Abstract
We reported a 75-year-old diabetic man, who developed opacification and neovascularization of the posterior capsule after extracapsular cataract extraction and posterior chamber intraocular lens implantation. The patient was treated with two injections of 2.5 mg of intravitreal bevacizumab. The treatment produced an important regression of the posterior capsular new vessels, allowing us to perform a successful Nd:YAG capsulotomy, clearing the visual axis and improving the visualization of the posterior pole. Even though, best corrected visual acuity was 20/200 due to diabetic macular edema.
Keywords: posterior capsule opacification, posterior capsule neovascularization, cataract surgery, postoperative complications, intravitreal bevacizumab
Introduction
Cataract surgery in diabetic patients is associated with higher risk of postoperative complications. Posterior capsule opacification (PCO), anterior capsule phimosis, severe inflammation (fibrinous exudates and membrane), cystoid macular edema, and exacerbation of diabetic retinopathy are a few of the most important postoperative complications (Krupsky et al 1991; Chung et al 2002; Hayashi et al 2002; Hauser et al 2004; Ivancic et al 2005; Ebihara et al 2006).
However the progression to a proliferative state is a common condition in these patients, finding new vessels behind the posterior capsule is a rare event. This particular finding is a hallmark of proliferative progression. The term, “rubeosis capsulare”, coined by Eifrig and colleagues (1990) is used to address this condition.
The role of the vascular endothelial growth factor (VEGF) in the pathogenesis of ischemic retinopathies is well known. It is a key factor in the development of retinal vascularization and its blockade has been related with rapid regressions of retina and iris new vessels secondary to proliferative diabetic retinopathy (Avery et al 2006).
Bevacizumab (Avastin; Genentech, Inc, South San Francisco, CA, USA) is a full-length humanized anti-VEGF monoclonal antibody, approved in the United States for the treatment of metastatic colorectal cancer. It has been used in ophthalmology as an off-label treatment of choroidal neovascularization, central retinal vein occlusion, and proliferative diabetic retinopathy, with encouraging preliminary results (Yang et al 2003; Bakri et al 2007).
We reported; a case of posterior capsule neovascularization in a diabetic patient who presented adequate regression of the new vessels with intravitreal bevacizumab, allowing us to perform a successful Nd:YAG capsulotomy without serious complications.
Case report
A 75-year-old diabetic male was attended in our department with referral to slow progressive visual loss in both eyes since 2 years prior. The visual loss was more significant in the right eye. He had relevant medical history of long standing type 2 diabetes mellitus, high blood pressure, and amputation of the left inferior limb due to a severe infection. The patient also had history of extracapsular cataract extraction with intraocular lens (IOL), implantation without complications three years before the first symptom, and proliferative diabetic retinopathy treated with panretinal photocoagulation in both eyes.
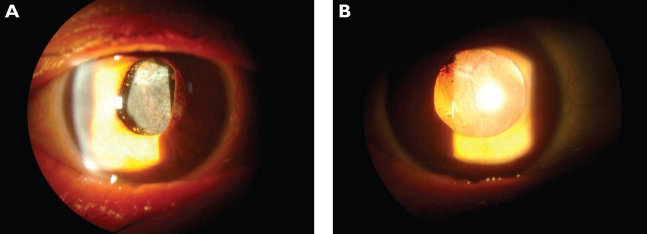
In the physical examination, the patient had visual acuity of count fingers in the right eye (OD) and 20/100 in the left eye (OS). There was a significant PCO, with severe neovascularization in the OD at the slit – lamp examination (Figure 1). We offered the patient an off-label treatment with intravitreal bevacizumab in the right eye. The patient agreed and signed an informed consent form.
Figure 1.
Right slit-lamp images showing PCO with severe neovascularization and granules of pigment over the IOL. A) Direct illumination. B) Retroillumination with mydriasis.
An intravitreal injection of 2.5 mg of bevacizumab was administered without complications. Five days after the treatment, there was a notorious decrease in the posterior capsule neovascularization. One month after, the neovascularization continued, we chose to give a second dose of intravitreal bevacizumab to our patient.
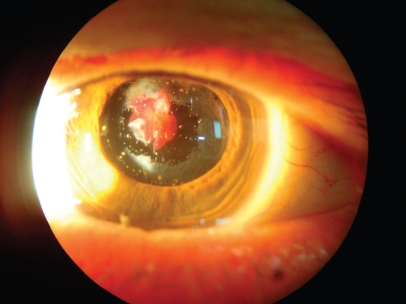
Two weeks after the second dose, there was no apparent neovascularization in the posterior capsule. We decided to perform a Nd:YAG capsulotomy. During the procedure, the patient had a small bleed (Figure 2), forming a clot that slowly disappeared 2 weeks after laser treatment.
Figure 2.
Slit-lamp image immediately after posterior capsulotomy. A small hemorrhage (clot) is seen behind the IOL.
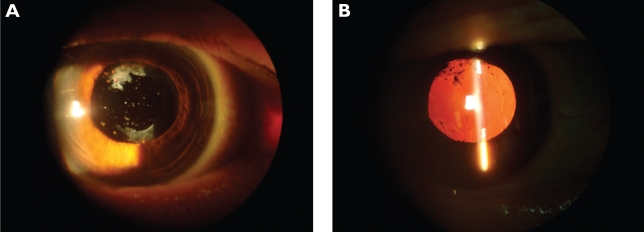
The final best corrected visual acuity in OD was 20/200 and 20/20 in OS with a clear visual axis (Figure 3). A persistent macular edema and active proliferative diabetic retinopathy was seen in the fluorescein angiography.
Figure 3.
Two months after treatment slit-lamp images. It shows a complete resolution of the clot and a clear visual axis. A) Direct illumination. B) Retroillumination.
Discussion
The incidence of PCO varies widely, depending on the cataract surgery technique, IOL material, edge design, history of intraocular inflammation, patient age, the presence of pseudoexfoliation before surgery, among others. Nevertheless, diabetes mellitus has been known historically, as a definitive risk factor (Schaumberg et al 1998; Edihara et al 2006). PCO in diabetic patients undoubtedly interferes with postoperative fundoscopy, retinal photocoagulation treatment and vitrectomy, so it is important to maintain a clear visual axis.
The progression of diabetic retinopathy stages after cataract surgery is a controversial issue. While some authors state that there is a definite progression, others state the opposite. They said that the progression seen after surgery is only the disease natural history (Murtha et al 2007).
The progression of diabetic retinopathy after cataract surgery includes the development of abnormal new vessels in the vitreous of untreated or insufficiently treated patients, macular edema, neovascular glaucoma and rubeosis iridis (Ivancic et al 2005). In this particular case, the neovascularization was so severe that reached and spread over the posterior capsule.
To our knowledge, there are only four reported cases in the literature of posterior capsule neovascularization after cataract surgery. Three of them had diabetic retinopathy. In the remaining case, the neovascularization was related to prior surgeries (pneumatic retinopexy and pars plana vitrectomy). The cases, until now reported, have been treated with vitrectomy and endophotocoagulation, intravitreal bevacizumab, and photodynamic therapy. There are no well defined treatments for this rare complication (Eifrig et al 1990; Ayata et al 2007; Eren et al 2007).
The other reported case, in which the patient was also treated with intravitreal bevacizumab, the detection of the new vessels behind the posterior capsule was done only one year after the surgery. The intravitreal dose was 1.25 mg and it required only one administration. One week after the treatment they performed a Nd:YAG capsulotomy with no complications. During the follow-up time of four weeks the patient did not present any complications (Eren et al 2007).
In our case, a single intravitreal injection of bevacizumab was not enough to induce an adequate regression of the posterior capsule neovascularization, so a second intravitreal injection was necessary to further decrease it and allow us to perform a Nd:YAG capsulotomy. During the procedure we had a small bleed, which slowly reduce until its complete disappearance, allowing a clear visual axis.
The follow-up time after the capsulotomy was two months. There were no complications in this time period. We consider that a longer follow-up time is needed to assure that there is no recurrence of new vessels in the remaining posterior capsule that can impair the visual acuity.
If the Nd:YAG capsulotomy would have been implemented without prior administration of the intravitreal bevacizumab, the vessels behind the posterior capsule would have been patent at the moment of the laser treatment. In this particular scenario, the risk of a major vitreous hemorrhage with the subsequent loss of vision and even an increase of the IOP is very high.
In summary, intravitreal bevacizumab was an effective and safe treatment that induces regression of posterior capsule neovascularization that allowed us to perform a Nd:YAG capsulotomy with minimal complications.
References
- Avery RL, Pearlman J, Pieramici DJ, et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology. 2006;113:1695–705. doi: 10.1016/j.ophtha.2006.05.064. [DOI] [PubMed] [Google Scholar]
- Ayata A, Unal M, Erşanli D, et al. Photodynamic therapy for posterior capsule neovascularization. J Cataract Refract Surg. 2007;33:1131–2. doi: 10.1016/j.jcrs.2007.02.025. [DOI] [PubMed] [Google Scholar]
- Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin) Ophthalmology. 2007;114:855–9. doi: 10.1016/j.ophtha.2007.01.017. [DOI] [PubMed] [Google Scholar]
- Chung J, Kim MY, Kim HS, et al. Effect of cataract surgery on the progression of diabetic retinopathy. J Cataract Refract Surg. 2002;28:626–30. doi: 10.1016/s0886-3350(01)01142-7. [DOI] [PubMed] [Google Scholar]
- Ebihara Y, Kato S, Oshika T, et al. Posterior capsule opacification after cataract surgery in patients with diabetes mellitus. J Cataract Refract Surg. 2006;32:1184–7. doi: 10.1016/j.jcrs.2006.01.100. [DOI] [PubMed] [Google Scholar]
- Eifrig DE, Hermsen V, McManus P, et al. Rubeosis capsulare. J Cataract Refract Surg. 1990;16:633–6. doi: 10.1016/s0886-3350(13)80783-3. [DOI] [PubMed] [Google Scholar]
- Eren E, Küçükerdönmez C, Yilmaz G, et al. Regression of neovascular posterior capsule vessels by intravitreal bevacizumab. J Cataract Refract Surg. 2007;33:1113–15. doi: 10.1016/j.jcrs.2007.01.040. [DOI] [PubMed] [Google Scholar]
- Hauser D, Katz H, Pokroy R, et al. Occurrence and progression of diabetic retinopathy after phacoemulsification cataract surgery. J Cataract Refract Surg. 2004;30:428–32. doi: 10.1016/S0886-3350(03)00579-0. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Hayashi H, Nakao F, et al. Posterior capsule opacification after cataract surgery in patients with diabetes mellitus. Am J Ophthalmol. 2002;134:10–16. doi: 10.1016/s0002-9394(02)01461-7. [DOI] [PubMed] [Google Scholar]
- Ivancic D, Mandic Z, Barac J, et al. Cataract surgery and postoperative complications in diabetic patients. Coll Antropol. 2005;29:55–8. [PubMed] [Google Scholar]
- Krupsky S, Zalish M, Oliver M, et al. Anterior segment complications in diabetic patients following extracapsular cataract extraction and posterior chamber intraocular lens implantation. Ophthalmic Surg. 1991;22:526–30. [PubMed] [Google Scholar]
- Murtha T, Cavallerano J. The management of diabetic eye disease in the setting of cataract surgery. Curr Opin Ophthalmol. 2007;18:13–18. doi: 10.1097/ICU.0b013e32801129fc. [DOI] [PubMed] [Google Scholar]
- Schaumberg DA, Dana MR, Christen WG, et al. A systematic overview of the incidence of posterior capsule opacification. Ophthalmology. 1998;105:1213–21. doi: 10.1016/S0161-6420(98)97023-3. [DOI] [PubMed] [Google Scholar]
- Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003;349:427–34. doi: 10.1056/NEJMoa021491. [DOI] [PMC free article] [PubMed] [Google Scholar]