Abstract
OBJECTIVE
To identify elements of data that have been shown to contribute to continuity of information between primary care providers and medical specialists providing care to adult asthma patients.
DESIGN
Systematic review of the literature followed by a 2-round modified Delphi consensus process.
SETTING
Province of Ontario.
PARTICIPANTS
Eight expert panelists, including 3 practising family physicians, a medical specialist knowledgeable in the treatment of asthma, a family physician previously involved in provincial initiatives related to primary care reform, an e-health technologist, a developer of evidence-based guidelines, and an operations and programs specialist.
METHODS
We completed a systematic literature review to identify important components of consultation reports. We then engaged an 8-member panel in a 2-round modified Delphi consensus process, which led to the identification of components deemed essential to good continuity of information.
MAIN FINDINGS
After 2 rounds, expert panelists reached consensus on 15 components, referred to here as minimum essential elements, of consultation reports generated by medical specialists in response to referring primary care providers’ consultation requests.
CONCLUSION
The expert panelists considered inclusion of the minimum essential elements in consultation reports essential to achieving good continuity of information. We assembled these elements in a suggested format for a consultation report. The format can be easily modified by practitioners caring for patients with other chronic diseases.
RÉSUMÉ
OBJECTIF
Identifier les éléments de données qui sont reconnus pour contribuer au suivi de l’information entre les soignants de première ligne et les spécialistes qui traitent des patients asthmatiques.
TYPE D’ÉTUDE
Revue systématique de la littérature, suivie d’un processus de consensus de type Delphi modifié en 2 rondes.
CONTEXTE
L’Ontario.
PARTICIPANTS
Huit panélistes experts, comprenant 3 médecins de famille actifs, un médecin spécialiste connaissant bien le traitement de l’asthme, un médecin de famille ayant déjà participé à des projets provinciaux en rapport avec la réforme des soins primaires, un technologiste de l’informatique de la santé, un responsable de directives fondées sur des données probantes et un spécialiste des opérations et programmes.
MÉTHODES
Nous avons fait une revue systématique de la littérature afin d’identifier les composantes importantes d’un rapport de consultation. Nous avons ensuite engagé un panel de 8 personnes dans un processus de consensus Delphi modifié en 2 rondes, ce qui a permis d’identifier certaines composantes jugées essentielles au bon suivi de l’information.
PRINCIPALES OBSERVATIONS
Après 2 rondes, les panélistes experts se sont entendus sur 15 composantes, qu’on désigne ici par le terme éléments essentiels minimaux, des rapports adressés par les spécialistes aux soignants de première ligne à la suite d’une demande de consultation.
CONCLUSION
Les panélistes experts étaient d’avis que pour assurer un suivi de l’information adéquat, les rapports de consultation devaient contenir un minimum d’éléments essentiels. Nous avons réuni ces éléments dans le format de rapport de consultation ici proposé. Ce format peut facilement être modifié selon les besoins des médecins qui traitent d’autres maladies chroniques.
Two of the most important challenges confronting primary care in the 21st century are improving coordination of patient care and mitigating the effects that increasing medical specialization has had on both coordination and continuity of care.1 Greater fragmentation of care—one consequence of increasing medical specialization—presents challenges to coordination and communication both for patients suffering from chronic diseases, such as asthma, diabetes, congestive heart failure, and depression, and for their care providers.2,3
Our focus in this article is coordination of care between primary care providers and specialists involved in treating adult asthma patients in Ontario. Asthma is among 4 ambulatory care–sensitive conditions, all chronic, that are associated with many hospitalizations deemed avoidable as long as patients have timely access to high-quality care in their communities. High-quality care includes disease prevention programs and appropriate primary health care.4 We contend that coordinating timely access to appropriate care is an outcome of high-quality decision making and that, in turn, the quality of decision making is profoundly affected by a concept referred to as informational continuity. Informational continuity means the use, transfer, and management of patient information. Good informational continuity is achieved with the accurate assimilation, timely transfer, and sharing of essential patient information among care providers, including relevant information on past events and patients’ personal circumstances.5
Here we focus on informational continuity pertinent to the consultation report—the medical specialist’s response to the referring provider. The consultation report is part of the referral-consultation process; its effectiveness depends upon timely and effective communication and a reciprocal exchange of relevant information between the referring physician and the specialist.6 Consultation reports should convey specialists’ assessments of patients’ current problems in response to referring providers’ questions. The consultation report generally focuses on next steps in the care of patients. In this case we specifically focus on continuity of information in the care of adult asthma patients.
While communicating relevant patient information in an effective and timely manner is clearly important, it is far from simple. A number of studies that evaluated communication between primary care practitioners and specialists highlighted substantial communication barriers, largely rooted in differing perspectives about information relevance and timeliness.7 Specialists, for example, include details they believe to be important, sometimes without fully addressing the referring physicians’ questions. Referring physicians, on the other hand, might dismiss information provided by specialists—some of it conceivably important for future care—and focus only on answers to their own specific questions.
This study addresses the communication barriers that arise at the interface between primary and specialty practitioners, focusing on the issue of information relevance. After we performed a systematic literature review to identify information components frequently used in the referral-consultation process, we asked an 8-member expert panel to establish the optimal content and format of a consultation report generated by medical specialists for primary care physicians to report on their adult asthma patients.
Methods
Systematic literature review
This paper reports on one aspect—consultation letters—of a larger study we undertook to look at a number of points of transfer of patient information among those providing care for adult asthma patients. We looked at referral letters, discharge summaries from hospitals and emergency departments, referrals to emergency departments, and reports generated by asthma education centres. We completed a systematic literature review of articles written in English and published between 1990 and 2005 that were identified through the following key words: shared care, communication between family physicians and specialists, referral patterns, information transfer, self care, discharge letters, specialists, referral and consultation letters, and letters. We searched for articles in Ovid MEDLINE, PubMed, ProQuest, and the Cochrane Database of Systematic Reviews.
Members of the research team, which included primary care practitioners and academic researchers, evaluated 111 articles. Each article was reviewed by 3 different team members; each group of 3 included either the principal investigator or the research coordinator, or both, and at least 1 practising primary care physician. A reviewer’s guide was developed by the team to review each article. The reviewer’s guide contained inclusion and exclusion criteria, including criteria related to article type, subjects or participants, setting, purpose, data sources, and theoretical frameworks (if any). The level of evidence used in each paper was ascertained and noted in the reviewer guide using a 6-level rubric applied and developed elsewhere.8,9
Of the 111 articles evaluated by the research team, 24 were selected. These were used to develop a list of 74 items or data elements related to patient information transfer in chronic care. These data elements spanned all of the points of transfer referred to above.
Identification of minimum essential elements
After completing the systematic review, we engaged an 8-member expert panel in a modified Delphi process to assess the importance of the 74 data elements. Our panelists were experts in the area of adult asthma care and included 3 practising family physicians, a medical specialist knowledgeable in the treatment of asthma, a family physician previously involved in provincial initiatives related to primary care reform, an expert in e-health technology, a specialist in reviews of operations and programs, and a developer of evidence-based practice guidelines relating to management of adult asthma.
The data elements were subjected to a 2-round Delphi consensus process. Materials for the first round were mailed to panelists in April 2005. Each package included a letter of instruction, an information booklet with a summary of the evidence for each element and related references, an answer booklet in which each item could be rated, and an addressed envelope with a return courier form.
Panelists were asked to rate each of the 74 data elements on the basis of its importance. They were asked how essential or necessary each item would be to ensuring high-quality patient information transfer and facilitating coordination of care between providers involved in managing adult asthma patients. Data elements were rated on a 9-point Likert scale, ranging from 1 (this item is not necessary at all) to 9 (this item is essential) with a midpoint of 5 (nice to have but not essential). Panelists were invited to provide their comments and suggestions for alternate wording, terminology, and item format and sequencing, and to add their own suggestions for new items.
Data from round 1 were entered into an Excel spreadsheet to facilitate consideration on the part of the research team. Materials for round 2 of the Delphi process were based on the ratings and related comments from round 1 and on discussions had by the research team members that focused on the panelists’ ratings and comments. In round 2, we asked the expert panelists to reconsider 49 data elements that had received only moderate consensus in round 1 and to consider 2 new items that were developed based on panelists’ feedback and on new research that came to our attention during the time between round 1 and round 2. Round 2 materials were mailed to the panelists in June 2005. They were very similar to the materials mailed to panelists in round 1, with the additional inclusion of a compilation of the panel’s ratings and comments from round 1.
The study protocol received ethics approval from the University of Toronto’s Ethics Review Committee.
Results
Evidence contained in the 24 articles reviewed was based mainly on observational studies or expert opinion. The systematic abstraction of data elements from these papers, combined with the subsequent Delphi process, allowed us to identify a set of essential elements that could be evaluated using more rigorous methods. Of the 74 original data elements, 25 achieved high consensus in round 1. In round 2, panelists rated 51 elements (2 new items and 49 original elements that had received only moderate consensus in round 1), and 29 of these achieved high consensus. Overall, 54 elements achieved high consensus; of these, 15 elements related specifically to the consultation report process between medical specialists and referring primary care providers. We refer to these 15 data elements, summarized in Table 1,6,7,9–18 as minimum essential elements.
Table 1.
Minimum essential elements for consultation letters
| MINIMUM ESSENTIAL ELEMENTS | LABEL IN FIGURE 1 | REASONS AND EXAMPLES |
|---|---|---|
| Patient’s (1) name, (2) date of birth, (3) contact information, and (4) OHIP number | Patient details | Identify patient, prevent medical errors, and ensure patient safety (Recommendation of expert panel) |
| Medical specialist’s (5) name and (6) contact information | Consultant details | Identify name and contact information of specific medical specialist who evaluated the patient10–12 |
| (7) Reason for the referral (as understood by the specialist) | Reason for referral as understood by specialist | State specific reason for referral, eg, “I saw Mr Jones, a 30-year-old man, for assessment after worsening of previously controlled asthma; also requested were medication recommendations and direct referral to CAE”13,14 |
| (8) Problem(s), as briefly identified by the referring physician or nurse practitioner | Specific problem(s) as identified by referring provider | Describe problem(s) that led to this referral, eg, “Healthy man with 10-y history of controlled asthma, recently experienced 2 emergency department visits in 10 d despite medication changes recommended by GP; patient is unable to control breathing and is using emergency inhaler daily; patient is unable to work owing to anxiety”6,11,13 |
| (9) Results of examination, tests, and procedures | Results of examination, tests, and procedures completed by specialist | Provide laboratory and investigation results for tests carried out by medical specialist; include results if available or identify if they are pending and, if so, how the referring provider can access them, eg, “Results March 22/07: CXR normal; PEF < 60%; routine bloodwork done here in my office within normal limits (copy of results included); no outstanding test results“6,15 |
| (10) Therapy proposed or initiated or the recommended treatment including all medications and their intended duration | All proposed treatments and medications | Itemize medication proposed or initiated by specialist; also identify medication discontinued by the specialist with reasons, eg, “Continue Ventolin 2 puffs QID; introduced LABA Serevent 2 puffs TID for 30 d until reassessed by specialist; continue using rescue breathing medication as per asthma action plan instructions”7,13,16,17 |
| (11) Problem(s), including answer(s) to specific question(s) posed by the referring provider | Answer(s) to specific question(s) posed by the referring provider | Eg, “Patient had not been taking routine Ventolin since March/07 and had recently started smoking again, both of which led to the recent exacerbation of symptoms”11 |
| (12) Primary or secondary diagnosis or problem | Primary and secondary diagnosis | Eg, “Exacerbation of controlled asthma” (Recommendation of expert panel) |
| (13) Plan of action developed for the patient OR management regimen (treatments or therapies proposed including medications) AND details regarding the specific verbal instructions or educational materials supplied to the patient | Signifies development of a plan of action for patient AND instructions and advice given to patient | Eg, “Provided patient a signed copy of asthma action plan, including clear instructions to take medication as prescribed, list of asthma medications, specific directions for medication changes when experiencing asthma symptoms, referral to CAE”7,18 |
| (14) Follow-up plan that specifies who is to do what and when. An important aspect is specifying who has been designated as responsible for the recommended actions (ie, patient, primary care provider, specialist, CAE, or another health care provider) | Follow-up plan recommended by specialist | Indicate follow-up arrangements booked or planned by the specialist’s office, eg, “Recheck appointment and repeat PFT to be done within 1 mo on or before May 1/07 at my office … appointment to be booked by patient” or “Appointment for initial assessment by CAE is to be booked for same day as specialist recheck appointment”11,16,18 |
| (15) Date prepared | Date prepared | Provide the date the consultation report was prepared (Recommendation of expert panel)12 |
CAE clinical asthma educator, CXR—chest x-ray, LABA—long-acting β2-agonist, OHIP—Ontario Health Insurance Plan, PEF—peak expiratory flow, PFT—peak flow test, QID—4 times daily, TID—3 times daily.
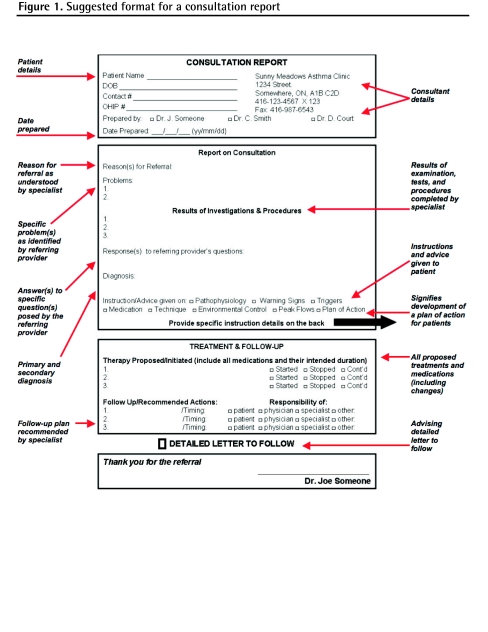
These elements now needed to be evaluated in clinical settings for their effect on continuity of patient information. To this end, and upon further consultation with our panelists and project team members, we assembled the minimum essential elements into a suggested format for a consultation report (Figure 1).*
Figure 1.
Suggested format for a consultation report
Discussion
In qualitative comments collected as part of the Delphi process, our panelists observed that omission of minimum essential elements inevitably leads to delays in care provision and to excessive expenditures of time and effort on the part of patients and their care providers as critical missing information is sought and retrieved. These omissions represent real barriers to informational continuity and to coordination of care, as they divert resources and cause delays in treatment. Barriers to continuity of information can be mitigated by providing the minimum essential elements in a logical format, like that we present in Figure 1.
A few empiric studies provide support for the use of standardized methods of transferring patient information. For example, in 1 study the inclusion of specific items in consultation letters increased recipient satisfaction; while the process by which these items were identified was not as rigorous as the one used in this study, the items are similar.10 We focus on the relevance of information here, but another study underscored the importance of timely communication to continuity of information and care and the advantages of standardized templates containing essential data elements, such as the one developed in this study.19 The consultation report could be used to convey time-critical patient information to primary care physicians.16 A 1-page report format such as that we present in Figure 1—which contains the time-critical, patient information upon which primary care providers can base their immediate care decisions—might be completed at the conclusion of the visit and faxed immediately to the referring physician. If necessary, the report could be followed by a more detailed consultation letter offering more specific details on results of investigations and procedures, and the recommendations related to treatment and follow-up; we have incorporated a check-box option in our sample consultation report to indicate if more information is to follow.
The work summarized here requires further study in clinical settings to assess the potential for the elements, whether in a standardized template like ours or an alternative presentation like those developed by others, to substantially improve communication and patient information transfer between medical specialists and primary care practitioners.10,16
Limitations
The minimum essential elements we identified as part of this study were derived from literature that focused exclusively on transfer of patient information relating to the care of adult asthma patients. While some of the data elements identified for the consultation report would likely be useful or valuable in reports relating to other conditions, several elements are clearly specific to the particular chronic disease we examined.
We used a modified Delphi consensus process in this study, an accepted approach in health care and elsewhere when the opinions of experts are used to facilitate policy development and prioritization.20–22 Despite careful attention in the selection of our expert panel, and our adherence to a rigorous modified Delphi consensus process, there are limitations to this method of achieving consensus with experts, as the opinions of experts are the only opinions being solicited and considered. While the use of a consensus approach served to achieve our goal of prioritizing among large numbers of potential data elements, the results of the consensus process do not replace a detailed quantitative analysis of the merits of our essential data elements in contributing good continuity of information; future studies should focus on testing these elements in clinical situations.
Conclusion
Medical specialists and primary care providers have different perspectives with respect to the relevance of information and what constitutes timeliness. Recent work cited here, as well as this study, suggests that continuity of information and care can be improved with the use of standardized communication tools containing minimum essential elements. Further improvements to continuity of information might be realized if the tool is part of a real-time reporting protocol, possibly included in an electronic medical record.16 A few comments offered informally by our panelists highlighted the facilitating effects that an electronic patient information context would have on the provision of both minimum essential elements and on the feasibility of providing more detailed additional patient treatment and follow-up information. In the event a paper-based system is used, the consultation report might appear on 1 side of a sheet, while a referral form, similar to one suggested in an earlier article, might appear on the reverse side.23
This paper describes one aspect of a larger study that examined patient information transfer between those providing care for adult asthma patients in Ontario and included information transferred among primary care practitioners, medical specialists, asthma educators, emergency department physicians, and providers of care in hospitals. In the larger study, in addition to information content, we examined other aspects of informational continuity including format (standardized or structured versus unstructured transfer mechanisms), mode (electronic, facsimile, and mail), and organizational context (in which we identified contextual factors that affect the accessibility, accuracy, completeness, and timeliness of information).
Acknowledgments
This study was funded through the Ontario Ministry of Health and Long-Term Care’s Primary Health Care Transition Fund.
EDITOR’S KEY POINTS
Improving the coordination of patient care and dealing with the effects of increasing medical specialization on continuity of care are 2 important challenges for family physicians.
Coordination of care between providers for complex, chronic conditions like asthma, diabetes, and heart failure can be improved by ensuring good continuity of information between family physicians and other specialists.
Using an expert panel, which included family physicians, and a consensus process, the authors identified the minimum essential elements for consultation reports generated by specialists in response to referrals from family physicians for patients with asthma.
A sample consultation report, which can be modified and used for other chronic conditions, was generated.
POINTS DE REPÈRE DU RÉDACTEUR
Améliorer la coordination des soins et s’adapter à une super-spécialisation médicale dans la continuité des soins représentent 2 défis importants pour le médecin de famille.
La coordination des soins entre ceux qui soignent des maladies chroniques complexes comme l’asthme, le diabète et l’insuffisance cardiaque peut être améliorée en s’assurant d’un bon suivi de l’information entre médecins de famille et spécialistes.
Avec l’aide d’un panel d’experts qui comprenait des médecins de famille et utilisait un processus de consensus, les auteurs ont identifié les éléments essentiels minimaux devant faire partie du rapport de consultation qu’un spécialiste adresse au médecin de famille qui lui a dirigé un patient asthmatique.
On propose ici un rapport de consultation type qui peut être adapté à d’autres maladies chroniques.
Footnotes
*Full text is available in English at www.cfp.ca.
*A blank version of the consultation report created based on the results of this study is available at www.cfp.ca. Go to the full text of this article on-line, then click on CFPlus in the menu at the top right-hand side of the page.
Contributors
Dr Berta contributed to the original conception and design of the study, completion of the original literature review, and development of the research questions used in the funding proposal; helped coordinate and participated in the systematic literature review; helped coordinate the Delphi consensus process; developed the original draft of and revised the article; and approved the final article for submission. Dr Barnsley contributed to the original conception of the study and the development of the funding proposal; participated in the systematic literature review; contributed to interpretation of data, development of indicators, and revisions of the article drafts; and approved the final article for submission. Drs Bloom, Cockerill, Davis, Jaakkimainen, Talbot, and Vayda contributed to the original conception of the study; participated in the systematic literature review; contributed to the interpretation of data, development of indicators, and revisions of the article drafts; and approved the final article for submission. Ms Mior contributed to the original conception and reconception of the study; helped coordinate and participated in the systematic literature review; helped coordinate the Delphi consensus process; contributed to interpretation of data, development of indicators, and revisions of the article drafts; and approved the final article for submission.
Competing interests
None declared
This article has been peer reviewed.
References
- 1.Ontario College of Family Physicians. Family medicine in the 21st century: a prescription for excellent healthcare. Toronto, ON: Ontario College of Family Physicians; 1999. . Available from: www.ocfp.on.ca/English/OCFP/Communications/Publications/default.asp?s=1. Accessed 2009 Apr 15. [Google Scholar]
- 2.Romanow R, Commission on the Future of Health Care in Canada . Building on values: the future of health care in Canada—final report. Ottawa, ON: Health Canada; 2002. . Available from: www.hc-sc.gc.ca/hcs-sss/hhr-rhs/strateg/romanow-eng.php. Accessed 2002 Dec 1. [Google Scholar]
- 3.Hellesø R, Lorensen M, Sorensen L. Challenging the information gap—the patient’s transfer from hospital to home health care. Int J Med Inform. 2004;73(7–8):569–80. doi: 10.1016/j.ijmedinf.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Canada. Canadian Institute for Health Information . Health care in Canada, 2003. Ottawa, ON: Canadian Institute for Health Information; 2003. Available from: www.icis.ca/cihiweb/dispPage.jsp?cw_page=AR_43_E. Accessed 2003 Jun 27. [Google Scholar]
- 5.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dojeiji S, Marks M, Keely E. Referral and consultation letters: enhancing communications between family physicians and specialists. Clin Invest Med. 1997;20(Suppl 4):S49. [Google Scholar]
- 7.Babington S, Wynne C, Atkinson CH, Hickey BE, Abdelaal AS. Oncology service correspondence: do we communicate? Australas Radiol. 2003;47(1):50–4. doi: 10.1046/j.1440-1673.2003.01129.x. [DOI] [PubMed] [Google Scholar]
- 8.Barnsley J, Berta W, Cockerill R, MacPhail J, Vayda E. Identifying performance indicators for primary care practices. Assessing levels of consensus. Can Fam Physician. 2005;51:700–1. . Available from: www.cfp.ca/cgi/reprint/51/5/700. Accessed 2009 Apr 9. [PMC free article] [PubMed] [Google Scholar]
- 9.D’Agostino RB, Kwan H. Measuring effectiveness. What to expect without a randomized control group. Med Care. 1995;33(4 Suppl):AS95–105. [PubMed] [Google Scholar]
- 10.Tattersall MH, Butow PN, Brown JE, Thompson JF. Improving doctors’ letters. Med J Aust. 2002;177(9):516–20. doi: 10.5694/j.1326-5377.2002.tb04926.x. [DOI] [PubMed] [Google Scholar]
- 11.Campbell B, Vanslembroek K, Whitehead E, van de Wauwer C, Eifell R, Wyatt M, et al. Views of doctors on clinical correspondence: questionnaire survey and audit of content of letters. BMJ. 2004;328(7447):1060–1. doi: 10.1136/bmj.38058.801968.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.College of Physicians and Surgeons of Alberta . The referral/consultation process. Edmonton, AB: College of Physicians and Surgeons of Alberta; 2003. Available from: http://uat-cpsa.softworksgroup.com/Libraries/Policies_and_Guidelines/The_Referral_Consultation_Process.sflb.ashx. Accessed 2009 Apr 20. [Google Scholar]
- 13.Ghandi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15(9):626–31. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodge JA, Jacob A, Ford MJ, Munro JF. Medical clinic referral letters. Do they say what they mean? Do they mean what they say? Scott Med J. 1992;37(6):179–80. doi: 10.1177/003693309203700606. [DOI] [PubMed] [Google Scholar]
- 15.Dupont C. Quality of referral letters. Lancet. 2002;359(9318):1701. doi: 10.1016/S0140-6736(02)08583-5. [DOI] [PubMed] [Google Scholar]
- 16.Scott IA, Mitchell CA, Logan E. Audit of consultant physicians’ reply letters for referrals to clinics in a tertiary teaching hospital. Intern Med J. 2004;34(1–2):31–7. doi: 10.1111/j.1444-0903.2004.00424.x. [DOI] [PubMed] [Google Scholar]
- 17.Ng WT, Caslake R, Counsell CE. Non-completion of changes to prescribed medications in people with Parkinson disease. Age Ageing. 2007;36(3):333–6. doi: 10.1093/ageing/afl175. Epub 2007 Jan 31. [DOI] [PubMed] [Google Scholar]
- 18.Koopman RJ, May KM. Specialist management and coordination of “out-of-domain care. Fam Med. 2004;36(1):46–50. [PubMed] [Google Scholar]
- 19.Farquhar MC, Barclay SI, Earl H, Grande GE, Emery J, Crawford RA. Barriers to effective communication across the primary/secondary interface: examples from the ovarian cancer patient journey (a qualitative study) Eur J Cancer Care (Engl) 2005;14(4):359–66. doi: 10.1111/j.1365-2354.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- 20.Shiffman RN, Shekelle P, Overhage JM, Slutsky J, Grimshaw J, Deshpande AM. Standardized reporting of clinical practice guidelines: a proposal from the conference on guideline standardization. Ann Intern Med. 2003;139(6):493–8. doi: 10.7326/0003-4819-139-6-200309160-00013. [DOI] [PubMed] [Google Scholar]
- 21.Kahan JP, Bernstein SJ, Leape LL, Hilborne LH, Park RE, Parker L, et al. Measuring the necessity of medical procedures. Med Care. 1994;32(4):357–65. doi: 10.1097/00005650-199404000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Lavis JN, Anderson GM. Appropriateness in health care delivery: definitions, measurement and policy implications. CMAJ. 1996;154(3):321–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Berta W, Barnsley J, Bloom J, Cockerill R, Davis D, Jaakkimainen L, et al. Enhancing continuity of information. Essential components of a referral document. Can Fam Physician. 2008;54:1432–3.e1–6. [PMC free article] [PubMed] [Google Scholar]