Abstract
Injection of the neurolytic agents into motor points of the biceps brachii or brachialis muscles is an effective treatment of spasticity of the elbow flexors in many stroke survivors. Accurate localization of the motor points of each muscle is necessary for enhancing the efficacy of motor point blocks. To identify the precise locations of the motor points (terminal nerve endings) of the biceps brachii and brachialis muscles in relation to anatomic surface landmarks for motor point blocks, we dissected 23 limbs from 12 cadavers. A reference line was defined as a line connecting the coracoid process with the lateral epicondyle of the humerus. The location of the motor points of the biceps brachii and brachialis muscles was identified in reference to the reference line. The motor point of the biceps brachii muscle was found to be approximately half of the reference line. In the brachialis muscle, the location of the motor point was 70% of the reference line from the coracoid process and 2 cm medial to the line. The results are expected to facilitate effective localization of the motor point block of these muscles in selective motor nerve block.
Keywords: Elbow, Flexor, Muscle Spasticity, Nerve Endings, Nerve Block
INTRODUCTION
Elbow flexion synergy of stroke survivors may occur reflexively or as early stages of voluntary control when spasticity is present. However, when spasticity of the elbow flexors is marked, it may contribute to the typical upper extremity posture in hemiplegia and limit rehabilitation efforts to improve function or at least minimize impairments (1). For patients who are ambulatory, walking with the elbow flexed impairs balance and may be cosmetically unacceptable. The patients with spasticity of the elbow flexion are most likely to show the pronation of the forearm, which is not performed by the biceps brachii. Furthermore, a major flexor of the elbow is the brachialis muscle, that has no role in supination (2). Thus, blocking the brachialis is expected to reduce spasticity of elbow flexion without eliminating the ability to generate supination torques.
Chemodenervation of the musculocutaneous nerve with neurolytic agents is an effective treatment of spasticity of the elbow flexors. The flexion spasticity at the elbow can be treated using injections of neurolytic agents designed to block the musculocutaneous nerve at the level of the axilla or upper arm (3-6). Blocking the main nerve trunk may produce profound weakness of the hemiparetic upper extremity (7, 8). Neurolytic agents may be spilled over the adjacent arteries and have a direct effect on vascular smooth muscles, resulting in a significant vasoconstriction (9). There might be temporary dysesthetic pain over the distribution of the lateral antebrachial cutaneous nerve after neurolysis (8, 10).
To avoid undesirable complications, motor point blocks of the biceps brachii or brachialis muscle may be more satisfactory. For phenol or alcohol neurolysis, precise localization of the motor points of each muscle is necessary to avoid blocking the sensory or major motor nerve. Previous anatomic studies have defined the motor point as the location where the motor branch entered the muscle belly (11, 12). However, there have been few studies that have investigated the location of the motor points of the biceps brachii and brachialis muscles. The present study, therefore, was conducted to identify the location of the motor points of these muscles relative to anatomic landmarks in order to facilitate the efficacy of motor point block.
MATERIALS AND METHODS
Twenty-three limbs from 12 cadavers were dissected for the study. There were 5 male and 7 female cadavers with an average age at time of death of 66 yr (range, 31 to 87). One limb was unsuitable for the study due to significant contracture of the elbow joint. Each cadaver was placed supine with the elbow extended in the anatomic position.
The skin and subcutaneous tissue were dissected from the elbow crease, exposing the entire biceps brachii. After cutting the biceps brachii tendon at the elbow, the muscle was detached from the brachialis. The musculocutaneous nerve was identified and the branches to the brachialis and biceps brachii were observed. The center of the location where the motor branch entered the muscle belly was designated as the motor point of each muscle.
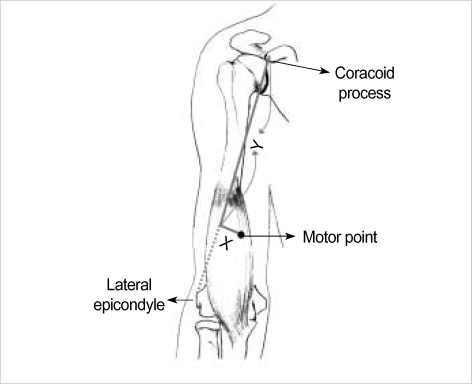
A tape measure was used to form a reference line connecting the coracoid process to the lateral epicondyle of the humerus (Fig. 1). For the brachialis muscle, the perpendicular line from the reference line to the motor point was measured and was recorded as an X value. The Y value was defined as the distance from the coracoid process to the point where the perpendicular line crossed the reference line. For the biceps brachii muscle, the X value was not measured as the location of the motor point was not fixed in a transverse plane after cutting the muscle at the elbow. The shortest distance between the coracoid process and the motor point was measured and was defined as the Y value. For both muscles, the Y value was also normalized into a percentage of the total length of the reference line and hence compared across all specimens.
Fig. 1.
Diagrammatic drawing of measurement of the location of the motor point of the brachialis muscle. The coracoid process and lateral epicondyle of the humerus were identified as reference points. The shortest distance between the reference points was measured and was defined as a reference line. The distance from the reference line to the motor point was recorded as an x value and the distance from the coracoid process to the point where the perpendicular line crossed the reference line was defined as a y value.
RESULTS
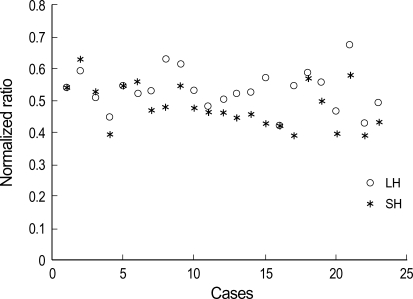
The mean length of the reference line between the coracoid process and the lateral epicondyle of the elbow was 26.76±1.59 cm. Each head of the biceps muscle was consistently innervated by a single branch of the nerve, respectively. The motor points of the biceps brachii were found to be approximately half of the distance from the coracoid process to the lateral epicondyle of the humerus (Fig. 2). The motor point of the short head of the biceps muscle was located 12.91±1.99 cm (48.24±6.88% of the reference line) distal to the coracoid process. In the long head of the muscle, the location of the motor point from the coracoid process was 14.22±1.75 cm (53.19±6.21%).
Fig. 2.
A plot of the location of the motor points in the biceps brachii muscles. The normalized ratio indicates the ratio of the distance from the coracoid process to the length of the reference line connecting from the coracoid process to the lateral epicondyle of the humerus. SH, short head; LH, long head.
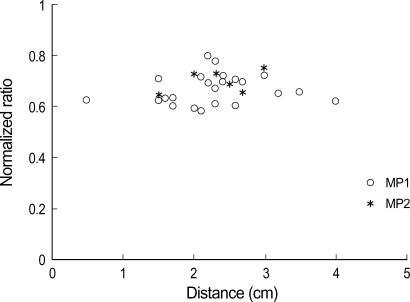
All brachialis muscles were innervated by one or two branches of the musculocutaneous nerve (seventeen with one branch and six with two branches); 7 arms also received a branch from the radial nerve. The first motor point of the brachialis muscle innervated by the musculocutaneous nerve was found to be 2.28±0.74 cm medial to the reference line (x value) and 17.84±1.77 cm (66.73±5.95%) of the reference line distal to the coracoid process (y value) (Fig. 3). The location of the second motor point was 2.33±0.53 cm in the x value and 18.57±1.98 cm (70.09±4.41%) in the y value. The motor point of the brachialis from a branch of the radial nerve was found to be 0.76±0.77 cm in the x value and 18.90±2.95 cm (70.19±10.61%) in the y value.
Fig. 3.
A plot of the location of the motor points in the brachialis muscle; x axis is the distance from the reference line to the motor point and y axis is the distance from the coracoid process to the point where the perpendicular line crosses the reference line. MP1, the first motor point; MP2, the second motor point.
DISCUSSION
Our study demonstrated that the motor point of the brachialis muscle was found to be approximately 70% of the reference line from the coracoid process to the lateral epicondyle of the elbow and 2 cm medial to the line. Buchanan and Erickson (13) performed anatomic dissections on 26 arms from 13 cadavers. They observed that the motor point of the biceps muscle was located at 53% of the length of the humerus and that of the brachialis was found to be distal one third of the humerus. These results are consistent with those of our dissection study. However, they did not document a horizontal location (the perpendicular distance from the reference line) of the motor point of the brachialis because they considered that its motor point could be best blocked from the medial side. Recently, Kim et al. (14) also reported similar results with no consideration of the horizontal distance.
The approach from the medial side of the arm is carried out by lifting adjacent neurovascular bundles along with the biceps brachii muscle (5). The brachial artery or the median nerve may be injured if these structures are not adequately lifted ventrally in cases of severe flexion spasticity. We need to predict the depth of the needle insertion to avoid passing through the motor nerve branches of the musculocutaneous nerve. Based on our data, an anterior approach may be considered; the needle is located approximately 2 cm medial to 70% of the reference line from the coracoid process to the lateral epicondyle of the elbow. However, the needle has to pass through the biceps brachii with the potential of minor spilling of the neurolytic agent. Further detailed studies are needed to determine any negative effect of the anterior approach on functional status.
The nerve supply to the brachialis muscle has not been clearly understood. Recently, standard testbooks of anatomy des- cribe a contribution from the radial nerve to inferolateral portion of this muscle but do not mention its incidence (15, 16). Ip and Chang (17) reported that the brachialis receives a constant innervation from the radial nerve in eight Chinese cadavers. Mahakkanukrauh and Somsarp (18) investigated the dual innervation of the brachialis muscle in 152 Thai cadaveric limbs. They found that all brachialis muscles received innervation from the musculocutaneous nerve and the radial nerve provided a dual supply in 81.6% of cases. These results imply that the musculocutaneous nerve or motor point block may not completely paralyze the brachialis muscle. The functional significance of the radial branch to brachialis has not been reported. The size of the motor distribution from the radial branch to brachialis may be variable (17, 18).
Blackburn et al. (19) recently reported the radial innervation of the brachialis in 42 UK Caucasian cadaveric limbs. They found that a radial nerve contribution to the innervation of the brachialis was present in 67% of cases, less than the incidence reported by previous studies. In our study, the dual innervation, occurred in a higher proportion of specimens than 30.4%. This may reflect interracial or ethnic differences in embryological development, or may be due to the small number of specimens. In our study, the motor point of the brachialis from a branch from the radial nerve was located approximately 1 cm lateral to the motor point from the musculocutaneous nerve innervation. Thus, if a motor point block of the brachialis muscle is not successful, there might be the possibility of a radial contribution which may require more lateral additional block.
According to our study, the motor point of the biceps brachii is likely to be located at approximately the halfway point of the upper arm. The motor point can be easily identified by the use of a surface stimulator on the skin of the mid arm. A needle electrode is then used to more accurately determine the location of the motor points of the muscle. In addition, our data may be helpful in determination of the recording location of the biceps muscle. In standard needle electromyography, the needle electrode is placed over the bulk of the biceps muscle (20). The lack of knowledge regarding the location of the motor points of the biceps muscle may lead to an erroneous placement of the needle electrode because the maximum bulk of the muscle may be found more distally in elbow extension.
In summary, the motor point of the biceps brachii muscle was located at approximately half of the arm. In the brachialis muscle innervated by one or two branches of the musculocutaneous nerve, the location of the motor points was likely to be 2 cm medial to distal one third of a reference line from the coracoid process to the lateral condyle of the elbow. Our results may allow precise localization of the motor points and offer more accurate approach. To validate this anatomic work in clinical practice, further clinical studies will be needed to compare therapeutic effects of selective motor point block with those of the musculocutaneous nerve block.
References
- 1.Mizrahi EM, Angel RW. Impairment of voluntary movement by spasticity. Ann Neurol. 1979;5:594–595. doi: 10.1002/ana.410050620. [DOI] [PubMed] [Google Scholar]
- 2.Calais-Germain B. The elbow. In: Anderson S, editor. Anatomy of movement. Seattle: Eastland Press; 1993. pp. 131–146. [Google Scholar]
- 3.Keenan MA, Tomas ES, Stone L, Gersten LM. Percutaneous phenol block of the musculocutaneous nerve to control elbow flexor spasticity. J Hand Surg Am. 1990;15:340–346. doi: 10.1016/0363-5023(90)90120-g. [DOI] [PubMed] [Google Scholar]
- 4.Garland DE, Rhoades ME. Orthopedic management of brain-injured adults. Part II. Clin Orthop Relat Res. 1978;131:111–122. [PubMed] [Google Scholar]
- 5.Keenan MA. Management of the spastic upper extremity in the neurologically impaired adult. Clin Orthop Relat Res. 1988;233:116–125. [PubMed] [Google Scholar]
- 6.Khalili AA, Betts HB. Isolated block of musculocutaneous and perineal nerves in the management of spasticity with special reference to the use of a nerve stimulator. Anesthesiology. 1967;28:219–222. [PubMed] [Google Scholar]
- 7.Garland DE, Thompson R, Waters RL. Musculocutaneous neurectomy for spastic elbow flexion in non-functional upper extremities in adults. J Bone Joint Surg Am. 1980;62:108–112. [PubMed] [Google Scholar]
- 8.Glenn MB. Nerve blocks for the treatment of spasticity. In: Katz RT, editor. Physical medicine and rehabilitation: state of the art reviews. Philadelphia: Hanley & Belfus; 1994. pp. 481–505. [Google Scholar]
- 9.Johnson ME, Sill JC, Brown DL, Halsey TJ, Uhl CB. The effect of the neurolytic agent ethanol on cytoplasmic calcium in arterial smooth muscle and endothelium. Reg Anesth. 1996;21:6–13. [PubMed] [Google Scholar]
- 10.Kong KH, Chua KS. Neurolysis of the musculocutaneous nerve with alcohol to treat poststroke elbow flexor spasticity. Arch Phys Med Rehabil. 1999;80:1234–1236. doi: 10.1016/s0003-9993(99)90021-7. [DOI] [PubMed] [Google Scholar]
- 11.Albert T, Yelnik A, Colle F, Bonan I, Lassau JP. Anatomic motor point localization for partial quadriceps block in spasticity. Arch Phys Med Rehabil. 2000;81:285–287. doi: 10.1016/s0003-9993(00)90072-8. [DOI] [PubMed] [Google Scholar]
- 12.Kim HS, Hwang JH, Lee PK, Kwon JY, Oh-Park MY, Kim JM, Chun MH. Localization of the motor nerve branches and motor points of the triceps surae muscles in Korean cadavers. Am J Phys Med Rehabil. 2002;81:765–769. doi: 10.1097/00002060-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Buchanan TS, Erickson JC. Selective block of the brachialis motor point. An anatomic investigation of musculocutaneous nerve branching. Reg Anesth. 1996;21:89–92. [PubMed] [Google Scholar]
- 14.Kim JS, Kwon JY, Kang SY, Park JW. Anatomical locations of the motor points of the biceps brachii and brachialis muscles. J Korean Acad Rehabil Med. 2004;28:592–595. [Google Scholar]
- 15.Jenkins DB. Hollinshead's functional anatomy of the limbs and back. 8th ed. Philadelphia: Saunders; 2002. [Google Scholar]
- 16.Johnson D, Ellis H. Upper arm. In: Standring S, Ellis H, Healy JC, Johnson D, Williams A, Collins P, Wigley C, editors. Gray's anatomy: the anatomical basis of clinical practice. 39th ed. Edinburgh: Churchill Livingstone; 2005. pp. 851–858. [Google Scholar]
- 17.Ip MC, Chang KS. A study on the radial supply of the human brachialis muscle. Anat Rec. 1968;162:363–371. doi: 10.1002/ar.1091620311. [DOI] [PubMed] [Google Scholar]
- 18.Mahakkanukrauh P, Somsarp V. Dual innervation of the brachialis muscle. Clin Anat. 2002;15:206–209. doi: 10.1002/ca.10014. [DOI] [PubMed] [Google Scholar]
- 19.Blackburn SC, Wood CP, Evans DJ, Watt DJ. Radial nerve contribution to brachialis in the UK Caucasian population: position is predictable based on surface landmarks. Clin Anat. 2007;20:64–67. doi: 10.1002/ca.20244. [DOI] [PubMed] [Google Scholar]
- 20.DeLagi EF, Perotto A, Iazzetti J, Morrison D. Anatomic guide for the electromyographer the limbs. 2nd ed. Springfield (IL): Charles C Thomas; 1981. [Google Scholar]