Abstract
Introduction
Persons living in rural areas tend to have poorer health than do those who live in urban areas. These disparities have been attributed, in part, to lack of access to care. As a proxy measure of access to care, researchers examined the rate of office visits after emergency department (ED) treatment for asthma between rural and urban areas and pediatric and adult patients in Hawaii.
Methods
A retrospective review of five years of insurance claims data was performed on 7064 ED visits for asthma. Demographic information and location and type of visit were analyzed by using logistic regression and survival analysis to examine rural/urban differences.
Results
Patients who had an office visit after their initial ED visit were 10% less likely to have a repeat ED visit within the month. Rural residents were significantly less likely to have both follow-up office and ED visits than were their urban counterparts when adjusted for age, sex, and morbidity. When adult patient statistics were compared with pediatric patient statistics, only the adult patients demonstrated a significant difference in time to followup between rural and urban patients.
Conclusion
Study results confirm that follow-up office visits are associated with a decrease in emergency visit rates and that adult rural residents are less likely to receive follow-up care than are their urban counterparts for a diagnosis of asthma. However, no significant differences were seen between followup for rural and urban children, which implies that access barriers are overcome for this group of rural residents. Further research should address the aspects of access that pertain to adults in rural areas.
Keywords: Rural, Health Disparities, Follow-Up Time, ED Visit, Asthma, Pediatric Differences, Hawaii
Introduction
Persons living in rural areas have higher rates of cancer1 and diabetes2 and mortality from heart attacks than do urban patients.3 In addition, persons in rural communities are more likely to die from accidents4 and suicide5 than are their urban counterparts. One hypothesis to explain these disparate health circumstances is lack of access to healthcare services in rural areas.
Disparities in access in rural areas include barriers associated with transportation and difficulty providing a full range of services.6 Fewer providers and fewer specialists can be found in rural areas than in urban areas,7 use of hospice services is significantly lower in rural communities than in urban areas,8 and more procedures are used in metropolitan hospitals than in rural hospitals.9 Furthermore, rural areas are reported to experience significant delays in emergency care after serious injury.10
One marker of access to health care may be the time it takes for patients to receive office-based follow-up care after an emergency department (ED) visit for an illness that requires routine care. Therefore, we hypothesized that time to followup for an office visit after an ED visit for asthma would be longer in rural areas than in urban areas because of barriers to accessing care, such as lack of providers and distance to providers.
Methods
A retrospective review of health insurance claims data was performed on records from the largest health insurer in the state of Hawaii.
Patients
After organizational and institutional review board approval were obtained, claims data were extracted, for all patients who had an ED visit for asthma (International Classification of Diseases, Ninth Revision code 493) from January 1, 1999, through December 31, 2004. The diagnosis of asthma was chosen because it is a chronic illness for which prompt and continuous medical therapy makes a significant difference in survival and for which follow-up visits after urgent ED visits are a standard of care.11 Inclusion criteria involved having had insurance for 12 months continuously before the ED visit and having an ED visit for asthma. Exclusion criteria included any patients who discontinued the insurance or died within four weeks of the ED visit. Of the patients who met criteria (had been enrolled for 12 months before and four weeks after ED visit), a single ED visit was selected randomly as the visit used for analysis.
Procedure
Demographic data, including age, sex, zip code, type of insurance, date of all ED visits for asthma, date of all office visits for asthma, morbidity index (provided by the insurer on a 1–5 scale based on number of chronic medical conditions), dollars paid for asthma care, and number of visits for asthma diagnoses in the last 12 months (as markers of severity of disease), were recorded for all patients who met the inclusion criteria.
Analysis
Zip codes were classified as urban if the area was considered metropolitan by the US Census.12 With this classification, all islands other than the most populated island of Oahu were considered rural.
Analysis included descriptive statistics, Kaplan-Meyer survival curves, and logistic regression analysis. Kaplan-Meyer survival curves were created to examine the rates of ED visits and office visits after an initial ED visit for asthma. Proportional hazards regression was used to determine relative rates of returning to the ED within 14 days, using office visits as a time-dependent variable. Logistic regression analysis was used to determine the odds ratio (OR) of having an office visit within seven days after an ED visit for asthma. Analyses were adjusted for age, sex, island of residence, calendar year, morbidity, urban or rural residence, costs of office visits in the past year, and number of ED visits in the past year. Logistic regression analyses were also performed for pediatric and adult samples separately.
Results
A total of 7064 patient records matched inclusion criteria. Table 1 summarizes the characteristics of the patients with asthma who visited the ED: 61% (4318) were adults, 63% (4412) resided in Oahu (urban), 54% (3787) were female, 46% (3277) were male, and 23% (1606) had high morbidity levels (levels 4 and 5). The mean (plus or minus standard deviation) age was 32 (±24.0) years. Children averaged 7.4 (±5.0) years of age, and adults averaged 46.4 (±18.3) years.
Table 1.
Demographic characteristics of 7064 patients who visited the emergency department for asthma, 1999–2004, Hawaii
| Characteristic | n | % |
| Age group | ||
| Children | 2746 | 38.9 |
| Adults | 4318 | 61.1 |
| Sex | ||
| Female | 3787 | 53.6 |
| Male | 3277 | 46.4 |
| Island of residence | ||
| Oahu | 4412 | 62.6 |
| Hawaii | 1233 | 17.5 |
| Maui | 531 | 7.5 |
| Kauai | 686 | 4.7 |
| Other | 192 | 2.7 |
| Morbidity level | ||
| 1 (lowest morbidity) | 1882 | 26.9 |
| 2 | 1785 | 25.5 |
| 3 | 1723 | 24.6 |
| 4 | 827 | 11.8 |
| 5 | 779 | 11.1 |
| Health insurance plan | ||
| Private | 4362 | 61.8 |
| Health maintenance organization | 2346 | 33.2 |
| Medicare | 355 | 5.0 |
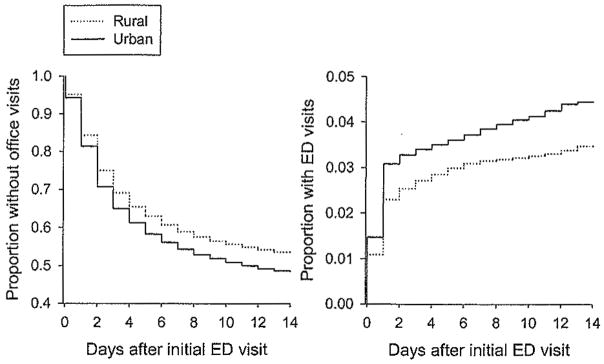
Forty six percent of all patients (3249/7064) had an office visit within two weeks of their ED visit, and 50.2% (1631/3249) of those who had an office visit did so by the second day after ED visit. Four percent of patients returned to the ED within two weeks of their initial visit, and 70.8% (222/314) of those who had a second ED visit in the first two weeks did so by the second day after their initial ED visit (Figure 1). Patients who had an office visit after their initial ED visit were 10% less likely to have a repeat ED visit within the month (rate ratio [RR] .9, 95% confidence interval [CI] .85–.94, P<.001).
Fig 1.
Proportion of patients with second emergency department (ED) visit and follow-up office visits after an initial ED visit for asthma among 7064 patients who visited the ED for asthma, 1999–2004, Hawaii.
Rural residents were significantly less likely to have a follow-up office visit within seven days than were their urban counterparts (OR .85, 95% CI .77–.94, P<.001) when adjusted for age, sex, calendar year, and morbidity (Table 2). Rural residents were also less likely to have a follow-up ED visit (RR .78, 95% CI, .63–.96, P=.02) when adjusted for age, sex, calendar year, and morbidity (Table 3). However, when pediatric patient statistics were isolated from adult statistics, only the adult patients demonstrated a significant difference in time to followup for both types of visits between rural and urban patients.
Table 2.
ORs and 95% CIs for having a follow-up office visit within seven days of an ED visit for asthma, comparing rural to urban residents, 1999–2004, Hawaii*
| Sample | Variable | OR (95% CI) | χ2 | P value |
|---|---|---|---|---|
| Total sample | ||||
| Rural vs urban | .85 (.77–.94) | 10.97 | <.001 | |
| Age in decades | .98 (.95–1.00) | 2.76 | .01 | |
| Female vs male | 1.10 (1.00–1.22) | 3.77 | .05 | |
| HMO vs private insurance | 1.09 (.99–1.21) | 2.82 | .09 | |
| Medicare vs private insurance | 1.03 (.80–1.31) | .04 | .83 | |
| Cost of office visits in last year | 1.17 (1.13–1.20) | 107.17 | <.001 | |
| Morbidity level 2 vs 1 | 1.08 (.94–1.23) | 1.2 | .27 | |
| Morbidity level 3 vs 1 | 1.26 (1.10–1.46) | 10.61 | .001 | |
| Morbidity level 4 vs 1 | 1.26 (1.05–1.51) | 6.41 | .01 | |
| Morbidity level 5 vs 1 | 1.11 (.90–1.35) | .95 | .33 | |
| Children | ||||
| Rural vs urban | .86 (.74–1.01) | 3.57 | .06 | |
| Age in decades | .83 (.71–.98) | 4.92 | .03 | |
| Female vs male | 1.07 (.91–1.26) | .74 | .39 | |
| HMO vs private insurance | 1.07 (.91–1.25) | .62 | .43 | |
| Cost of office visits in last year | 1.36(1.27–1.45) | 80.8 | <.001 | |
| Morbidity level 2 vs 1 | .87 (.72–1.05) | 2.13 | .14 | |
| Morbidity level 3 vs 1 | .92 (.73–1.16) | .49 | .48 | |
| Morbidity level 4 vs 1 | 1.35 (.94–1.94) | 2.6 | .11 | |
| Morbidity level 5 vs 1 | .70 (.44–1.11) | 2.28 | .13 | |
| Adults | ||||
| Rural vs urban | .82 (.73–.93) | 9.29 | .002 | |
| Age in decades | 1.04 (.99–1.08) | 2.67 | .10 | |
| Female vs male | 1.17 (1.03–1.34) | 5.8 | .02 | |
| HMO vs private insurance | 1.15 (1.00–1.32) | 4.0 | .05 | |
| Medicare vs private insurance | .92 (.71–1.18) | .45 | .50 | |
| Cost of office visits in last year | 1.11 (1.08–1.15) | 42.94 | <.001 | |
| Morbidity level 2 vs 1 | 1.25 (1.03–1.52) | 4.95 | .03 | |
| Morbidity level 3 vs 1 | 1.42 (1.17–1.73) | 12.43 | <.001 | |
| Morbidity level 4 vs 1 | 1.30 (1.04–1.64) | 5.19 | .03 | |
| Morbidity level 5 vs 1 | 1.22 (.95–1.57) | 2.42 | .12 | |
OR = odds ratio, CI = confidence interval, ED = emergency department, HMO = health maintenance organization.
Analyses included 4318 adults and 2062 children. Generalized R2 values for the three regression models were .028 for the total sample, .049 for children, and .027 for adults. The percentage concordance was 60.3 for the total sample, 63.0 for children, and 60.1 for adults. For costs, the ORs are per $100 in office visit costs. Results are shown for variables significant (P<.05) in one or more regression models. Models also included the number of ED visits in the past year and indicators for calendar year.
Table 3.
RRs (95% CIs) of subsequent ED visits comparing rural to urban residents who had an initial ED visit for asthma, 1999–2004, Hawaii*
| Sample | Variable | RR (95% CI) | χ2 | P value |
|---|---|---|---|---|
| Total sample | ||||
| Rural vs urban | .78 (.63–.96) | 5.55 | .02 | |
| Age in decades | 1.08(1.03–1.14) | 9.56 | .002 | |
| Female vs male | .93(75–1.14) | .5 | .48 | |
| HMO vs private insurance | 1.32 (1.05–1.64) | 5.9 | .02 | |
| Medicare vs private insurance | .95 (.62–1.46) | .06 | .81 | |
| Number of ER visits in last year | 1.36 (1.22–1.52) | 28.67 | <.001 | |
| Morbidity level 2 vs 1 | 1.02 (.73–1.41) | .01 | .92 | |
| Morbidity level 3 vs 1 | 1.30 (.95–1.79) | 2.66 | .10 | |
| Morbidity level 4 vs 1 | 1.36 (.93–1.98) | 2.58 | .11 | |
| Morbidity level 5 vs 1 | 1.37 (.91–2.04) | 2.3 | .13 | |
| Children | ||||
| Rural vs urban | .92 (.62–1.35) | .19 | .66 | |
| Age in decades | 1.00 (.67–1.49) | .0 | .99 | |
| Female vs male | 1.00 (.67–1.50) | 0 | .99 | |
| HMO vs private insurance | 1.24 (.84–1.83) | 1.13 | .29 | |
| Number of ER visits in last year | 1.00 (.56–1.81) | .0 | .99 | |
| Morbidity level 2 vs 1 | .94 (.58–1.53) | .05 | .82 | |
| Morbidity level 3 vs 1 | 1.11 (.64–1.91) | .14 | .71 | |
| Morbidity level 4 vs 1 | .97 (.41–2.28) | .01 | .94 | |
| Morbidity level 5 vs 1 | .25 (.03–1.88) | 1.81 | .18 | |
| Adults | ||||
| Rural vs urban | .72 (.56–.93) | 6.58 | .01 | |
| Age in decades | 1.03 (.94–1.12) | .38 | .54 | |
| Female vs male | .87 (.68–1.12) | 1.17 | .2 | |
| HMO vs private insurance | 1.33 (1.02–1.75) | 4.28 | .04 | |
| Medicare vs private insurance | 1.02 (.65–1.60) | .01 | .94 | |
| Number of ER visits in last year | 1.39(1.24–1.56) | 31.11 | <.001 | |
| Morbidity level 2 vs 1 | 1.14 (.71–1.82) | .3 | .58 | |
| Morbidity level 3 vs 1 | 1.61 (1.05–2.49) | 4.69 | .03 | |
| Morbidity level 4 vs 1 | 1.72 (1.07–2.77) | 4.98 | .03 | |
| Morbidity level 5 vs 1 | 1.91 (1.15–3.15) | 6.32 | .01 | |
RR = rate ratio, CI = confidence interval, ED = emergency department, HMO = health maintenance organization.
Analyses included 4318 adults and 2062 children. Results are shown for variables significant (P<.05) in one or more regression models. Models also included the costs of office visits in the past year and indicators for calendar year.
Discussion
As expected, rural residents were less likely to receive follow-up care, both in the office and the ED. Since this study used insurance claims, all patients in the study sample had medical coverage; therefore, financial causes are unlikely to account for the differences found. Distance to care and number of available providers may strongly influence the receipt of after-care for asthma in rural areas. Further research should examine distance of patient zip code from a hospital or primary care office to determine if followup is directly related to distance from provider. Similarly, physician density in a specific zip code should be analyzed to determine if time to followup is associated with number of available providers in the area.
An unexpected finding of this study was that no significant difference was observed in follow-up rates for rural children with asthma compared with urban children. This finding implies that although barriers to accessing care may exist, they are overcome when parents need to obtain care for their children with asthma. Other studies have shown that factors associated with improved outpatient pediatric asthma follow-up rates include having medical insurance, high-acuity diagnoses, and higher socioeconomic status,13 Interventions used to increase follow-up rates, such as scheduling the appointment from the ED14 and nurse follow-up phone calls, can increase follow-up rates.15 Interestingly, asthma coaching and monetary incentives did not increase follow-up rates.16 Therefore, research should be directed at determining which interventions are most helpful and cost-effective at increasing outpatient followup for asthma.
A weakness of this study is the fact that the analysis does not control for ethnicity or family income, as these are not factors included with billing records. In fact, rural areas have a higher number of ethnic minorities and lower average household income. Prior studies have found that ethnicity is associated with acute resource use in followup for asthma,17 so this must be included in future studies in this area. Finally, qualitative interviews with asthma patients of different ages could shed light on reasons for disparities in follow-up rates.
Implications for Improving Health Disparities
Understanding the barriers to appropriate follow-up care in rural areas will assist health policy makers in developing solutions to challenges faced by rural community members.
References
- 1.Jong K, Smith DP, Yu XQ, Goumas C, O’Connell D, Armstrong BK. Remoteness and cancer incidence, mortality and survival in New South Wales 1992 to 1996. Sydney: The Cancer Council NSW; 2002. [Google Scholar]
- 2.Grandinetti A, Chang HK, Mau MK, et al. Prevalence of glucose intolerance among native Hawaiians in two rural communities. Native Hawaiian Health Research (NHRR) Project. Diabetes Care. 1998;221(4):549–554. doi: 10.2337/diacare.21.4.549. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin LM, MacLehose RF, Hart LG, et al. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004;20(2):99–108. doi: 10.1111/j.1748-0361.2004.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 4.National Rural Health Association. [Accessed 4/19/2004];What’s different about rural health care? Available at: http//www.nrharural.org/pagefile/different.html.
- 5.Singh GK, Siahpush M. Increasing rural-urban health gradients in US suicide mortality, 1970–1997. Am J Public Health. 2002;92(7):1161–1167. doi: 10.2105/ajph.92.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waitzfelder BE, Engel CC, Jr, Gilbert FL., Jr Substance abuse in Hawaii: perspectives of key local human service organizations. Subst Abus. 1998;19(1):7–22. doi: 10.1080/08897079809511369. [DOI] [PubMed] [Google Scholar]
- 7.Rural Healthy People 2010. [Accessed 4/20/2004];Healthy People2010: a companion document for rural areas. Available at: http://www.srph.tamushsc.Edu/rhp2010/
- 8.Virnig BA, Moscovice IS, Durham SB, et al. Do rural elders have limited care to Medicare hospice services? J Am Geriatr Soc. 2004;52(5):731–735. doi: 10.1111/j.1532-5415.2004.52213.x. [DOI] [PubMed] [Google Scholar]
- 9.Heller RF, O’Connell RL, D’Este C, Lim L, Fletcher PJ. Differences in cardiac procedures among patients in metropolitan and non-metropolitan hospitals in New South Wales after acute myocardial infarction and angina. Aust J Rural Health. 2000;8:310–317. doi: 10.1046/j.1440-1584.2000.00300.x. [DOI] [PubMed] [Google Scholar]
- 10.National Rural Health Association. [Accessed 4/19/2004];What’s different about rural health care? Available at: http//www.nrharural.org/pagefile/different.html.
- 11.Williams SG, Schmidt DK, Redd SC, Storms W. Key clinical activities for quality asthma care: recommendations of the National Asthma Education and Prevention Program. MMWR Recomm Rep. 2003;52(RR6):1–8. [PubMed] [Google Scholar]
- 12.US Census Bureau. Current lists of metropolitan and micropolitan statistical and areas definitions. Updated December 2005 (OMB Bulletin No. 06-01). Available at: http://www.census.gov/population/www/estimates/metrodef.html.
- 13.Wang NE, Kiernan M, Golzari M, Gisondi MA. Characteristics of pediatric patients at risk of poor emergency department after care. Acad Emerg Med. 2006;13(8):840–847. doi: 10.1197/j.aem.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 14.Magnusson AR, Hedges JR, Vanko M, McCarten K, Moorhcad JC. Follow-up compliance after emergency department evaluation. Ann Emerg Med. 1993;22:560–567. doi: 10.1016/s0196-0644(05)81942-0. [DOI] [PubMed] [Google Scholar]
- 15.Wong KW, Wong FKY, Chan MF. Effects of nurse-initiated telephone follow-up on self-efficacy among patients with chronic obstructive pulmonary disease. J Adv Nurs. 2005;49(2):210–222. doi: 10.1111/j.1365-2648.2004.03280.x. [DOI] [PubMed] [Google Scholar]
- 16.Smith SR, Jaffe DM, Highstein G, Fisher EB, Trinkaus KM, Strunk RC. Asthma coaching in the pediatric emergency department. Acad Emerg Med. 2006;13(8):835–839. doi: 10.1197/j.aem.2006.03.565. [DOI] [PubMed] [Google Scholar]
- 17.Ng TP, Lim TK, Abisheganaden J, Eng P, Sin FL. Factors associated with acute health care use in a national adult asthma management program. Ann Allergy Asthma, Immunol. 2006;97(6):784–793. doi: 10.1016/S1081-1206(10)60970-2. [DOI] [PubMed] [Google Scholar]