Abstract
Cervical cord compression due to osteochondroma in hereditary multiple exostosis (HME) is a rare condition, especially in young children. In this report, we discuss a rare case of cervical osteochondroma presenting as Brown-Sequard syndrome (BSS) in a 7-year-old boy with HME. The child was admitted because of hemiparesis involving the right limbs and hypoesthesia on the left side following mild trauma. MR image revealed cord compression by osteochondroma of the C7 lamina. We removed the osteocondroma and the neurological deficit was improved.
Keywords: Osteochondroma, Hereditary multiple exostosis, Brown-Sequard syndrome
INTRODUCTION
Hereditary multiple exostosis (HME) is the most common form of bone dysplasia2,5). It is an autosomal dominant disease with predominance in males and a benign condition characterized by presence of multiple exostosis or osteochondroma arising from long and flat bones2,9). Spinal cord compression resulting from vertebral osteochondroma is a rare complication and generally becomes symptomatic during the second and third decades of life5,7). We report an unusual case of cervical osteochondroma presenting as Brown-Sequard syndrome (BSS) following mild trauma in a 7-year-old boy with HME.
CASE REPORT
History and examination
A 7-year-old boy complained of motor weakness involving the right extremities following fall down 1 month before admission. The boy complained of difficulty in spooning up and assembling a toy. On physical examination, he had multiple palpable exostosis over the bones of his limbs and clavicles. The patient was diagnosed with HME at the age of 6 years and his father and grandmother also had HME. Neurological examination revealed BSS showing a slight hemiparesis (grade 4) on the right side and hypesthesia on the left side below C6 dermatome. MR image showed a mass arising from the right C6 lamina with evident cord compression (Fig. 1). Further investigation with computed tomography (CT) demonstrated a sessile bony mass arising from the upper border of the C7 lamina and projecting ventral to the C6 lamina, not arising from the C6 lamina (Fig. 2).
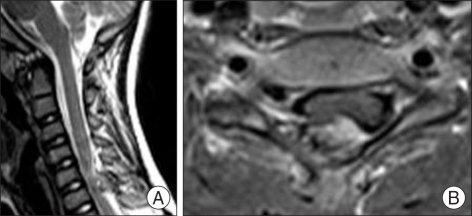
Fig. 1.
Sagittal (A) and axial (B) T1-weighted magnetic resonance images showing an elliptical mass compressing the right posterolateral spinal cord at the C6 segment.
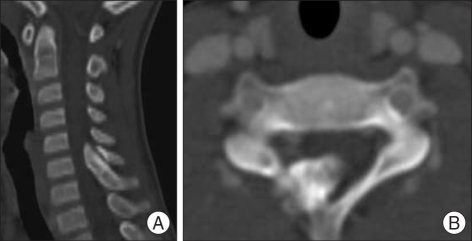
Fig. 2.
Sagittal (A) and axial (B) computed tomography scan showing a sessile bony mass arising from the upper border of the C7 lamina projecting ventral to the C6 lamina.
Operation
We performed a partial hemilaminectomy of the upper C7 portion and lower C6 portion without facet damage and excised the mass totally. The diameter of the mass was 1 cm and the inner surface was white and smooth due to the covering of cartilage (Fig. 3). There was no adhesion between the mass and dura, and we were able to remove the mass without difficulty. Histopathological examination demonstrated fibrocartilaginous cells with ossification in the ligament and confirmed osteochondroma
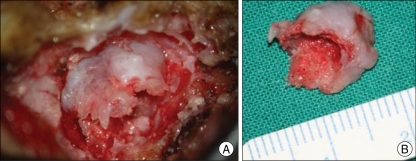
Fig. 3.
Intraoperative finding (A) showing total resection through right partial hemilaminectomy and a resected mass (B) 1 cm in diameter showing covering with a thin layer of cartilage.
Postoperative course
After the operation, the patient's weakness was improved to grade 4+/5 and sensory deficit completely disappeared. The patient was discharged by the eighth postoperative day.
DISCUSSION
HME is a benign condition characterized by multiple cartilage-capped bony outgrowths in the metaphysis of long bone and flat bones2,5,7). It is a genetic disorder with an autosomal dominant pattern of inheritance2,9). In our case, the patient's father and grandmother had HME, so we could easily make the diagnosis of HME preoperatively. Malignant transformation may occur in up to 20% of patients with HME4,10). These exostosis, also called osteochondromas, involve the vertebral column in approximately 7-9% of cases, and 50% of these cases arise from the cervical spine5). Spinal cord compression resulting from HME occurs in young adults, usually in the second and third decades with male predominance2,5,6). In review of the literature, the youngest patient with cervical osteochondroma was 7 years of age, same as our case3). The most common site of involvement was C2 and C7. The duration of symptoms is variable and ranges from 1 month to 9 years5,8). However, acute onset is very rare, especially combined with BBS, in a young child. Identification of motor weakness in a child is relatively easy but identification of sensory loss is not because verbal expression of specific sensory loss is difficult at this age, especially when the degree of neurological deficit is mild. Therefore, the age of 7 years may be the minimal age at which BBS can be diagnosed. The patient's age, specific presenting symptom as BBS, and involvement of the C7 lamina make our case extremely rare.
In most cases, the surgical outcome is good and laminectomy is the most common treatment method4). However, to prevent postlaminectomy kyphosis, laminectomy should be minimized, especially, in young patients. Laminotomy or posterior fusion could be chosen as an alternative method1). In our case, we tried to minimize laminectomy through partial hemilaminectomy, and postlaminectomy kyphosis was not observed during follow up period.
CONCLUSION
We report a rare case of cervical osteochondroma presenting BSS in a 7-year-old boy with HME. In young children, the cervical osteochondroma can be totally removed and laminectomy can be minimized to prevent postlaminectomy kyphosis.
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2008 (No. 6-2008-0290).
References
- 1.Bhojraj SY, Panjwani JS. A new management approach to decompression, posterior stabilization, and fusion for cervical laminar exostosis with cord compression in a case of diaphyseal aclasis. Case report and review of the literature. Spine. 1993;18:1376–1379. doi: 10.1097/00007632-199308000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Cirak B, Karabulut N, Palaoglu S. Cervical osteochondroma as a cause of spinal cord compression in a patient with hereditary multiple exostoses : computed tomography and magnetic resonance imaging findings. Australas Radiol. 2002;46:309–311. doi: 10.1046/j.1440-1673.2002.01067.x. [DOI] [PubMed] [Google Scholar]
- 3.Eder HG, Oberbauer RW, Ranner G. Cervical cord compression in hereditary multiple exostoses. J Neurosurg Sci. 1993;37:53–56. [PubMed] [Google Scholar]
- 4.Gille O, Pointillart V, Vital JM. Course of spinal solitary osteochondromas. Spine. 2004;30:E13–E19. [PubMed] [Google Scholar]
- 5.Giudicissi-Filho M, de Holanda CVM, Borba LAB, Rassi-Neto A, Ribeiro CAA, de Oliveira JG. Cervical spinal cord compression due to an osteochondroma in hereditary multiple exostosis : case report and review of the literature. Surg Neurol. 2006;66(Suppl 3):S7–S11. doi: 10.1016/j.surneu.2006.05.057. [DOI] [PubMed] [Google Scholar]
- 6.Khosla A, Martin DS, Awwad EE. The solitary intraspinal vertebral osteochondroma. An unusual cause of compressive myelopathy : features and literature review. Spine. 1999;24:77–81. doi: 10.1097/00007632-199901010-00019. [DOI] [PubMed] [Google Scholar]
- 7.Ratliff J, Voorhies R. Osteochondroma of the C5 lamina with cord compression : case report and review of the literature. Spine. 2000;25:1293–1295. doi: 10.1097/00007632-200005150-00017. [DOI] [PubMed] [Google Scholar]
- 8.Song KJ, Lee KB. Solitary osteochondroma of the thoracic spine causing myelopathy. Eur J Pediatr Surg. 2007;17:210–213. doi: 10.1055/s-2007-965124. [DOI] [PubMed] [Google Scholar]
- 9.Stieber JR, Dormans JP. Manifestations of hereditary multiple exostoses. J Am Acad Orthop Surg. 2005;13:110–120. doi: 10.5435/00124635-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Willms R, Hartwig CH, Bohm P, Sell S. Malignant transformation of a multiple cartilaginous exostosis-a case report. Int Orthop. 1997;21:133–136. doi: 10.1007/s002640050136. [DOI] [PMC free article] [PubMed] [Google Scholar]