Abstract
We report a sebaceous carcinoma confined to the corneoscleral limbus without involvement of the eyelid. A 60-year-old man, who showed multiple masses on the corneaoscleral limbus and limbal ulceration but with normal eyelids, underwent surgical en-bloc excision of the masses. Histopathologic examination revealed a sebaceous carcinoma. Three weeks after excision, multiple pagetoid recurrences were found along the bulbar conjunctiva 2 mm away from the limbus. After the application of topical mitomycin C, the pagetoid spread regressed completely. After a 2 year follow-up, no other local or systemic recurrences were observed. This report shows that the ulcerative mass which is confined to only the corneoscleral limbus may be a sebaceous carcinoma even without eyelid involvement. Topical mitomycin C may be effective for treating pagetoid spread of sebaceous carcinoma of limbal origin.
Keywords: Sebaceous carcinoma, Limbus, Conjunctiva, Pagetoid recurrence, Mitomycin C
Sebaceous carcinoma is a rare but important eyelid tumor.1-4 Sebaceous carcinoma originates from cells that comprise sebaceous glands.1-3 There is an abundance of sebaceous glands in the ocular region, particularly in the tarsus (meibomian glands) and in association with the cilia (Zeis glands).1 Hence, sebaceous carcinoma commonly arises from the meibomian gland of the tarsus, the glands of Zeis, and the sebaceous glands of caruncle.1,4-6 Sebaceous carcinoma confined to the bulbar conjunctiva without involvement of other periocular tissues is very rare, and only a few such cases have so far been reported.1,7-9
Herein, we report a patient who showed sebaceous carcinoma confined just to the corneaoscleral limbus without lid involvement, suggesting a primary limbal origin. Pagetoid recurrence, which occurred after en-bloc excision of the mass, completely regressed on topical application of mitomycin C.
Case Report
This 60-year-old man had been complaining of persistent conjunctival and limbal injection of the left eye for 3 months prior to being seen by us. The patient felt no pain and had no previous ocular or medical history except for hypertension and was being followed by his cardiologist. He had no family history of malignancy. He had been treated with topical steroid for 2 months with the impression of scleritis before referral. When he was referred to our clinic, the best-corrected visual acuity (BCVA) was 20/20 in the right eye and 20/30 in the left eye. Intraocular pressure (IOP) values were normal bilaterally. Slit-lamp examination revealed diffuse conjunctival injection and multiple nodular masses which were confined to inferior limbus and inferior bulbar conjunctiva along the limbus. The masses showed salmon-colored pebbly appearance with abundant vascularization, and peripheral corneal ulceration presented along with the masses (Fig. 1). There was no other involvement in the perioribital area, including palpebral conjunctiva, tarsus, lid and eyebrow of the left eye. Anterior chambers were clear, and fundus findings were normal. We tentatively diagnosed the conjunctival masses as squamous cell carcinoma and recommended en-bloc excisional biopsy of the lesions.
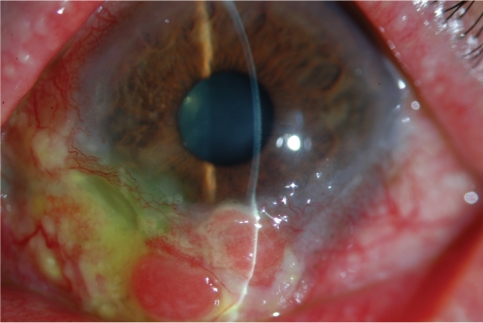
Fig. 1.
Slit-lamp examination showed diffuse conjunctival injection and multiple nodular masses confined to inferior limbus and inferior bulbar conjunctiva along the limbus. The masses showed salmon-colored pebbly appearance accompanying peripheral corneal ulceration.
He underwent en-bloc excision of masses with no touch and dry technique, cryotherapy with double freeze-thaw technique and permanent amniotic membrane transplantation.
Histologically, the mass was located beneath the conjunctival epithelium and showed infiltrative growth pattern. No capsulation around the mass was noted. The tumor cells were arranged in a lobular pattern (Fig. 2A). Some tumor cells nests showed comedo-type necrosis in the center of the nest (Fig. 2B). Tumor cells were composed of two kinds of cells; less differentiated cells and lipid-producing cells (Fig. 2C). The former were situated peripherally, whereas the latter were located centrally. Mitotic activity was frequently seen, and mitotic cell count ranged from three to five per 10 high-power fields. The diagnosis was sebaceous carcinoma. Systemic evaluation showed no evidence of metastasis in head and neck computed tomography, including parotid gland and bone scan. Three weeks later, we found multiple pagetoid spread along the bulbar conjunctiva 2 mm away from the limbus (Fig. 3) with conjunctival injection. There were no other tarsalor lid lesions on meticulous examination. We started topical application of 0.04% mitomycin C (MMC) four times a day. Six cycles were given to the patient, each cycle consisting of 1 week of topical application of 0.04% MMC and 1 week-off therapy to prevent epithelial toxicity. At the end of the second cycle, all of the pagetoid recurrences disappeared. At the end of sixth cycle, clear conjunctiva and cornea were observed after the sebaceous carcinoma regressed completely without corneal epithelial decompensation (Fig. 4). Other orbital and periorbital tissues were normal. The BCVA were 20/20 in the both eyes. Two years after excision of tumor together with topical mitomycin application, the patient remains disease-free.
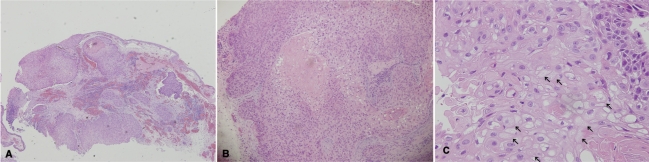
Fig. 2.
Light microscopic view of the tumor. (A) At low magnification, the tumor is composed of relatively well-delineated lobules of sebaceous cells (×40). (B) At medium magnification, the tumor cell nest shows comedo-type necrosis (×100). (C) At higher magnification, the large cells with sebaceous differentiation, some of which are vacuolated, have small nuclei and clear cytoplasm (×200).
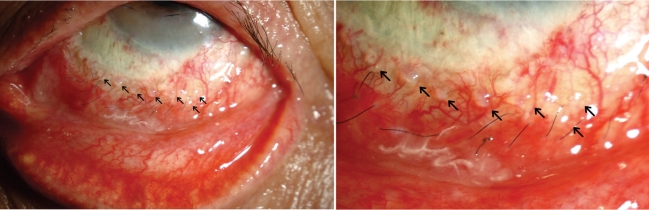
Fig. 3.
Slit lamp examination revealed multiple pagetoid spread along with bulbar conjunctiva 2 mm away from the limbus (arrows).
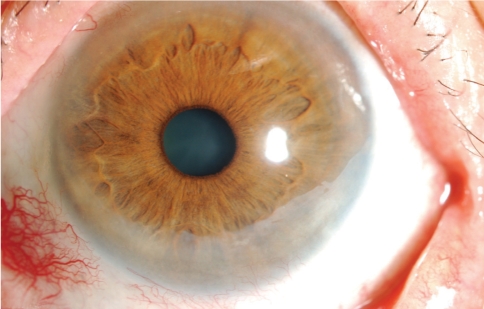
Fig. 4.
This photo shows clear conjunctiva and cornea after sebaceous carcinoma regressed completely.
Discussion
Sebaceous carcinoma is known as a neoplasm of the eyelid. In addition, it is notorious for masquerading common benign condition such as chronic blepharitis.10 Furthermore, sebaceous carcinoma of conjunctiva without underlying mass is extremely rare, therefore it is very difficult to diagnose the sebaceous carcimoma of conjunctiva early, and it is often misdiagnosed as other tumorous condition. There are only few reported cases of conjunctival intraepithelial sebaceous carcinoma. Honavar and associates reported 1 case of a 33-year-old woman who underwent excision of tumor, and the specimen showed that sebaceous carcinoma was confined to the palpebral conjunctiva without deep involvement of meibomian glands or Zeis glands.7 Margo and Grossniklaus reported 2 cases of a 58-year-old woman and a 71-year-old man whose exenteration specimens showed intraepithelial sebaceous carcinoma involving the tarsal and bulbar conjunctiva. There was no other involvement of sebaceous carcinoma in the specimen.8 Our present case was particular in several respects. The patient appealed to the injection of conjunctiva at first, and he was misdiagnosed as scleritis and was mishandled with topical corticostreroid for 2 months before referral. Immunosuppression might have contributed to the progression of tumor.7,11,12 As a matter of fact, the sebaceous carcinoma was confined to the limbus and the near bulbar conjunctiva. To our best knowledge, there has been no report about primary sebaceous carcinoma which is confined to the corneoscleral limbus without any underlying lesion, suggesting a limbal origin. It suggests that limbal epithelial stem cells may have a pleuripotential power which can differentiate not only into squamous epithelial cells but also into sebaceous cells.
Gross finding about peripheral corneal ulceration of our case corresponds with the characteristics of basal cell carcinoma or sebaceous carcinoma which finding was previously reported.13 However, limbal location suggests that it would be likely to be squamous cell carcinoma. Hence, the present case should be differentiated from other types of carcinoma such as basal cell carcinoma, squamous cell carcinoma, and clear cell carcinoma that is a rare varinant of squamous cell carcinoma of the skin and can simulates sebaceous carcinoma.14-16 Sebaceous carcinoma is an unencapsulated infiltrating mass, and tumor cells of sebaceous carcinoma has lipid globules within the finely vacuolated, frothy cytoplasm.1 Furthermore growth pattern of sebaceous carcinoma like lobular pattern, comedocarcinoma pattern, and papillary pattren can be of assistance to differentiate from other tumors.1 In contrast to sebaceous carcinoma, however, squamous cell carcinoma is generally better differentiated, has more abundant eosinophilic cytoplasm without lipid vacuoles, and may show squamous eddy formation and keratin cysts.1 Clear cell carcinoma has 'bubbled' cytoplasm that is due to hydropic change rather than the accumulation of lipid.14 Frozen section with oil red O stain helps to differentiate clear cell carcinoma from sebaceous carcinoma. In case of basal cell carcinoma, tumor lobules typically show peripheral palisading of nuclei and retraction artifact, findings that are not seen with this sebaceous carcinoma.
The optimal management of sebaceous carcinoma remains controversial.1,7 Generally, the first step is to establish the diagnosis and determine the extent of the disease. And if the lesion is small and circumscribed, complete excision is recommended.1 Currently, cryotherapy is routinely used as a supplemental treatment after excision.1,17 Topical chemotherapy has been used effectively in sebaceous carcinoma with pagetoid invasion and also broadly in other ocular surface neoplasm.1,4,18-20 Based on these studies, we completely excised the tumor and administered cryotherapy by double freeze-thaw technique. After local recurrence with pagetoid appearance, we applied mitomycin C topically. Mitomycin C is a non-cell cycle specific alkylating agent which inhibits cell proliferation, and has successfully been used in the treatment of conjuntival-corneal intraepithelial neoplasia.4,18,20,21 As far as we are aware of, there are only 3 reports that used mitomycin C in the treatment of sebaceous carcinoma.4,21,22 Similarly, pagetoid recurrence of sebaceous carcinoma of the corneaoscleral limbus in our present case was also effectively regressed with topical mitomycin C.
Our study has a limitation that lids or tarsus which appeared to be normal on slit lamp examination had not histopathologically been proven by map biopsies. Because our initial tentative diagnosis was squamous cell carcinoma, we didn't take map biopsies during excisional biopsy. In addition, the pagetoid recurrence near the limbus was well controlled within 3 weaks by topical mitomycin C, and no other suspicious lesion was detected at that time. Hence, re-excision with map biopsies was not considered. Nevertheless, we believe that there was no other lesion existed, because of grossly normal appearances of other areas on assiduous slit lamp examination and no additional recurrence of any other location in 2 year-follow up.
In conclusion, we report a patient with primary sebaceous carcinoma confined to the corneaoscleral limbus, suggesting limbal origin. When patients visit clinic with masses of limbal conjunctiva, the sebaceous carcinoma should be considered as a differential diagnosis. If local pagetoid recurrence of sebaceous carcinoma of limbal origin is detected, topical mitomycin C can be considered as a primary choice of treatment.
Footnotes
The concept of this paper was reported at the 96th meeting of the Korean Ophthalmological Society, October, 2006.
References
- 1.Shields JA, Demirci H, Marr BP, et al. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005;50:103–122. doi: 10.1016/j.survophthal.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Burns SJ, Foss AJ, Butler TK. Outcome of periocular sebaceous gland carcinoma. Ophthal Plast Reconstr Surg. 2005;21:353–355. doi: 10.1097/01.iop.0000176273.32152.70. [DOI] [PubMed] [Google Scholar]
- 3.Boniuk M, Zimmerman LE. Sebaceous carcinoma of the eyelid, eyebrow, caruncle and orbit. Int Ophthalmol Clin. 1972;12:225–257. [PubMed] [Google Scholar]
- 4.Tumuluri K, Kourt G, Martin P. Mitomycin C in sebaceous gland carcinoma with pagetoid spread. Br J Ophthalmol. 2004;88:718–719. doi: 10.1136/bjo.2003.034215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jakobiec FA. Sebaceous tumors of the ocular adnexa. Principles and Practice of Ophthalmology. 1994;3:1745–1770. [Google Scholar]
- 6.Cook BE, Bartley GB. Treatment options and future prospects for the management of eyelid malignancies An evidence-based update. Ophthalmology. 2001;108:2088–2098. doi: 10.1016/s0161-6420(01)00796-5. [DOI] [PubMed] [Google Scholar]
- 7.Honavar SG, Shields CL, Maus M, et al. Primary intraepithelial sebaceous gland carcinoma of the palpebral conjunctiva. Arch Ophthalmol. 2001;119:764–767. doi: 10.1001/archopht.119.5.764. [DOI] [PubMed] [Google Scholar]
- 8.Margo CE, Grossniklaus HE. Intraepithelial sebaceous neoplasia without underlying invasive carcinoma. Surv Ophthalmol. 1995;39:293–301. doi: 10.1016/s0039-6257(05)80106-7. [DOI] [PubMed] [Google Scholar]
- 9.Margo CE, Lessner A, Stern GA. Intraepithelial sebaceous carcinoma of the conjunctiva and skin of the eyelid. Ophthalmology. 1992;99:227–231. doi: 10.1016/s0161-6420(92)31988-8. [DOI] [PubMed] [Google Scholar]
- 10.Theodore FH. Conjunctival carcinoma masquerading as chronic conjunctivitis. Eye Ear Nose Throat Mon. 1967;46:1419–1420. [PubMed] [Google Scholar]
- 11.Penn I. Tumors after renal and cardiac transplantation. Hematol Oncol Clin North Am. 1993;7:431–445. [PubMed] [Google Scholar]
- 12.Singh SK, Gupta AK, Jha V, et al. Treatment of oropharyngeal cancer in renal transplant recipients without cessation of immunosuppressive therapy. Transplant Proc. 2006;38:2088–2089. doi: 10.1016/j.transproceed.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Sainz de la Maza M, Foster CS. Peripheral ulcerative keratitis and malignancies. Cornea. 1994;13:364–367. doi: 10.1097/00003226-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Kuo T. Clear cell carcinoma of the skin. A variant of the squamous cell carcinoma that simulates sebaceous carcinoma. Am J Surg Pathol. 1980;4:573–583. doi: 10.1097/00000478-198012000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Suster S. Clear cell tumors of the skin. Semin Diagn Pathol. 1996;13:40–59. [PubMed] [Google Scholar]
- 16.Margo CE, Groden LR. Primary clear cell carcinoma of the conjunctiva. Arch Ophthalmol. 2008;126:436–438. doi: 10.1001/archopht.126.3.436. [DOI] [PubMed] [Google Scholar]
- 17.Kass LG. Role of cryotherapy in treating sebaceous carcinoma of the eyelid. Ophthalmology. 1990;97:2–4. doi: 10.1016/s0161-6420(90)32633-7. [DOI] [PubMed] [Google Scholar]
- 18.Poothullil AM, Colby KA. Topical medical therapies for ocular surface tumors. Semin Ophthalmol. 2006;21:161–169. doi: 10.1080/08820530500351694. [DOI] [PubMed] [Google Scholar]
- 19.Shields CL, Naseripour M, Shields JA, Eagle RC., Jr Topical mitomycin-C for pagetoid invasion of the conjunctiva by eyelid sebaceous gland carcinoma. Ophthalmology. 2002;109:2129–2133. doi: 10.1016/s0161-6420(02)01239-3. [DOI] [PubMed] [Google Scholar]
- 20.Chalasani R, Giblin M, Conway RM. Role of topical chemotherapy for primary acquired melanosis and malignant melanoma of the conjunctiva and cornea: review of the evidence and recommendations for treatment. Clin Experiment Ophthalmol. 2006;34:708–714. doi: 10.1111/j.1442-9071.2006.01356.x. [DOI] [PubMed] [Google Scholar]
- 21.Frucht-Pery J, Sugar J, Baum J, et al. Mitomycin C treatment for conjunctival-corneal intraepithelial neoplasia: a multicenter experience. Ophthalmology. 1997;104:2085–2093. doi: 10.1016/s0161-6420(97)30055-4. [DOI] [PubMed] [Google Scholar]
- 22.Khong JJ, Muecke J. Complications of mitomycin C therapy in 100 eyes with ocular surface neoplasia. Br J Ophthalmol. 2006;90:819–822. doi: 10.1136/bjo.2005.086850. [DOI] [PMC free article] [PubMed] [Google Scholar]