Abstract
Low numeracy skills and obesity are both common. Numeracy skills are used in healthy weight management to monitor caloric intake. The relationship between obesity and numeracy skills in adult primary care patients is unknown. A cross-sectional study enrolled adult, English-speaking primary care patients. BMI was assessed by self-report; numeracy and literacy skills were measured with the Wide Range Achievement Test, 3rd Edition (WRAT-3) and the Rapid Estimate of Adult Literacy in Medicine (REALM), respectively. The relationship between numeracy and BMI was described with Spearman's rank correlation and linear regression analyses. In 160 patients, the mean (s.d.) age was 46 (16) years, 66% were white, 70% were female, and 91% completed high school. The mean BMI was 30.5 (8.3) kg/m2. Less than 9th grade numeracy skills were found in 66% of the participants. Participants with numeracy skills <9th grade had a mean BMI of 31.8 (9.0) whereas those with numeracy skills ≥9th grade had a mean BMI of 27.9 (6.0), P = 0.008. Numeracy was negatively and significantly correlated with BMI (ρ = −0.26, P = 0.001). This correlation persisted after adjusting for age, sex, race, income, years of education, and literacy (β coefficient = −0.14; P = 0.010). Literacy skills were not associated with BMI. We found a significant association between low numeracy skills and higher BMI in adult primary care patients. A causal relationship cannot be determined. However, numeracy may have important clinical implications in the design and implementation of healthy weight management interventions and should be further evaluated to determine the magnitude of its effect.
Numeracy, an important component of literacy, can be broadly defined as the ability to use numbers in everyday life (1). Health numeracy is using numbers in a health-related context that may involve calculations, dates, tables, graphs, deduction, risk interpretation, and other skills (2). In 2003, the National Assessment of Adult Literacy found that >110 million Americans have basic or poor quantitative skills (3).
Numeracy may be important in the management of weight. Overweight and obese patients are often counseled to monitor their caloric intake, read food labels, track daily steps, and understand disease risk associated with excess weight. A recent study found that patients with low numeracy skills had greater difficulty interpreting food labels (4). Another recent study found no correlation between literacy and obesity but did not investigate the relationship between numeracy and obesity (5). This study examined the association between numeracy skills and weight status as measured by BMI.
Methods
Setting and participants
Between July 2006 and August 2007, a convenience sample of participants were enrolled from an academic primary care clinic where they were referred by clinic staff. Exclusion criteria included age <18 years, non-English speaking, dementia, and corrected visual acuity equal to or worse than 20/50 by a Rosenbaum Pocket Vision Screener. Patients received $10 for study participation. This study was approved by the Institutional Review Board of Vanderbilt University for exemption under 45 CFR 46.101(b)(2) for surveys or observations where no identifying information was collected. Oral consent was obtained from all study participants.
Measures
Demographic and anthropometric information was obtained from patient interview. Height and weight were self-reported by the patient after measurement by clinic staff. Literacy was measured using the Rapid Estimate of Adult Literacy in Medicine (REALM). The REALM is a validated instrument that assesses one's ability to read common medical words and correlates highly with other measures of reading comprehension (6). Numeracy was assessed with the Wide Range Achievement Test, 3rd Edition (WRAT-3) (ref. 7). The WRAT-3 is a validated measure that tests general arithmetic skills including counting, number symbols and computation and represents general numeracy skills. The WRAT-3 is standardized to a mean of 100 by age and sex.
Statistical analysis
Analyses were performed using STATA 9.2 (STATA, College Park, TX). Descriptive analyses of all variables were performed. Numeracy and literacy were examined both as continuous variables (primary analysis) and also categorical variables (confirmatory analysis). They were categorized a priori <9th grade or ≥9th grade. The relationship between numeracy and BMI was examined using Spearman's rank correlation or Wilcoxon rank sum, based on parametric attributes.
Analyses were performed for unadjusted and adjusted linear regression models including potential confounding variables determined a priori, including age, sex, race, income, years of education, and REALM score.
Results
From July 2006 to August 2007, 248 patients were referred for study participation. Of these, 77 patients declined to participate and 2 patients met exclusion criteria. Of the 169 (69%) who consented to participate, 160 (95%) completed the study.
The mean age (s.d.) was 46 (16) years, 66% were white, 70% were female, and 23% reported yearly income <$20,000. Ninety-one percent of participants reported completing high school or obtaining their Certificate of General Educational Development. Twenty-three percent had <9th grade literacy skills and 66% of participants had <9th grade numeracy skills. The mean BMI (s.d.) was 30.5 (8.3) kg/m2. Twenty-six percent of participants reported having dyslipidemia, 38% reported hypertension, 8% reported coronary artery disease, and 17% reported diabetes (Table 1).
Table 1.
Participant characteristics
| Characteristics | All participants (n = 160) | Low numeracy (<9th grade) (n = 106) | Adequate numeracy (≥9th grade) (n = 54) |
|---|---|---|---|
| BMI (kg/m2)a | 30.5 (8.3) | 31.8 (9.0) | 27.9 (6.0)** |
| WRAT-3a | 89.1 (16) | 80.9 (11) | 105 (9.1)* |
| Demographics | |||
| Age (years)a | 46.0 (16) | 45.1 (16) | 47.6 (15) |
| Female (n) (%) | 112 (70) | 74 (70) | 38 (70) |
| Non-white race (n) (%) | 55 (34) | 51 (48) | 4 (7.3)* |
| Income (n) = 154 | |||
| <$10,000 (n) (%) | 25 (16) | 23 (23) | 2 (3.8)** |
| $10,000 to <$20,000 (n) (%) | 11 (7) | 8 (7.9) | 3 (5.7) |
| $20,000 to <$40,000 (n) (%) | 39 (25) | 31 (31) | 8 (15) |
| $40,000 to $60,000 (n) (%) | 29 (19) | 17 (17) | 12 (23) |
| >$60,000 (n) (%) | 50 (32) | 22 (22) | 28 (53) |
| Education (years)a | 14.3 (2.9) | 13.3 (2.4) | 16.1 (2.8)* |
| <High school (n) (%) | 15 (9.4) | 14 (13) | 1 (1.9)** |
| ≥High school or GED (n) (%) | 145 (91) | 92 (87) | 53 (98) |
| REALM (0−66)a | 61.0 (8.7) | 59.1 (10) | 64.8 (2.1)* |
| <9th grade literacy skills (n) (%) | 36 (22.5) | 33 (31) | 3 (5.6)* |
| ≥9th grade literacy skills (n) (%) | 124 (77.5) | 73 (69) | 51 (94) |
GED, Certificate of General Educational Development; REALM, Rapid Estimate of Adult Literacy in Medicine; WRAT-3, Wide Range Achievement Test, 3rd Edition.
Mean (s.d.).
P < 0.001
P < 0.05.
The relationship between numeracy and BMI is shown in Figure 1. Numeracy was negatively correlated with BMI (ρ = −0.26, P = 0.0010) whereas literacy was not correlated with BMI (ρ = −0.0052, P = 0.51). When numeracy and literacy were treated as categorical variables, low numeracy was associated with higher BMI. Participants with numeracy skills <9th grade had a mean BMI (s.d.) of 31.8 (9.0) whereas participants with numeracy skills ≥9th grade had a mean BMI (s.d.) of 27.9 (6.0), P = 0.008. (Table 1) Categorical literacy skills were not associated with BMI (<9th grade literacy—BMI 31.7 (9.9); ≥9th grade literacy—BMI 30.2 (7.8), P = 0.50). Participants with a BMI ≥30 were significantly more likely to have numeracy skills <9th grade level than participants with a BMI <30 (74% vs. 59%, P = 0.033); however, no significant difference was found for participants with literacy skills <9th grade (24% vs. 21%, P = 0.37).
Figure 1.
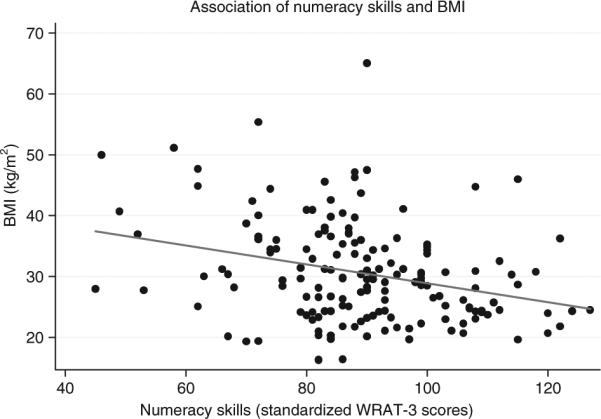
Scatterplot with linear prediction of standardized WRAT-3 scores to BMI. WRAT-3, Wide Range Achievement Test, 3rd Edition.
In linear regression models adjusting for age, sex, race, income, and years of education, the association of numeracy skills and BMI remained consistent with a β coefficient of −0.14, P = 0.01. None of the other variables, including literacy skills, were significantly associated with BMI (β = 0.038; P = 0.71 for REALM score).
Discussion
This study demonstrates a statistically significant negative association between numeracy skills and BMI. This study did not find a relationship between literacy skills and BMI. The finding of a negative correlation between numeracy and excess weight, if verified by subsequent research, may have important clinical implications in weight management practice as many current weight-reducing recommendations rely on quantitative skills to monitor caloric intake and energy expenditure and understand risk associated with excess weight. Patients with low numeracy skills may not be able to interpret or apply traditional weight management counseling effectively. Patients with low numeracy skills may benefit from numeracy-sensitive interventions to promote weight loss. For example, patients with low numeracy may be less able to interpret nutrition food labels and may have greater weight loss with a meal replacement plan.
This study has several limitations. As a cross-sectional study, causal inferences must be made with caution. This study cannot determine whether patients with lower numeracy skills are at increased risk for developing obesity due to poorer understanding of weight management–related issues, or whether patients with obesity are less likely to acquire adequate numeracy skills. In childhood and adolescent studies, obesity is associated with poorer school performance, lower self-esteem and self-efficacy (8). In addition, human observational studies have shown that obesity is related to cognitive impairment in adults (9–11). Longitudinal studies are needed to better understand the relationship of low numeracy and excess weight. The study population was generally well educated and had high literacy skills. Although this may limit the generalizability of the study's findings, it highlights the high prevalence of low numeracy. Replication of these findings in a randomly selected population is needed to confirm these results. Additionally, literacy and numeracy skills may be markers for unmeasured confounders of socioeconomic status or other factors that are also related to obesity.
Poor numeracy is a very common problem, and the measurement of numeracy skills before weight loss program participation could help to identify barriers to a patient's success in weight loss. Addressing numeracy could be an important consideration in the design of effective educational programs tailored to improve patient understanding and patient behavior. Caution must be taken to prevent the development of any negative stereotypes from this approach. Interventions tailored to numeracy skills should be used only to aid in the successful weight management of patients with obesity and not to illicit any embarrassment or added stress. Future studies in weight management should consider the potential role of patient numeracy skills.
ACKNOWLEDGMENTS
M.M.H. was supported by the Vanderbilt Environmental Health Science Scholars Program (NIEHS 1K12ES01585501). R.L.R. has received support from a National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Career Development Award (NIDDK 5K23DK065294), from the American Diabetes Association (Novo Nordisk Clinical Research Award), the Pfizer Clear Health Communication Initiative, and the Vanderbilt Diabetes Research and Training Center (NIDDK 5P60DK020593).
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
ReFeRences
- 1.Rothman R, Montori V, Cherrington A, Pignone M. Perspective: the role of numeracy in health care. J Health Commun. doi: 10.1080/10810730802281791. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ancker JS, Kaufman D. Rethinking health numeracy: a multidisciplinary literature review. J Am Med Inform Assoc. 2007;14:713–721. doi: 10.1197/jamia.M2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kutner M, Greenberg E, Jin Y, et al. Literacy in Everyday Life: Results from the 2003 National Assessment of Adult Literacy. National Center for Education Statistics; Washington, DC: 2007. [Google Scholar]
- 4.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 5.Wolf MS, Gazmararian JA, Baker DW. Health literacy and health risk behaviors among older adults. Am J Prev Med. 2007;32:19–24. doi: 10.1016/j.amepre.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 7.Wilkinson G. The Wide Range Achievement Test—Third Edition (WRAT-3) Wide Range; Wilmington, DE: 1993. [Google Scholar]
- 8.Taras H, Potts-Datema W. Obesity and student performance at school. J Sch Health. 2005;75:291–295. doi: 10.1111/j.1746-1561.2005.00040.x. [DOI] [PubMed] [Google Scholar]
- 9.Wolf PA, Beiser A, Elias MF, et al. Relation of obesity to cognitive function: importance of central obesity and synergistic influence of concomitant hypertension. The Framingham Heart Study. Curr Alzheimer Res. 2007;4:111–116. doi: 10.2174/156720507780362263. [DOI] [PubMed] [Google Scholar]
- 10.Geroldi C, Frisoni GB, Paolisso G, et al. Insulin resistance in cognitive impairment: the InCHIANTI study. Arch Neurol. 2005;62:1067–1072. doi: 10.1001/archneur.62.7.1067. [DOI] [PubMed] [Google Scholar]
- 11.Jeong SK, Nam HS, Son MH, Son EJ, Cho KH. Interactive effect of obesity indexes on cognition. Dement Geriatric Cognitive Disord. 2005;19:91–96. doi: 10.1159/000082659. [DOI] [PubMed] [Google Scholar]


