Abstract
This study evaluated the prevalence of metabolic syndrome and investigated its association with being overweight in Korean adolescents. Data were obtained from 1,393 students between 12 and 13 yr of age in a cross-sectional survey. We defined the metabolic syndrome using criteria analogous to the Third Report of the Adult Treatment Panel (ATP III) as having at least three of the following: fasting triglycerides ≥100 mg/dL; HDL <50 mg/dL; fasting glucose ≥110 mg/dL; waist circumference >75th percentile for age and gender; and systolic blood pressure >90th percentile for age, gender, and height. Weight status was assessed using the age- and gender-specific body mass index (BMI), and a BMI ≥85th percentile was classified as overweight. Of the adolescents, 5.5% met the criteria for the metabolic syndrome, and the prevalence increased with weight status; it was 1.6% for normal weight and 22.3% in overweight (p<0.001). In multivariate logistic regression analyses among adolescents, overweight status was independently associated with the metabolic syndrome (odds ratio, 17.7; 95% confidence interval, 10.0-31.2). Since childhood metabolic syndrome and obesity likely persist into adulthood, early identification helps target interventions to improve future cardiovascular health.
Keywords: Metabolic Syndrome, Overweight, Adolescents
INTRODUCTION
The third National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP III) defines the metabolic syndrome as the presence of at least three of the following five risk factors in an individual: central or abdominal obesity, hypertriglyceridemia, hypertension, low HDL-cholesterol, and high fasting glucose levels. The metabolic syndrome is a major risk factor for cardiovascular disease and type 2 diabetes (1, 2). Components of the metabolic syndrome are present in children and adolescents, as well as in adults (3). However, the metabolic syndrome has not been well characterized in children or adolescents in terms of criteria, prevalence, or clinical implications, although studies have examined abnormalities caused by the metabolic syndrome (4, 5).
The incidence of overweight children and adolescents has been increasing in Asia with urbanization and economic development (6). Over the past 10 yr, the rate of overweight Korean children and adolescents aged 5-20 yr has doubled (7). Obesity is associated with dyslipidemia (8), type 2 diabetes (9), and long-term vascular complications (10, 11).
The prevalence of the metabolic syndrome is high in obese children and adolescents, and increases with the degree of obesity. In a sample of adolescents in the United States who were included in the third National Health and Nutrition Examination Survey (NHANES III) conducted between 1988 and 1994, the prevalence of the metabolic syndrome was 6.8% among overweight adolescents and 28.7% among obese adolescents (5, 12).
In Korea, the metabolic syndrome in adolescents has not been studied in the criteria for diagnosis, prevalence or risk factors. Therefore, this study examined the prevalence of metabolic syndrome based on the criteria proposed by de Ferranti et al. (13), and investigated the association between being overweight and the metabolic syndrome in first-year middle school students in Korea.
MATERIALS AND METHODS
Study subjects
The Dong-gu District in Gwangju city is a well-defined geographic area that includes seven middle schools. The subjects were recruited from first-year students in these seven middle schools. All 1,393 students completed a questionnaire survey, underwent a physical examination and had blood drawn after fasting for at least 12 hr. This study did not obtained written informed consent from all parents and children before any testing procedures and was not approved by the institutional review board.
Questionnaire survey
The study subjects were evaluated using a self-administerd questionnaire to determine family medical history, current health status, self-reported experience about smoking, drinking and exercising regularly, and socioeconomic and demographic information.
Anthropometric measurement
Height and weight were measured using an automatic height-weight scale to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2). Overweight and obesity were determined using data form the 1998 Korean Association of Pediatrics growth charts for Koreans (14). Those with a BMI <85th percentile were classified as normal weight; those with a BMI ≥85th percentile, but <95th percentile, were classified as overweight; those with a BMI ≥95th percentile were considered obese; and all those with a BMI ≥85th percentile were classified as overweight and obese (15). Using a fiberglass tape measure, waist circumference was measured at the midpoint between the bottom of the rib cage and the top of the iliac crests.
Measuring metabolic risk factors
The components of the metabolic syndrome (blood pressure, fasting glucose, triglycerides, and HDL-cholesterol concentrations), as well as the total serum cholesterol concentration, were measured in all subjects.
Blood pressure was measured twice with a mercury sphygmomanometer while the subjects were seated after 10 min of rest, and the two measurements were averaged for analysis.
After a 12-hr overnight fast, blood samples were drawn from an antecubital vein in each subjects into vacutainer tubes. Fasting glucose concentration was measured using the glucose oxidase method, and total cholesterol and triglycerides levels were measured using enzymatic procedures with an autoanalyzer (model 747; Hitachi, Tokyo, Japan). The HDL-cholesterol fraction was measured enzymatically after precipitating the lipoproteins containing apo-B with MnCl2.
Definition of the metabolic syndrome
The definition of the metabolic syndrome used in this study was that for adolescents proposed by de Ferranti et al. (13), their cirteria were based closely on the ATP III, which uses waist circumference as a measure of central obesity; percentiles for age and gender were those most often associated with central obesity in children across genders and races (16). Therefore, adolescents who had a waist circumference ≥70th percentile for age and gender from our sample population were classified as having central obesity. Systolic hypertension was defined as having blood pressure values ≥90th percentile for age, gender, and height (17). Participants were classified as having hypertriglyceridemia if they had ≥100 mg/dL, low HDL if they had values <50 mg/dL, and elevated fasting glucose if they had serum glucose values ≥110 mg/dL (18). Individuals with at least three of these abnormalities were defined as having the metabolic syndrome.
Statistical methods
The data are expressed as frequencies or as means with standard deviations. The prevalence of the metabolic syndrome was calculated overall and by gender. The methods used for analysis were the χ2-test and multivariate logistic regression analysis using the computer software SPSS version 12.0 software (SPSS Inc., Chicago, IL, U.S.A.). Statistical significance was established at p<0.05. The results of the logistic regression analysis are expressed as odds ratios with 95% confidence intervals.
RESULTS
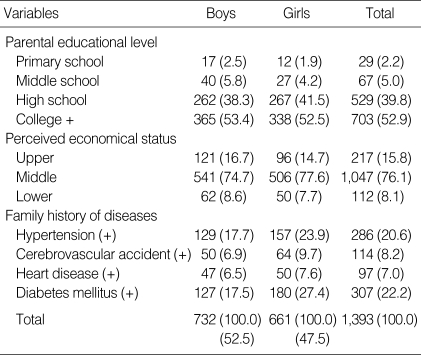
The descriptive characteristics of the students separated by gender are presented in Table 1, 2. The prevalence of family history of hypertension and diabetes were 20.6% and 22.2%, respectively. The mean (standard deviation) age of the students was 12.8 (0.4) yr, and various characteristics were similar to both genders.
Table 1.
Distribution of general characteristics of the students (Unit: person (%))
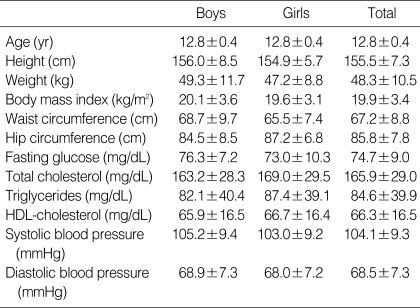
Table 2.
Clinical and biochemical characteristics of the students
Data are means±standard deviations.
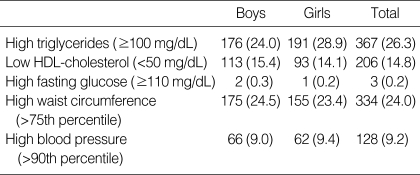
The prevalence of individual components of the metabolic syndrome was 26.3% for high triglycerides, 14.8% for low HDL-cholesterol, 0.2% for impaired fasting glucose, 24.0% for abnormal waist circumference, and 9.2% for high blood pressure (Table 3).
Table 3.
Prevalence of individual metabolic abnormalities by gender (Unit: person (%))
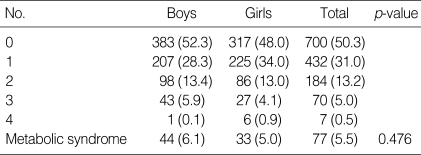
Nearly half (49.7%) of students had at least one metabolic abnormality, and 5.5% had the metabolic syndrome. In boys and girls, the prevalence of metabolic syndrome was 6.1% and 5.0%, respectively; the differences was not statistically significant. Four abnormalities were found in seven students (0.5%), while no student met all five criteria (Table 4).
Table 4.
Prevalence of the number of risk factors of the metabolic syndrome (Unit: person (%))
Tested by chi-square test.
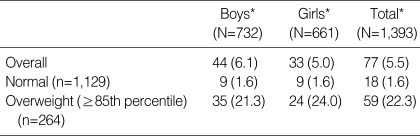
Compared to normal-weight students, overweight students had a higher prevalence of the metabolic syndrome (1.6% vs. 22.3%), and the difference was statistically significant (p<0.001) (Table 5).
Table 5.
Prevalence of the metabolic syndrome by weight status (Unit: person (%))
*Normal-overweight comparison significant at p<0.001.
In the multivariate logistic regression, being overweight was independently associated with the metabolic syndrome after adjusting for gender, age, family history of hypertension and diabetes mellitus, regular exercise and amount of meals (odds ratio, 17.7; 95% confidence interval, 10.0-31.2) (Table 6).
Table 6.
Association in multivariate analysis of weight status with metabolic syndrome in adolescents
*Results were adjusted for age, gender, family history of hypertension and diabetes mellitus, regular exercise, and amount of meals.
DISCUSSION
Although no universally accepted definition for the metabolic syndrome in adolescents has been formulated, the definition of Cook et al. (5) has been uesd most widely. However, this definition is based on the 1992 National Cholesterol Education Program guidelines; thus the definition had been devised before ATP III and wide recognition of the metabolic syndrome, using more restrictive cutoffs for lipids and abdominal circumference. Translating their definition to pediatric percentiles, HDL cholesterol levels of 40 mg/dL represents the 10th to 25th percentile in boys and 10th to 15th percentile in girls, which are below the adult 40th percentile. The higher triglyceride cutpoint of 110 mg/dL represents the 85th to 95th pediatric percentiles, also higher than the adult 75th to 85th percentiles. The abdominal circumference cutpoint of the 90th percentile is higher than the 75th percentile used in the definition by de Ferranti et al. (13).
In addition to definition by Cook et al. (5), other definitions of pediatric metabolic syndrome have been used in various populations (5, 12, 18, 19). In contrast to other criteria, the definition used here given by de Ferranti et al. (13) was based closely on the more inclusive ATP III adult criteria, considering the effects of age, gender, and puberty, and therefore, encompasses a larger population of adolescents.
Using a pediatric definition based closely on ATP III, we found that the prevalence of the metabolic syndrome in Korean adolescents aged 12 and 13 yr was 5.5%. The metabolic syndrome was most common in overweight adolescents, with a prevalence of 22.3%, compared to only 1.6% for normal-weight adolescents. Moreover, nearly half of all students had at least one metabolic abnormality. The difference in the prevalence of the metabolic syndrome between overweight and normal-weight adolescents was remarkable and further underscores the importance of small losses of weight for potentially avoiding the development of the metabolic syndrome and related sequelae. Our finding is similar to other published results (5, 20).
The mechanisms underlying the development of the metabolic derangements that occur in the metabolic syndrome are not fully understood. The most widely accepted hypothesis involves a complex interaction between insulin resistance and obesity that is modified by social, environmental, and genetic factors (21, 22). Pediatric researchers have found that they persist from childhood to adulthood, leading one to suspect that the metabolic syndrome also continues into adulthood (18). In fact, childhood obesity predicts the development of the metabolic syndrome in adulthood (23). The metabolic syndrome has an important immediate impact: adolescents with the metabolic syndrome have a lower exercise capacity than obese and normal-weight controls (24). Obesity alone increases the risk of hypertension, cholecystitis, and slipped capital femoral epiphysis, and is associated with psychosocial symptoms in children (25).
Several limitations of these data should be considered. Our study subjects were 12 or 13-yr old first-year middle school students from one district of a city. In addition, the blood pressure and waist circumference criteria were derived from percentiles of our subjects. Therefore, caution should be exercised when generalizing these data to other Korean adolescents.
In this study, the metabolic syndrome was found to exist almost entirely in overweight students. Our data suggest that the prevalence of the metabolic syndrome among adolescents will increase unless effective obesity prevention efforts are implemented for youths. Practitioners should be aware of the clustering of metabolic abnormalities in adolescents, and affected students should receive risk-reducing interventions. Understanding the prevalence of the metabolic syndrome among adolescents may foster interventions and research; further investigation might better illuminate its pathophysiology and relationship to cardiovascular disease.
ACKNOWLEDGMENTS
We sincerely thank the Department of Public Health of Gwang-ju, the members of the visiting health team from Dong-gu Public Health Center and the middle schools and their students for their kind help in collecting our data.
Footnotes
This work was supported by research funds from Activity Group for Chronic Disease Management in Gwang-ju, 2005.
References
- 1.Ford ES, Giles WH. A comparison of the prevalence of the metabolic syndrome using two proposed definitions. Diabetes Care. 2003;26:575–581. doi: 10.2337/diacare.26.3.575. [DOI] [PubMed] [Google Scholar]
- 2.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 3.Jiang X, Srinivasan SR, Webber LS, Wattigney WA, Berenson GS. Association of fasting insulin level with serum lipid and lipoprotein levels in children, adolescents and young adults: the Bogalusa Heart Study. Arch Int Med. 1995;155:190–196. [PubMed] [Google Scholar]
- 4.Ronnemaa T, Knip M, Lautala P, Viikari J, Uhari M, Leino A, Kaprio EA, Salo MK, Dahl M, Nuutinen EM. Serum insulin and other cardiovascular risk indicators in children, adolescents and young adults. Ann Med. 1991;23:67–72. doi: 10.3109/07853899109147933. [DOI] [PubMed] [Google Scholar]
- 5.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 6.Sakamoto N, Wansorn S, Tontisirin K, Marui E. A social epidemiologic study of obesity among preschool children in Thailand. Int J Obes Relat Metab Disord. 2001;25:389–394. doi: 10.1038/sj.ijo.0801477. [DOI] [PubMed] [Google Scholar]
- 7.Rho JH, Lee DW, Choi JM. Prevalence of childhood obesity in Korea. J Korean Pediatr Soc. 2001;44:208. [Google Scholar]
- 8.Goran MI, Gower BA. Abdominal obesity and cardiovascular risk in children. Coron Artery Dis. 1998;9:483–487. doi: 10.1097/00019501-199809080-00003. [DOI] [PubMed] [Google Scholar]
- 9.Arslanian S. Type 2 diabetes in children: clinical aspects and risk factors. Horm Res. 2002;57(Suppl 1):19–28. doi: 10.1159/000053308. [DOI] [PubMed] [Google Scholar]
- 10.Berenson GS, Srinivasan SR, Bao W, Newman WP, III, Rracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 11.Steinberger J, Daniels SR. Obesity, insulin resistance, diabetes, and cardiovascular risk in children: an American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism) Circulation. 2003;107:1448–1453. doi: 10.1161/01.cir.0000060923.07573.f2. [DOI] [PubMed] [Google Scholar]
- 12.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 13.de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in american adolescents: findings from the third National Health and Nutrition Examination Survey. Circulation. 2004;110:2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 14.Korean Association of Pediatrics. 1998 KAP growth charts: Korea. In: Hong CE, editor. Pediatrics. Seoul: Daehan; 2002. p. 1245. [Google Scholar]
- 15.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations: the Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics. 1998;102:E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 16.Daniels SR, Khoury PR, Morrison JA. Utility of different measures of body fat distribution in children and adolescents. Am J Epidemiol. 2000;152:1179–1184. doi: 10.1093/aje/152.12.1179. [DOI] [PubMed] [Google Scholar]
- 17.National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98:649–658. [PubMed] [Google Scholar]
- 18.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27(Suppl 1):S5–S10. doi: 10.2337/diacare.27.2007.s5. [DOI] [PubMed] [Google Scholar]
- 19.Katzmarzyk PT, Pérusse L, Malina RM, Bergeron J, Després JP, Bouchard Cl. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: the Quebec Family Study. J Clin Epidemiol. 2001;54:190–195. doi: 10.1016/s0895-4356(00)00315-2. [DOI] [PubMed] [Google Scholar]
- 20.Chu NF, Rimm EB, Wang DJ, Liou HS, Shieh SM. Relationship between anthropometric variables and lipid levels among school children: the Taipei Children Heart Study. Int J Obes Relat Metab Disord. 1998;22:66–72. doi: 10.1038/sj.ijo.0800546. [DOI] [PubMed] [Google Scholar]
- 21.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kaartashov AI, Ludwig DS. Diary consumption, obesity and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287:2081–2089. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 22.Reaven GM. Insulin resistance and compensatory hyperinsulinemia: role in hypertension, dyslipidemia, and coronary heart disease. Am Heart J. 1991;121(pt 2):1283–1288. doi: 10.1016/0002-8703(91)90434-j. [DOI] [PubMed] [Google Scholar]
- 23.Liese AD, Mayer-Davis EJ, Tyroler HA, Davis CE, Keil U, Duncan BB, Heiss G. Development of the multiple metabolic syndrome in the ARIC cohort: joint contribution of insulin, BMI, and WHR: Atherosclerosis Risk in Communities. Ann Epidemiol. 1997;7:407–416. doi: 10.1016/s1047-2797(97)00047-1. [DOI] [PubMed] [Google Scholar]
- 24.Vanhala MJ, Vanhala PT, Keinanen-Kiukaanniemi SM, Kumpusalo EA, Takala JK. Relative weight gain and obesity as a child predict metabolic syndrome as an adult. Int J Obes Relat Metab Disord. 1999;23:656–659. doi: 10.1038/sj.ijo.0800898. [DOI] [PubMed] [Google Scholar]
- 25.Torok K, Szelenyi Z, Porszasz J, Molnar D. Low physical performance in obese adolescent boys with metabolic syndrome. Int J Obes Relat Metab Disord. 2001;25:966–970. doi: 10.1038/sj.ijo.0801646. [DOI] [PubMed] [Google Scholar]
- 26.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]