Abstract
AIM: To evaluate the management of Italian children with cholelithiasis observed at Pediatric and Surgical Departments linked to Italian Society of Pediatric Gastroenterology Hepatology and Nutrition.
METHODS: One-hundred-eighty children (90 males, median age at diagnosis 7.3 years; range, 0-18 years) with echographic evidence of cholelithiasis were enrolled in the study; the data were collected by an anonymous questionnaire sent to participating centers.
RESULTS: One hundred seventeen patients were treated with ursodeoxycholic acid; in 8 children dissolution of gallstones was observed, but the cholelithiasis recurred in 3 of them. Sixty-five percent of symptomatic children treated became asymptomatic. Sixty-four patients were treated with cholecystectomy and in only 2 cases a postoperative complication was reported. Thirty-four children received no treatment and were followed with clinical and echographic controls; in no case the development of complications was reported.
CONCLUSION: The therapeutic strategies were extremely heterogeneous. Ursodeoxycholic acid was ineffective in dissolution of gallstones but it had a positive effect on the symptoms. Laparoscopic cholecystectomy was confirmed to be an efficacy and safe treatment for pediatric gallstones.
Keywords: Pediatric cholelithiasis, Ursodeoxycholic acid, Laparoscopic cholecystectomy, Gallstones, Children
INTRODUCTION
In the last years following the extensive use of ultrasound scanning an increasing number of children with cholelithiasis has been identified. In a population based study, prevalence of gallstones and biliary sludge in children was of 1.9% and 1.46%, respectively[1]. In an analogue study, performed in Italian adults, the overall prevalence of gallstones diseases was of 9.5% in men and 18.9% in women[2].
Gallstones disease is the most common and costly of all digestive disease in the United States, resulting in 700 000 cholecystectomies and as many as 1 000 000 hospitalizations annually[3]. The frequency of hospital admission and operation for gallstones increased in Western countries since the 1950s[4]. In England the age-standardized hospital admission rate for cholelithiasis enhanced from 68.7 to 104.9 per 100 000 population between 1989/1990 and 1999/2000 and it increased progressively with age from 1.1 per 100 000 in the 0-14 year age group to 277.1 per 100 000 in the ≥ 85-year age group in 1999/2000[5].
Guidelines for management of cholelithiasis are available for adults. Cholecystectomy is recommended for symptomatic patients and for those asymptomatic with a predisposition for malignancy (calcified gallbladder wall or family history of gallbladder cancer). For asymptomatic patients an expectant management with periodical clinical and echographic controls is recommended[6,7]. On the contrary, little is known about natural history and management of cholelithiasis in childhood. So far, guidelines for management of children with gallstones are lacking. Surgical options for pediatric cholelithiasis include open or laparoscopic cholecystectomy[8]. At the present, laparoscopic technique is considered the gold standard for cholecystectomy in children for reduced pain, absence of an upper abdominal incision and scar formation and a shorter period of hospitalization[9–12]. The non-surgical approach is based on the use of ursodeoxycholic acid (UDCA); UDCA can reduce cholesterol saturation in bile and progressively dissolve cholesterol gallstones[13,14]. Treatment of radiolucent gallstones with UDCA has been well documented in adults[15–17]; on the contrary, little information is available for children[18,19]. Another approach to pediatric cholelithiasis is represented by expectant management, in which the patients are not treated with medical or surgical therapies but are followed up with periodical clinical and ultrasound controls.
The aim of our multicenter retrospective study was to evaluate the management of Italian children with cholelithiasis observed at Pediatric and Surgical Departments linked to Italian Society of Pediatric Gastroenterology Hepatology and Nutrition (SIGENP).
MATERIALS AND METHODS
Subjects
A retrospective study aimed to evaluate the management of the Italian children with cholelithiasis observed at Medical and Surgical Pediatric Departments linked to SIGENP during the period 1995-2005 was performed. An anonymous questionnaire that investigates age, sex, clinical presentation of cholelithiasis, risk factors for cholelithiasis, basal liver function tests and ultrasonographic findings was proposed to SIGENP members. Seven departments (six medical and one surgical) agreed to participate to the study, three in Northern Italy, one in central regions and three in southern Italy. Each department sent data to the Coordinating Centre in Naples for statistical analysis. The SIGENP approved the project. All patients with echographic evidence of cholelithiasis with age range 0-18 years were enrolled in the present study. The diagnosis of cholelithiasis was based on the presence of echogenic foci that produced acoustic shadowing in the gallbladder or in the region of gallbladder fossa. Sludge was defined as non-shadowing, echogenic, intraluminal sediment. When the sludge was seen at the same time of gallstones, the children were considered to have cholelithiasis. The children with diagnosis of biliary sludge were excluded from the present study. Gallstones were distinguished in radio-lucent and radio-opaque on the basis of radiographic aspect. In all patients risk factors for cholelithiasis such as hemolytic disorders, familiarity for gallstones, obesity, total parenteral nutrition (NPT), hepatobiliary chronic disease, cystic fibrosis, therapy with ceftriaxone, abdominal surgery, IgA deficiency and Gilbert’s disease were investigated. The gallstones in patients without risk factors for cholelithiasis were considered idiopathic. With regard to clinical presentation the patients were distinguished in two groups: asymptomatic and symptomatic. Asymptomatic children had no abdominal discomfort or gastrointestinal complaints; their gallstones were diagnosed incidentally on ultrasound examinations for causes unrelated to cholelithiasis. As previously reported, symptomatic children were divided into those with colicky pain, those with typical biliary tract symptoms (right upper quadrant or epigastric pain, nausea, vomiting and food intolerance) and with atypical symptoms[1].
Management
For each patient, type of treatment and outcome were evaluated. For patients treated with UDCA, therapy was considered effective in case of complete gallstone dissolution at ultrasound scanning and disappearance of clinical symptoms. For surgically treated patients, efficacy of treatment was evaluated on the basis of disappearance of clinical symptoms without the development of “post-cholecystectomy syndrome”. Gallstone recurrence was defined as detection of echogenic foci in the gallbladder that produced acoustic shadowing, after that at least in an occasion disappearance of gallstones was documented at ultrasound scanning. We recorded clinical, laboratory and echographic features of all patients, type of treatment and outcome.
Statistical analysis
Data were analyzed with the χ2 test and with Fisher’s exact test and Student’s t-test as appropriate. P < 0.05 was considered significant.
RESULTS
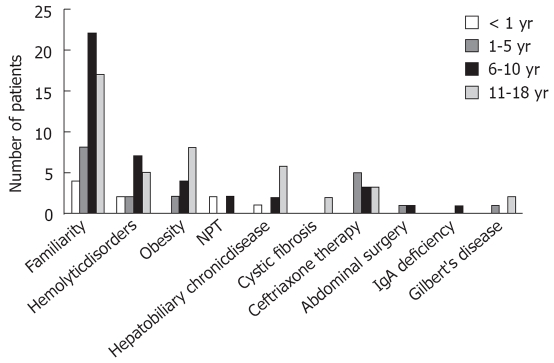
During the period 1995-2005, 196 children with gallstones or biliary sludge (98 males; median age at diagnosis 7.3 years; range, 0-18 years) were observed at Pediatric Medical Departments of Naples (56 cases), Milan (22 cases), Rome (19 cases), Bari (16 cases), S. Giovanni Rotondo (7 cases), Ferrara (6 cases) and at Pediatric Surgical Department of Brescia (70 cases). 181 patients (92.3%) had gallstones and 15 (7.7%) had biliary sludge and so were excluded from the study. In the patients with gallstones, the sex ratio was equal, but in the adolescent group (12-18 years) there was a female predilection for gallstones. Eighty-six (47.5%) children showed one or more risk factors for gallstones at personal and familial anamnesis (Table 1). Ninety-five (52.5%) patients had no risk factors and their cholelithiasis was defined as idiopathic. Presence of one or more relatives with cholelithiasis represented the most common risk factor at any age, with a sensitive increase of frequency with age (Figure 1). Positive family history for cholelithiasis was described in maternal branch in 27 patients (52.9%), in the paternal in 12 cases (23.6%) and in both branches in 10 patients (19.6%), while in 2 (3.9%) children cholelithiasis was found in the brother and in the sister, respectively. Presence of relatives with cholelithiasis, obesity and hemolytic disorders were the predominant risk factors in children with gallstones. According to presence of symptoms at diagnosis, the patients were divided in asymptomatic (64 patients, 35.3%) and symptomatic (117 patients, 64.7%).
Table 1.
Risk factors for cholelithiasis in 181 children observed at Pediatric Medical and Surgical Department
| Risk factor | Pediatric medical departments | Pediatric surgical department | Total |
| Hemolytic disorders | 9 | 7 | 16 |
| Familiarity | 46 | 5 | 51 |
| Obesity | 14 | 0 | 14 |
| NPT1 | 0 | 4 | 4 |
| Hepatobiliary chronic disease | 8 | 1 | 9 |
| Cystic fibrosis | 2 | 0 | 2 |
| Ceftriaxone therapy | 4 | 7 | 11 |
| Abdominal surgery | 2 | 0 | 2 |
| IgA deficiency | 1 | 0 | 1 |
| Gilbert’s disease | 2 | 1 | 3 |
| No risk factors identified | 55 | 40 | 95 |
NPT: Total parenteral nutrition.
Figure 1.
Risk factors for cholelithiasis and age at diagnosis.
In the context of the symptomatic children with regard to clinical presentation, four groups of patients could be distinguished: 51 (43.6%) patients (28 males, median age 10 years; range, 3 mo-18 years) with colicky pain with or without jaundice; 50 (42.7%) patients (25 males, median age 7 years; range, 2 mo-16 years) with typical chronic biliary tract symptoms; 12 patients (10.3%) (3 males, median age 6.5 years; range, 3 mo-14 years) with atypical symptoms; 4 (3.4%) children (2 males, median age 5.6 years; range, 2-13 years) with pancreatitis/cholecystitis.
The distribution of clinical presentations in the different age groups showed that the rate of colicky pain was higher in older children; instead as for the other clinical presentations, there was no correlation with age at diagnosis. According to therapy, patients could be divided in 3 groups: 117 (64.6%) children treated with UDCA, 64 (35.3%) children treated with laparoscopic or laparotomic cholecystectomy and 34 (18.8%) observed with expectant management. It is to note that 34 children were treated with UDCA in a first phase and thereafter, for persistence of gallstones, with cholecystectomy.
The clinical characteristics, type of therapy and outcome of studied patients are reported in Tables 2 and 3.
Table 2.
Clinical characteristics, type of treatment and outcome in 119 children with cholelithiasis observed at Pediatric Medical Department
| UDCA therapy | Cholecystectomy | Wait and see | |
| Asymptomatic | 33 | 2 | 17 |
| Colicky pain | 18 | 7 | 6 |
| Typical biliary tract symptoms | 26 | 4 | 7 |
| Atypical symptoms | 6 | 0 | 3 |
| Pancreatitis/Cholecystitis | 0 | 1 | 0 |
| Resolution of lithiasis | 6 | 14 | 0 |
| Recurrence of lithiasis | 3 | 0 | 0 |
| Resolution of symptoms | 40 | 14 | 0 |
| Recurrence of symptoms | 0 | 3 | 0 |
| Total of patients | 83 | 14 | 33 |
Table 3.
Clinical characteristics, type of treatment and outcome in 62 children with cholelithiasis observed at Pediatric Surgical Department
| UDCA therapy | Cholecystectomy | Wait and see | |
| Asymptomatic | 8 | 9 | 1 |
| Colicky pain | 12 | 23 | 0 |
| Typical biliary tract symptoms | 9 | 14 | 0 |
| Atypical symptoms | 3 | 3 | 0 |
| Pancreatitis/Cholecystitis | 2 | 1 | 0 |
| Resolution of lithiasis | 2 | 50 | 0 |
| Recurrence of lithiasis | 0 | 0 | 0 |
| Resolution of symptoms | 9 | 50 | 0 |
| Recurrence of symptoms | 0 | 0 | 0 |
| Total of patients | 34 | 50 | 1 |
Patients observed at medical departments
Medical treatment: Eighty-three (69.7%) of 119 patients with gallstones observed at Medical Departments were treated with UDCA (25 mg/kg per day; range 18-30 mg/kg per day) for median period of 13 (range, 3-96) mo. Thirty-three (39.8%) patients had radiolucent gallstones, 17 (20.4%) radio-opaque gallstones, while 33 patients (39.8%) did not undergo radiographic examination. The median of diameter maximum of gallstones was 8 (range, 2-45) mm. All children completed the therapy without any adverse effects. During UDCA therapy they underwent an ultrasound scanning every 3-6 mo. The gallstones completely disappeared in only 6 (7.2%) children (4 radio-lucent and 2 with unknown radiographic-aspect), but the cholelithiasis recurred in 3 (50%) of them; in one child, gallstones reappeared after 6 years and in the other two biliary sludge were observed after 6 and 10 mo, respectively. Four of 6 patients with gallstones dissolution were symptomatic at diagnosis; all 4 children were relieved of their symptoms during UDCA therapy. The other 2 children remained asymptomatic during the observation period. In other 4 patients disappearance of gallstones was observed, but three of them had a pseudolithiasis (following antibiotic-therapy with ceftriaxone) and one had fetal gallstones. Since these conditions are described as auto-resolving diseases[20–23], the disappearance was not considered induced by UDCA. In 73 (87.9%) patients treated with UDCA there was persistence of gallstones. Forty-three patients were symptomatic at diagnosis. In 36 (83.7%) of these patients resolution of clinical discomfort was observed, while in 7 (16.3%) of them symptoms persisted unchanged during the therapy. The other 30 (41.1%) children remained asymptomatic during the treatment. Eleven (13.2%) patients underwent cholecystectomy at the suspension of medical therapy for either recurrence or persistence of symptoms. Significant differences in terms of sex, age, characteristics of gallstones (diameters, Rx-aspect) and risk factors for cholelithiasis were not found among the patient’s responders and non-responders to UDCA.
Surgical treatment: Fourteen (11.8%) patients with gallstones observed at Pediatric Medical Departments were surgically treated. At x-ray examination, 4 (28.6%) of them had radiolucent gallstones, 6 (42.8%) radio-opaque stones; in the remaining 4 (28.6%) cases the radiographic aspect of gallstones was unknown. Eleven (78.6%) patients were symptomatic and 3 (21.4%) asymptomatic. The median of diameter maximum of gallstones was 7 (range, 3-33) mm. In 10 (71.4%) cases cholecystectomy was performed by laparoscopic techniques and in 4 (28.6%) by laparotomy. There were no post-operative complication and in no case residual cholelithiasis or recurrence of gallstones during the follow-up were observed. In three patients recurrence of clinical symptoms after treatment (post-cholecystectomy syndrome) was described.
Expectant management: Thirty-three (27.7%) patients were not treated, but they were observed with clinical, laboratory and ultrasonographic controls every 3-6 mo. Two patients (6%) had radiolucent stones, 16 (48.5%) radio-opaque cholelithiasis and the other 15 (45.5%) had not been submitted to x-ray examination. The median of diameter maximum of gallstones was 9 (range, 2-23) mm. In no case development of complication was observed and none of the 17 (51.5%) asymptomatic patients became symptomatic during the follow up (median duration of follow-up, 9 mo, range 1-45).
Patients observed at surgical department
Seventy patients enrolled in the present study come from the Pediatric Surgical Department of Brescia. To avoid selection bias in the evaluation of the treatment and the outcome we have decided to separately analyze the children of this center.
Sixty-two patients had gallstones and 8 had biliary sludge and so were excluded from the study (median age 7 years; range, 0-18 years). Forty-eight (77.4%) patients were symptomatic at diagnosis, while 14 (22.6%) were asymptomatic. Thirty-four children (54.8%) with gallstones (21 radio-lucent, 9 radio-opaque, and 4 unknown radiographic aspect) were treated with UDCA (median dose 18 mg/kg per day; range, 5-30 mg/kg per day; median duration 5 mo; range, 2-36 mo). Twenty-six patients were symptomatic and eight were asymptomatic. Following UDCA therapy, nine (34.6%) of 26 symptomatic patients became symptom free, while in 17 (65.4%) cases the symptoms persisted unchanged during the therapy. Gallstones completely disappearance in 2 (5.9%) radiolucent cases. In other 2 patients spontaneous resolution of lithiasis was observed (pseudo-lithiasis induced by ceftriaxone). In the remaining thirty (88.2%) patients (17 radiolucent gallstones, 9 radio-opaque and 4 with unidentified radiographic-aspect) UDCA was inefficacy with persistence of gallstones despite therapy. Twenty-three of these children underwent cholecystectomy, while 7 were followed with periodical controls. The other 27 patients were directly treated with surgical approach. In forty patients (80%) cholecystectomy was performed by laparoscopic technique and in 10 (20%) cases by laparotomic approach. Histological analysis of the removed gallbladders was available for 39 patients: thirty-three (84.6%) had chronic cholecystitis, 2 (5.1%) papillomatosis, 1 (2.6%) adenoma of gallbladder and only 3 (7.7%) patients had normal gallbladder wall. Postoperative complications were not reported except in a child who developed a laparocele and in another who had dilatation of choledochus duct. In no case the post-cholecystectomy syndrome was observed.
Only one (1.6%) patient was not treated and followed with periodical clinical and echographic controls.
DISCUSSION
Although cholelithiasis is considered as an uncommon condition in children, recent series document an increasing detection of this disorder[1]. This increase may be explained by the increased use of abdominal ultrasound scanning in childhood. The frequency of pediatric gallstones, documented in studies in which patients were selected according to initial symptoms, resulted in prevalence’s between 0.13% and 0.22%[1,24]. In Wesdorp’s study, in which patients with cholelithiasis were obtained by screening 4200 abdominal ultrasound scans performed for different reasons such as typical biliary symptoms, general abdominal symptoms or routinely check-ups, a higher prevalence of gallstones and biliary sludge (1.9% and 1.46%, respectively) was observed. For its typology the present study cannot give information on the epidemiology of pediatric cholelithiasis, but it has however confirmed some aspects previously reported, as major frequency in the female only after puberty, increase of the cases with age, association with some risk factors such as familiarity for cholelithiasis, obesity and hemolytic disorders[1,25,26]. It was previously reported that approximately 80% of adults with gallstones are asymptomatic[2,27]. Instead we have found that only one third of children with cholelithiasis were asymptomatic. This could be explained by the tertiary nature of involved centers or may indicate that asymptomatic cholelithiasis is less frequently in children, as described in other studies[1].
Although the prevalence of cholelithiasis in children is increasing, little information is available about the management of this disorder in childhood. There are only few data on pediatric cholelithiasis and in the majority of cases the studies were performed on a limited number of patients. In our study, in which the management of cholelithiasis was evaluated in a large cohort of children observed at Medical and Surgical Department linked to SIGENP, both diagnostic approach and therapeutic strategies were extremely heterogeneous. As for diagnostic approach, abdominal X-ray was not performed in all cases; in fact, radiographic aspect of gallstones in a third of patients was not evaluated. As for treatment, although in adults UDCA therapy is recommended only for a specific subset of patients[15], in the present study this drug was used in about two third of cases and only in half of cases the gallstones were radiolucent. Our study confirmed that UDCA was ineffective in dissolution of gallstones in the vast majority of the cases. In addition, there was an important rate of recurrence of cholelithiasis after primary dissolution. Instead UDCA had a positive effect on the symptoms determining the disappearance of abdominal discomfort in the vast majority of the symptomatic patients treated.
In our study laparoscopic cholecystectomy was confirmed to be an efficacy and safe procedure in the treatment of pediatric gallstones for the low rate of post-operative complications (3%) and post-cholecystectomy syndrome (4.7%). In contrast to Wesdorp’s study, in which 45% of children with biliary symptoms or colicky pain had recurrence of their symptoms after treatment (Endoscopic Retrograde Cholangiopancreatography (ERCP) or cholecystectomy), in our study the post-cholecystectomy syndrome was observed only in a small percentage of cases. This difference may be explained by the greater recurrence of symptoms associated with ERCP than with cholecystectomy.
The histological analysis of the removed gallbladders showed structural alterations such as chronic cholecystitis, papillomatosis and adenoma in the majority of cases; in only few cases the gallbladder wall was normal. Therefore, for long life expectancy of children, expectant management may not be safe in pediatric patients. In fact, in contrast to adults in whom the natural history of gallstones is well documented, in children it is not known. In adults only 1%-4% per year will develop symptoms or complications of gallstones disease; only 10% will develop symptoms in the first five years after diagnosis and approximately 20% by 20 years[28–30].
A fifth of patients with gallstones enrolled in our study were not treated and followed with periodical clinical and echographic controls; in none of them any complication occurred during the follow-up (median 9 mo; range, 3-45). It is to note, however, that in our study the observation period of untreated was too short to evaluate the effective rate of complications.
Considering the typology of the present study and the heterogeneous management observed in our patients, we are unable to provide clear indications for management of cholelithiasis in children. However on the basis of the available studies and our results, the following approach might be suggested. Firstly, the children with gallstones should be divided in two groups on the basis of clinical presentation: symptomatic and asymptomatic. As for asymptomatic gallstones, considering the low rate of complications observed and the favorable natural history described in adults, we recommend an expectant management with periodical clinical and ultrasonographic controls. On the other hand, as for symptomatic gallstones, considering the low rate of post-operative complications and post-cholecystectomy syndrome, we suggest surgical approach with laparoscopic cholecystectomy. For its inefficacy on dissolution of gallstones and for high recurrence rate of gallstones, UDCA should not be used in pediatric gallstones, except in symptomatic children with contraindication to surgery for reduce the clinical symptoms.
It is necessary that this approach is validated in further studies including a larger number of children; furthermore, it would be desirable to known in larger series the natural history of cholelithiasis in childhood.
COMMENTS
Background
Although recent extensive use of abdominal ultrasound scanning has identified an increased number of cholelithiasis, little is known about the natural history and management of this disorder in childhood.
Innovations and breakthroughs
Only few data on pediatric cholelithiasis are available and in the majority of cases the studies were performed on limited number of patients. In our study, the management of cholelithiasis was retrospectively evaluated in a large cohort of children observed at Medical and Surgical Department linked to Italian Society of Pediatric Gastroenterology Hepatology and Nutrition (SIGENP).
Applications
The present study suggests a possible approach to pediatric cholelithiasis. It is desirable, however, that this approach is validated in further prospective studies including a larger number of children.
Peer review
This retrospective study is well done and nicely written and focused on a relevant topic (cholelithiasis in children).
Peer reviewer: Dario Conte, Professor, GI Unit-IRCCS Osp. Maggiore, Chair of Gastroenterology, Via F. Sforza, 35, Milano 20122, Italy
S- Editor Sun YL L- Editor Alpini GD E- Editor Liu Y
References
- 1.Wesdorp I, Bosman D, de Graaff A, Aronson D, van der Blij F, Taminiau J. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr. 2000;31:411–417. doi: 10.1097/00005176-200010000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Attili AF, Carulli N, Roda E, Barbara B, Capocaccia L, Menotti A, Okoliksanyi L, Ricci G, Capocaccia R, Festi D. Epidemiology of gallstone disease in Italy: prevalence data of the Multicenter Italian Study on Cholelithiasis (M.I.COL.) Am J Epidemiol. 1995;141:158–165. doi: 10.1093/oxfordjournals.aje.a117403. [DOI] [PubMed] [Google Scholar]
- 3.Bar-Meir S. Gallstones: prevalence, diagnosis and treatment. Isr Med Assoc J. 2001;3:111–113. [PubMed] [Google Scholar]
- 4.Bateson MC. Gallstones and cholecystectomy in modern Britain. Postgrad Med J. 2000;76:700–703. doi: 10.1136/pmj.76.901.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang JY, Ellis C, Majeed A, Hoare J, Tinto A, Williamson RC, Tibbs CJ, Maxwell JD. Gallstones--an increasing problem: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:561–569. doi: 10.1046/j.1365-2036.2003.01439.x. [DOI] [PubMed] [Google Scholar]
- 6.Treatment of gallstone and gallbladder disease. SSAT patient care guidelines. J Gastrointest Surg. 2004;8:363–364. doi: 10.1016/j.gassur.2003.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Ransohoff DF, Gracie WA. Treatment of gallstones. Ann Intern Med. 1993;119:606–619. doi: 10.7326/0003-4819-119-7_part_1-199310010-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kim PC, Wesson D, Superina R, Filler R. Laparoscopic cholecystectomy versus open cholecystectomy in children: which is better? J Pediatr Surg. 1995;30:971–973. doi: 10.1016/0022-3468(95)90323-2. [DOI] [PubMed] [Google Scholar]
- 9.Esposito C, Gonzalez Sabin MA, Corcione F, Sacco R, Esposito G, Settimi A. Results and complications of laparoscopic cholecystectomy in childhood. Surg Endosc. 2001;15:890–892. doi: 10.1007/s004640000042. [DOI] [PubMed] [Google Scholar]
- 10.Mattioli G, Repetto P, Carlini C, Granata C, Montobbio G, Cagnazzo A, Barabino A, Gandullia P, Jasonni V. Medium-term results after cholecystectomy in patients younger than 10 years. Surg Endosc. 2001;15:1423–1426. doi: 10.1007/s00464-001-9029-2. [DOI] [PubMed] [Google Scholar]
- 11.Holcomb GW 3rd, Morgan WM 3rd, Neblett WW 3rd, Pietsch JB, O'Neill JA Jr, Shyr Y. Laparoscopic cholecystectomy in children: lessons learned from the first 100 patients. J Pediatr Surg. 1999;34:1236–1240. doi: 10.1016/s0022-3468(99)90159-8. [DOI] [PubMed] [Google Scholar]
- 12.Clements RH, Holcomb GW 3rd. Laparoscopic cholecystectomy. Curr Opin Pediatr. 1998;10:310–314. doi: 10.1097/00008480-199806000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Paumgartner G, Pauletzki J, Sackmann M. Ursodeoxycholic acid treatment of cholesterol gallstone disease. Scand J Gastroenterol Suppl. 1994;204:27–31. doi: 10.3109/00365529409103622. [DOI] [PubMed] [Google Scholar]
- 14.Hofmann AF. Pharmacology of ursodeoxycholic acid, an enterohepatic drug. Scand J Gastroenterol Suppl. 1994;204:1–15. doi: 10.3109/00365529409103618. [DOI] [PubMed] [Google Scholar]
- 15.Strasberg SM, Clavien PA. Cholecystolithiasis: lithotherapy for the 1990s. Hepatology. 1992;16:820–839. doi: 10.1002/hep.1840160332. [DOI] [PubMed] [Google Scholar]
- 16.Tomida S, Abei M, Yamaguchi T, Matsuzaki Y, Shoda J, Tanaka N, Osuga T. Long-term ursodeoxycholic acid therapy is associated with reduced risk of biliary pain and acute cholecystitis in patients with gallbladder stones: a cohort analysis. Hepatology. 1999;30:6–13. doi: 10.1002/hep.510300108. [DOI] [PubMed] [Google Scholar]
- 17.Petroni ML, Jazrawi RP, Lanzini A, Zuin M, Pazzi P, Fracchia M, Boga E, Facchinetti D, Alvisi V, Galatola G, et al. Repeated bile acid therapy for the long-term management of cholesterol gallstones. J Hepatol. 1996;25:719–724. doi: 10.1016/s0168-8278(96)80244-3. [DOI] [PubMed] [Google Scholar]
- 18.Gamba PG, Zancan L, Midrio P, Muraca M, Vilei MT, Talenti E, Guglielmi M. Is there a place for medical treatment in children with gallstones? J Pediatr Surg. 1997;32:476–478. doi: 10.1016/s0022-3468(97)90610-2. [DOI] [PubMed] [Google Scholar]
- 19.Colombo C, Bertolini E, Assaisso ML, Bettinardi N, Giunta A, Podda M. Failure of ursodeoxycholic acid to dissolve radiolucent gallstones in patients with cystic fibrosis. Acta Paediatr. 1993;82:562–565. doi: 10.1111/j.1651-2227.1993.tb12754.x. [DOI] [PubMed] [Google Scholar]
- 20.Biner B, Oner N, Celtik C, Bostancioglu M, Tuncbilek N, Guzel A, Karasalihoglu S. Ceftriaxone-associated biliary pseudolithiasis in children. J Clin Ultrasound. 2006;34:217–222. doi: 10.1002/jcu.20228. [DOI] [PubMed] [Google Scholar]
- 21.Papadopoulou F, Efremidis S, Karyda S, Badouraki M, Karatza E, Panteliadis C, Malaka K. Incidence of ceftriaxone-associated gallbladder pseudolithiasis. Acta Paediatr. 1999;88:1352–1355. doi: 10.1080/080352599750030077. [DOI] [PubMed] [Google Scholar]
- 22.Suma V, Marini A, Bucci N, Toffolutti T, Talenti E. Fetal gallstones: sonographic and clinical observations. Ultrasound Obstet Gynecol. 1998;12:439–441. doi: 10.1046/j.1469-0705.1998.12060439.x. [DOI] [PubMed] [Google Scholar]
- 23.Munjuluri N, Elgharaby N, Acolet D, Kadir RA. Fetal gallstones. Fetal Diagn Ther. 2005;20:241–243. doi: 10.1159/000085077. [DOI] [PubMed] [Google Scholar]
- 24.Palasciano G, Portincasa P, Vinciguerra V, Velardi A, Tardi S, Baldassarre G, Albano O. Gallstone prevalence and gallbladder volume in children and adolescents: an epidemiological ultrasonographic survey and relationship to body mass index. Am J Gastroenterol. 1989;84:1378–1382. [PubMed] [Google Scholar]
- 25.Reif S, Sloven DG, Lebenthal E. Gallstones in children. Characterization by age, etiology, and outcome. Am J Dis Child. 1991;145:105–108. doi: 10.1001/archpedi.1991.02160010111028. [DOI] [PubMed] [Google Scholar]
- 26.Holcomb GW Jr, Holcomb GW 3rd. Cholelithiasis in infants, children, and adolescents. Pediatr Rev. 1990;11:268–274. doi: 10.1542/pir.11-9-268. [DOI] [PubMed] [Google Scholar]
- 27.Barbara L, Sama C, Morselli Labate AM, Taroni F, Rusticali AG, Festi D, Sapio C, Roda E, Banterle C, Puci A. A population study on the prevalence of gallstone disease: the Sirmione Study. Hepatology. 1987;7:913–917. doi: 10.1002/hep.1840070520. [DOI] [PubMed] [Google Scholar]
- 28.Meshikhes AW. Asymptomatic gallstones in the laparoscopic era. J R Coll Surg Edinb. 2002;47:742–748. [PubMed] [Google Scholar]
- 29.Vauthey JN, Saldinger PF. The natural history of gallstones and asymptomatic gallstones. In: Blumgart LH, Fong Y, editors. Surgery of the liver and biliary tract. 3rd ed. London: Company LTD, Saunders WB; 2000. pp. 643–649. [Google Scholar]
- 30.Sakorafas GH, Milingos D, Peros G. Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 years after the introduction of laparoscopic cholecystectomy. Dig Dis Sci. 2007;52:1313–1325. doi: 10.1007/s10620-006-9107-3. [DOI] [PubMed] [Google Scholar]