Abstract
Substantial research has documented pervasive disparities in the prevalence, severity, and morbidity of asthma among minority populations compared to non-Latino whites. The underlying causes of these disparities are not well understood, and as a result, the leverage points to address them remain unclear. A multilevel framework for integrating research in asthma health disparities is proposed in order to advance both future research and clinical practice. The components of the proposed model include health care policies and regulations, operation of the health care system, provider/clinician-level factors, social/environmental factors, and individual/family attitudes and behaviors. The body of research suggests that asthma disparities have multiple, complex and inter-related sources. Disparities occur when individual, environmental, health system, and provider factors interact with one another over time. Given that the causes of asthma disparities are complex and multilevel, clinical strategies to address these disparities must therefore be comparably multilevel and target many aspects of asthma care. Clinical Implications: Several strategies that could be applied in clinical settings to reduce asthma disparities are described including the need for routine assessment of the patient’s beliefs, financial barriers to disease management, and health literacy, and the provision of cultural competence training and communication skills to health care provider groups.
Keywords: Asthma disparities, multi-level model of asthma disparities, clinical recommendations
Introduction
Substantial evidence across multiple avenues of research has documented pervasive asthma disparities between minorities and non-Latino whites. Higher rates of asthma prevalence are consistently found among certain minority racial/ethnic groups, particularly African American, American Indian and Puerto Rican populations.1-3 There is also substantial evidence of worse asthma control among minority populations compared to non-Latino whites (NLW), including significantly higher rates of asthma exacerbations and missed days from school or work,4-6 greater rates of emergency department (ED) utilization,7-9 higher hospitalization rates,9-12 as well as greater asthma mortality risk.13, 14
Although the literature in asthma disparities is evolving rapidly, considerably more research has been conducted with certain minority groups, such as African Americans and Latinos, compared to others, such as Native Americans. Additionally, the manifestation of disparities across different racial/ethnic groups may differ substantially. For example, Latinos of Mexican origin present with lower asthma prevalence and morbidity compared to whites,1, 2 and children of African American and Puerto Rican origin appear to have the highest prevalence as compared to non-Latino whites,3 with Puerto Ricans exhibiting the highest prevalence of any other ethnic/racial group.1 On the other hand, African Americans demonstrate higher rates of hospitalization9, 10, 12, 15 and higher rates of asthma mortality13, 14 compared to NLW and Latino populations. These findings suggest that what constitutes “disparity” may differ by racial/ethnic group.
Although ethnic/racial disparities in asthma have been well established, the underlying causes of these disparities are poorly understood, and as a result, the leverage points to address them remain unclear. In the present paper, we present a brief review of current findings that have emerged in key areas of research on health care disparities in asthma, and propose a multilevel framework for integrating this substantial literature. Our model is derived from the Institute of Medicine’s 2002 landmark report on unequal care, which focused on 1) health care policies and regulations, 2) operation of the health care system, and 3) provider/clinician-level factors. In addition to these health care system factors, we also consider broader 4) social/environmental factors, and 5) individual/family attitudes and behaviors that may have a role in asthma disparities. Below we present empirical support for the processes included in the main domains of our proposed model and suggest how this model can be helpful in advancing both future research and clinical practice.
1) Health Care Policy Factors
There is evidence that certain health care policies may contribute to disparities in asthma outcomes, and that cost control strategies implemented by public health plans may differentially affect minority populations. Minorities are over-represented in government sponsored health plans such as Medicare, which are federally and state regulated for cost control. As a result, minority populations may receive restricted access to specialists and preventive care, thus resulting in lower quality of health care.16, 17
Access to Care
Factors common to publicly insured plans, such as decreased use of preventive care and limited referrals to asthma specialists, have been associated with higher rates of hospitalization, ED use and increased risk of mortality 18, 19. Restricted access to specialists may contribute to disparities in asthma morbidity, given that there is evidence that specialists are more likely to prescribe controller medications than primary care providers, independent of the patient’s minority status.19, 20
Eligibility and Co-payment
In an effort to control costs, many states have enacted policies to reduce Medicaid eligibility and manage prescription drug benefits, either by lowering the payments to pharmacies, or by introducing co-payments.16 There is preliminary evidence that the introduction of these restrictions may negatively affect asthma outcomes among minorities and the poor16, hence increasing existing disparities. In support of this notion, one study demonstrated that doubling existing co-payments resulted in a 21% reduction in the number of prescriptions filled for asthma.21 Rand and colleagues22 found that among African American families covered by Medicaid, out of pocket payments for health care were an important predictor of ED use for an asthma exacerbation.22 These findings suggest that increasing out of pocket costs to disadvantaged groups may diminish access to medication and to appropriate strategies for preventive management of exacerbations.
2) Operation of the Health Care System
Adherence with Guidelines
National guidelines23 continue to stress that families and health care providers should collaborate actively to manage asthma, with an emphasis on preventive management. Preventive management includes strategies to avert asthma episodes through control of relevant environmental triggers, regular use of controller medications for patients with persistent symptoms, use of an asthma action plan, and referrals to specialists when indicated. In addition, assessment of asthma severity at initial presentation should guide treatment initiation, with repeated assessments of asthma control to determine if relevant treatment adjustments need to be made. Research demonstrates that many health care providers have difficulty adhering to these established guidelines24-26, particularly providers who treat minorities.27
There is evidence that providers often fail to provide a prescription for controller medications even when children present with symptoms of persistent asthma,28 and that this under-prescription of controller medications is even more pronounced for minority children as compared to NLW’s.29, 30 In a recent study of prescription practices of pediatricians treating children with mild persistent asthma, pediatricians in practices with more than 25% of African American children in their practice reported prescribing daily use of controller medications less frequently (31%) than pediatricians in all practices (51%).31 Other research has shown that African American and Latino children are less likely to have inhaled corticosteroids (ICS) prescribed during an ED visit, and less likely to have ICS filled prior to the ED visit as compared to NLW’s.8, 9, 32
Practice policies
Practice policies within managed care Medicaid setting may also have an impact on asthma outcomes. For example, Lieu and colleagues33 found that settings in which the organization provided reports about asthma screening to physicians, promoted access and continuity of care, and implemented cultural competence training for staff had better asthma outcomes and higher patient-rated quality of care after adjusting for patient demographics and baseline asthma status. In practice settings that promoted these policies, patients were less likely to under use controller medications, and demonstrated better indicators of physical status at follow up.
3) Health Provider/Clinician Factors
Although less commonly studied, it should be acknowledged that individual provider characteristics and beliefs have the potential to contribute to disparities in asthma outcomes. The IOM report 17 proposes that, although most providers intend to provide equitable care, subtle forms of discrimination may contribute to disparities in health care. The report proposes three mechanisms that may produce discriminatory provider practices: Unintentional bias against minorities in interpreting the patient’s symptoms and in decision making, greater clinical uncertainty when interacting with minority patients, and beliefs or stereotypes held by the provider. Unintentional bias results from the marked differences that often exist between physicians and patients belonging to other socio-economic class or racial/ethnic groups. Physicians are likely to share the same beliefs or stereotypes of minorities shared by the culture in which they live and these in turn may affect the care they give. These three sources of practice bias are more likely to occur when physicians have poor understanding of the patient’s ethnic and cultural disease models, and limited knowledge of patient preferences regarding disease management approaches.34 In what follows we provide some evidence that minorities with asthma may receive poorer treatment within the clinical encounter as compared to NLW’s with asthma.
Bias/Stereotyping
Asthma is a disease for which assessment of current level of asthma severity is crucial for appropriate treatment. Provider assessment and interpretation of patient-reported symptoms are crucial in determining asthma severity level. Thus, ineffective provider communication often results in misclassification of asthma symptom severity among minority patients. One study of patients enrolled in 15 managed care organizations showed that under classification of asthma severity by physicians was significantly more common among African Americans than NLW’s, and that this underestimation was associated with lower patient use of inhaled corticosteroids (ICS).35
Providers may unconsciously behave in ways that confirm their stereotypes, even though consciously they intend to provide equal treatment.36 For example, some physicians believe that African Americans are less adherent with treatment37, a notion which could lead to lower prescription rates of controller medications, and less emphasis on preventive education. Although this belief is supported by research showing that African-Americans and other minorities are less likely to adhere to medication38,39 these findings do not reflect the behavior of all members of a group, and should not be used to predict individual patient’s behaviors. Further, non-adherence may result from remediable, but often hidden barriers such as inadequate patient education, health beliefs or poor health literacy. Physicians who communicate effectively and get to know their patients as unique individuals will therefore be best able to identify and address patient barriers to adherence.
Cultural Competence
Providers’ greater misclassification of severity for minority groups may be due to cultural differences. Asthma treatment relies on the accuracy of the patient’s symptom reporting, and provider comprehension and interpretation of those reports for appropriate diagnosis and treatment. When the family and provider come from different cultural backgrounds, and/or speak different languages, difficulties in the cross cultural communication may compromise the acquisition of the necessary information to make an accurate diagnosis, or assess severity, develop a trusting relationship and treat adequately.40-42 Research in this area is limited, and although investigations of the contribution of limited cultural competence and provider bias to asthma disparities may be challenging to implement, such research may provide greater insight into the mechanisms underlying disparities in disease management behavior and outcomes for patients with asthma.
4) Individual/Family Factors
Emerging research has examined the role that biologic and genetic risk factors may play in asthma disparities.43, 44 While these inherent risk factors likely contribute to susceptibility and/or severity, it is also clear that substantial variation in asthma outcomes may be mediated through the influence of individual behavioral and psychosocial differences on self-management. We describe below these potentially modifiable individual/family factors that may contribute to asthma disparities.
Health Beliefs
Given that one of the most central recommendations for management of persistent asthma symptoms is the use of daily controller medications, and that the use of quick-relief medications is recommended for all patients with asthma45, attitudes toward medication use are an important factor to consider in understanding disparities in disease management and course.
Attitudes towards medication impact utilization of physician-recommended as well as alternative medications, and, ultimately, health outcomes. For example, use of home remedies to manage asthma has been reported frequently among Latinos46, 47 and African Americans.48, 49 The use of home remedies as an initial response to symptoms may delay timely treatment, causing symptoms to progress and become more severe. There is evidence that many patients never tell their physicians about the use of home remedies,50 and that greater discussion of how to integrate home remedies with conventional asthma treatment would be well-received by patients with asthma.48
In addition to use of alternative medications, there is some evidence that general beliefs about medication efficacy and concerns about medication use vary widely by ethnicity. One qualitative study with African-American parents documented numerous concerns and barriers to medication use.49 Parents noted many concerns about medication and side effects, such as the belief that children would become addicted to asthma medicines. A recent survey study51 indicated that relative to non-minority parents of children with asthma, minority parents’ concerns about medication more frequently outweighed belief in the need for medication. Other research has indicated that Latino and NLW parents hold different beliefs in medication necessity relative to concern, with Latino parents acknowledging higher levels of concern about medication use and addiction in relation to medication necessity.52
Adherence with therapy
Even if families receive and fill a prescription for controller medication, adherence is generally poor53 and most compromised among minority patients.38, 39 In one early study, Apter and colleagues38 found adherence to ICS among adults with moderate to severe asthma to be approximately 63% of prescribed doses. Racial/ethnic minority status, Spanish as primary language, and poor patient-clinician communication were all associated with poor adherence.38 In another more recent study, African American adults were found to have low ICS adherence relative to NLW’s (40% vs. 58%).54 Studies with pediatric groups demonstrate a similar pattern. A recent investigation found that minority children (predominately African-American) took significantly fewer doses of inhaled steroids relative to non-minority children (35% vs. 62% of prescribed doses, respectively).55 Another study found a similar difference in medication adherence rates between minority and nonminority children with asthma (37% vs. 53% of prescribed doses, respectively), and that these differences remained when controlling for socioeconomic status.56
There is some evidence that the concerns about medications more frequently held by minorities may be a factor in low medication adherence however, study findings have been mixed. In one study, negative beliefs were associated with poor self-reported adherence among parents of children with asthma, although actual medication use was not measured.51 Among adults with asthma, there is some indication that medication beliefs may mediate the association between minority status and low adherence to ICS, and that “readiness to take ICS” may predict adherence for African Americans with asthma.57 In other words, culturally different medication beliefs may be a factor in explaining the observed association between minority status and low adherence to ICS. Another study however, found that although attitude toward ICS use was predictive of adherence, it did not mediate the association between race-ethnicity and adherence.58 Negative beliefs about controller medications, and associated underuse, may be an important factor in the observed ethnic disparities in asthma morbidity however, the mechanisms through which these factors interface with other sources of disparity, such as health care access and financial resources, merit further investigation.
Health Literacy
Health literacy may also be a barrier to patient understanding of physician educational information. In one study of elderly patients insured by a large private health care plan, 33.9% of English-speaking and 53.9% of Spanish-speaking respondents were found to have inadequate or marginal health literacy.59 Poor health literacy is also more common among low income and minority patients.60 Substantial research has confirmed that low health literacy is associated with overall poorer health outcomes for several conditions including asthma.60, 61 There is some evidence that providing tailored asthma self-management education can be a useful strategy among low-literacy adults with asthma,62 suggesting that how providers identify and communicate with patients with low health literacy may have an impact on disease management outcomes.
5) Social/Environmental Factors
Americans with low socioeconomic status (SES), whether measured by income or occupation have higher levels of illness than higher income populations.63 People with low incomes in general have poorer health and shorter life expectancy.64 For certain racial groups such as African Americans, mortality rates in almost every illness including asthma are higher than whites independent of income level.63 Furthermore, minorities and individuals with low SES are more likely to engage in high risk behaviors associated with asthma exacerbations such as smoking, and are also less likely to quit smoking than high income populations.65, 66
It is well known that a vast majority of minorities live in neighborhoods where most families are below the federal poverty level and in segregated neighborhoods where the majority of families belong to the same minority group (68). 67 Although poverty has been associated with poor health in general, in the case of asthma the evidence has been equivocal, with three studies finding an association between neighborhood poverty and increased asthma prevalence independent of individual risk factors64, 68 and two other studies finding no association, particularly for Hispanic adults.67, 69
It is well demonstrated, however, that individuals of low SES often live in urban neighborhoods characterized by greater exposure to environmental toxins and violence, and higher levels of stress.70 A growing number of studies have shown that these multiple social and economic stressors characteristic of poor urban neighborhoods affect health independent of individual vulnerabilities.71, 72
Environmental Factors
Housing in impoverished areas is more likely to have above average exposure to indoor allergens such as dust mite, rodent allergens, cockroach allergens, mold and mildew.64, 73 Low-income communities have higher concentration of buildings that emit environmental pollutants into the ambient air.74 Although it is not clear whether air pollutants cause asthma, level of air pollution is correlated with morbidity of respiratory illnesses.75 Minority children are also significantly more likely to be exposed to passive cigarette smoke, which is a known contributor to asthma prevalence and morbidity.76, 77
Stress/violence
Residents of poor neighborhoods may experience stress related to lack of neighborhood safety, violence and discrimination.78 There is increasing evidence that stress may influence the onset and course of asthma, particularly for those in urban environments. In addition, levels of maternal stress79 and distress80 have been associated with increased risk for asthma onset. Stress related to exposure to violence in high risk neighborhoods has been associated with asthma exacerbations.81 Several other studies have found an association between stress, asthma and atopy.82-84 In one novel study, chronic stress was associated with immunological profiles in a sample of children with asthma.85 Specifically, the pathway between SES and immune function (higher production of IL-5 and increased eosinophil counts) was explained by differences in chronic stress and threat perception.
Depression
Poverty is linked with a markedly higher risk of depression.86 An emerging literature links depression in low-income individuals with less confidence in asthma treatment effectiveness, less self-efficacy to cope with asthma episodes, poor adherence to therapy, higher use of emergency, hospitalization and outpatient services, higher functional impairment, higher number of asthma episodes and decreased use of preventive services.87-89
Stress and socioeconomic disadvantage clearly increases risk for asthma and places additional burdens on asthma management. One recent study of urban children with asthma found that although poverty was independently associated with increased risk for asthma morbidity, a cumulative risk index consisting of multiple risks associated with urban neighborhoods (e.g., neighborhood unsafety), urban living (e.g., exposure to ETS), and cultural experiences (e.g., acculturative stress) and accounted for additional variance in morbidity indexes than poverty alone.47 These findings suggest that models that attempt to depict social and economic influences on asthma outcomes among minority groups will need to capture multiple levels of risk.
A Multi-level Conceptual Model for Explaining and Addressing Asthma Disparities
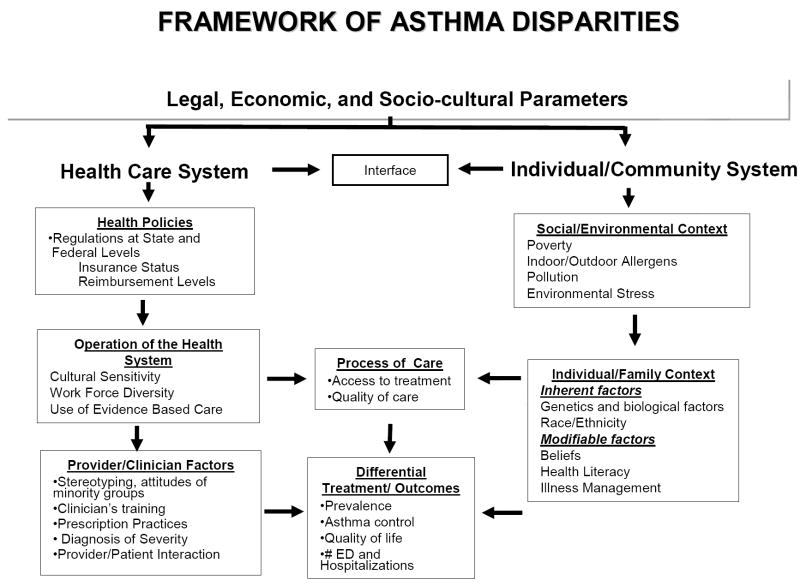
The body of research in this area suggests that no single risk factor has emerged as the primary cause of disparities. Instead, asthma disparities have multiple, complex and inter-related sources. Therefore, to move forward in our understanding of asthma disparities and development of effective interventions it will be necessary to frame our future research within a conceptual model that incorporates a range of risk factors at multiple levels of influence. We propose a multilevel multifaceted, conceptual model to explain the mechanisms involved in the observed disparities in asthma. (See Figure 1). The model is based on an expanded definition of the IOM model that depicts disparities as racial and ethnic differences in access, health care quality or health care outcomes not due to differences in appropriateness of care, health status or patient preferences.17, 90 This definition considers racial/ethnic disparities as requiring remediation even if they arise through differences in income, insurance and other mechanisms outside the clinical condition.91 Given that the effect of social class in explaining disparities is likely to be as potent as that of race/ethnicity, and there are likely to be interactions between class and ethnicity92, we include income and access factors as important contributors to asthma disparities.
Figure 1.
Multilevel Asthma Disparities Model
The key domains relating to the health care system are depicted on the left-hand side of Figure 1. As in our previous model4 and because of the increasing evidence of genetic and biological differences related to the risk for asthma and its course, we add emphasis on individual-level variables, as well as individual-based processes that are modifiable, but may contribute to disparities (e.g. medication beliefs, and illness management behaviors). Additionally, we include a fourth domain of external environmental factors (e.g., indoor/outdoor allergens, pollution and neighborhood stresses), which may be particularly critical for the onset and progression of asthma (See right hand side Figure 1). The components within and across the domains are assumed to interact with each other to affect the process of care that, in turn, influences disparity outcomes.
Practical Implications of Applying a Multi-level Asthma Disparities Model for Research and Clinical Practice
It is apparent from this review that understanding ethnic and/or cultural disparities in asthma morbidity and prevalence is a complicated process. While multiple risk factors have been identified, no single variable directly accounts for large differences in outcomes. If we are to reduce asthma disparities there is a need to obtain a better understanding of the complex ways in which multiple variables interact, and the relative weight that each one contributes to inequalities in asthma morbidity and prevalence. Research that examines the complex relationships among factors at the socioeconomic, health system and individual level that increase the risk for poor asthma outcomes among the poor and racial/ethnic minorities is needed.
For example, it is possible that genetic variations in medication response found among some African Americans and some subgroups of Latinos with asthma44, 45 may relate to individual beliefs about the efficacy of medication. The process of care in which these beliefs are discussed and addressed is shaped by the health care literacy of the patient, the health care system, and elements of the patient-provider interaction (e.g., provider biases about patient receptivity to medication use). Health care policies then influence the accessibility of medication to patients. Asthma management occurs through multiple channels, and to truly understand the mechanisms underlying health care disparities we need to use a broad lens to consider the wide range of influence on health care behavior. For this reason, the next generation of research will require a more sophisticated analytic tool box that incorporates such strategies as multilevel modeling.93
It is important to note that some domains within the model may be more important or modifiable than other domains. For example, although genetic factors clearly influence the onset and expression of asthma2, 43, other factors such as those within the health care system, the patient-provider relationship, and the individual/family domain are more amenable to intervention. Research regarding the efficacy and cost effectiveness of treatment approaches that affect changes in these various levels of influence is needed to inform treatment course.
Culturally sensitive clinicians, who are well trained facilitate effective communication with the family and provide the appropriate prevention education, intervention, and evidence based treatment can offset many of the disparities related to asthma morbidity. Providers can make special efforts with minority children to monitor changes in clinical status, and to modify therapy more frequently when needed. Clinicians may need to spend more time with minority patients so that they are able to better understand the patient’s context, medication and health beliefs that may be interfering with treatment adherence and to more effectively meet the needs of patients with low health literacy. We acknowledge, however that this recommendation may be difficult to implement given the managed care health care policies in many states that require high productivity of providers in order to remain financially solvent.
Finally, asthma cannot be controlled effectively unless people have affordable access to a full range of services and quality of care. Health policies can make insurance plans more accessible, expand Medicaid and S-CHIP coverage and reimbursement to physicians, as well as reimburse for prevention interventions that are culturally sensitive. Quality management strategies such as “pay for performance”, as well as electronic health records that facilitate monitoring show promise to improve quality of care if implemented in Medicaid.16
Clinical Implications and Recommendations
Our review of the literature and proposed model underscores that the causes of asthma disparities are complex and multilevel. Clinical strategies to address these disparities must therefore be comparably multilevel and targeted. We believe that disparities occur when individual, environmental, health system, and provider factors interact with each other in multiple ways, and that these interactions may vary according to the person’s particular needs that change with time. With this preamble in mind we offer a number of suggestions that may begin to ameliorate the asthma disparities observed among ethnic racial groups. (see Table I). The first step is for the clinician to acknowledge the complexity of the issues that may contribute to poor asthma outcomes among minorities.94 Poor outcomes are often due to divergence between physician recommendations and the implementation of a treatment plan. Patients’ lack of adherence to recommended treatment is likely related to a cascade of factors that include patient health literacy, medication beliefs, patient-provider communication, and health care access.
Table I.
Clinical Practice Strategies to Address Asthma Disparities
| Disparity Observed | Clinical Practice Strategies |
|---|---|
| Increased likelihood that health care providers will under treat asthma | Incorporate routine clinic screening for asthma control Audit asthma treatment plans for appropriateness |
| Increased risk of patient non-adherence | Assess patients’ treatment expectation, beliefs and concerns about asthma and asthma therapy Inquire about use of complementary medications or complementary therapies Routinely assess financial barriers to adherence Reduce or eliminate co-pays |
| Increased risk of patient-provider communication/language barriers | Implement cultural competence and communication skills training for staff and physicians Increase availability of translators Increase work force diversity |
| Increased exposure to high-risk environments | Offer counseling and referral for smoking cessation/passive smoke avoidance assistance –.e.g. 1-800-QUITNOW. Public health departments may also offer free or low-cost programs. Offer education on allergens and triggers |
| Increased risk of low health literacy | Avoid complicated medical terms Use “tell me back” strategy to confirm understanding Use low-literacy asthma educational materials |
| Increased risk of depression | Consider routine screening for depression with appropriate referral |
At the level of the provider group or clinic, clinical strategies that routinely assess asthma control and appropriateness of treatment, as well as interventions designed to improve provider-patient communication about patient preference, asthma beliefs and barriers to care are promising strategies for addressing the disparity observed in the quality of care received by minority populations.33, 95
Population-based projections indicate that the proportion of the United States population that is considered “minority” will continue to increase over the next several decades, ultimately surpassing the NLW majority by 2050.96 In addition, increasing pressures on the economy may limit publicly available resources and initiate further restrictions on health care coverage, heightening the risk that existing disparities in asthma will not just continue, but will increase. The most effective intervention for addressing asthma disparities would likely be the abolishment of poverty and racial bias. Until then, our asthma research and our clinical strategies will necessarily have to become increasingly integrated, multi-faceted and multilevel.
Acknowledgments
We acknowledge the help provided by Drs. Greg Fritz, and Barbara Jandasek from Brown University.
Financial Support: This study was supported by NIH Grant # 5P60 MD002261-02 funded by the National Center for Minority Health and Health Disparities, and 5 U01 HL 072519-05 Canino (PI) and R01 HL45157 Fritz (PI) from the National Heart, Lung and Blood Institute.
Abbreviations
- ED
emergency department
- ICS
inhaled corticosteroids
- SES
socio economic status
- NLW
non-Latino white
References
- 1.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 2.Hunninghake GM, Weiss ST, Celedon JC. Asthma in Hispanics. Am J Respir Crit Care Med. 2006;173:143–63. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Disease Control and Prevention. The State of Childhood Asthma, United States: 1980-2005. 2006 is available at www.cdc.gov/nchs.
- 4.Canino G, Koinis-Mitchell D, Ortega AN, McQuaid EL, Fritz GK, Alegria M. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Soc Sci Med. 2006;63:2926–37. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, et al. Racial/ethnic variation in asthma status and management practices among children in managed medicaid. Pediatrics. 2002;109:857–65. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 6.Haselkorn T, Lee JH, Mink DR, Weiss ST. Racial disparities in asthma-related health outcomes in severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol. 2008;101:256–63. doi: 10.1016/S1081-1206(10)60490-5. [DOI] [PubMed] [Google Scholar]
- 7.Ginde AA, Espinola JA, Camargo CA., Jr Improved overall trends but persistent racial disparities in emergency department visits for acute asthma, 1993-2005. J Allergy Clin Immunol. 2008;122:313–8. doi: 10.1016/j.jaci.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse LK, Deshpande S, Vezina M. Disparities in asthma hospitalizations among children seen in the emergency department. J Asthma. 2007;44:833–7. doi: 10.1080/02770900701750163. [DOI] [PubMed] [Google Scholar]
- 9.Shields AE, Comstock C, Weiss KB. Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics. 2004;113:496–504. doi: 10.1542/peds.113.3.496. [DOI] [PubMed] [Google Scholar]
- 10.Akinbami L. The state of childhood asthma, United States, 1980-2005. Adv Data. 2006:1–24. [PubMed] [Google Scholar]
- 11.Erickson SE, Iribarren C, Tolstykh IV, Blanc PD, Eisner MD. Effect of race on asthma management and outcomes in a large, integrated managed care organization. Arch Intern Med. 2007;167:1846–52. doi: 10.1001/archinte.167.17.1846. [DOI] [PubMed] [Google Scholar]
- 12.Gupta RS, Carrion-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–8. doi: 10.1016/j.jaci.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 13.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–22. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 14.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990-1995. Am J Respir Crit Care Med. 2000;161:504–9. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 15.Fisher-Owens SA, Turenne WM, Chavanu K, Slonim AD. Racial Disparities in Children Hospitalized with Asthma at Academic Childrens’ Hospitals. Pediatric Asthma, Allergy & Immunology. 2006;19:162–71. [Google Scholar]
- 16.Shields AE. Trends in private insurance, Medicaid/State Children’s Health Insurance Program, and the health-care safety net: implications for asthma disparities. Chest. 2007;132:818S–30S. doi: 10.1378/chest.07-1903. [DOI] [PubMed] [Google Scholar]
- 17.Smedley BD, Stith AY, Nelson AR. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Board of Health Sciencies Policy, Institute of Medicine; Washington, D.C.: 2002. Unequal treatment confronting racial and ethnic disparities in health care. [Google Scholar]
- 18.Berman S, Armon C, Todd J. Impact of a decline in Colorado Medicaid managed care enrollment on access and quality of preventive primary care services. Pediatrics. 2005;116:1474–9. doi: 10.1542/peds.2005-0923. [DOI] [PubMed] [Google Scholar]
- 19.Joseph CL, Havstad SL, Ownby DR, Johnson CC, Tilley BC. Racial differences in emergency department use persist despite allergist visits and prescriptions filled for antiinflammatory medications. J Allergy Clin Immunol. 1998;101:484–90. doi: 10.1016/S0091-6749(98)70355-0. [DOI] [PubMed] [Google Scholar]
- 20.Finkelstein JA, Lozano P, Farber HJ, Miroshnik I, Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Arch Pediatr Adolesc Med. 2002;156:562–7. doi: 10.1001/archpedi.156.6.562. [DOI] [PubMed] [Google Scholar]
- 21.Goldman DP, Joyce GF, Escarce JJ, Pace JE, Solomon MD, Laouri M, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291:2344–50. doi: 10.1001/jama.291.19.2344. [DOI] [PubMed] [Google Scholar]
- 22.Rand CS, Butz AM, Kolodner K, Huss K, Eggleston P, Malveaux F. Emergency department visits by urban African American children with asthma. J Allergy Clin Immunol. 2000;105:83–90. doi: 10.1016/s0091-6749(00)90182-9. [DOI] [PubMed] [Google Scholar]
- 23.National Institutes of Health, NH, Lung, and Blood Institute. National Asthma Education and Prevention Program. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. NIH; Washington (DC): 2007. NIH publication no. 07-4051. [Google Scholar]
- 24.Cabana MD, Ebel BE, Cooper-Patrick L, Powe NR, Rubin HR, Rand CS. Barriers pediatricians face when using asthma practice guidelines. Arch Pediatr Adolesc Med. 2000;154:685–93. doi: 10.1001/archpedi.154.7.685. [DOI] [PubMed] [Google Scholar]
- 25.Diette GB, Skinner EA, Markson LE, Algatt-Bergstrom P, Nguyen TT, Clark RD, et al. Consistency of care with national guidelines for children with asthma in managed care. J Pediatr. 2001;138:59–64. doi: 10.1067/mpd.2001.109600. [DOI] [PubMed] [Google Scholar]
- 26.Finkelstein JA, Lozano P, Shulruff R, Inui TS, Soumerai SB, Ng M, et al. Self-reported physician practices for children with asthma: are national guidelines followed? Pediatrics. 2000;106:886–96. [PubMed] [Google Scholar]
- 27.Flores G, Lee M, Bauchner H, Kastner B. Pediatricians’ attitudes, beliefs, and practices regarding clinical practice guidelines: a national survey. Pediatrics. 2000;105:496–501. doi: 10.1542/peds.105.3.496. [DOI] [PubMed] [Google Scholar]
- 28.Halterman JS, Yoos HL, Kaczorowski JM, McConnochie K, Holzhauer RJ, Conn KM, et al. Providers underestimate symptom severity among urban children with asthma. Arch Pediatr Adolesc Med. 2002;156:141–6. doi: 10.1001/archpedi.156.2.141. [DOI] [PubMed] [Google Scholar]
- 29.Kozyrskyj AL, Mustard CA, Simons FE. Socioeconomic status, drug insurance benefits, and new prescriptions for inhaled corticosteroids in schoolchildren with asthma. Arch Pediatr Adolesc Med. 2001;155:1219–24. doi: 10.1001/archpedi.155.11.1219. [DOI] [PubMed] [Google Scholar]
- 30.Riekert KA, Butz AM, Eggleston PA, Huss K, Winkelstein M, Rand CS. Caregiver-physician medication concordance and undertreatment of asthma among inner-city children. Pediatrics. 2003;111:e214–20. doi: 10.1542/peds.111.3.e214. [DOI] [PubMed] [Google Scholar]
- 31.Sawicki GS, Smith L, Bokhour B, Gay C, Hohman KH, Galbraith AA, et al. Periodic use of inhaled steroids in children with mild persistent asthma: what are pediatricians recommending? Clin Pediatr (Phila) 2008;47:446–51. doi: 10.1177/0009922807312184. [DOI] [PubMed] [Google Scholar]
- 32.Boudreaux ED, Emond SD, Clark S, Camargo CA., Jr Race/ethnicity and asthma among children presenting to the emergency department: differences in disease severity and management. Pediatrics. 2003;111:e615–21. doi: 10.1542/peds.111.5.e615. [DOI] [PubMed] [Google Scholar]
- 33.Lieu TA, Finkelstein JA, Lozano P, Capra AM, Chi FW, Jensvold N, et al. Cultural competence policies and other predictors of asthma care quality for Medicaid-insured children. Pediatrics. 2004;114:e102–10. doi: 10.1542/peds.114.1.e102. [DOI] [PubMed] [Google Scholar]
- 34.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 35.Okelo SO, Wu AW, Merriman B, Krishnan JA, Diette GB. Are physician estimates of asthma severity less accurate in black than in white patients? J Gen Intern Med. 2007;22:976–81. doi: 10.1007/s11606-007-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burgess DJ, Fu SS, van RM. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004:1154–9. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Ryn M, Burke JE. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 38.Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157:1810–7. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- 39.Wells K, Pladevall M, Peterson EL, Campbell J, Wang M, Lanfear DE, et al. Race-ethnic differences in factors associated with inhaled steroid adherence among adults with asthma. Am J Respir Crit Care Med. 2008;178:1194–201. doi: 10.1164/rccm.200808-1233OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richardson LD, Babcock Irvin C, Tamayo-Sarver JH. Racial and ethnic disparities in the clinical practice of emergency medicine. Acad Emerg Med. 2003;10:1184–8. doi: 10.1111/j.1553-2712.2003.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 41.Flores G, Abreu M, Schwartz I, Hill M. The importance of language and culture in pediatric care: case studies from the Latino community. J Pediatr. 2000;137:842–8. doi: 10.1067/mpd.2000.109150. [DOI] [PubMed] [Google Scholar]
- 42.Diette GB, Rand C. The contributing role of health-care communication to health disparities for minority patients with asthma. Chest. 2007;132:802S–9S. doi: 10.1378/chest.07-1909. [DOI] [PubMed] [Google Scholar]
- 43.Barnes KC. Genetic epidemiology of health disparities in allergy and clinical immunology. J Allergy Clin Immunol. 2006;117:243–54. doi: 10.1016/j.jaci.2005.11.030. quiz 55-6. [DOI] [PubMed] [Google Scholar]
- 44.Burchard EG, Avila PC, Nazario S, Casal J, Torres A, Rodriguez-Santana JR, et al. Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. Am J Respir Crit Care Med. 2004;169:386–92. doi: 10.1164/rccm.200309-1293OC. [DOI] [PubMed] [Google Scholar]
- 45.National Asthma Education and Prevention Program. Expert Panel Report 3: guidelines for the diagnosis and management of asthma N, Washington (DC) 2007 NIH publication no. 07- Available at http://www.nhlbi.nih.gov/guidelines/asthma/
- 46.Bearison DJ, Minian N, Granowetter L. Medical management of asthma and folk medicine in a Hispanic community. J Pediatr Psychol. 2002;27:385–92. doi: 10.1093/jpepsy/27.4.385. [DOI] [PubMed] [Google Scholar]
- 47.Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Esteban C, Canino G, et al. Multiple urban and asthma-related risks and their association with asthma morbidity in children. J Pediatr Psychol. 2007;32:582–95. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.George M, Birck K, Hufford DJ, Jemmott LS, Weaver TE. Beliefs About Asthma and Complementary and Alternative Medicine in Low-Income Inner-City African-American Adults. J Gen Intern Med. 2006;21:1317–1324. doi: 10.1111/j.1525-1497.2006.00624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspectives. Pediatrics. 2000;106:512–9. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 50.Pachter LM, Cloutier MM, Bernstein BA. Ethnomedical (folk) remedies for childhood asthma in a mainland Puerto Rican community. Arch Pediatr Adolesc Med. 1995;149:982–8. doi: 10.1001/archpedi.1995.02170220048007. [DOI] [PubMed] [Google Scholar]
- 51.Conn KM, Halterman JS, Lynch K, Cabana MD. The impact of parents’ medication beliefs on asthma management. Pediatrics. 2007;120:e521–6. doi: 10.1542/peds.2006-3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McQuaid EL, Koinis Mitchell D, Walders N, Nassau JH, Kopel SJ, Klein RB, et al. Pediatric asthma morbidity: the importance of symptom perception and family response to symptoms. J Pediatr Psychol. 2007;32:167–77. doi: 10.1093/jpepsy/jsj112. [DOI] [PubMed] [Google Scholar]
- 53.Bender B, Boulet LP, Chaustre I, Rand C. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. Asthma. [Google Scholar]
- 54.Williams LK, Joseph CL, Peterson EL, Moon C, Xi H, Krajenta R, et al. Race-ethnicity, crime, and other factors associated with adherence to inhaled corticosteroids. J Allergy Clin Immunol. 2007;119:168–75. doi: 10.1016/j.jaci.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 55.Bender BG, Rankin A, Tran ZV, Wamboldt FS. Brief-interval telephone surveys of medication adherence and asthma symptoms in the Childhood Asthma Management Program Continuation Study. Ann Allergy Asthma Immunol. 2008;101:382–6. doi: 10.1016/S1081-1206(10)60314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28:323–33. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 57.Le TT, Bilderback A, Bender B, Wamboldt FS, Turner CF, Rand CS, et al. Do asthma medication beliefs mediate the relationship between minority status and adherence to therapy? J Asthma. 2008;45:33–7. doi: 10.1080/02770900701815552. [DOI] [PubMed] [Google Scholar]
- 58.Apter AJ, Boston RC, George M, Norfleet AL, Tenhave T, Coyne JC, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it’s not just black and white. J Allergy Clin Immunol. 2003;111:1219–26. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- 59.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. Jama. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 60.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 61.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 62.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24:325–34. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 64.Pearlman DN, Zierler S, Meersman S, Kim HK, Viner-Brown SI, Caron C. Race disparities in childhood asthma: does where you live matter? J Natl Med Assoc. 2006;98:239–47. [PMC free article] [PubMed] [Google Scholar]
- 65.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80–94. [PubMed] [Google Scholar]
- 66.Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio M, et al. Issues in identifying asthma and estimating prevalence in an urban school population. J Clin Epidemiol. 2002;55:870–81. doi: 10.1016/s0895-4356(02)00451-1. [DOI] [PubMed] [Google Scholar]
- 67.Claudio L, Stingone JA, Godbold J. Prevalence of childhood asthma in urban communities: the impact of ethnicity and income. Ann Epidemiol. 2006;16:332–40. doi: 10.1016/j.annepidem.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 68.Saha C, Riner ME, Liu G. Individual and neighborhood-level factors in predicting asthma. Arch Pediatr Adolesc Med. 2005;159:759–63. doi: 10.1001/archpedi.159.8.759. [DOI] [PubMed] [Google Scholar]
- 69.Juhn YJ, Sauver JS, Katusic S, Vargas D, Weaver A, Yunginger J. The influence of neighborhood environment on the incidence of childhood asthma: a multilevel approach. Soc Sci Med. 2005;60:2453–64. doi: 10.1016/j.socscimed.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 70.Ren XS, Amick BC, Williams DR. Racial/ethnic disparities in health: the interplay between discrimination and socioeconomic status. Ethn Dis. 1999;9:151–65. [PubMed] [Google Scholar]
- 71.Ellen IG, Mijanovich T, Dillman KN. Neighborhood effects on health: Exploring the links and assessing the evidence. J Urban Affairs. 2001;23:391–408. [Google Scholar]
- 72.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126:309–37. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 73.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 74.Claudio L, Tulton L, Doucette J, Landrigan PJ. Socioeconomic factors and asthma hospitalization rates in New York City. J Asthma. 1999;36:343–50. doi: 10.3109/02770909909068227. [DOI] [PubMed] [Google Scholar]
- 75.Choudhury AH, Gordian ME, Morris SS. Associations between respiratory illness and PM10 air pollution. Arch Environ Health. 1997;52:113–7. doi: 10.1080/00039899709602873. [DOI] [PubMed] [Google Scholar]
- 76.Berman BA, Wong GC, Bastani R, Hoang T, Jones C, Goldstein DR, et al. Household smoking behavior and ETS exposure among children with asthma in low-income, minority households. Addict Behav. 2003;28:111–28. doi: 10.1016/s0306-4603(01)00221-0. [DOI] [PubMed] [Google Scholar]
- 77.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: U.S. Departamento of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 78.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75:3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 79.Kozyrskyj AL, Mai XM, McGrath P, Hayglass KT, Becker AB, Macneil B. Continued exposure to maternal distress in early life is associated with an increased risk of childhood asthma. Am J Respir Crit Care Med. 2008;177:142–7. doi: 10.1164/rccm.200703-381OC. [DOI] [PubMed] [Google Scholar]
- 80.Mrazek DA, Klinnert MD, Mrazek P, Macey T. Early asthma onset: consideration of parenting issues. J Am Acad Child Adolesc Psychiatry. 1991;30:277–82. doi: 10.1097/00004583-199103000-00017. [DOI] [PubMed] [Google Scholar]
- 81.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005;5:23–9. doi: 10.1097/00130832-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 83.Wright RJ. Stress and atopic disorders. J Allergy Clin Immunol. 2005;116:1301–6. doi: 10.1016/j.jaci.2005.09.050. [DOI] [PubMed] [Google Scholar]
- 84.Sandberg S, Paton JY, Ahola S, McCann DC, McGuinness D, Hillary CR, et al. The role of acute and chronic stress in asthma attacks in children. Lancet. 2000;356:982–7. doi: 10.1016/S0140-6736(00)02715-X. [DOI] [PubMed] [Google Scholar]
- 85.Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker HA, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: the role of psychological stress. J Allergy Clin Immunol. 2006;117:1014–20. doi: 10.1016/j.jaci.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 86.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 87.McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. Gen Hosp Psychiatry. 2007;29:214–22. doi: 10.1016/j.genhosppsych.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Opolski M, Wilson I. Asthma and depression: a pragmatic review of the literature and recommendations for future research. Clin Pract Epidemol Ment Health. 2005;1:18. doi: 10.1186/1745-0179-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.ten Brinke A, Ouwerkerk ME, Zwinderman AH, Spinhoven P, Bel EH. Psychopathology in patients with severe asthma is associated with increased health care utilization. Am J Respir Crit Care Med. 2001;163:1093–6. doi: 10.1164/ajrccm.163.5.2004020. [DOI] [PubMed] [Google Scholar]
- 90.Alegría M, Pescosolido B, Canino G. A Socio-Cultural Framework for Mental Health and Substance Abuse Service Disparities. In: Sadock BJ, Sadock VA, Ruiz P, editors. Comprehensive Textbook of Psychiatry. Baltimore: Wolters Kluwer Health, Lippincott Williams & Wilkins; in press. [Google Scholar]
- 91.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93:248–55. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health. 2005;95:260–5. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Apter AJ. The influence of health disparities on individual patient outcomes: what is the link between genes and environment? J Allergy Clin Immunol. 2006;117:345–50. doi: 10.1016/j.jaci.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 95.Joseph CL, Williams LK, Ownby DR, Saltzgaber J, Johnson CC. Applying epidemiologic concepts of primary, secondary, and tertiary prevention to the elimination of racial disparities in asthma. J Allergy Clin Immunol. 2006;117:233–40. doi: 10.1016/j.jaci.2005.11.004. quiz 41-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Passel J, Cohen D. Pew Research Center: Social & Demographic Trends. Washington, DC: 2008. Immigrant to play lead role in future US growth. [Google Scholar]