Abstract
Purpose
To investigate changes in dry eye symptoms and diagnostic test values after cataract surgery and to address factors that might influence those symptoms and test results.
Methods
Twenty-eight eyes from 14 patients with preoperative dry eye (dry eye group) and 70 eyes from 35 patients without preoperative dry eye (non-dry eye group) were studied prospectively. In each group, we measured values such as tear break-up time (tBUT), Schirmer I test (ST-I), tear meniscus height (TMH), and subjective dry eye symptoms (Sx), and evaluated the postoperative changes in these values. We also evaluated the influence of corneal incision location and shape on these values. The correlations between these values and microscopic light exposure time and phacoemulsification energy were investigated.
Results
In the dry eye group, there were significant aggravations in Sx at 2 months postoperatively and in TMH at 3 days, 10 days, 1 month, and 2 months postoperatively, compared with preoperative values. All dry eye test values were significantly worse after cataract surgery in the non-dry eye group. With regard to incision location, there was no difference in tBUT, Sx, ST-I, or TMH in either the dry eye group or the non-dry eye group at any postoperative time point. Regarding incision shape, there was no difference in tBUT, Sx, ST-I or TMH at any postoperative time point in the dry eye group. In the superior incision sub-group of the non-dry eye group, tBUT and Sx were worse in the grooved incision group at day 1. In the temporal incision sub-group of the non-dry eye group, Sx were worse in the grooved incision group at 1 day, 3 days, and 10 days postoperatively. In both groups, significant correlations were noted between microscopic light exposure time and dry eye test values, but no correlation was noted between phacoemulsification energy and dry eye test values.
Conclusions
Cataract surgery may lead to dry eye. A grooved incision can aggravate the symptoms during the early postoperative period in patients without dry eye preoperatively. Long microscopic light exposure times can have an adverse effect on dry eye test values.
Keywords: Cataract surgery, Dry eye
Dry eye-associated symptoms, such as foreign body sensation and fatigue, frequently occur after cataract surgery.1-6 Affected patients may experience red or watery eyes along with constant foreign body sensation.3 Several published studies have documented the aggravation of dry eye symptoms and signs after LASIK and PRK.5,6 Some studies have even reported aggravation of dry eye symptoms and signs after cataract surgery.3,4 However, the follow-up of dry eye symptoms after cataract surgery and analysis of correlating risk factors has not been undertaken. We studied changes in dry eye symptoms (Sx) and diagnostic test values such as tear break-up time (tBUT), Schirmer I test (ST-I) and tear meniscus height (TMH) after cataract surgery, and sought to determine the intraoperative factors that might affect these symptoms and test results.
Materials and Methods
This prospective study was approved by the Institutional Review Board. A total of 98 eyes from 49 patients with bilateral cataracts were included in this study. Exclusion criteria were: pre-existing ocular disease such as glaucoma or uveitis, disorders of the lid or nasolacrimal pathway, and previous ocular surgery. We excluded the data of patients who were current smokers. Patients who had ocular allergies, pterygia, or blepharitis were also excluded because those factors could have an influence on the dry eye test results.7-9 We compared the test values between the right and left eyes of each patient to account for individual differences. Preoperatively, we divided patients into four operative method groups as follows (Table 1): bilateral superior incisions with grooved incision of the right eye and single plane incision of the left eye; bilateral temporal incisions with grooved incision of the right eye and single plane incision of the left eye; bilateral grooved incisions with temporal incision of the right eye and superior incision of the left eye; bilateral single plane incisions with temporal incision of the right eye and superior incision of the left eye. We constructed these groups so we could compare the effect of incision location without the effect of incision shape and compare the effect of incision shape without the effect of incision location. The time interval between operation on the right eye and on the left eye was 1 day.
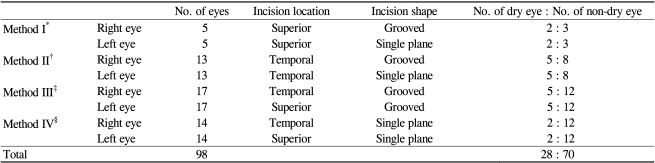
Table 1.
Preoperative classification of 4 operative method groups
*bilateral superior incisions with grooved incision of the right eye and single plane incision of the left eye; †bilateral temporal incisions with grooved incision of the right eye and single plane incision of the left eye; ‡bilateral grooved incisions with temporal incision of the right eye and superior incision of the left eye; §bilateral single plane incisions with temporal incision of the right eye and superior incision of the left eye.
Clinical Data Collection
We measured the TMH, ST-I and tBUT in that order preoperatively and assessed subjective dry eye symptoms. The time interval between ST-I and tBUT was at least 10 minutes.
Tear film stability was assessed using fluorescein tBUT. A fluorescein-impregnated strip wet with non-preserved saline solution was placed in the inferior fornix and the patient was asked to blink several times. Using a cobalt blue filter and slit lamp microscopy, we determined the time required for the first area of tear film break-up to appear after a complete blink. The test was repeated three times, and the average was calculated.
We evaluated the ST-I without corneal anesthesia. The test lasted 5 minutes, and the length of wetted paper was directly read off the scale on the paper itself. The Schirmer test was only performed once.
The TMH was evaluated by reading the scale on slit lamp microscopy without fluorescein.
We quantified the intensity of dry eye symptoms from 0 to 4 as follows; 0=none, 1=mild, 2=moderate, 3=severe, 4=very severe. The frequency of dry eye symptoms was quantified as follows; 0=none, 1=some of the time, 2=half of the time, 3= most of the time, 4=all of the time. The aggravation of dry eye (when blink frequency is reduced such as while watching TV, computer monitors, driving) was quantified as follows; 0=none, 1=mild, 2=moderate, 3=severe, 4=very severe. The total dry eye symptom score was calculated as follows10: intensity score + frequency score + aggravation score. Scores ranged from 0 to 12, with higher scores indicating more severe symptoms. We classified the 98 eyes into two groups according to the preoperative values of ST-I. We classified those eyes with preoperative ST-I<10 mm into the dry eye group and those with preoperative ST-I≥10 mm into the non-dry eye group.11,12 The high negative predictive value of diagnostic criteria using ST-I<10 mm/5min can inhibit potential dry eye patients from being classified as the non-dry eye group. Thus, with this criteria, we can suggest that the appearance of dry eye signs following cataract operation should be newly developed signs not affected by potential pre-operative, preexisting dry eye. During the operation, the total length of microscopic light exposure was noted, along with phacoemulsification power and time. Total phacoemulsification energy was calculated as follows: phacoemulsification power × phacoemulsification time.
Postoperatively, the tBUT, TMH, and Sx were examined at 1, 3, and 10 days and 1 and 2 months. ST-I was examined at 10 days, 1 month, and 2 months. We also analyzed changes in these test variables according to corneal incision location and shape in the dry eye group and the non-dry eye group. We evaluated the influence of microscopic light exposure time and phacoemulsification energy on these dry eye test values in both the dry eye group and the non-dry eye group.
Preoperative and Postoperative Topical Medication and Treatment
Before cataract surgery, levofloxacin and NSAID eye drops were instilled four times a day for 1 day. Eye drops with 2.5% percent phenylephrine and tropicamide were used to dilate the pupil an 90 minutes before cataract surgery. Eye drops used after cataract surgery included levofloxacin four times a day for 1 month, dexamethasone four times a day for 1 week and fluorometholone eye drops four times a day in the succeeding 3 weeks. One corneal suture was removed at 1 month postoperatively.
Surgical Technique
AMO Sovereign was used for cataract surgery. A standard phacoemulsification technique was used, beginning with the administration of retrobulbar and Nadbath anesthesia by a single surgeon. A 3.2 mm-sized corneal incision was made using a shallow grooved incision or single plane incision at the superior or temporal location. A 1.0 mm-sized paracentesis was made about 50° apart from the main incision. A foldable acrylic PC-IOL was implanted in the capsular bag. After irrigation and aspiration, a corneal suture was placed. An assistant hydrated the cornea upon the surgeon's command or when the assistant felt like hydration was necessary. Postoperatively, the eye was covered for 1 day.
Statistical Analysis
Data were analyzed by using the Mann-Whitney U test and Wilcoxon Signed Ranks test. SPSS 11.5 for Windows was used for analysis. Spearman's correlation test was used to determine the associations between variables. A p<0.05 was considered statistically significant.
Results
Table 2 shows the preoperative characteristics in the dry eye group and the non-dry eye group. Although we classified the eyes with preoperative ST-I<10 mm into the dry eye group, tBUT values in the dry eye group were less than 10 sec. Preoperative tBUT, Sx, and ST-I values were significantly different between the dry eye group and the non-dry eye group (p<0.05, Mann-Whitney U test). However, in both groups, the preoperative values for tBUT, Sx, ST-I, and TMH were not different between the right and left eyes, as expected (p>0.05, Mann-Whitney U test).
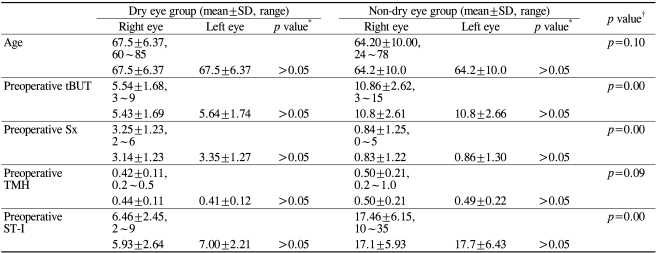
Table 2.
Preoperative characteristics of the dry eye group and the non-dry eye group
*p value=Mann-Whitney U test, comparing right eye and left eye; †p value=Mann-Whitney U test, comparing the dry eye group and the non-dry eye group.
Postoperative Changes over Time
Table 3 and Figure 1 show changes in tBUT, Sx, ST-I, and TMH over time.
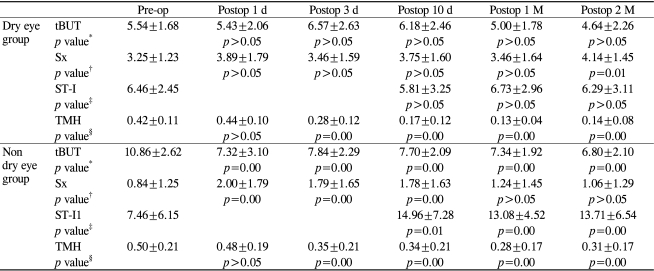
Table 3.
Changes of tear break-up time (tBUT), dryness symptoms (Sx), Schirmer I test value (ST-I) and tear meniscus height (TMH) over time in the dry eye group and the non-dry eye group
*Wilcoxon-Signed Ranks test, compared values of tBUT (tear break-up time, second) between preoperative and postoperative values at specified time point; †Wilcoxon-Signed Ranks test, compared values of Sx (dry eye symptom) between preoperative and postoperative values at specified time point; ‡Wilcoxon-Signed Ranks test, compared values of ST-I (Schirmer test I, mm) between preoperative and postoperative values at specified time point; §Wilcoxon-Signed Ranks test, compared values of TMH (tear meniscus height, mm) between preoperative and postoperative values at specified time point.
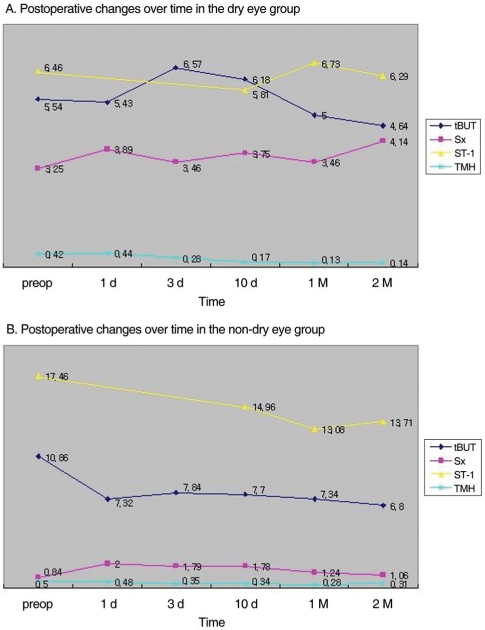
Fig. 1.
Postoperative changes in tear break-up time (tBUT, second), dryness symptoms (Sx), Schirmer test I (ST-I, mm) and tear meniscus height (TMH, mm) over time in both the dry eye (A) and non-dry eye group (B). In the dry eye group, there were significant aggravations in Sx at 2 months postoperative and in TMH at 3 days, 10 days, 1 month, and 2 months postoperative (p<0.05). In the non-dry eye group, almost all dry eye test values were significantly worse after cataract surgery (p<0.05).
In the dry eye group, there were significant aggravations in Sx at 2 months postoperative and in TMH at 3 days, 10 days, 1 month, and 2 months postoperative (p<0.05, Wilcoxon signed rank test).
In the non-dry eye group, almost all dry eye test values were significantly worse after cataract surgery (p<0.05, Wilcoxon signed rank test).
Comparison of Values according to Incision Location
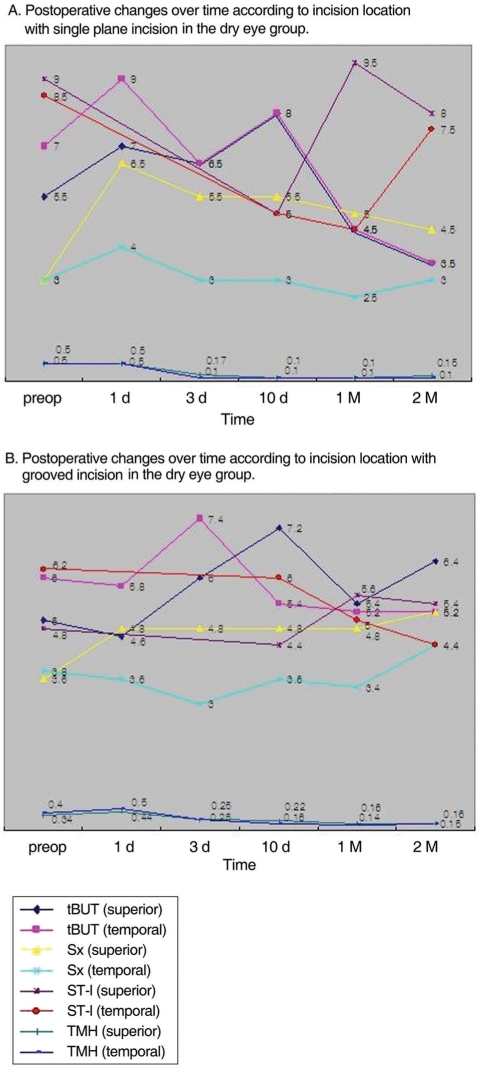
Figure 2 compares values for tBUT, Sx, ST-I, and TMH over time, according to incision location in the dry eye group.
Fig. 2.
Postoperative changes in tear break-up time (tBUT, second), dryness symptoms (Sx), Schirmer test I (ST-I, mm) and tear meniscus height (TMH, mm) over time according to incision location with a single plane (A) or grooved incision (B) in the dry eye group. There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the single plane incision sub-group at any postoperative time point (p>0.05). There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the grooved incision sub-group at any postoperative time point (p>0.05).
There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the single plane incision sub-group at any postoperative time point (p>0.05, Mann-Whitney U test).
There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the grooved incision subgroup at any postoperative time point (p>0.05, Mann-Whitney U test).
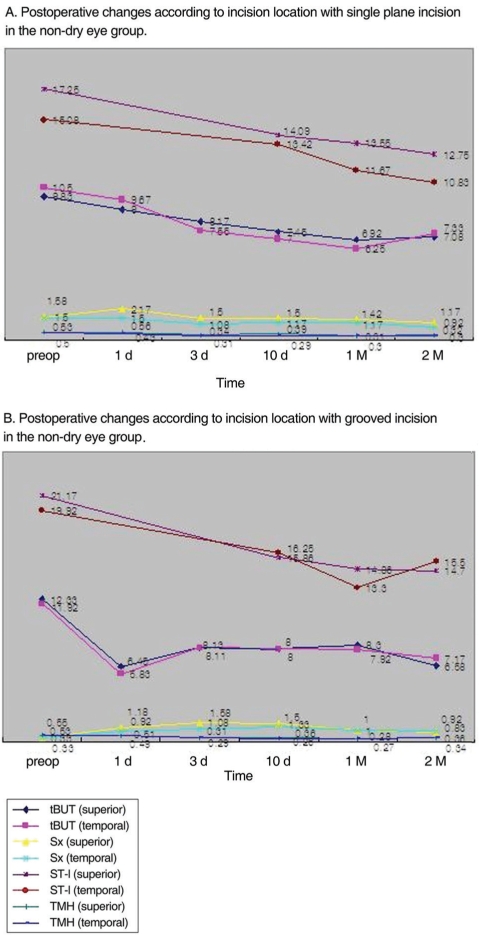
Figure 3 compares values for tBUT, Sx, ST-I, and TMH over time, according to incision location in the non-dry eye group.
Fig. 3.
Postoperative changes in tear break-up time (tBUT, second), dryness symptoms (Sx), Schirmer test I (ST-I, mm) and tear meniscus height (TMH, mm) over time according to incision location with a single plane (A) or grooved incision (B) in the non-dry eye group. There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the single plane incision sub-group at any postoperative time point (p>0.05). There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the grooved incision sub-group at any postoperative time point (p>0.05).
There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the single plane incision sub-group at any postoperative time point (p>0.05, Mann-Whitney U test).
There was no difference in tBUT, Sx, ST-I, or TMH according to incision location in the grooved incision subgroup at any postoperative time point (p>0.05, Mann-Whitney U test).
Comparison of Values according to Incision Shape
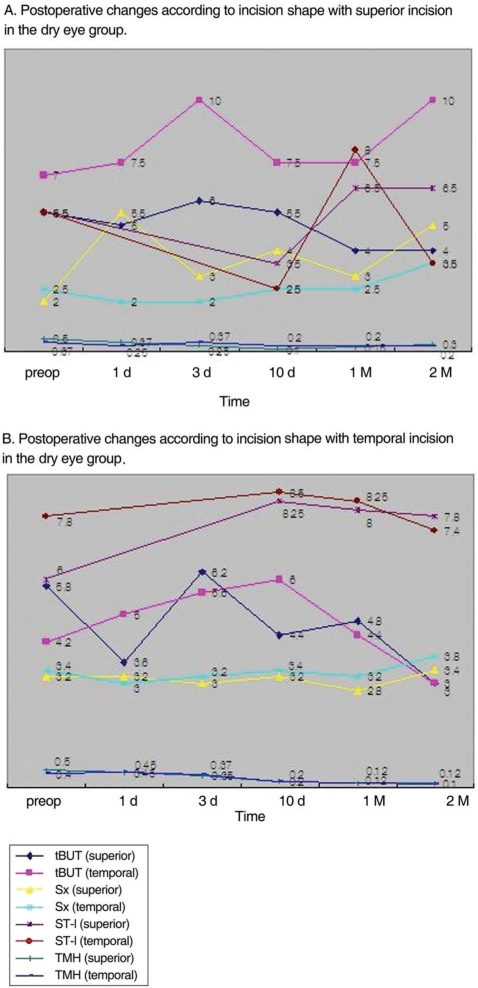
Figure 4 shows changes in tBUT, Sx, ST-I, and TMH over time, according to incision shape in the dry eye group.
Fig. 4.
Postoperative changes in tear break-up time (tBUT, second), dryness symptoms (Sx), Schirmer test I (ST-I, mm) and tear meniscus height (TMH, mm) over time according to incision shape with a superior (A) or temporal incision (B) in the dry eye group. There was no difference in tBUT, Sx, ST-I or TMH according to incision shape in the superior incision sub-group at any postoperative time point (p>0.05). There was no difference in tBUT, Sx, ST-I or TMH according to incision shape in the temporal incision sub-group at any postoperative time point (p>0.05).
There was no difference in tBUT, Sx, ST-I or TMH according to the incision shape in the superior incision subgroup or the temporal incision sub-group at any postoperative time point (p>0.05, Mann-Whitney U test).
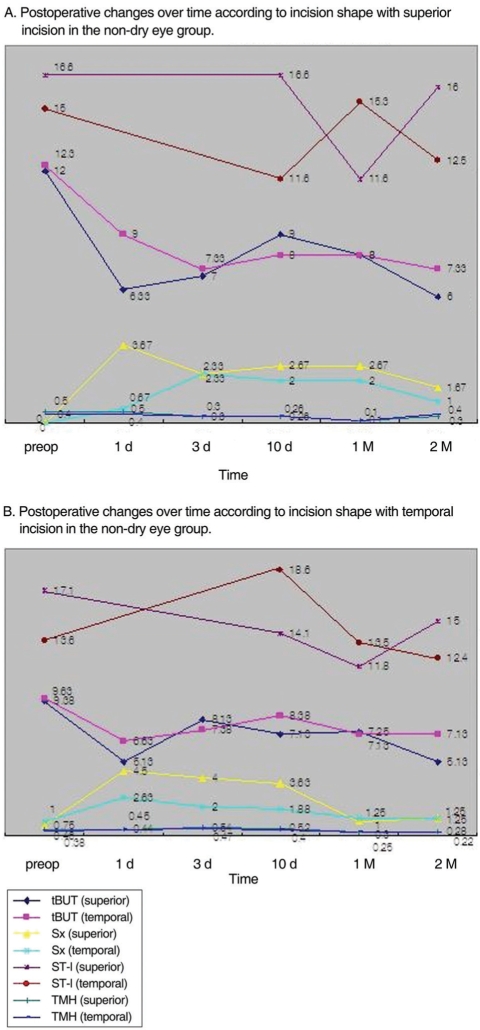
Figure 5 shows changes in tBUT, Sx, ST-I, and TMH over time, according to the incision shape in the non-dry eye group.
Fig. 5.
Postoperative changes in tear break-up time (tBUT, second), dryness symptoms (Sx), Schirmer test I (ST-I, mm) and tear meniscus height (TMH, mm) over time according to incision shape with a superior (A) or temporal incision (B) in the non-dry eye group. tBUT were shorter and Sx were worse with grooved incision than single plane incision at postoperative day 1 in the superior incision sub-group (p=0.04). Sx were worse in the grooved incision subgroup at 1 day (p=0.00), 3 days (p=0.01), and 10 days (p=0.01) postoperative in the temporal incision sub-group.
tBUT were shorter and Sx were worse with the grooved incision than the single plane incision at postoperative day 1 in the superior incision sub-group (p=0.04, Mann-Whitney U test).
Sx were worse in the grooved incision sub-group at 1 day, 3 days, and 10 days postoperative in the temporal incision sub-group (p=0.00, p=0.01, p=0.01, Mann-Whitney U test).
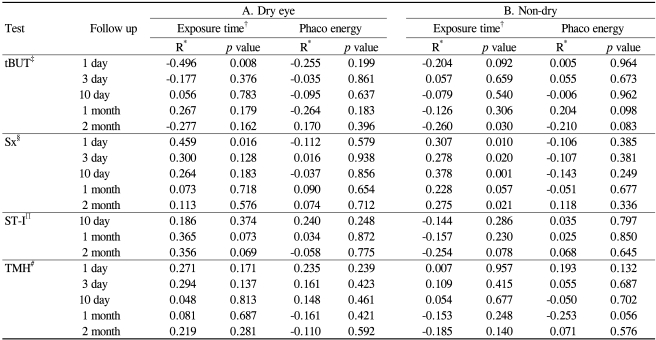
Correlation with Exposure Time to Microscopic Light and Phacoemulsification Energy
Table 4 shows the correlations between dry eye work-up values and microscopic light exposure time as well as between dry eye work-up values and phacoemulsification energy. In the dry eye group, significant correlations were detected between microscopic light exposure time and tBUT and Sx at postoperative day 1. However, there were no correlations between phacoemulsification energy and dry eye test variables. In the non-dry eye group, significant correlations were noted between the microscopic light exposure time and Sx at 1 day, 3 days, 10 days, and 2 months postoperative and in tBUT at 2 months postoperative. There was no correlation between phacoemulsification energy and dry eye test variables.
Table 4.
Correlation between dry eye test values and microscopic light exposure time and between dry eye test values and phacoemulsification energy in the dry eye group (A) and the non-dry eye group (B)
*R=Spearmann Correlation Coefficient; †Exposure Time=Exposure Time to microscopic light; ‡tBUT=tear break-up time; §Sx=dry eye symptom; ∥ST-I=Schirmer test I; #TMH=tear meniscus height.
Discussion
Dry eye sensation frequently occurs after cataract surgery. Affected patients may experience red or watery eyes and constant foreign body sensation. Lesions such as superficial punctate keratitis and epithelial defects may be seen on the cornea.
Generally, the etiology of dry eye following cataract surgery is characterized by one of two mechanisms.1 One patient group experienced an increase in pre-existing dry eye symptoms and the other group experienced surgically-induced dry eye. There are many factors that might affect the ocular surface environment after cataract surgery. Topical anesthesia and eye drops containing preservatives like benzalkonium chloride are well known to have effects on the corneal epithelium.1,13 Exposure to light from the operating microscope might also be associated with postoperative dry eye.1 Most corneal surgical procedures disrupt the normal organization of the corneal innervation, and this results in pathologic changes of the cornea and attendant discomfort.4
Previous studies have shown that tBUT and the barrier function of the corneal epithelium are affected in the early postoperative period after cataract surgery.1,3 In our study, we observed the aggravation of dry eye symptoms and diagnostic test results after cataract surgery compared with preoperative measurements.
We also noted the effect of incision shape on dry eye symptoms and diagnostic test results. Corneal tunnel incisions are classified by their wound architecture as single plane (when there is no groove at the external edge of the incision), shallow grooved (when the initial groove is less than 400 µm), or deeply grooved (when they are deeper than 400 µm).14,15 In grooved incisions, there may be difficulties associated with persistent foreign body sensation and the pooling of mucus and debris within the groove.14 In the non-dry eye group, we observed significant aggravation of dry eye symptoms in patients with grooved incisions over single plane incisions. In the dry eye group, incision shape did not have an effect on the test variables.
With the advent of foldable lenses, there has been increasing interestin temporal corneal incisions. There are obvious advantages to the temporal location, including easy accessibility, low astigmatism, and enhancement of the red reflex.16 However, in our study, with respect to development or aggravation of dry eye after cataract surgery, there was no difference in postoperative dry eye test values between the superior and temporal incision sub-groups in either the dry or the non-dry eye group.
Most surgical procedures that cause denervation of the cornea result in impaired epithelial wound healing, increased epithelial permeability, decreased epithelial metabolic activity and loss of cytoskeletal structures associated with cellular adhesion.4,17 Corneal sensation is a function of the long ciliary nerves of the ophthalmic division of the fifth (trigeminal) cranial nerve. The large nerves of the long ciliary nerve trunk enter the limbus predominantly at the 9-o'clock and 3-o'clock positions. The fact that the long ciliary nerves enter the eye at these positions explains why corneal sensation is significantly greater at the temporal and nasal limbus.4,17 The physiologic role of corneal innervation in the normal cornea is unclear, but it has been suggested that active involvement of neuroregulation is responsible for maintenance of the integrity and repair of the corneal epithelium.17 Furthermore, intact corneal sensation is partially responsible for tear secretion. With decreased corneal sensation, there is a decrease in tear production.17
LASIK entails the severing of the corneal nerves by amicrokeratome and photoablation of the anterior stromal nerves. Both processes damage corneal innervation.5,17 It has been suggested that this damage is due to the fact that the superior-hinge flap severs both arms of the branches of the long ciliary nerves, whereas the nasal-hinge flap preserves one of the nerve plexuses. Hence, use of a wide hinge and a nasal rather than a superior hinge preserves more corneal innervation and reduces the incidence or exacerbation of dry eye resulting from the procedure.17
We expected that there would be a more significant decrease in dry eye test values in the temporal incision group compared to the superior incision group because we assumed that there would be a greater decrease in sensation by cutting the large trunk of corneal nerves entering the limbus predominantly at the 9-o'clock and 3-o'clock positions, as in LASIK surgery. However, we found no difference in dry eye test values according to incision location in either group. There may be many differences between the incision of LASIK and that of cataract surgery with respect to incision width, depth, and location. In cataract surgery, although the width of the incision is very small, the incision depth extends to involve the entire cornea.18,19 Therefore, corneal denervation may differ between the two surgeries.
Many surgeons prefer the grooved incision to the single plane incision because of the greater wound strength when pressure is applied to the posterior lip of the wound.20 However, in this study, grooved incisions significantly exacerbated dry eye symptoms in the non-dry eye group; there was no such exacerbation in the dry eye group. We believe this disparity may be due to the following. In the dry eye group, there were preexisting symptoms and low values on diagnostic tests, so the aggravation of subjective postoperative symptoms and test values might be relatively small compared to those seen in preoperative non-dry, healthy eyes.
We noted changes in dry eye symptoms and signs before and after corneal suture removal. Although we expected that removal of the corneal suture would improve dry eye symptoms and signs, there was aggravation of symptoms in the dry eye group, but no significant difference in the non-dry eye group. However, we were unable to examine the pure effect of suture removal. We examined the dry eye test values and symptoms 1 month after suture removal, and the effect of passing time and tapering of eye drops during that period may have affected outcomes. Generally, the presence of a corneal suture would aggravate dry eye symptoms and signs.2 However, in our study, removal of the suture did not improve the dry eye test values. Furthermore, in the dry eye group, symptoms were aggravated irrespective of suture removal.
The use of ultrasound in cataract surgery may damage corneal structures such as the epithelium, stroma, keratocyte, endothelium, and nerve plexuses.21 In our study, phacoemulsification energy did not aggravate dry eye symptoms or signs in either group.
Many reports have addressed iatrogenic retinal phototoxicity related to operating microscope exposure.22-24 Aside from retinal phototoxicity, as mentioned in the results of our study, microscopic light exposure may aggravate dry eye symptoms and signs in both the dry eye and non-dry eye group. Hazards due to specific light components from the operating microscope may be decreased through the use of appropriate filters and short exposure times.23
There are some limitations to this study. First, the Schirmer test and measurements of tBUT and TMH are easy to perform. However, they may give varied results, and this compromises their reliability.25 We measured the ST-I, so reflex tearing was included. Second, the value of dry eye symptoms are expressed as a numerical value representing subjective ocular irritation symptoms such as dryness, burning, foreign body sensation, heaviness of the lids, and ocular fatigue. A third limitation is the short follow-up period.
In conclusion, we observed that cataract surgery is capable of aggravating dry eye and affecting dry eye test values. Therefore, the following should be considered in the perioperative period. Before surgery, patients should be informed about the possible increase in dry eye symptoms. Intraoperative exposure to the microscopic light should be minimized. The clinician should also be cognizant of the fact that grooved incisions, despite their advantages in other respects, can aggravate dry eye symptoms and signs in eyes that were healthy preoperatively.
References
- 1.Hiroko BM. Cataract Surgery in the Presence of other ocular comorbidities. In: Steinert RF, editor. Cataract Surgery: Technique, Complication and Management. Saunders; 2004. chap. 32. [Google Scholar]
- 2.Jagat R, Amit G, Gagandeep SB, et al. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28:1386–1389. doi: 10.1016/s0886-3350(02)01387-1. [DOI] [PubMed] [Google Scholar]
- 3.Xue-Min Li, Lizhong H, Jinping H, Wei W. Investigation of dry eye disease and analysis of the pathologic factors in patients after cataract surgery. Cornea. 2007;26:S16–S20. doi: 10.1097/ICO.0b013e31812f67ca. [DOI] [PubMed] [Google Scholar]
- 4.Kohlhaas M. Corneal sensation after cataract and refractive surgery. J Cataract Refract Surg. 1998;24:1399–1409. doi: 10.1016/s0886-3350(98)80237-x. [DOI] [PubMed] [Google Scholar]
- 5.Ang RT, Dartt DA, Tsubota K. Dry eye after refractive surgery. Curr Opin Ophthalmol. 2001;12:318–322. doi: 10.1097/00055735-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Belmonte C. Eye Driness Sensations after Refractive surgery: Impaired Tear Secretion or "Phantom" Cornea? J Refract Surg. 2007;23:598–602. doi: 10.3928/1081-597X-20070601-11. [DOI] [PubMed] [Google Scholar]
- 7.Altinors DD, Akca S, Akova YA, et al. Smoking associated with damage to the lipid layer of the ocular surface. Am J Ophthalmol. 2006;141:1016–1021. doi: 10.1016/j.ajo.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 8.Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 9.Lee AJ, Lee J, Saw SM, et al. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol. 2002;86:1347–1351. doi: 10.1136/bjo.86.12.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and Validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118:615–621. doi: 10.1001/archopht.118.5.615. [DOI] [PubMed] [Google Scholar]
- 11.Vitali C, Moutsopoulos HM, Bombardieri S. The European community study group on diagnostic criteria for Sjogren's syndrome.sensitivity and specificity of tests for ocular and oral involvement in Sjogren's syndrome. Ann Rheum Dis. 1994;53:637–647. doi: 10.1136/ard.53.10.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khanal S, Tomlinson A, McFadyen A, et al. Dry eye diagnosis. Invest Ophthalmol Vis Sci. 2008;49:1407–1414. doi: 10.1167/iovs.07-0635. [DOI] [PubMed] [Google Scholar]
- 13.Walker TD. Benzalkonium Toxicity. Clin Experiment Ophthalmol. 2004;32:657. doi: 10.1111/j.1442-9071.2004.00922.x. [DOI] [PubMed] [Google Scholar]
- 14.Fine IH, Hoffman RS, Packer M. Profile of clear corneal cataract incisions demonstrated by ocular coherence tomography. J Cataract Refract Surg. 2007;33:94–97. doi: 10.1016/j.jcrs.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Fine IH, Hoffmann RS, Packer M. Incision Construction. In: Steinert RF, editor. Cataract Surgery: Technique, Complication and Management. Saunders; 2004. chap.12. [Google Scholar]
- 16.Jaffe NS, Jaffe MS, Jaffe GF. Cataract Surgery and Its Complications. 6th ed. Mosby; 1997. Surgical Technique. chap. 9. [Google Scholar]
- 17.Donnenfeld ED, Solomon K, Perry HD, et al. The effect of hinge position on corneal sensation and dry eye after LASIK. Ophthalmology. 2003;110:1023–1029. doi: 10.1016/S0161-6420(03)00100-3. [DOI] [PubMed] [Google Scholar]
- 18.Chang-Ling T, Vannas A, Holden BA, O'Leary DJ. Incision Depth Affects the recovery of corneal sensitivity and neural regeneration in the cat. Invest Ophthalmol Vis Sci. 1990;31:1533–1541. [PubMed] [Google Scholar]
- 19.Chan-Ling T, Tervo K, Tervo T, et al. Long term neural regeneration in the rabbit following 180 degress Limbal Incision. Invest Ophthalmol Vis Sci. 1987;28:2083–2088. [PubMed] [Google Scholar]
- 20.Ernest PH, Neuhann T. Posterior limbal incision. J Cataract Refract Surg. 1996;23:78–84. doi: 10.1016/s0886-3350(96)80274-4. [DOI] [PubMed] [Google Scholar]
- 21.Mencucci R, Ambrosini S, Ponchietti C, et al. Ultrasound thermal damage to rabbit corenas after simulated phacoemulsification. J Cataract Refract Surg. 2005;31:2180–2186. doi: 10.1016/j.jcrs.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 22.Michels M, Sternberg P., Jr Operating microscope_induced retinal phototoxicity: Pathophysiology, Cinical Manifestations and Prevention. Surv Ophthalmol. 1990;34:237–252. doi: 10.1016/0039-6257(90)90025-q. [DOI] [PubMed] [Google Scholar]
- 23.Michael R, Wegener A. Estimation of safe exposure time from an ophthalmic operating microscope with regard to ultraviolet radiation and blue-light hazards to the eye. J Opt Soc Am A Opt Image Sci Vis. 2004;21:1388–1392. doi: 10.1364/josaa.21.001388. [DOI] [PubMed] [Google Scholar]
- 24.Pavilack MA, Brod RD. Site of potential operating microscope light-induced phototoxicity on the human retina during temporal approach eye surgery. Ophthalmology. 2001;108:381–385. doi: 10.1016/s0161-6420(00)00536-4. [DOI] [PubMed] [Google Scholar]
- 25.Serin D, Karsloğlu S, Kyan A, Alagöz G. A simple approach to the repeatability of the Shirmer test without anesthesia. Cornea. 2007;26:903–906. doi: 10.1097/ICO.0b013e3180950083. [DOI] [PubMed] [Google Scholar]