Abstract
The aim of this study was to assess the feasibility and efficacy of laparoscopic myomectomy (LM) for large myomas. A subpopulation of 51 patients with myomas 8 cm or larger in diameter was selected from 155 patients who underwent LM at Kangbuk Samsung Hospital from July 2003 to November 2006. The mean age of the patients was 34.9±5.6 yr, mean parity was 0.6±0.9, and 8 patients had a previous operative history. The most common operative indication was a palpable abdominal mass (24 patients, 47%). The mean operating time was 85.6±38.9 min, and the mean diameter of the largest myoma was 9.3±1.8 cm. The mean change in hemoglobin concentration was 2.1±1.2 g/dL. Histopathological diagnosis included 49 patients of leiomyoma (96.1%) and 2 patients of leiomyoma with adenomyosis (3.9%). Postoperatively, a transfusion was done in 7 patients, and a case of subcutaneous emphysema was noted. None of the operations was switched to laparotomy. With the newly-developed screw and the port placement system that was modified from the Choi's 4-trocar method to obtain better surgical vision, LM of large myomas proved to be one of the efficient and feasible methods.
Keywords: Laparoscopic Myomectomy, Myoma Uteri, Laparoscopy
INTRODUCTION
Laparoscopic myomectomy (LM) currently brings more attention because of increased demands on uterine conservation and less invasive management of myomas. The advantages of LM are shorter hospitalization, faster recovery, fewer adhesions, and less blood loss (1). In spite of the increasing improvements in laparoscopic instruments and techniques, advanced laparoscopic technical skills are required to perform LM with success (2). Technical problems inherent to the removal of large uterine myomas include hemostasis, uterine closure, and removal of the uterine tissue. Furthermore, the risk of laparoconversion is proportional to the surgeons' technical expertise (3-5). To overcome these limitations, minilaparotomic myomectomy or gasless LM is recommended for large uterine myomas (6-8). However, LM offers less postoperative analgesia and faster postoperative recovery than minilaparotomic myomectomy, and the additional instruments required in gasless LM are not needed in LM (2). To perform successful LM with the advantages mentioned above, we developed a new screw for easy pulling and pushing movement, which replaces the conventional screw that is easily broken. The objective of this study is to verify efficacy and feasibility of LM for large myomas through the newly-developed screw and the port placement system that has derived from the Choi's 4-trocar method (9).
MATERIALS AND METHODS
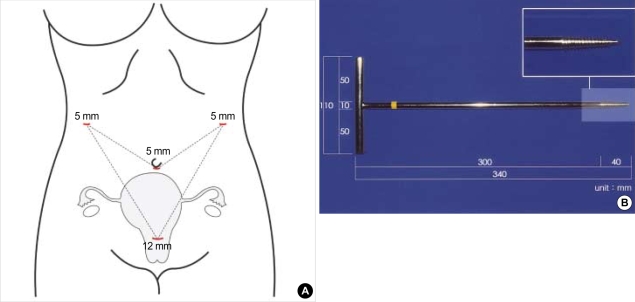
A subpopulation of 51 patients whose myomas were 8 cm or larger in diameter was selected from 155 patients who underwent LM at Kangbuk Samsung Hospital from July 2003 to November 2006. The size of myoma was confirmed by ultrasonography prior to the operation. All patients underwent preoperative assessments including detailed medical history, pelvic examination, gynecologic ultrasonography, and Pap smear. All procedures were performed by the surgeon (the corresponding author) who developed the port placement system and the new screw (Fig. 1). We reviewed the clinical charts, and the operative and anesthetic records, and analyzed the data on the patients' age, parity, operating time, diameter of the largest myoma, number of the removed myomas, hospital stay, change in hemoglobin concentration from before surgery to postoperative day 1, operative indications, previous operative history, histopathological reports, complications, and the pregnancy state after LM. The total operating time was defined as the time from the insertion of the first trocar to closure of all port sites. Statistical analysis was performed by using the findings from SAS program (V 9.1, SAS Institute Inc., NC). Student's t-test and chi-square test were used to compare the findings from this study with those from previous studies. A p value less than .05 was considered as statistically significant.
Fig. 1.
(A) Port placement system of laparoscopic myomectomy for large myomas. (B) New metallic screw.
Operative techniques
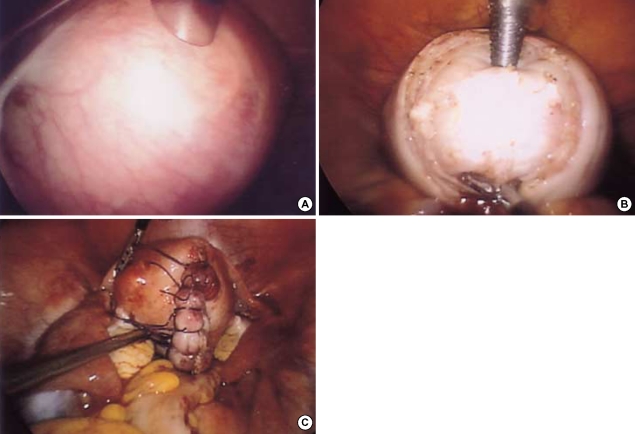
The procedure was performed under general anesthesia with endotracheal intubation. The patient was placed in a modified dorsal lithotomy position, a foley catheter was inserted before a uterine manipulator was fixed on the cervix to allow uterine manipulation. As shown in Fig. 1A, the modified Choi's 4-trocar method was utilized in all operations during trocar insertion (9). Carbon dioxide was insufflated through the trocar sleeve to create a pneumoperitoneum, and the intra-abdominal pressure was maintained at 15 mmHg. When surgical preparation was completed, 30 mL of a solution containing 10 IU vasopressin (Vasopressin®, Hanlim Pharm, Yongin, Korea) per 100 mL normal saline was injected into the tissue adjacent to the base and the capsule of the uterine myoma. A vertical incision was made in the most prominent portion of the uterine myoma to partially remove the capsule of the uterine myoma. Subsequently, the screw was inserted perpendicularly into the most prominent part of myoma through the suprapubic 12-mm trocar. In the next step, the operator held the knob of the screw in his left hand and operated metzembaum scissors or grasping forceps with his right hand during dissection of the myoma. The first assistant, who held a 5-mm telescope in his left hand and grasping forceps in his right hand, helped the operator dissect the uterine myoma. Traction and countertraction was applied to the uterine myoma using the screw with ease. After dissection, the myoma was placed within a cul-de-sac. A direct vision confirmed any damages in the uterine endometrium. Approximation and hemostasis of the inner myometrial layers were done using interrupted sutures of 1-0 polyglactin 910 (Vicryl®, Ethicon Inc, Somerville, NJ, U.S.A.) via an intracorporeal suture technique. For the outer myometrial layer and the serosa, approximation was done via an extracorporeal suture technique using interrupted sutures with polyglycolic acid sutures (Lap-suture®, Sejong Medical, Seoul, Korea) (Fig. 2). After the uterus was stitched, it was examined to determine the presence of uterine bleeding. We selectively used bilateral uterine artery ligation for patients who wanted to preserve their uterus although they did not want future pregnancy. For the purpose of hemostasis, bipolar coagulator or unipolar coagulator was not used in the operation, and unipolar coagulator was rarely used while separating the myoma from a capsule. If there was no bleeding, a 12-mm diameter trocar was removed. Then, a morcellator (X-tract Tissue Morcellator®, Gynecare, Somerville, NJ, U.S.A.) was placed into the abdominal cavity to enable safe removal of the uterine myoma from the abdominal cavity. If no further bleeding was present, intraabdominal irrigation was performed, and the incision site was covered with an absorbable adhesion barrier (Interceed®, Gynecare, Somerville, NJ, U.S.A.). Although no bleeding was present at the time, the possibility of delayed bleeding still existed, and thereby the drain was inserted through 5-mm trocar and CO2 was eliminated.
Fig. 2.
(A) Intramural myoma of 9 cm in diameter on the posterior uterine wall on ultrasonography. (B) An image of a new metallic screw fixed to the myoma after peeling off the capsule of the myoma. (C) An image of the uterus after laparoscopic myomectomy.
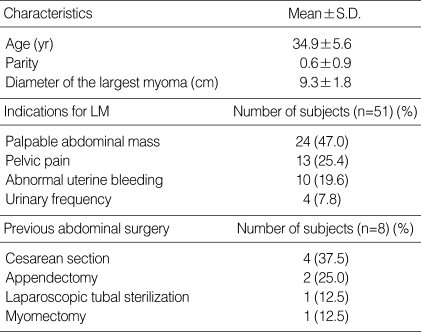
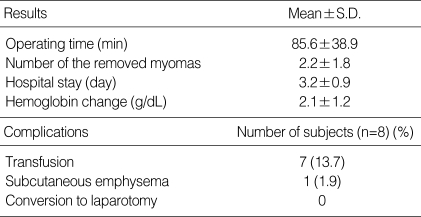
RESULTS
The characteristics of patients are summarized in Table 1. The diameter of the myoma was greater than or equal to 15 cm in 2 cases (15.2 cm and 15.0 cm) and was between 10 cm and 14 cm in 12 cases. The total number of the resected myomas was 111. With regard to the position of the uterine myoma, intramural was 46 patients and subserosal was 5 patients. The post-operative results are summarized in Table 2. Combined operations including laparoscopic incidental appendectomy in 12 patients, ovarian cystectomy in 6 patients, and adhesiolysis in 3 patients were done with LM. The heaviest weight of the remored myoma was 795 gm. Among the patients who did not want future pregnancy, and was predicted to have severe bleeding, two patients underwent laparoscopic bilateral uterine artery ligation. A morcellator was used to extract the resected myomas from 48 patients. The posterior culdotomy was performed to safely extract myoma in 3 remaining patients who had previously received vaginal delivery. The histopathological diagnosis was leiomyoma in 49 patients (96.1%) and leiomyoma with adenomyosis in 2 patients (3.9%). For the case of adenomyosis, since no visible difference was found with leiomyoma, the operative method was very similar to the operation performed in the other patients. None of the procedures had to be converted to laparotomy. There was no intraoperative complication. Seven patients underwent transfusion both intraoperatively and postoperatively, of whom six received 2 pints of packed RBC and one received 4 pints. Because of the low hemoglobin value of 8-9 g/dL prior to operation in 3 patients, transfusion was performed regardless of minor bleeding. For one patient with seven myomas and 3 patients with larger myomas each with a diameter of 11 cm, 13 cm, and 15 cm, transfusion was performed due to severe bleeding. The case of myoma with a diameter of 13 cm required 4 pints of transfusion. Subcutaneous emphysema occurred in one patient, but no further events were noted after conservative treatment. Three patients became pregnant following LM. Two of these women gave birth to a healthy baby by cesarean section, and neither intraabdominal adhesion nor dehiscence was noted in the operation field. One remaining patient received vaginal delivery and there were no complications such as uterine rupture.
Table 1.
Clinical characteristics of laparoscopic myomectomy
LM, laparoscopic myomectomy.
Table 2.
Operative and postoperative data
DISCUSSION
In recent years, social and cultural changes, and the wide-spread use of contraceptives have delayed the age of first pregnancy. Consequently, uterine preservation is increasingly requested when symptomatic myomas are diagnosed during the reproductive ages (2). In comparison with abdominal myomectomy (AM), LM provides advantages of shorter hospitalization, faster recovery, fewer adhesions, less blood loss, and better cosmetic effects than AM (1, 10).
The surgical procedure for performing LM of a large uterine myoma consists of three stages. Primarily, surgeons must obtain the good surgical vision and dissect the myoma away from the normal uterine tissue. In patients with a uterine myoma large enough to reach the umbilical level, it has been suggested that a trocar be positioned superior to the umbilicus, the high epigastric port-placement technique (11). However, there are a few disadvantages, such as the need for 7 trocars and increased cost associated with the high epigastric port-placement technique. Thus we have suggested the new technique called Choi's 4-trocar method for LM (9). We found several advantages of this method. First, the operator is able to use both hands freely and to improve visibility through 2 trocars placed on either side of the epigastric area on the upper parallel line from the virtual line drawn horizontally across the umbilicus. If the uterus is too large and it intercepts the view of the right, the 5-mm telescope can be replaced into the right trocar, with the other surgical instruments replaced into the umbilical trocar. Thus it is easier to operate on the right side of the uterus. The minimal directional changes in the operator's sight because of the high lateral trocar, ensure the visibility of the right side, that the operator does not have to move, and that no more than 4 trocars are required. Secondly, in the Choi's 4-trocar method, all trocars are located in the "safe zone" avoiding potential injury to the ilioinguinal and iliohypogastric nerves and the inferior epigastric arteries. Third, the risk of injury, the risk of intestinal herniation, and the scar size are reduced by placing the telescope into both the right and left 5-mm trocar ports and by use of only one 12-mm trocar for myoma screw or morcellator (9). As the effective enucleation of the myoma is the most crucial step in LM, surgeons must fully extract the uterine myoma, irrespective of its size or location (12). Large uterine myomas are difficult to enucleate because they restrict the amount of space available for pushing and pulling actions. The softening that accompanies degenerative changes of the uterine myomas makes it very difficult to perform maneuvers such as traction-countertraction and insertion using the conventional myoma screw (13). The conventional type of screw has the following disadvantages: 1) it is not firmly fixed to the myoma; 2) it does not exert sufficient force during traction and is easily broken while manipulating large uterine myomas; and 3) it cannot be easily inserted into soft large uterine myomas that have undergone degenerative changes. To overcome the disadvantages of the conventional screw, we developed a 10-mm metallic screw. This screw is effectively designed for easier and stronger fixation on myoma. Moreover, the connecting part of the former screw between bolt and shaft that measured only 2.2 mm in diameter is easily breakable when handling a large myoma, but the identical size of diameter in the proximal part of a bolt and a shaft of the new screw reduces the risk of break-age cohile successfully passing on the force of operator (Fig. 1B). This screw can be fixed firmly to the uterine myoma, which enables tension to be applied in all directions, facilitating extraction of the uterine myoma and shortening the operating time. The second step of the LM procedure comprises the reconstruction of defective area of the uterine myometrium and effective hemostasis. In instances of large defective areas resulting from surgery of large uterine myomas, the extracorporeal suture technique enhanced with the intracorporeal suture will be more effective for approximation, hemostasis, and the maintenance of integrity (14). Our experiences have shown the same effect. Finally, to extract the resected uterine myoma safely outside the abdominal cavity, posterior colpotomy is done via a vaginal or an abdominal route using a morcellator.
LM has shown no increase of complications such as uterine rupture than AM (15, 16). Among the tree post-LM patients who became pregnant in our series, two patients received cesarean section and one patient received vaginal delivery, and none of the patients showed any sign of complication.
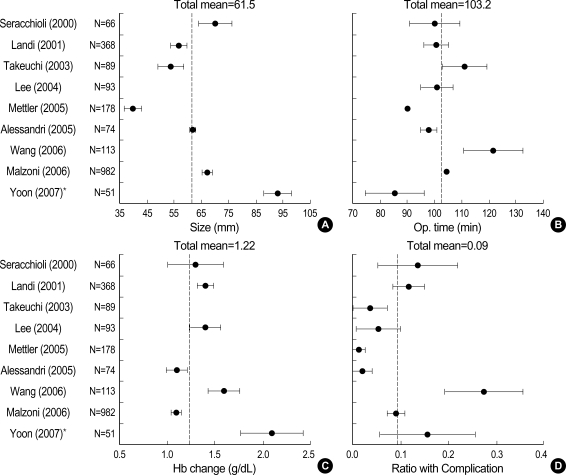
The first LM was performed by Semm et al. (17). Today, larger intramural myomas are also enucleated by LM. The previous studies on LM are summarized in Table 3 (2, 10, 12, 15, 18-21), and our results were compared with the previous data (Fig. 3). The results using a different unit from the previous studies and those without standard deviation were excluded from the analysis. The size of myoma in our study was larger than in other studies. The mean size of myomas in the previous studies was 61.5 mm, significantly smaller than that in our study (93±18 mm). Our operating time was shorter than the total mean operating time of the previous studies. Our study showed a higher Hb change (g/dL) compared to the total mean value of Hb change in the previous studies. The mean ratio with complication of our study was similar to that of the previous studies. Moreover, the previous studies showed major complications demanding a secondary operation, but our study showed only minor complications such as subcutaneous emphysema and transfusion. The laparoconversion rate, being 0-4.3% in the previous studies, was 0% in our study. The size of myoma has been reported to be in a positive correlation with blood loss, operating time, and laparoconversion rate (12, 18). Considering that the myoma size of our study is larger than that of previous studies, if we performed LM in the circumstance of the same myoma size, our study could produce even better results in operating time, complication, and laparoconversion rate with relatively comparable results in the hemoglobin change. In conclusion, the use of the new port placement system and the newly-developed screw has significantly improved efficiency and feasibility of LM for large myomas.
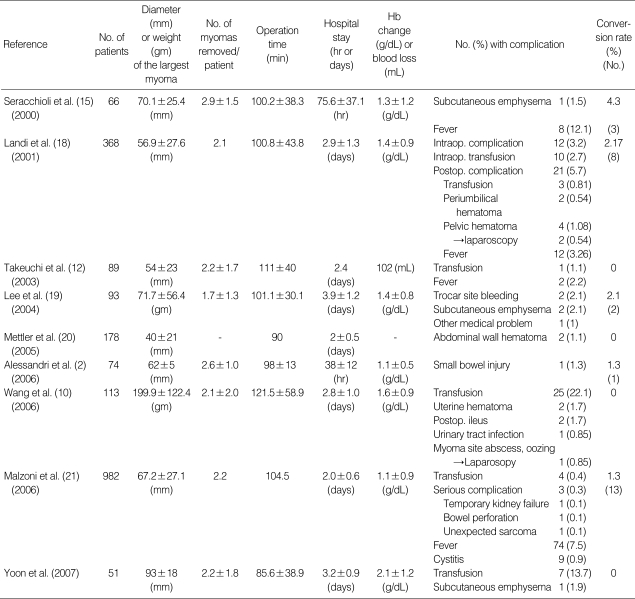
Table 3.
Summary of previous studies on laparoscopic myomectomy
Results are expressed as mean±S.D.
Fig. 3.
Comparison between this study and the previous studies in myoma size (A), operating time (B), hemoglobin change (C), and ratio with complication (D).
References
- 1.Hurst BS, Matthews ML, Marshburn PB. Laparoscopic myomectomy for symptomatic uterine myomas. Fertil Steril. 2005;83:1–23. doi: 10.1016/j.fertnstert.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Alessandri F, Lijoi D, Mistrangelo E, Ferrero S, Ragni N. Randomized study of laparoscopic versus minilaparotomic myomectomy for uterine myomas. J Minim Invasive Gynecol. 2006;13:92–97. doi: 10.1016/j.jmig.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Sinha R, Hegde A, Warty N, Patil N. Laparoscopic excision of very large myomas. J Am Assoc Gynecol Laparosc. 2003;10:461–468. doi: 10.1016/s1074-3804(05)60145-4. [DOI] [PubMed] [Google Scholar]
- 4.Marret H, Chevillot M, Giraudeau B. Factors influencing laparoconversions during the learning curve of laparoscopic myomectomy. Acta Obstet Gynecol Scand. 2006;85:324–329. doi: 10.1080/00016340500438165. [DOI] [PubMed] [Google Scholar]
- 5.Marret H, Chevillot M, Giraudeau B. A retrospective multicentre study comparing myomectomy by laparoscopy and laparotomy in current surgical practice. What are the best patient selection criteria? Eur J Obstet Gynecol Reprod Biol. 2004;117:82–86. doi: 10.1016/j.ejogrb.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 6.Damiani A, Melgrati L, Marziali M, Sesti F, Piccione E. Laparoscopic myomectomy for very large myomas using an isobaric (gasless) technique. JSLS. 2005;9:434–438. [PMC free article] [PubMed] [Google Scholar]
- 7.Glasser MH. Minilaparotomy myomectomy: a minimally invasive alternative for the large fibroid uterus. J Minim Invasive Gynecol. 2005;12:275–283. doi: 10.1016/j.jmig.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Fanfani F, Fagotti A, Bifulco G, Ercoli A, Malzoni M, Scambia G. A prospective study of laparoscopy versus minilaparotomy in the treatment of uterine myomas. J Minim Invasive Gynecol. 2005;12:470–474. doi: 10.1016/j.jmig.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Choi JS, Kyung YS, Kim KH, Lee KW, Han JS. The four-trocar method for performing laparoscopically-assisted vaginal hysterectomy on large uteri. J Minim Invasive Gynecol. 2006;13:276–280. doi: 10.1016/j.jmig.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Wang CJ, Yuen LT, Lee CL, Kay N, Soong YK. Laparoscopic myomectomy for large uterine fibroids: a comparative study. Surg Endosc. 2006;20:1427–1430. doi: 10.1007/s00464-005-0509-7. [DOI] [PubMed] [Google Scholar]
- 11.Lee YS. Benefits of high epigastric port placement for removing the very large uterus. J Am Assoc Gynecol Laparosc. 2001;8:425–428. doi: 10.1016/s1074-3804(05)60343-x. [DOI] [PubMed] [Google Scholar]
- 12.Takeuchi H, Kuwatsuru R. The indications, surgical techniques, and limitations of laparoscopic myomectomy. JSLS. 2003;7:89–95. [PMC free article] [PubMed] [Google Scholar]
- 13.Sinha R, Hegde A, Warty N, Mahajan C. Laparoscopic myomectomy: enucleation of the myoma by morcellation while it is attached to the uterus. J Minim Invasive Gynecol. 2005;12:284–289. doi: 10.1016/j.jmig.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Ostrzenski A. A new laparoscopic myomectomy technique for intramural fibroids penetrating the uterine cavity. Eur J Obstet Gynecol Reprod Biol. 1997;74:189–193. doi: 10.1016/s0301-2115(97)02751-6. [DOI] [PubMed] [Google Scholar]
- 15.Seracchioli R, Rossi S, Govoni F, Rossi E, Venturoli S, Bulletti C, Flamigni C. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: a randomized comparison with abdominal myomectomy. Hum Reprod. 2000;15:2663–2668. doi: 10.1093/humrep/15.12.2663. [DOI] [PubMed] [Google Scholar]
- 16.Kim HC, Oh ST. Safety and usefulness of laparoscopic myomectomy for intramural myoma in reproductive women. Korean J Obstet Gynecol. 2000;43:659–664. [Google Scholar]
- 17.Semm K, Mettler L. Technical progress in pelvic surgery via operative laparoscopy. Am J Obstet Gynecol. 1980;138:121–127. doi: 10.1016/0002-9378(80)90021-6. [DOI] [PubMed] [Google Scholar]
- 18.Landi S, Zaccoletti R, Ferrari L, Minelli L. Laparoscopic myomectomy: technique, complications, and ultrasound scan evaluations. J Am Assoc Gynecol Laparosc. 2001;8:231–240. doi: 10.1016/s1074-3804(05)60583-x. [DOI] [PubMed] [Google Scholar]
- 19.Lee SY, Ryu HH, Lee CB, Joo EH, Kim SK. Clinical review on 93 cases of laparoscopic myomectomy. Korean J Obstet Gynecol. 2004;47:1107–1112. [Google Scholar]
- 20.Mettler L, Schollmeyer T, Shelat NR, Jonat W. Update on laparoscopic myomectomy. J Gynecol Surg. 2005;2:173–177. [Google Scholar]
- 21.Malzoni M, Sizzi O, Rossetti A, Imperato F. Laparoscopic myomectomy: a report of 982 procedures. Surg Technol Int. 2006;15:123–129. [PubMed] [Google Scholar]