Abstract
AIM: To investigate the relationship between loss of heterozygosity (LOH) for mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/IGF2R) and the outcomes for primary HCC patients treated with partial hepatectomy.
METHODS: The LOH for M6P/IGF2R in primary HCC patients was assessed using six different gene-specific nucleotide polymorphisms. The patients studied were enrolled to undergo partial hepatectomy.
RESULTS: M6P/IGF2R was found to be polymorphic in 73.3% (22/30) of the patients, and of these patients, 50.0% (11/22) had tumors showing LOH in M6P/IGF2R. Loss of heterozygosity in M6P/IGF2R was associated with significant reductions in the two year overall survival rate (24.9% vs 65.5%; P = 0.04) and the disease-free survival rate (17.8% vs 59.3%; P = 0.03).
CONCLUSION: These results show M6P/IGF2R LOH predicts poor clinical outcomes in surgically resected primary HCC patients.
Keywords: Loss of heterozygosity, Mannose 6-phosphate/insulin-like growth factor 2 receptor, Hepatocellular carcinoma
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common type of malignancy, being especially prevalent in the Southeast Asian and sub-Saharan African populations[1]. Etiological risk factors for HCC formation include hepatitis virus infection, alcohol consumption and dietary exposure to aflatoxin B1[1,2]. In Korea and Taiwan, approximately 90% of all patients with HCC are Hepatitis B surface antigen (HbsAg)-positive, and prospective studies have found Hepatitis B virus carriers have a 200-fold increase in relative risk for HCC. The mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/IGF2R) is mapped at the chromosome location 6q25-27[3], which is predicted to contain a liver tumor suppressor gene[4]. This gene encodes a receptor which functions in intracellular lysosomal enzyme trafficking, transforming growth factor beta (TGF-β) activation, and IGF2 degradation[5]. Granzyme B internalization by the M6P/IGF2R is also required for cytotoxic T cells to induce apoptosis in cells targeted for death, resulting in this receptor being referred to as a “death receptor”[6]. Elevated IGF2 levels during murine development arising from M6P/IGF2R deficiency result in cardiac abnormalities, cleft palate, fetal overgrowth and prenatal lethality[7]. Furthermore, the large-offspring syndrome found in cloned animals is frequently associated with epigenetic changes in M6P/IGF2R imprinting regulation which result in decreased gene expression[8]. Thus, M6P/IGF2R plays a crucial role in regulating mammalian fetal growth and development. M6P/IGF2R is also mechanistically involved in the genesis of human cancer[9–12]. M6P/IGF2R loss of heterozygosity (LOH), coupled with intragenic loss-of-function mutations in the remaining allele, is a common event in human cancers[6,10]. Tumor cell growth is inhibited when M6P/IGF2R expression is restored to normal, whereas it is increased when gene expression is reduced[13–16]. The results of these mutational and functional studies clearly show M6P/IGF2R possesses the characteristics necessary to be classified as a tumor suppressor gene[17]. Our results show M6P/IGF2R LOH in primary HCC patients predicts poor therapeutic outcomes.
MATERIALS AND METHODS
Patients
Paraffin-embedded tissue sections from 30 patients, who were confirmed histopathologically to have HCC, were obtained from the Gyeongsang National University and the Catholic University of Korea. All patients had a history of hepatitis virus infection and/or cirrhosis, and had undergone partial hepatectomy for the treatment of their disease.
Tissue microdissection and loss of heterozygosity analysis for M6P/IGF2R
Microdissection of 10-μm histology sections from tumor tissue and the surrounding normal liver tissue was performed as described in previous studies[18,19]. Briefly, paraffin-embedded sections were deparaffinized in xylene (2 × 5 min), exposed for 2 min to graded ethanol washes (namely, 100%, 95%, 70% and 50% ethanol) and rehydrated in H2O before staining. The tissue sections were then stained for 30 s with 2% methylene blue and rinsed in H2O before allowing them to air dry. Tumor tissue and the surrounding normal tissue (50-cells) were carefully microdissected using a serial section stained with hematoxylin-eosin for comparison. The normal tissue used for genotyping was connective tissue. The dissected tissues were then placed in 75 μL of Tris-ethylenediamine-tetraacetic acid buffer (10 mmol/L Tris-HCl, pH 8.0 at 25°C and 0.5 mmol/L ethylenediamine tetraacetic acid, pH 8.0 at 25°C containing 5 μL of 20 g/L proteinase K (Boehringer Mannheim, Indianapolis, IN). This mixture was incubated at 52°C for 3 h and then at 85°C for 10 min. Polymerase chain reaction (PCR) analysis was conducted using 5 μL of this mixture, as described below. Six single nucleotide polymorphisms (Table 1), identified as c. 901C > G (exon 6), c. 1197A > G (exon 9), c. 1737G > A (exon 12), c. 2286A > G (exon 16), c. 6206A > G (exon 40) and c. X47-5t > a (exon 47), were also analyzed following 2 rounds of nested PCR. The exon-specific forward and reverse primers have been previously described[19,20]. The exons containing these polymorphisms were amplified by PCR from genomic DNA under conditions identical to those described above. The single nucleotide polymorphisms used to determine the loss of heterozygosity in M6P/IGF2R were assessed by directly sequencing the PCR products according to the manufacturer’s protocol (Thermo Sequenase, USB Corporation, Cleveland, OH). Taq DNA polymerases may introduce sequence errors during PCR amplification, and unequal amplification of the two alleles can result in the false positive detection of a loss of heterozygosity. Thus, both normal and tumor DNA templates were amplified in three independent PCR reactions, and assessed for LOH in M6P/IGF2R.
Table 1.
M6P/IGF2R LOH analysis of paraffin-embedded tissue
| Position | Nucleotide | Genotype | Amplicon size (bp) | F1 primer (5’-3’) | R1 primer (5’-3’) | Nested primer (5’-3’) |
| Exon 6 | 901 | C/G | 91 | CACCAGGCGTTTGATGTTGG | CTCCAGCAAGGACCTGACTTTC | CCTCCGATGCTGTTGGCGT |
| Exon 9 | 1197 | A/G | 123 | ACTAAGTAAGACTGTAATCTTCTAATACC | GTCTGTGGAGAAACTG AAATACAG | AATACCTATTCATATAAAACAAGCCTC |
| Exon 12 | 1737 | G/A | 111 | TATTTGTCACAGAGTGCTGCAGG | GGCATCCAGTTTGGAATGAGTTAG | GGAAGATCTAGGTGATGCTTTTC |
| Exon 16 | 2286 | A/G | 187 | GAAGCTTTCATATTATGATGGGATG | GAGGATACTCATGCCTGTGGTG | CATCGCGCTCCCTGAGGATACT |
| Exon 40 | 6206 | A/G | 118 | GGGTGTGATGTGACATTTGAGTGG | GCCTTCCCAGTCCACCCGC | GGAGTGCAAATTCGTCCAGAAAC |
| Exon 47 | X47-5 | t/a | 161 | ATGCCCTCTCTACACTGGAGTA | GTAAGCTGACCACTTGCTGTAGG | CAGTGATAAGTAAGCTGACC |
Due to the potential for contaminating the tumor tissue sample with normal stroma, allele loss in informative patients was defined as a > 50% decrease in the ratio of the two alleles in tumor tissue versus that in the surrounding normal stromal tissue. This was quantified using a densitometer.
Statistical analysis
Overall survival and disease-free survival rate represented the clinical end-point. All curves were computed using the Kaplan-Meier method starting from the time of study entry. Curves for different sub-groups were compared by the Cox-Mantel test. A chi-squared test was used to compare the clinical characteristics between M6P/IGF2R-informative and M6P/IGF2R-excluded patients, and between informative patients with and without LOH in M6P/IGF2R. A P < 0.05 was considered to be statistically significant.
RESULTS
Analysis of LOH in M6P/IGF2R
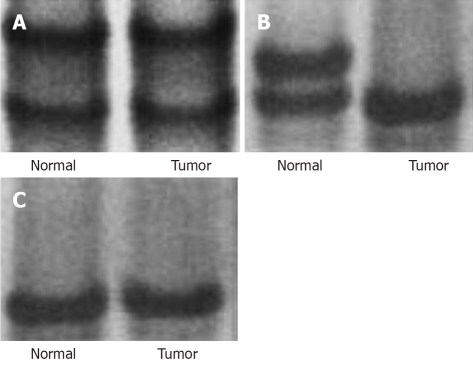
The study population consisted of a total of 30 patients who were enrolled in a retrospective clinical trial for primary HCC from March 1999 to June 2003 (Table 2). Among the 30 patients, 22 (73.3%) were informative (that is, polymorphic), and the tumors in 50% (11/22) of these patients exhibited LOH in M6P/IGF2R (Figure 1). There was no significant difference between M6P/IGF2R-informative patients and those not used in this study in terms of the clinical characteristics of sex, age, liver cirrhosis, tumor of differentiation, size of tumor, or type of hepatitis.
Table 2.
Patient characteristics n (%)
| Characteristics | Total patients (n = 30) | Informative patients (n = 22) |
| Age: yr | 36-78 (Median: 58) | 39-78 (Median: 59) |
| Gender: male/female | 22 (73.3)/8 (26.7) | 16 (72.7)/6 (27.3) |
| Disease etiology | ||
| HBV | 18 (60.0) | 15 (68.2) |
| HCV | 6 (20.0) | 3 (13.6) |
| Alcohol | 6 (20.0) | 4 (18.2) |
| Tumor Grade | ||
| Well differentiation | 9 (30.0) | 6 (27.3) |
| Moderate differentiation | 11 (36.7) | 8 (36.4) |
| Poor differentiation | 10 (33.3) | 8 (36.4) |
| Liver Histology | ||
| Chronic hepatitis | 3 (10.0) | 2 (9.1) |
| Cirrhosis | 21 (70.0) | 16 (72.7) |
| Nonspecific reaction | 6 (20.0) | 4 (18.2) |
| Tumor size (cm) | ||
| < 2 | 4 (13.3) | 2 (9.1) |
| 2-5 | 14 (46.7) | 11 (50.0) |
| > 5 | 12 (40.0) | 9 (40.9) |
| No. of Tumor | ||
| Single | 18 (60.0) | 12 (54.5) |
| Multiple | 12 (40.0) | 10 (45.5) |
| AJCC Stage | ||
| II | 18 (60.0) | 12 (54.5) |
| IIIA | 12 (40.0) | 10 (45.5) |
Figure 1.
There are three results in the LOH analysis for M6P/IGF2R in primary hepatocellular carcinoma (HCC). A: Informative HCC without LOH in M6P/IGF2R; B: Informative HCC with LOH in M6P/IGF2R; C: Non-informative HCC.
Clinical outcome
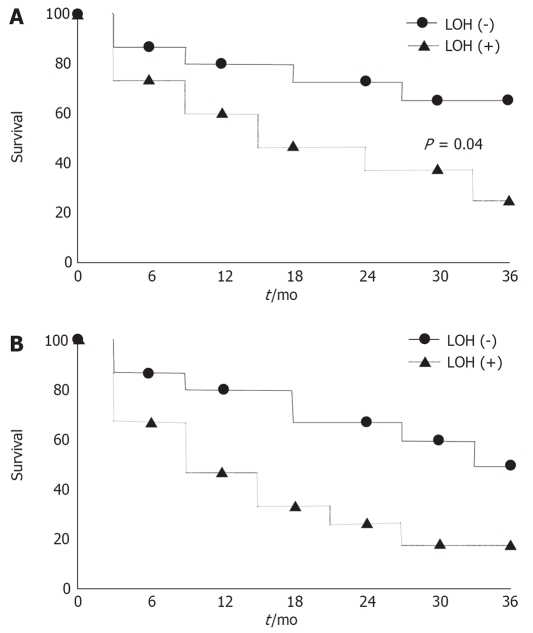
The median follow-up for surviving patients enrolled in this trial was 33 mo (range: 2 to 62 mo). The median survival times were 34 mo and 23 mo for overall survival and disease free survival, respectively. There was no relationship between LOH in M6P/IGF2R and clinical factors, such as sex, age, liver cirrhosis, tumor differentiation, tumor size, or the type of hepatitis. The median overall survival times in patients with and without LOH in M6P/IGF2R were 18 mo and 44 mo, respectively, and the two year overall survival rates were 24.9% and 65.5%, respectively (log-rank, P = 0.04) (Figure 2A). Likewise, the median disease-free survival rates in patients with and without LOH in M6P/IGF2R were 12 mo and 36 mo, respectively, and the 3 year disease-free survival rates were 17.8% and 59.3%, respectively (log-rank, P = 0.03) (Figure 2B). The clinical relevance of LOH in M6P/IGF2R to both overall survival and disease-free survival rates was confirmed in the analysis (P < 0.05 for both comparisons). These results indicate that LOH in M6P/IGF2R results in poor patient outcome when surgical resection is employed, since all other measured clinical characteristics of the primary HCC patients were comparable to those in patients with a non-mutated M6P/IGF2R tumor suppressor gene.
Figure 2.
A: The overall survival according to loss of heterozygosity in M6P/IGF2R; B: The disease free survival according to loss of heterozygosity in M6P/IGF2R.
DISCUSSION
M6P/IGF2R LOH occurs frequently in human breast, liver and lung cancer[9,10,20]. Mutation in M6P/IGF2R is also commonly found in gastrointestinal and gynecological cancers, because the coding sequence of M6P/IGF2R contains a poly-G region, which is a mutational target in tumors with mismatch repair deficiencies and microsatellite instability[12,21]. Functional studies show the introduction of an exogenous wild-type M6P/IGF2R with a single inactivated allele into human colorectal cancer cells significantly decreases cell growth rate and enhances apoptosis[13]. Conversely, the loss of M6P/IGF2R expression promotes cancer cell growth by increasing intracellular signaling from both the receptors, the insulin-like growth factor 1 receptor and the insulin receptors[22]. Kong et al[10] demonstrated mutations in both alleles of the M6P/IGF2R are found in more than 50% of squamous cell carcinomas of the lung. In the present study, we demonstrated M6P/IGF2R LOH in primary HCC is also associated with poor patient prognosis. Loss of heterozygosity in malignancy can also occur due to chromosomal deletion or somatic recombination resulting in uniparental disomy[23]. Because chromosomal deletion can affect more than one gene, M6P/IGF2R LOH does not rule out the possibility of a loss of adjacent genes with tumor suppressor functions in HCC. This study also showed improvements in overall survival and disease-free survival in those patients undertaking surgical resection for primary HCC with M6P.IGF2R LOH. It was found patients with mutations in M6P/IGF2R had a significantly worse prognosis than those who had a non-mutated M6P/IGF2R allele.
M6P/IGF2R is normally imprinted in mice, with only the maternal copy of the gene being expressed[24]. By contrast, both copies of M6P/IGF2R are expressed in humans, because genomic imprinting at this locus was lost in the primate lineage approximately 70 million years ago[25]. Importantly, the restoration of biallelic M6P/IGF2R expression in mice results in a marked reduction in offspring weight late in embryonic development that persists into adulthood[26]. This demonstrates that M6P/IGF2R allelic loss or haploid insufficiency markedly enhances cell proliferation and/or survival during fetal development. Therefore, the mutation of even a single allele of M6P/IGF2R in human somatic cells is predicted to promote cell growth. Haploid insufficiency of tumor suppressor genes, such as Nf2, p27Kip1, p53 and TGF-β, is known to promote tumor formation[27–29]. Yamada et al[9] demonstrated that, in patients chronically infected with Hepatitis B and/or Hepatitis C viruses, mutations in M6P/IGF2R take place not only in HCC, but also in the phenotypically normal hepatocytes adjacent to these tumors. Interestingly, only one M6P/IGF2R allele is inactivated in the adjacent cirrhotic tissue, even when both alleles are mutated in the HCC. These findings are consistent with the normal appearing, preneoplastic hepatocytes forming clonal masses in the liver, because M6P/IGF2R haploid insufficiency affords them with a selective growth and/or survival advantage relative to normal hepatocytes[30].
In conclusion, this study shows the analysis of M6P/IGF2R LOH provides clinical significance in surgically resected primary HCC patients.
COMMENTS
Background
The associated nature of hepatocellular carcinoma (HCC) and mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/GF2R) is well reported. However, there is scant research on the clinical significance of loss of heterozygosity (LOH) in M6P/GF2R in patients with primary HCC. In the present study, we aimed to investigate the relationship between LOH for M6P/IGF2R and various factors, including survival rate, in primary HCC patients treated with partial hepatectomy.
Research frontiers
Several studies have investigated various types of cancer, including HCC, in which LOH for M6P/IFG2R might appear. We studied the relationship between LOH for M6P/IGF2R and HCC, and confirmed the survival rate is directly related to the LOH for M6P/IGF2R.
Innovations and breakthroughs
The present research studied cases with primary HCC, but research on the usefulness of LOH for M6P/IGF2R should be continued by comparing cases with metastatic HCC, cholangiocarcinoma and other tumors.
Applications
The results of this study suggest the presence of LOH for M6P/IGF2 may represent some poor prognostic factors in primary HCC patients treated with hepatectomy.
Peer review
The paper represents a real advance in the loss of heterozygosity for M6P/IGF2R in patients with primary HCC. The conclusions are valuable. The methodology is correct and the results are well presented.
Acknowledgments
This paper was presented in part at the 97th Annual Meeting of the American Association for Cancer Research, April 1-5, 2006, Washington, DC.
Supported by The Special Clinical Fund of Gyeongsang National University Hospital
Peer reviewer: Ned Snyder, Professor, University of Texas Medical Branch, 301 University, University of Texas Medical Branch, Galveston, Texas 77555-0764, United States
S- Editor Yang RH L- Editor McGowan D E- Editor Wang HF
References
- 1.Bartlett DL. Cancer of the liver. In: DeVita VT Jr, Hell-man S, Rosenberg SA., editors. Cancer: Principles & Practice of Oncology. Philadelphia: Lippincott; 2005. pp. 986–1009. [Google Scholar]
- 2.Groopman JD, Wogan GN, Roebuck BD, Kensler TW. Molecular biomarkers for aflatoxins and their application to human cancer prevention. Cancer Res. 1994;54:1907s–1911s. [PubMed] [Google Scholar]
- 3.Laureys G, Barton DE, Ullrich A, Francke U. Chromosomal mapping of the gene for the type II insulin-like growth factor receptor/cation-independent mannose 6-phosphate receptor in man and mouse. Genomics. 1988;3:224–229. doi: 10.1016/0888-7543(88)90083-3. [DOI] [PubMed] [Google Scholar]
- 4.Buendia MA. Genetics of hepatocellular carcinoma. Semin Cancer Biol. 2000;10:185–200. doi: 10.1006/scbi.2000.0319. [DOI] [PubMed] [Google Scholar]
- 5.Jirtle RL. Mannose 6-phosphate receptors. In: Creidton TE, editor. Encyclopedia of Molecular Biology. New York: Wiley-Liss; 1999. pp. 1441–1447. [Google Scholar]
- 6.Motyka B, Korbutt G, Pinkoski MJ, Heibein JA, Caputo A, Hobman M, Barry M, Shostak I, Sawchuk T, Holmes CF, et al. Mannose 6-phosphate/insulin-like growth factor II receptor is a death receptor for granzyme B during cytotoxic T cell-induced apoptosis. Cell. 2000;103:491–500. doi: 10.1016/s0092-8674(00)00140-9. [DOI] [PubMed] [Google Scholar]
- 7.Filson AJ, Louvi A, Efstratiadis A, Robertson EJ. Rescue of the T-associated maternal effect in mice carrying null mutations in Igf-2 and Igf2r, two reciprocally imprinted genes. Development. 1993;118:731–736. doi: 10.1242/dev.118.3.731. [DOI] [PubMed] [Google Scholar]
- 8.Young LE, Fernandes K, McEvoy TG, Butterwith SC, Gutierrez CG, Carolan C, Broadbent PJ, Robinson JJ, Wilmut I, Sinclair KD. Epigenetic change in IGF2R is associated with fetal overgrowth after sheep embryo culture. Nat Genet. 2001;27:153–154. doi: 10.1038/84769. [DOI] [PubMed] [Google Scholar]
- 9.Yamada T, De Souza AT, Finkelstein S, Jirtle RL. Loss of the gene encoding mannose 6-phosphate/insulin-like growth factor II receptor is an early event in liver carcinogenesis. Proc Natl Acad Sci USA. 1997;94:10351–10355. doi: 10.1073/pnas.94.19.10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong FM, Anscher MS, Washington MK, Killian JK, Jirtle RL. M6P/IGF2R is mutated in squamous cell carcinoma of the lung. Oncogene. 2000;19:1572–1578. doi: 10.1038/sj.onc.1203437. [DOI] [PubMed] [Google Scholar]
- 11.Ouyang H, Shiwaku HO, Hagiwara H, Miura K, Abe T, Kato Y, Ohtani H, Shiiba K, Souza RF, Meltzer SJ, et al. The insulin-like growth factor II receptor gene is mutated in genetically unstable cancers of the endometrium, stomach, and colorectum. Cancer Res. 1997;57:1851–1854. [PubMed] [Google Scholar]
- 12.Hankins GR, De Souza AT, Bentley RC, Patel MR, Marks JR, Iglehart JD, Jirtle RL. M6P/IGF2 receptor: a candidate breast tumor suppressor gene. Oncogene. 1996;12:2003–2009. [PubMed] [Google Scholar]
- 13.Souza RF, Wang S, Thakar M, Smolinski KN, Yin J, Zou TT, Kong D, Abraham JM, Toretsky JA, Meltzer SJ. Expression of the wild-type insulin-like growth factor II receptor gene suppresses growth and causes death in colorectal carcinoma cells. Oncogene. 1999;18:4063–4068. doi: 10.1038/sj.onc.1202768. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Ge Y, Landman N, Kang JX. Decreased expression of the mannose 6-phosphate/insulin-like growth factor-II receptor promotes growth of human breast cancer cells. BMC Cancer. 2002;2:18. doi: 10.1186/1471-2407-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu ZL, Luo DZ, Wen JM. Expression and significance of tumor-related genes in HCC. World J Gastroenterol. 2005;11:3850–3854. doi: 10.3748/wjg.v11.i25.3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang JX, Bell J, Beard RL, Chandraratna RA. Mannose 6-phosphate/insulin-like growth factor II receptor mediates the growth-inhibitory effects of retinoids. Cell Growth Differ. 1999;10:591–600. [PubMed] [Google Scholar]
- 17.Clurman B, Groudine M. Tumour-suppressor genes. Killer in search of a motive? Nature. 1997;389:122–123. doi: 10.1038/38116. [DOI] [PubMed] [Google Scholar]
- 18.De Souza AT, Hankins GR, Washington MK, Fine RL, Orton TC, Jirtle RL. Frequent loss of heterozygosity on 6q at the mannose 6-phosphate/insulin-like growth factor II receptor locus in human hepatocellular tumors. Oncogene. 1995;10:1725–1729. [PubMed] [Google Scholar]
- 19.Oka Y, Waterland RA, Killian JK, Nolan CM, Jang HS, Tohara K, Sakaguchi S, Yao T, Iwashita A, Yata Y, et al. M6P/IGF2R tumor suppressor gene mutated in hepatocellular carcinomas in Japan. Hepatology. 2002;35:1153–1163. doi: 10.1053/jhep.2002.32669. [DOI] [PubMed] [Google Scholar]
- 20.De Souza AT, Hankins GR, Washington MK, Orton TC, Jirtle RL. M6P/IGF2R gene is mutated in human hepatocellular carcinomas with loss of heterozygosity. Nat Genet. 1995;11:447–449. doi: 10.1038/ng1295-447. [DOI] [PubMed] [Google Scholar]
- 21.Souza RF, Appel R, Yin J, Wang S, Smolinski KN, Abraham JM, Zou TT, Shi YQ, Lei J, Cottrell J, et al. Microsatellite instability in the insulin-like growth factor II receptor gene in gastrointestinal tumours. Nat Genet. 1996;14:255–257. doi: 10.1038/ng1196-255. [DOI] [PubMed] [Google Scholar]
- 22.Osipo C, Dorman S, Frankfater A. Loss of insulin-like growth factor II receptor expression promotes growth in cancer by increasing intracellular signaling from both IGF-I and insulin receptors. Exp Cell Res. 2001;264:388–396. doi: 10.1006/excr.2000.5121. [DOI] [PubMed] [Google Scholar]
- 23.Robinson WP. Mechanisms leading to uniparental disomy and their clinical consequences. Bioessays. 2000;22:452–459. doi: 10.1002/(SICI)1521-1878(200005)22:5<452::AID-BIES7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 24.Barlow DP, Stoger R, Herrmann BG, Saito K, Schweifer N. The mouse insulin-like growth factor type-2 receptor is imprinted and closely linked to the Tme locus. Nature. 1991;349:84–87. doi: 10.1038/349084a0. [DOI] [PubMed] [Google Scholar]
- 25.Killian JK, Nolan CM, Wylie AA, Li T, Vu TH, Hoffman AR, Jirtle RL. Divergent evolution in M6P/IGF2R imprinting from the Jurassic to the Quaternary. Hum Mol Genet. 2001;10:1721–1728. doi: 10.1093/hmg/10.17.1721. [DOI] [PubMed] [Google Scholar]
- 26.Wutz A, Theussl HC, Dausman J, Jaenisch R, Barlow DP, Wagner EF. Non-imprinted Igf2r expression decreases growth and rescues the Tme mutation in mice. Development. 2001;128:1881–1887. doi: 10.1242/dev.128.10.1881. [DOI] [PubMed] [Google Scholar]
- 27.Islam MQ, Islam K. A new functional classification of tumor-suppressing genes and its therapeutic implications. Bioessays. 2000;22:274–285. doi: 10.1002/(SICI)1521-1878(200003)22:3<274::AID-BIES9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 28.Quon KC, Berns A. Haplo-insufficiency? Let me count the ways. Genes Dev. 2001;15:2917–2921. doi: 10.1101/gad.949001. [DOI] [PubMed] [Google Scholar]
- 29.Lynch CJ, Milner J. Loss of one p53 allele results in four-fold reduction of p53 mRNA and protein: a basis for p53 haplo-insufficiency. Oncogene. 2006;25:3463–3470. doi: 10.1038/sj.onc.1209387. [DOI] [PubMed] [Google Scholar]
- 30.Jirtle RL. Genomic imprinting and cancer. Exp Cell Res. 1999;248:18–24. doi: 10.1006/excr.1999.4453. [DOI] [PubMed] [Google Scholar]