Abstract
This study was performed to determine the incidence and seroprevalence of hepatitis A virus (HAV) infections in young soldiers in the Republic of Korea Army. From January 2000 through December 2004, a total of 147 hepatitis A cases were reported to the Armed Forces Medical Command. The annual incidence rates were 7.4 per 100,000 persons in 2000, 1.6 in 2001, 4.4 in 2002, 9.8 in 2003, and 6.2 in 2004, based on the reported cases among approximately 500,000 soldiers. All patients were males with a median age of 21 yr (range, 19-27). The most common symptom was nausea (86.5%), and all patients had recovered without complications. In addition, in order to evaluate the seroprevalence of HAV infection in young adults, serum samples were obtained from randomly selected young subjects among those who had been admitted to the Armed Forces Capital Hospital from September 2005 to February 2006. A total of 200 subjects were enrolled in the study to analyze the anti-HAV immune status. The overall anti-HAV IgG seropositive rate was 2% (4/200, 95% CI, 0.60-5.21%). Given the changing epidemiology of the disease and the associated increase in morbidity, it was suggested that the routine HAV vaccination for Korean military personnel might be necessary.
Keywords: Hepatitis A, Incidence, Military Personnel, Seroprevalence
INTRODUCTION
Viral hepatitis is a major public health problem throughout the world. Although hepatitis A virus (HAV) infection is a self-limited disease, the infection in adults causes significant morbidity, resulting in long absences from work for several weeks, possible hospitalization, and occasional mortality resulting from acute fulminant hepatitis (1, 2). Infection rates have declined with better hygiene practice and public sanitation, but remain heterogeneous across geographic and socioeconomic strata (1, 2).
Hepatitis A has become a major cause of acute viral hepatitis in young adults in Korea since 1996 (3-7). Korea seems to be a country in transition from a high to low endemic region and faces the paradox of increasing disease burden with decreasing disease incidence. The current national immunization guide recommends HAV vaccination for individuals at increased risk of infection or its complications (3, 4). The guide also states that a universal immunization program should be considered, but further discussion is needed (3, 4).
Korea, has a draft system, and the military has been especially vigilant for viral hepatitis, since active disease not only impairs an individual's military readiness, but also can threaten a large number of troops. Military personnel are considered to have a higher risk for hepatitis A than the civilian population (8). However, there are no data available regarding HAV infection in Korean military personnel. Thus, the goal of this study was to determine the incidence rate and the prevalence of antibody to hepatitis A in young soldiers in the Republic of Korea (ROK) Army.
MATERIALS AND METHODS
The database of the Armed Forces Medical Command (Defense Medical Information System; DEMIS) was reviewed to identify the number of hepatitis A cases reported. In the ROK Army, it is mandatory to report individual cases of communicable diseases, including viral hepatitis, to the Department of Preventive Medicine in the Armed Forces Medical Command (9). We analyzed the data of hepatitis A cases that had been submitted from January 2000 to December 2004. The annual incidence rate was defined as cases per 100,000 persons per year among approximately 500,000 soldiers. The cases were defined as epidemic cases when more than two cases had occurred in the same military unit within a 4-week period. We retreived data from electronic medical records (DEMIS) and obtained baseline demographic and clinical information, including age, gender, clinical symptoms, and laboratory findings.
In addition, we planned an additional study in order to evaluate the seroprevalence of HAV infection. Serum samples were obtained from randomly selected subjects among those who had been admitted to the Armed Forces Capital Hospital from September 2005 to February 2006. Patients who are over 25 yr old, chronic disease cases, viral hepatitis cases, and females were excluded. We, therefore, planned to obtain a specific study group that included healthy young military personnel. Informed consent was obtained. Anti-HAV IgG and anti-HBs IgG antibodies were measured by AXSYM (Abbott Laboratories, Wiesbaden, Germany). The test was performed in an automated format, and cut-off values were established according to the instructions by the manufacturer.
RESULTS
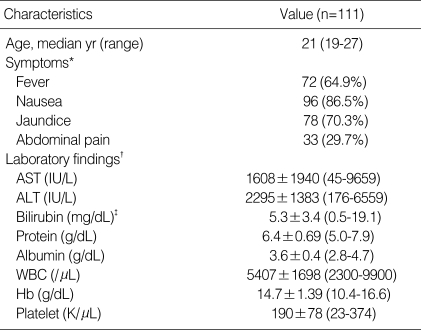
A total of 147 cases of hepatitis A were reported in young Korean soldiers from January 2000 through December 2004. Of these, 64 (43.5%) cases were reported as epidemic cases, and the remaining 83 (56.5%) were reported as sporadic cases (Table 1). The mean annual incidence of hepatitis A was 5.9 per 100,000 persons, based on the cases reported among approximately 500,000 soldiers. The annual incidence rates were 7.4 per 100,000 persons in 2000, 1.6 in 2001, 4.4 in 2002, 9.8 in 2003, and 6.2 in 2004. A total of 111 male patients with acute hepatitis A were analyzed and their median age was 21 yr old (range, 19 to 27 yr). The remaining 36 cases were excluded from the analysis since the medical records were unavailable. Table 2 shows clinical characteristics and initial laboratory findings of patients with acute hepatitis A in the military personnel of Korea. The most common symptom was nausea (86.5%), and all patients had recovered without complications.
Table 1.
Annual incidence of the hepatitis A cases reported among young Korean soldiers
Table 2.
Clinical characteristics and initial laboratory findings of patients with acute hepatitis A in the military personnel of Korea
*Values are reported as no. (%) of patients unless otherwise indicated.
†Values are reported as mean±standard deviation (range). ‡Peak bilirubin level (mg/dL); 7.2±4.6 (1.8-22.9).
A total of 200 subjects were enrolled in the study to analyze anti-HAV immune status. All patients were male with a median age of 21 yr (range, 19-24). The overall anti-HAV IgG seropositive rate was 2% (4/200, 95% CI, 0.60-5.21%). The prevalence of anti-HBs IgG was detected as 72.9% (146/200, 95% CI, 66.44-78.69%).
DISCUSSION
In this study of HAV infections among Korean soldiers, the data suggested that the annual incidence of hepatitis A was approximately 6 per 100,000 persons. The cases of hepatitis A reported have sustained steadily over the past 5 yr, and 11 outbreaks in the military personnel have been reported. An anti-HAV IgG seropositivity of 2% in our study was lower than those reported in these age groups in other developing countries (2, 10).
In Korea, the incidence and seroprevalence of hepatitis A in military personnel have not been previously available. Reliable epidemiological data are essential for the adequate control of viral hepatitis. It is necessary to know the exact number of new cases in order to place the prevalence of HAV infections in a proper perspective and establish a realistic control program. To the best of our knowledge, this is the first study on the extent of HAV infections among young soldiers in ROK Army which has a draft system.
In the past, hepatitis A epidemics were mainly related to the overcrowding and lack of hygienic sanitary conditions typical for military life. In addition, most papers reporting hepatitis A epidemics in the forces were published before 1990 (8). Almost all of the studies published thereafter discussed the efficacy of the vaccine and suggest different vaccination schedules for the militaries, taking it for granted that they were a high-risk group and need prophylaxis (8). Militaries are considered just as a sample of the general population in most papers, in which a decrease in seroprevalence was generally found for all population groups in recent years. In fact, a recent paper reported a hepatitis A incidence rate in militaries similar to that found in the general population (11). Now, due to the improvement of the sanitation level, the risk is mainly ascribed to travels to high endemicity areas.
Among Korean civilians, the overall seropositivity rate of HAV IgG in subjects under 20 yr of age was 63.8% in 1979 and 50.3% in 1989, followed by a rapid decline to 11.7% in 1995, and 4.6% in 1996 (3). The results of epidemiologic studies including our data indicate that Korea is in transition from a high- to low-endemicity region (3, 6). The seroprevalence of HAV infection in young Korean soldiers was approximately 2%, comparable to that in low endemicity countries (12).
The low rate of natural infection clearly indicates that a large part of the younger population is susceptible to HAV infection with the potential for large-scale outbreaks, unless they acquire proper immunity. Food-born or water-born outbreaks in susceptible people may become a problem in the future. The strong evidence for the decreasing incidence of HAV infection as a result of improved personal hygiene and living conditions, supported by the economic growth, will increase the risk of future outbreaks (8, 10).
Inactivated hepatitis A vaccine has been available since 1997 in Korea (3, 4). The vaccine is recommended for use in people including children who are at increased risk of infection (3, 4). However, immunization with hepatitis A vaccine is not recommended in healthy young adults as part of a routine immunization schedule. Since 1996, several outbreaks of hepatitis A in young adults and school children have indicated that there is a need for active immunization in adolescents and young adults at increased risk, such as military personnel. As suggested by Sohn et al., Korea requires an evaluation of the cost-effectiveness of implementing a routine schedule of HAV immunization in children (3). The evaluation of the cost-effectiveness of routine immunization of HAV in Korean military personnel is also warranted. For Hepatitis B immunization, a cost-effectiveness study was conducted by military investigators, who concluded that screening for hepatitis B immunity was cost-effective when the prevalence of immunity was >12% in new military recruits (13). When considering HAV immunization for young Korean soldiers, our data suggest that the routine screening for hepatitis A immunity may not be cost-effective.
This study was based on the data of routine reportes and medical records. Thus, the quality of the data may not be optimal. Patient with minor symptoms were not included in the data if they did not seek medical attention or if they were not reported.
In conclusion, we described a population-based study of the epidemiology of HAV infections among the military personnel of Korea, and the overall HAV seroprevalence was approximately 2%. Given the changing epidemiology of the disease and the associated increase in morbidity, it is suggested that the routine HAV vaccination of Korean military personnel might be mandatory.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Ministry of National Defense, or the Government of Korea.
This study was presented in part at the 44th Annual Meeting of IDSA, Toronto, Canada., October 2006.
References
- 1.Oncu S, Oncu S, Sakarya S. Hepatitis A and B seropositivity among medical students. Health Policy. 2005;74:39–45. doi: 10.1016/j.healthpol.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Jacobsen KH, Koopman JS. Declining hepatitis A seroprevalence: a global review and analysis. Epidemiol Infect. 2004;132:1005–1022. doi: 10.1017/s0950268804002857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohn YM, Rho HO, Park MS, Park JH, Choi BY, Ki M, Jang WI. The changing epidemiology of hepatitis A in children and the consideration of active immunization in Korea. Yonsei Med J. 2000;41:34–39. doi: 10.3349/ymj.2000.41.1.34. [DOI] [PubMed] [Google Scholar]
- 4.Kang JH, Lee KY, Kim CH, Sim D. Changing hepatitis A epidemiology and the need for vaccination in Korea. Asian Pac J Allergy Immunol. 2004;22:237–242. [PubMed] [Google Scholar]
- 5.Han SH, Lee SH, Roh BJ, Shim SC, Cho SC, Sohn JH, Lee DH, Kee CS. An outbreak of hepatits A in South Korean military personnel: a clinical and epidemiologic study. Korean J Hepatol. 2001;7:392–400. [Google Scholar]
- 6.Cha JY, Jun JK, An M, Oh HM, Kim YK, Kim SY, Kim YJ, Cha YK, Park BY, Lee KJ, Cho MK. A seroepidemiological study of anti-HAV IgG in Korean combat policemen. Korean J Med. 1999;57:988–993. [Google Scholar]
- 7.Kwak YH, Shin JH, Jung SK, Rhee JE, Suh GJ, Lee CH, Youn YK. Clinical review of acute hepatitis A in an emergency center. J Korean Soc Emerg Med. 2002;13:306–311. [Google Scholar]
- 8.Franco E, Giambi C, Ialacci R, Coppola RC, Zanetti AR. Risk groups for hepatitis A virus infection. Vaccine. 2003;21:2224–2233. doi: 10.1016/s0264-410x(03)00137-3. [DOI] [PubMed] [Google Scholar]
- 9.Lee SO, Ryu SH, Park SJ, Ryu JS, Woo JH, Kim YS. Meningococcal diseases in the Republic of Korea Army: incidence and serogroups determined by PCR. J Korean Med Sci. 2003;18:163–166. doi: 10.3346/jkms.2003.18.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cianciara J. Hepatitis A shifting epidemiology in Poland and Eastern Europe. Vaccine. 2000;18(Suppl 1):S68–S70. doi: 10.1016/s0264-410x(99)00469-7. [DOI] [PubMed] [Google Scholar]
- 11.D'Amelio R, Molica C, Biselli R, Stroffolini T. Surveillance of infectious diseases in the Italian militars as pre-requisite for tailored vaccination programme. Vaccine. 2001;19:2006–2011. doi: 10.1016/s0264-410x(00)00436-9. [DOI] [PubMed] [Google Scholar]
- 12.Pham B, Duval B, De Serres G, Gilca V, Tricco AC, Ochnio J, Scheifele DW. Seroprevalence of hepatitis A infection in a low endemicity country: a systematic review. BMC Infect Dis. 2005;5:56. doi: 10.1186/1471-2334-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott PT, Niebuhr DW, McGready JB, Gaydos JC. Hepatitis B immunity in United States military recruits. J Infect Dis. 2005;191:1835–1841. doi: 10.1086/429965. [DOI] [PubMed] [Google Scholar]