Abstract
Hepatic splenosis refers to heterotopic auto-transplantation and implantation of splenic tissue resulting from the spillage of cells from the spleen after splenic trauma or splenectomy. The true incidence of splenosis is unknown, because this entity is usually an incidental finding at surgery. Splenic implants are usually multiple, and can be localized anywhere in the peritoneal cavity. Splenic implants in the peritoneal cavity may be confused with renal tumors, abdominal lymphomas and endometriosis. We describe computed tomography (CT) and magnetic resonance imaging (MRI) findings in a rare case of multiple intra-abdominal splenosis located along the hepatic surface and adjacent to the upper pole of the right kidney, mimicking a renal neoplasm.
Keywords: Abdomen, Computed tomography, Magnetic resonance imaging, Liver, Spleen
INTRODUCTION
Hepatic splenosis refers to heterotopic auto-transplantation and implantation of splenic tissue resulting from the spillage of cells from the spleen after splenic trauma or splenectomy, occurring in up to 67% of patients who have a splenic rupture[1,2]. Splenic implants are usually multiple and can be localized anywhere in the peritoneal cavity, but they usually occur on the serosal surfaces of the small and large bowel, the peritoneum, the mesentery and the diaphragm[3].
We describe computed tomography (CT) and magnetic resonance imaging (MRI) findings in a rare case of intra-abdominal multiple splenosis located along the hepatic surface and in close proximity to the upper pole of the right kidney, mimicking a renal neoplasm.
CASE REPORT
A 39-year-old man with a history of Crohn’s disease was admitted to our institution because of persistent abdominal pain. Physical examination and past medical history were unremarkable except for the previous history of chronic inflammatory bowel disease and an emergency splenectomy performed at the age of 15 after a car accident. An abdominal ultrasound was performed, revealing small bowel wall thickening at the level of the terminal ileum and minimal ascites in the peritoneal cavity. Ultrasound also revealed the presence of a 4 cm solid echogenic mass in the upper pole of the right kidney.
An helical CT examination showed a well-demarcated 3 cm mass in the sub-capsular posterior portion of the seventh segment of the right hepatic lobe adjacent to the upper pole of the right kidney. The mass was hypodense compared with the surrounding liver parenchyma on unenhanced helical CT examination, and showed heterogeneous enhancement in the arterial phase after the administration of contrast material, becoming hypodense compared with the surrounding parenchyma, during the portal (Figure 1) and equilibrium phases. The CT scan also identified two similar nodular lesions medially to the left lobe of the liver, and adjacent to the upper pole of the left kidney and the pancreatic tail (Figure 1).
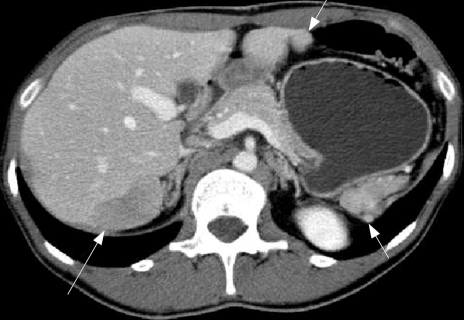
Figure 1.
Contrast-enhanced helical CT obtained during the portal phase of acquisition, showing a hypodense 3 cm lesion along the posterior surface of the seventh segment of the right lobe of the liver (long white arrow), and two similar nodular lesions medially to the left lobe of the liver and adjacent to the upper pole of the left kidney and the pancreatic tail (small white arrows).
A contrast-enhanced helical MRI scan was subsequently obtained, which confirmed the presence of a 3 cm hepatic lesion along the posterior surface of the seventh segment and in close proximity to the upper pole of the right kidney. Furthermore, MRI identified two additional lesions along the lateral surface of the right hepatic lobe and more clearly identified the other intra-abdominal nodular implants medially to the left hepatic lobe and adjacent to the upper pole of the left kidney and the pancreatic tail. These lesions appeared hypointense on T1-weighted unenhanced MRI scans (Figure 2A) and slightly hyperintense on T2-weighted images (Figure 2B), showing nonhomogeneous enhancement during the arterial phase, and hypointensity during the portal and equilibrium phases. The patient subsequently underwent surgical resection of the mass described along the surface of the seventh segment of the liver and adjacent to the upper pole of the right kidney, to exclude the presence of a renal neoplasm. Histopathologic examination indeed demonstrated the benign nature of the lesion, which consisted of splenic tissue. In addition, surgical exploration confirmed the presence of additional foci of splenic tissue in the abdominal cavity.
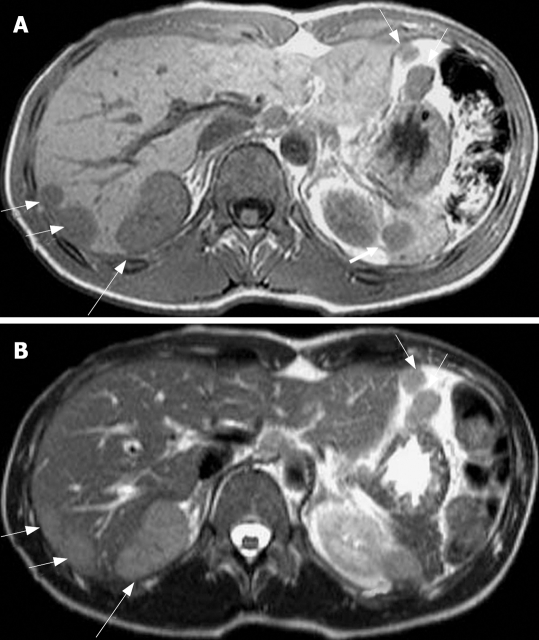
Figure 2.
Different image showing a hypointense 3 cm lesion along the posterior surface of the seventh segment of the right lobe of the liver (long white arrow) and 5 additional lesions in the sub-capsular portion of the seventh segment of the liver, medially to the left lobe of the liver and adjacent to the upper pole of the left kidney and the pancreatic tail (small white arrows). A: Unenhanced T1-weighted (TR: 218, TE: 4.6 ms) axial MRI scan; B: T2-weighted (TR: 417, TE: 80 ms) axial image.
DISCUSSION
Hepatic splenosis or the heterotopic implantation of splenic tissue after splenic trauma or splenectomy is a common but under diagnosed entity, occurring in up to 67% of patients who have suffered from a splenic rupture[1–4]. The true incidence of this rare condition is unknown, because splenosis is usually an incidental finding at surgery. The implants can be solitary or multiple, and can occur throughout the peritoneal cavity or chest[3] if splenic rupture is associated with a diaphragmatic tear. The nodules of splenosis do not generally grow to a large size, because they do not have their own blood supply. Although splenic implants are generally asymptomatic, they can lead to recurrent episodes of abdominal pain or small bowel obstruction secondary to adhesive bands of splenic implants. Most patients who undergo surgery for splenosis present to the surgeon with a diagnosis of intestinal obstruction or appendicitis. Although several cases of splenosis have been described in the past[1,5], this case is the first to describe multiple intra-abdominal heterotopic splenic implants, particularly involving the sub-capsular portion of the liver and the right retroperitoneal space, adjacent to the upper pole of the right kidney, with correlative CT and MRI findings. Differential diagnoses of splenosis include endometriosis, peritoneal mesothelioma, renal neoplasms[6], abdominal lymphomas[7] hepatic adenomas[8] and peritoneal metastatic implants. Both 99mTc-red blood cell SPECT scans and 99mTc-sulphur colloid scans can also be used to differentiate splenosis from malignancies and several reports have described the usefulness of these nuclear medicine techniques to avoid unnecessary surgical intervention[9,10]. MRI contrast agents composed of super-paramagnetic iron oxide particles that show a tissue-specific bio-distribution to phagocytic reticuloendothelial cells of liver and spleen after intravenous injection, have also been used in the past in patients with splenosis[3]. These agents produce local inhomogeneities in the magnetic field causing rapid dephasing of transverse magnetization, resulting in a loss of signal intensities on MRI of both ectopic splenic tissue and normal spleen. MRI offers the advantages over nuclear medicine techniques of combining higher spatial resolution with a physiological test of reticuloendothelial cell uptake[11]. Due to MRI’s superior contrast resolution compared with CT, MRI better enabled the identification of multiple intra-abdominal splenic lesions, in particular along the posterior hepatic surface, allowing the presence of a renal neoplasm in the right retroperitoneal space to be excluded. MRI findings coupled with the patient’s history of previous splenectomy allowed the correct diagnosis of multiple intra-abdominal splenosis to be made.
Peer reviewer: Cynthia Levy, MD, Assistant Professor of Medicine, Division of Gastroenterology, Hepatology, and Nutrition, University of Florida College of Medicine, Unite States
S- Editor Yang RH L- Editor McGowan D E- Editor Lu W
References
- 1.Fleming CR, Dickson ER, Harrison EG Jr. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414–419. doi: 10.1016/0002-9343(76)90380-6. [DOI] [PubMed] [Google Scholar]
- 2.De Vuysere S, Van Steenbergen W, Aerts R, Van Hauwaert H, Van Beckevoort D, Van Hoe L. Intrahepatic splenosis: imaging features. Abdom Imaging. 2000;25:187–189. doi: 10.1007/s002619910042. [DOI] [PubMed] [Google Scholar]
- 3.Berman AJ, Zahalsky MP, Okon SA, Wagner JR. Distinguishing splenosis from renal masses using ferumoxide-enhanced magnetic resonance imaging. Urology. 2003;62:748. doi: 10.1016/s0090-4295(03)00509-0. [DOI] [PubMed] [Google Scholar]
- 4.Brancatelli G, Vilgrain V, Zappa M, Lagalla R. Case 80: splenosis. Radiology. 2005;234:728–732. doi: 10.1148/radiol.2343030695. [DOI] [PubMed] [Google Scholar]
- 5.Kim KA, Park CM, Kim CH, Choi SY, Park SW, Kang EY, Seol HY, Cha IH. An interesting hepatic mass: splenosis mimicking a hepatocellular carcinoma (2003:9b) Eur Radiol. 2003;13:2713–2715. doi: 10.1007/s00330-003-1978-5. [DOI] [PubMed] [Google Scholar]
- 6.Kiser JW, Fagien M, Clore FF. Splenosis mimicking a left renal mass. AJR Am J Roentgenol. 1996;167:1508–1509. doi: 10.2214/ajr.167.6.8956586. [DOI] [PubMed] [Google Scholar]
- 7.Schenkein DP, Ahmed E. Case records of the Massachusetts General Hospital. Weekly clinic-pathological exercises: Case 29-1995 A 65-year-old man with mediastinal Hodgkin’s disease and a pelvic mass. N Engl J Med. 1995;333:784–791. doi: 10.1056/NEJM199509213331208. [DOI] [PubMed] [Google Scholar]
- 8.Gruen DR, Gollub MJ. Intrahepatic splenosis mimicking hepatic adenoma. AJR Am J Roentgenol. 1997;168:725–726. doi: 10.2214/ajr.168.3.9057523. [DOI] [PubMed] [Google Scholar]
- 9.Williams G, Rosen MP, Parker JA, Kolodny GM. Splenic implants detected by SPECT images of Tc-99m labeled damaged red blood cells. Clin Nucl Med. 2006;31:467–469. doi: 10.1097/01.rlu.0000226937.42087.1f. [DOI] [PubMed] [Google Scholar]
- 10.Hagan I, Hopkins R, Lyburn I. Superior demonstration of splenosis by heat-denatured Tc-99m red blood cell scintigraphy compared with Tc-99m sulfur colloid scintigraphy. Clin Nucl Med. 2006;31:463–466. doi: 10.1097/01.rlu.0000226907.36840.b3. [DOI] [PubMed] [Google Scholar]
- 11.Storm BL, Abbitt PL, Allen DA, Ros PR. Splenosis: superparamagnetic iron oxide-enhanced MR imaging. AJR Am J Roentgenol. 1992;159:333–335. doi: 10.2214/ajr.159.2.1632350. [DOI] [PubMed] [Google Scholar]