achieve a long-lasting placement and may experience frequent placement moves and transfers to restrictive settings like group homes and residential treatment facilities that have been traditionally associated with poor outcomes 3.
Research over the last two decades has demonstrated a strong association between frequent placement moves in foster care and poor outcomes 4-7 This research inevitably suggests an opportunity for the child welfare system to improve well-being outcomes by prioritizing those services and interventions that seek to facilitate permanent long-lasting placements. However, this inference assumes that decisions of caseworkers or services received by children and their families are the primary factors that influence placement stability and later outcomes. Such an inference fails to consider the possibility that many of these children are unable to achieve such stability due to their attributes upon entering care. It may therefore be problematic to assume that improving efficiency in the way placement decisions are made or in the services offered to families would impact a population where half of the children already have serious behavioral and mental health problems upon entering care.8-15
For this reason, determining whether placement stability influences outcomes irrespective of a child's baseline attributes and problems may inform whether the child welfare system, by improving its own efficiency in supervising placement decisions, might be able to improve outcomes for many of its children. However, to date, disentangling the cascading relationship between a child's problems and their subsequent placement stability has been a challenge for investigators, and has rarely been reported in the literature.16 Our group recently described the placement stability of a group of children from the National Survey of Child & Adolescent Well-Being (NSCAW), and found that a child's behavioral problems at entry into foster care could not entirely explain the risk of behavioral problems 3 years downstream. Children without behavioral problems at baseline who either reunified home or did not achieve any stability were twice as likely to have behavioral problems at 36 months compared to children who achieved early stability (defined as a long-lasting placement within 45 days of entry into foster care).17
Although provocative, this prior study was purely descriptive and did not capture all attributes in a child's maltreatment history, health, and birth parents’ characteristics that might influence their likelihood of placement stability and poor outcomes downstream. The current study attempts to explain the relationship between a child's well being and placement history by applying a propensity score analysis on a cohort of children continuously in foster care from the National Survey of Child & Adolescent Well-Being (NSCAW). The goal was to identify the innate contribution of a child's placement stability toward their risk for behavioral problems 18 months after entering foster care.
Methods
NSCAW was the primary data source for this analysis, a nationally representative prospective cohort study whose primary aim was to study the health and well-being of children reported to child welfare over a 3-year follow-up period. The study included children who were recruited after a maltreatment report to child welfare from October 1999 - December 2000. Observations were collected through interviews with children, teachers, caregivers, caseworkers, and biological parents at baseline, 12 months, 18 months, and 36 months after enrollment.
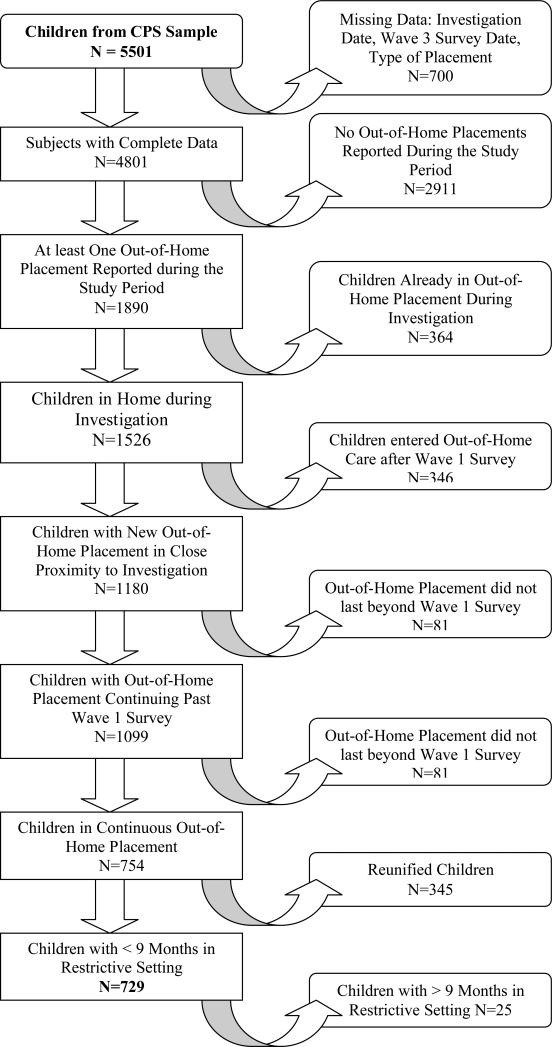
From the original 5,501 children, we restricted our sample to those children residing at home during the initial investigation for maltreatment and who were subsequently placed into out-of-home care, which continually lasted for at least 18 months (see Figure 1). We also excluded subjects with missing data and the small minority of children who spent more than 9 months in a group home or residential treatment facility, as their stability in a restrictive setting might have biased our findings toward the null hypothesis. Finally, we chose to include only children continuously in out-of-home care because potential interventions with regard to placement stability would by definition impact this group the most, as opposed to those children whose family service plans carried a high probability of reunification home.
Figure 1.
Study population derived from the National Survey of Child and Adolescent Well-Being
The primary exposure variable for this study was the child's placement stability over the first 18 months in out-of-home care. We adapted the methodology of James and colleagues in San Diego3 to identify three distinct levels of stability for children entering out-of-home care. Early stability was defined as those children who achieved a long-lasting placement within 45 days of entry into out-of-home care, which was maintained for the period of observation. Children with late stability achieved a long-lasting placement, but only after 45 days. And unstable children failed to achieve a long-lasting placement that was maintained for at least 9 months until the end of the observation period.
The primary outcome for the study was the child's behavioral well-being after 18 months in out-of-home care. We created a composite behavioral well-being variable constructed from two behavioral assessment tools: the Child Behavior Checklist (CBCL) for children aged two and older, and temperament scores for infants under two. Combining both tools allowed us to include a population of children from birth until 15 years of age.
The CBCL is an often-used measure of known reliability and validity, 18 and was administered to children two years of age and older at baseline and again after 18 months. Individual questions are rated using a 3-point Likert scale, in which the caregiver is asked about the frequency of a behavioral problem (“not or never true”, “somewhat or sometimes true”, and “very or often true”). The scores on individual items are then summed in a total behavioral problems scale, which are normed by age to identify standardized categories of normal, borderline (>83rd percentile), and clinical range (>90th percentile) for referral for mental health treatment. For our study, we used these normed cut-points to dichotomize our outcome variable as normal behavior vs. borderline or clinically important abnormal behavior for children over two years of age.
For children under two years of age, we included temperament scores that were developed originally for the National Longitudinal Survey of Youth (NLSY) that combined elements from Rothbart's Infant Behavior Questionnaire and Campos and Kagan's Compliance Scale.19 The temperament scores are designed to assess temperament or behavior style in infants, and although they include several domains, we restricted our analyses to the negative hedonic domain for children under one year, and the difficult/negative hedonic domain for children between 1 and 2 years of age (both asked the same questions). These domains measured possible early behavioral problems that at baseline would have rendered the child at greater risk for placement instability. Typical questions in these domains include whether the child cries around strangers, gets upset when the primary caregiver leaves, or has trouble self-soothing. Items are summed using a 5-point Likert scale for each question (Never/Almost Never to Almost Always). Individual items are totaled to report a continuous raw score, the higher of which indicates the likelihood of later behavioral problems.
The composite behavioral well-being outcome variable ultimately combined the dichotomized CBCL scores on the older children with a dichotomized variable of the infant temperament scores. The cut-point of the temperament scores was chosen as one standard deviation from the mean as determined on the sample of children included in the NLSY from 1992 (the most generalizable sample on which these scores have been applied).19 Our team felt comfortable combining the temperament and CBCL scores because prior data had suggested that temperament scores are highly correlated with behavior in older children, and preliminary analyses with our data (not shown) confirmed this to be true.19 A similar methodology was also used to encode the child's baseline behavioral well-being, likely the most important baseline attribute that might have confounded the relationship between placement stability and subsequent well-being.
Covariates included a broad array of child, birth parent and maltreatment history characteristics that are potentially important determinants of whether a child would experience placement instability and poor well-being downstream. Child-level factors included the child's age (categorized as 0−1, 2−10, and 11−15 years), race (White non-Hispanic, Black, Hispanic, Other), sex, history of chronic medical problems (yes/no), and baseline behavioral well-being (as noted above, dichotomized as normal vs. abnormal). Birth parent characteristics included a history of mental health problems, drug or alcohol use, history of domestic violence or arrests. Child maltreatment characteristics included the type of maltreatment (physical abuse, sexual abuse, or neglect/abandonment) or whether the child had a prior history of investigations, substantiated reports or out-of-home care.
Because of the unequal probabilities of selection in the stratified, clustered design elements in the NSCAW data, weighted frequencies are reported to generalize the findings to a nationally representative group of children entering out-of-home care. Due to the great variability of the design weights (range 1−6908), we trimmed the design weights above the 95th percentile.20 Separate analyses (not provided) revealed that trimming the weights at the 95th percentile had minimal effect on point estimates for unadjusted associations but reduced the variance of estimates by a factor of 2. Additional trimming did not reduce variance substantially to warrant further adjustment of the weights for analyses.
To adjust for the baseline characteristics that may have confounded the relationship between placement stability and well-being, we used a propensity score analysis in which characteristics of the child, birth parent, and maltreatment history were entered into an ordinal logistic regression model that predicted the likelihood of placement instability. Factors that were significant in bivariate chi-square analyses (p<0.2) were added to the multivariate model. Because we were not concerned with over-fitting the propensity score model, we expanded the baseline score of the CBCL and temperament scores to quartiles. Age was interacted with the child's baseline well-being score to account for the differences in interpretation of the scores and type of measure across age. After fitting the model, a post-estimation probability of placement stability was calculated for each child, and these probabilities were then divided into tertiled categories that expressed the likelihood of placement instability for each child (low, medium, or high). Further model diagnostics confirmed that the propensity score tertiles balanced the covariates in the model as intended.
The propensity score categories (or from here forward, the risk categories for placement instability) were subsequently added as a covariate to a logistic regression model predicting the likelihood of behavioral problems at 18 months as a function of a child's placement stability. After constructing the model, we used conditional standardization 21 to estimate the probability of behavioral problems (with 95% confidence intervals) for children in each level of risk for instability and by the stability they actually achieved.
All analyses were conducted using STATA 9.0 software (STATA Corporation, College Station, Texas). The study was approved by the National Data Archive for Child Abuse & Neglect, and the institutional review board at The Children's Hospital of Philadelphia.
Results
From the population of 5,501 children in the NSCAW CPS sample, 729 children remained in continuous foster care throughout the 18-month follow up period and spent no more than 9 months in a restricted residential setting. Of these children in our study population, 38% were under 2 years, 41% were between 2 and 10 years, and 22% were 11 years and older. More than half of the children were female (57%) and the vast majority of children were either Caucasian (44%) or African American (38%) with the remaining children of Hispanic (13%) or Other (6%) origin. At the time of entry into this study, 12% of children under 2 years old had abnormal temperament scores, and almost half (46%) of children older than 2 years had abnormal CBCL scores. This resulted in 33% of the overall study population having abnormal behavior scores, as well as roughly half (45%) of the total population reporting some health problem at baseline.
Most children entering foster care at the beginning of this study either suffered physical abuse (40%) or were neglected or abandoned by their caregiver (37%), while 7% of children were sexually abused and 15% suffered some other type of abuse. Overall, 66% of all children had some prior history with child protective services, and more than half reported a biological caregiver with either serious mental or behavioral problems (54%), a history of domestic violence or arrests (58%), or problems with either drugs or alcohol (53%).
The unadjusted association between a child's baseline attributes and placement stability at 18 months appears in Table 1. After 18 months in foster care, 52% of children achieved early stability, 19% achieved late stability and 28% remained unstable. Early stabilizers were more likely to be young (p=0.02), have normal baseline behavior (p=0.07), have no prior history with Child Protective Services (p=0.03), and have birth parents that did not have serious mental or behavioral problems (p=0.09).
Table 1.
Unadjusted association between a child's baseline attributes and placement stability at 18 months.
| Early Stability | Late Stability | Unstable | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | % | (n) | % | (n) | % | (n) | F Stat | p-value | |
| 52.2 | (354) | 19.4 | (164) | 28.4 | (211) | ||||
|
Demographics | |||||||||
| < 2 years | 57.2 | (184) | 18.8 | (89) | 24.1 | (76) | 3.1 | 0.02 | |
| Child's Age | 2 − 10 years | 58.0 | (130) | 16.7 | (47) | 25.4 | (76) | ||
| |
> 10 years |
34.8 |
(40) |
23.1 |
(27) |
42.2 |
(59) |
|
|
| Sex of Child |
Female | 53.1 | (201) | 19.9 | (91) | 27.0 | (101) | 0.2 | 0.82 |
| Male |
51.0 |
(153) |
18.7 |
(73) |
30.3 |
(110) |
|
|
|
| White (Non-Hispanic) | 51.4 | (130) | 18.9 | (65) | 29.7 | (77) | 0.6 | 0.72 | |
| Race and Ethnicity of Child | Black | 55.6 | (154) | 18.6 | (71) | 25.8 | (81) | ||
| Hispanic | 44.6 | (48) | 26.6 | (18) | 28.8 | (31) | |||
| Other | 48.7 | (20) | 15.4 | (9) | 35.9 | (19) | |||
|
Child Health | |||||||||
| Child's Baseline Behavior |
Normal | 56.6 | (267) | 18.7 | (114) | 24.7 | (130) | 2.7 | 0.07 |
| Abnormal |
44.8 |
(85) |
21.5 |
(50) |
33.8 |
(76) |
|
|
|
| Any Child Health Problems at Baseline | Yes | 49.8 | (161) | 19.3 | (89) | 30.9 | (103) | 0.4 | 0.64 |
| No | 54.2 | (193) | 19.4 | (75) | 26.3 | (108) | |||
|
Abuse/Maltreatment History | |||||||||
| Neglect or abandonment | 44.7 | (99) | 23.8 | (48) | 31.5 | (70) | 1.1 | 0.35 | |
| Type of Abuse Reported | Physical | 58.4 | (157) | 15.3 | (67) | 26.3 | (82) | ||
| Sexual | 41.5 | (21) | 18.5 | (11) | 40.1 | (20) | |||
| |
Other |
55.1 |
(44) |
19.4 |
(19) |
25.5 |
(19) |
|
|
| Any History of CPS Involvement | Yes | 47.6 | (220) | 19.3 | (107) | 33.1 | (156) | 3.5 | 0.03 |
| No | 61.2 | (134) | 19.5 | (57) | 19.3 | (156) | |||
|
Birth Parent Characteristics | |||||||||
| Caregiver Has Serious Mental / Behavioral Problems |
Yes | 47.5 | (195) | 19.8 | (87) | 32.8 | (132) | 2.4 | 0.09 |
| No |
57.7 |
(159) |
18.9 |
(77) |
23.4 |
(79) |
|
|
|
| Caregiver History of Domestic Violence or Arrests |
Yes | 51.7 | (204) | 18.9 | (93) | 29.5 | (116) | 0.15 | 0.86 |
| No |
53.0 |
(150) |
20.1 |
(71) |
26.9 |
(95) |
|
|
|
| Caregiver Problems with Drugs or Alcohol | Yes | 54.3 | (196) | 17.2 | (95) | 28.5 | (106) | 0.7 | 0.50 |
| No | 50.0 | (158) | 21.7 | (69) | 28.3 | (105) | |||
The unadjusted association between a child's baseline attributes and behavioral well-being outcomes at 18 months appears in Table 2. After the follow up period, 38% of children measured abnormal on the composite well-being measure, compared to 33% at baseline. As expected, the greatest predictor of a child's behavioral outcome at 18 months was their assessment of behavioral problems at baseline (p<0.001). Placement stability was also an important predictor of behavioral outcomes in these unadjusted analyses; 31% of children who achieved early stability, 38% of late stability and 51% of unstable children had abnormal behavioral outcomes after 18 months (P=0.004).
Table 2.
Unadjusted association between a child's baseline attributes and behavioral well-being outcomes at 18 months.
| Normal | Abnormal | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | % | (n) | % | (n) | F Stat | p-value | |
| 62.4 | (425) | 37.6 | (264) | ||||
|
Demographics | |||||||
| < 2 years | 73.3 | (254) | 26.7 | (85) | 3.7 | 0.03 | |
| Child's Age | 2−10 years | 56.9 | (123) | 43.1 | (115) | ||
| |
> 10 years |
52.8 |
(48) |
47.2 |
(64) |
|
|
| Sex of Child |
Female | 64.8 | (230) | 35.2 | (144) | 1.2 | 0.28 |
| Male |
59.3 |
(195) |
40.7 |
(120) |
|
|
|
| White (Non-Hispanic) | 61.5 | (152) | 38.5 | (105) | 0.3 | 0.84 | |
| Race and Ethnicity of Child | Black | 63.0 | (179) | 37.0 | (114) | ||
| Hispanic | 68.6 | (65) | 31.4 | (25) | |||
| Other | 64.3 | (28) | 35.8 | (15) | |||
|
Child Health | |||||||
| Child's Baseline Behavior |
Normal | 73.6 | (357) | 26.4 | (129) | 28.8 | <0.0001 |
| Abnormal |
40.0 |
(67) |
60.0 |
(131) |
|
|
|
| Any Child Health Problems at Baseline | Yes | 56.5 | (190) | 43.5 | (141) | 3.4 | 0.07 |
| No | 67.2 | (235) | 32.8 | (123) | |||
|
Abuse/Maltreatment History | |||||||
| Neglect or abandonment | 61.6 | (125) | 38.4 | (81) | 0.0 | 0.99 | |
| Type of Abuse Reported | Physical | 61.7 | (184) | 38.3 | (109) | ||
| Sexual | 59.3 | (19) | 40.7 | (27) | |||
| |
Other |
62.4 |
(49) |
37.6 |
(28) |
|
|
| Any History of CPS Involvement | Yes | 58.3 | (261) | 41.7 | (192) | 4.4 | 0.04 |
| No | 70.1 | (164) | 29.9 | (72) | |||
|
Birth Parent Characteristics | |||||||
| Caregiver Has Serious Mental / Behavioral Problems |
Yes | 58.6 | (223) | 41.4 | (165) | 2.1 | 0.16 |
| No |
66.8 |
(202) |
33.2 |
(99) |
|
|
|
| Caregiver History of Domestic Violence or Arrests |
Yes | 61.7 | (245) | 38.3 | (145) | 0.1 | 0.74 |
| No |
63.4 |
(180) |
36.6 |
(119) |
|
|
|
| Caregiver Problems with Drugs or Alcohol | Yes | 69.1 | (249) | 30.9 | (124) | 5.3 | 0.02 |
| No | 55.0 | (176) | 45.0 | (140) | |||
Notwithstanding the importance of a child's baseline behavior toward future well-being, other attributes also appeared in unadjusted analysis to be associated with the child's behavioral outcome at 18 months. Children with good behavioral outcomes tended to be younger (p=0.03), have no history of health problems (p=0.07), and no prior history with Child Protective Services (p=0.04). Children with better outcomes were also less likely to have a biological parent with a serious mental or behavioral problem (p=0.16), but interestingly more likely to have a biological parent who had a problem with drugs or alcohol (p=0.02).
Each of the factors associated with placement stability and/or well-being were considered in the propensity score analysis that determined the risk groups for placement instability. Factors that were no longer significant in the multivariate model and did not change the estimates for key factors of interest were dropped to create the most parsimonious model. After estimating the predicted probability of placement instability for each child, the children were divided into tertiles to describe low, medium and high levels of baseline risk for placement instability; 37% of children were in the low risk group, 30% in the medium risk group and 33% in the high risk group. Sixty-three percent of the low-risk children and 56% of the medium risk children achieved early stability, compared with only 39% of the high-risk children. At the same time, 38% of the high-risk children had unstable histories, compared to 20% and 26% among the low and medium risk groups respectively.
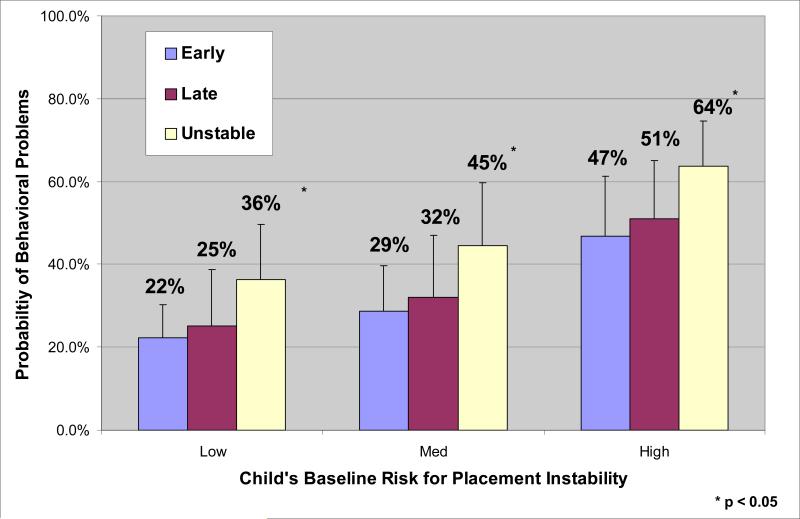
The predicted probabilities of behavioral problems at 18 months, derived from the final multivariate model that included the risk group for instability and each child's observed stability, appear in Figure 2. Children with unstable placements had twice the odds of having behavior problems as children who achieved early stability at every level of risk for instability (OR=1.99, 95% CI [1.13, 3.50]). Among the low risk group, the probability of behavioral problems among early stabilizers was 22%, compared to 36% among unstable children, showing a 63% increase in behavior problems due to instability. Among the high-risk group, behavioral problems were much more likely across all levels of stability and there remained a large increase in predicted behavioral problems among unstable children. Children who achieved early stability had a probability of behavioral problems of 47%, while 64% of unstable high-risk children were estimated to have behavior problems, indicating a 36% increase in behavior problems due to instability.
Figure 2.
Probability of Behavioral Problems at 18 Months, by Child's Placement Stability & Baseline Risk for Problems
Discussion
The current study provides the most compelling evidence to date that placement stability, independent of a child's problems at entry into care, can influence well-being for children in out-of-home care. Regardless of a child's baseline risk for instability in this study, those children who failed to achieve placement stability were estimated to have a 36%−63% increased risk of behavioral problems compared with children who achieved any stability in foster care. The impact of placement stability on behavioral problems was not trivial, as even among the children who carried a low risk for placement instability, 1 in 5 children (20%) failed to achieve any stability in the first 18 months of foster care.
That nearly 1 in 3 children overall failed to achieve any placement stability reveals that across the nation, there is likely to be ample opportunity to influence rates of placement stability at the local level. Prior data from one county that contributed data to NSCAW has also revealed that 70% of all placement moves in that county were administrative in nature and seemingly unrelated to the behavior of the child.22 Many of these moves involved a change in caseworker, agency, or an adjudicated decision made irrespective of the child's attachment within a foster home. While it is clear that not all placement moves were preventable, the magnitude of administrative moves, a topic receiving little attention in the literature, presents a considerable opportunity to improve stability by applying best practice to administrative decision making.
Interventions to improve placement stability and downstream outcomes have been relatively unstudied, but the number of opportunities for intervention is likely to be many. For the pediatric community that is often on the sidelines of children moving in and out of foster care, these results should encourage practitioners to take a greater involvement in helping children in foster care to access services, in supporting foster parents in managing child behavior issues, and in working with the child welfare system to consider alternatives to placement change or strategies to prevent them. Indeed, the responsibility for intervention does not belong to the child welfare system alone, as the interaction with the health care system and the timeliness in which children receive preventative services, particularly mental health, has continued to be a problem.23, 24
Nevertheless, over the past decade, many states, in response to the Adoption and Safe Families Act and the Child Family Service Reviews (CFSR) that began in the year 2000, have increasingly devoted resources toward managing health and related services for children in the child welfare system. The result has been an increasing number of “joint ventures” and cross-sector partnerships with health care agencies to promote service integration and improve accessibility and quality of care. In many systems, behavioral health workers have joined child welfare units to screen children upon entry into care to identify at-risk children as soon as possible, a solution long recommended by the American Academy of Pediatrics, the Child Welfare League of America, and the American Academy of Child & Adolescent Psychiatry.24-28
Independent of the management of health resources, child welfare systems have other opportunities to improve the practice by which their placement decisions are made and to increase the resources they devote toward stabilizing children in placement. For example, since 2002, the City of Philadelphia, Pennsylvania and it's contracted foster care agencies began implementing performance-based contracts for children entering general foster care and kinship care. Performance incentives focusing on well-being were embedded in agency contracts providing a clear incentive for agencies to ensure permanent homes for children, to universally screen all children coming into care, and to restrict caseloads moving between agencies. As of 2005, after the permanency and stability expectations placed on provider agencies rose, the rate at which children achieved permanency through reunification, adoption or permanent legal custody increased by 84%. In addition, movement of children to higher levels of placement or to other foster care agencies decreased by 50% (by communication with Cheryl Ransom Garner, Commissioner of the Department of Human Services for the city of Philadelphia, Pennsylvania). These data are promising and demand further research to determine the impact on well-being outcomes downstream.
There are important limitations to consider when interpreting our findings. While the placement stability variable we used better accounted for the qualitative experience of children in foster care, it certainly could not be inclusive of all the types of experiences children have, including, for example, whether children were placed with kin or non-relatives in out-of-home care. Future work will need to consider how type of placement a child has interacts with placement stability in predicting future well-being. It is also certainly possible that we are over-representing the impact of placement stability on well-being, because of the inability to detect all risk factors at the family level or other misclassification at baseline. However, to the degree that misclassification also impacted our outcome variable, we instead could have biased ourselves toward the null hypothesis of no association, making our findings all the more striking. In addition, these findings may have limited generalizability at the local level, so that local child welfare systems will need to to conduct their own analyses to better understand the needs of children in their care and consider opportunities for intervention.
These limitations aside, our data are nevertheless compelling and provide a starting point for discussion of a more integrated approach to improving the stability and permanency of placements for children within the child welfare system. By demonstrating that nearly half of children entering out-of-home care have serious behavioral problems, our study joins a chorus of prior studies that have demonstrated that the majority of children in out-of-home care have serious behavioral problems. However, our study departs from those prior studies in highlighting that placement experience is a significant contributor to a child's risk for behavioral problems unrelated to the baseline problems a child had upon referral for placement. Future studies will need to address the multiple aspects of a child's well-being and measure other outcomes over longer periods of observation to determine if improvements in permanency and adoption truly beget long-standing benefits to children. However, with renewed focus on permanency for children in out-of-home care, placement stability is already emerging as an important measure of process for the child welfare system. This will undoubtedly lead to new interventions to improve stability for children, and the future will hold whether such interventions can improve the lives of some of our most vulnerable children.
References
- 1.Wulczyn FH, Brunner K, Chen L. Adoption Dynamics: The impact of the Adoption and Safe Families Act. 2004 Chapin Hall Center for Children at the University of Chicago: updated version of http://aspe.hhs.gov/hsp/fostercare-issues02/ASFA/index.htm.
- 2.Adoption and Foster Care Analysis and Reporting System 2005 U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children's Bureau, www.acf.hhs.gov/programs/cb. [PubMed]
- 3.James S, Landsverk JA, Slymen DJ. Placement movement in out-of-home care: patterns and predictors. Children & Youth Services Review. 2004;26(2):185–206. [Google Scholar]
- 4.Pecora P, Kessler R, Williams J, et al. Improving family foster care: findings from the Northwest Foster Care Alumni Study. Seattle, WA: 2005. Casey Family Programs, available at http://www.casey.org. [Google Scholar]
- 5.Taussig HN. Children who return home from foster care: a 6-year prospective study of behavioral health outcomes in adolescence. Pediatrics. 2001;108(1):E10. doi: 10.1542/peds.108.1.e10. [DOI] [PubMed] [Google Scholar]
- 6.Jonson-Reid M, Barth R. From maltreatment to juvenile incarceration: uncovering the role of child welfare services. Child Abuse & Neglect. 2000;24(4):505–520. doi: 10.1016/s0145-2134(00)00107-1. [DOI] [PubMed] [Google Scholar]
- 7.Barth RP, Jonson-Reid M. Outcomes after child welfare services: Implications for the design of performance measures. Children & Youth Services Review. 2000;22(9−10):763–787. [Google Scholar]
- 8.Simms MD. The foster care clinic: a community program to identify treatment needs of children in foster care. Journal of Developmental & Behavioral Pediatrics. 1989;10(3):121–128. [PubMed] [Google Scholar]
- 9.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000;106(4 Suppl):909–918. [PubMed] [Google Scholar]
- 10.Rosenfeld AA, Pilowsky DJ, Fine P, et al. Foster care: an update. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):448–457. doi: 10.1097/00004583-199704000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Halfon N, Mendonca A, Berkowitz G. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Archives of Pediatrics & Adolescent Medicine. 1995;149(4):386–392. doi: 10.1001/archpedi.1995.02170160040006. [DOI] [PubMed] [Google Scholar]
- 12.Chernoff R, Combs-Orme T, Risley-Curtiss C, Heisler A. Assessing the health status of children entering foster care. Pediatrics. 1994;93(4):594–601. [PubMed] [Google Scholar]
- 13.Landsverk JA, Garland AF, Leslie LK. Mental health services for children reported to child protective services. Vol. 2. Sage Publications; 2002. Thousand Oaks. [Google Scholar]
- 14.Trupin EW, Tarico VS, Low BP, Jemelka R, McClellan J. Children on child protective service caseloads: Prevalence and nature of serious emotional disturbance. Child Abuse & Neglect. 1993;17(3):345–355. doi: 10.1016/0145-2134(93)90057-c. [DOI] [PubMed] [Google Scholar]
- 15.Clausen JM, Landsverk J, Ganger W, Chadwick D, Litrownik A. Mental health problems of children in foster care. Journal of Child & Family Studies. 1998;7(3):283–296. [Google Scholar]
- 16.Newton RR, Litrownik AJ, Landsverk JA. Children and youth in foster care: distangling the relationship between problem behaviors and number of placements. Child Abuse & Neglect. 2000;24(10):1363–1374. doi: 10.1016/s0145-2134(00)00189-7. [DOI] [PubMed] [Google Scholar]
- 17.Rubin DM, Hafner L, Luan X, Localio AR. Placement stability and early behavioral outcomes for children in out-of-home care.. Paper presented at: Child Protection: Using Research to Improve Policy and Practice; Washington, DC. 2005. [Google Scholar]
- 18.Achenbach TM. Manual for the Child Behavioral Checklist and 1991 profile. University of Vermont, Dept. of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- 19.Mott F, Baker P, Ball D, Keck C, S L. The NLSY Children 1992. Center for Human Resource Research, Ohio State University; Columbus, Ohio: 1998. [Google Scholar]
- 20.Korn EL, Graubard BI. Analysis of large health surveys. Accounting for the sampling design. Journal of the Royal Statistical Society: Series A (Statistics in Society) 1995;58:263–295. [Google Scholar]
- 21.Flanders W, Rhodes P. Large sample confidence intervals for regression standardized risks, risk ratios, and risk differences. Journal of Chronic Disease. 1987;40:697–704. doi: 10.1016/0021-9681(87)90106-8. [DOI] [PubMed] [Google Scholar]
- 22.James S. Why Do Foster Care Placements Disrupt? An Investigation of Reasons for Placement Change in Foster Care. Social Service Review. 2004;78(4):601–627. [Google Scholar]
- 23.Burns BJ, Phillips SD, Wagner RH, et al. Mental health need and access to mental health services by youths involved with child welfare: a national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- 24.Rubin D, Halfon N, Raghavan R, Rosenbaum S. Protecting children in foster care: why proposed Medicaid cuts harm our nation's most vulnerable youth. Casey Family Programs; Washington, D.C.: 2005. [Google Scholar]
- 25.Committee on Early Childhood A, and Dependent C, American Academy of P Health care of young children in foster care. Pediatrics. 2002;109(3):536–541. doi: 10.1542/peds.109.3.536. [DOI] [PubMed] [Google Scholar]
- 26.Hepburn K, McCarthy J. Making Interagency Initiatives Work for Children and Families in the Child Welfare System. Georgetown University Center for Child & Human Development; Washington, DC: 2003. access at http://gucchd.georgetown.edu/programs/child_welfare_initiative/promising.html. [Google Scholar]
- 27.McCarthy J. Meeting the health care needs of children in the foster care system. Georgetown University; Washington, D.C.: 2002. [Google Scholar]
- 28.McCarthy J, McCullough C. A View from the Child Welfare System. Georgetown University Center for Child & Human Development; Washington, DC: 2003. access at http://gucchd.georgetown.edu/files/products_publications/cw2.pdf. [Google Scholar]
- 29.Rubin DM, Alessandrini EA, Feudtner C, Mandell D, Localio AR, Hadley T. Placement stability and mental health costs for children in foster care. Pediatrics. 2004;113(5):1336–1341. doi: 10.1542/peds.113.5.1336. [DOI] [PubMed] [Google Scholar]
- 30.Halfon N, Berkowitz G, Klee L. Mental health service utilization by children in foster care in California. Pediatrics. 1992;89(6 Pt 2):1238–1244. [PubMed] [Google Scholar]
- 31.Takayama JI, Bergman AB, Connell FA. Children in foster care in the state of Washington. Health care utilization and expenditures. JAMA. 1994;271(23):1850–1855. [PubMed] [Google Scholar]