Abstract
The Veterans Health Administration (VHA) serves the health care needs of an adult, predominantly male, and aging population. The aging profile of VHA patients is 25% greater than the civilian sector (DVA 2001). Aged patients are at higher risk for falls. In February 2002, 6 VHA medical centers profiled their inpatients’ fall risk profile as one aspect of program initiatives targeted at reducing veterans’ fall risk and fall-related injuries, participating in a one-day collection of fall risk measurement using the Morse Fall Scale (MFS) for all inpatients (n=1819), acute and long-term care units. Data results are reported for age, MFS score, and the relationship between age and score, and by type of ward/unit, ie, predominately acute and critical care or long-term care. The results of this prevalence study documented that the veteran inpatient population are at high-risk for anticipated physiological falls. This Veteran Integrated Services Network-wide Deployment of an Evidence-based Program to Prevent Patient Falls study was completed as part of a nationally funded clinical initiative, National Program Initiative 20-006-1.
Keywords: fall risk assessment, fall risk prevalence, inpatient falls, Morse Fall Scale
Introduction
Falls and fall-related injuries have a significant societal impact in terms of deteriorating quality of life, suffering, lost productivity, need for daily living care, and healthcare costs. An estimated one in three older adults living in the community fall each year (CDC 2005). Some studies have found that around 10% of falls end in serious injury (HHS 2004). One third to one half of the US population aged 65 and older will fall (Ignatavicius 2000; Anonymous 2003; Anderson 2004), resulting in 300 000 hip fractures annually (Anonymous 2003; Anderson 2004), with rising morbidity and mortality rates in other countries (Johnson et al 2001). Hip fractures result in US healthcare expenditures totaling $20.2 billion per year (Anonymous 2003; Anderson 2004).
Falls are the second most common adverse event within healthcare institutions following medication errors (Kohn et al 2000). If falls and fall-related injuries are common, costly, and dangerous, this is especially true for elderly and/or disabled patients in hospitals, as well as across the full continuum of care (Rubenstein et al 1994, 2001; Englander et al 1996; Brainsky et al 1997; Doweiko 2000).
Fall risk profiling
Hospitals have begun to address the problem of inpatient falls in a variety of ways. One of the most common ways is the development of a fall prevention program to decrease the risk of falls and fall-related injuries. The first step in decreasing a patient’s risk for falls and fall-related injuries is by profiling individuals’ level of fall risk. This risk profiling requires consistent application of a valid, reliable fall risk assessment tool that identifies patients at risk. Once these patients are identified, nursing staff and administrators can then identify patient-specific strategies to prevent falls and incorporate these into the plan of care. (Morse 1997)
Different patient risk factors and healthcare settings require different strategies; and a priori, most staff and administrators would assume that patients in a long-term care setting would present with different and higher risk scores than those in acute care. This a prior assumption was confirmed in a study by Morse (1997) in 16 patient care units in 2 institutions over a 5-month period. We are unaware of any similar study using a single fall risk assessment tool to assess falls risk in multiple hospitals. As part of a Veterans Integrated Services Network (VISN)-wide fall prevention program, we undertook a fall prevalence study of inpatients in 6 medical centers during a 2-day period to determine fall risk profiles for different inpatient populations in our institutions.
Materials and methods
Fall risk assessment
Different types of falls require different prevention strategies. Falls can be classified into accidental falls, anticipated physiological falls, and unanticipated physiological falls (Morse 1997). Accidental falls, about 14% of falls, are falls from slips or trips, and are often caused by environmental factors, such as water on the floor, or electrical cord, or by errors of judgment, such as not locking the wheelchair before rising. Recognition and correction of environmental hazards and orienting patients to their environment are the keys to reduction of these types of falls. Unanticipated physiological falls cannot be predicted and comprise about 8% of falls. These include such events such as seizures or faintings, and nursing staff can target prevention towards repeat events or reducing injury.
Anticipated physiological falls are the types of falls that are most common (78%), and offer the greatest opportunity for intervention if patients at high risk are identified early and a patient-specific prevention plan is designed and implemented. It is the patient at risk for this type of falls that the Morse Fall Scale (MFS) is designed to identify (Table 1). The MFS is used widely in healthcare to assess patients’ risk for anticipated physiological falls – those falls that we anticipate will occur to the patients’ existing physiological status, history of falls, and decreased mobility at assessment (Morse 1997).
Table 1.
Morse Fall Scale score
| Choose highest applicable score from each category | Circle all that apply at the time of this fall | |
|---|---|---|
| History of falling | No | 0 |
| Yes | 25 | |
| Secondary diagnosis (More than one diagnosis) | No | 0 |
| Yes | 15 | |
| Ambulatory aid | None, on bedrest, uses W/C, or nurse assists | 0 |
| Crutches, cane(s), walker | 15 | |
| Furniture | 30 | |
| IV/Heparin lock or saline | No | 0 |
| PIID | Yes | 20 |
| Gait/transferring | Normal, on bedrest, immobile | 0 |
| Weak (Uses touch for balance) | 10 | |
| Impaired (Unsteady, difficulty rising to stand) | 20 | |
| Mental status | Oriented to own ability | 0 |
| Forgets limitation | 15 | |
| Total Morse Fall Scale score at the time of fall (high risk >50) | ||
Planning and purpose
In 1999, patient safety leaders in the 6 VISN 8 medical centers examined consistency of fall risk assessment tools and practices. They found that nurses were not using the same valid, reliable fall risk instrument that provided the basis for clinical decision-making and evidence-based intervention. Therefore, nursing executives met with patient safety leaders, and agreed to implement the MFS for use across all inpatient settings. Patients were to be assessed upon admission, and at change in status. The MFS was incorporated into the patient assessment forms and staff were trained in its use.
The present study was just one small part of a 2-year evidence-based fall prevention program starting in 2000 in 2 VISNs, VISN 8 and 22, funded by VHA headquarters. The goal of this program was to enhance the quality, appropriateness, and cost effectiveness of healthcare delivered to veterans who are at risk for falling in acute care, long term care, and community-based settings. Comparisons of falls rates and injury rates across and between VISNs was one stage towards achieving our objective of building infrastructures that support patient safety by creating safer environments for all patients. A number of programs and products were developed from this program for national distribution.
The purpose of the fall risk prevalence study was to profile inpatient fall risk across our 6 VISN 8 medical centers. This VISN-wide study of fall risk was approved by all nursing executives, and was authorized under approved program evaluation protocols processed through research and development and investigational review board. Reliability was assessed at 2 time points (January and April 2001) prior to the initiation of the prevalence study. Paired inter-rater reliability indicated readiness for implementing the prevalence study: (Pearson’s product moment correlation coefficient [r]=0.912; p<0.0001) and (r=0.925; p<0.0001) for January and April 2001, respectively.
Study design
Since no fall risk prevalence study has been reported in the literature, we followed the study design for the pressure ulcer prevalence survey, commonly conducted in inpatient settings (Amlung et al 2001). We employed a similar cross-sectional study design for our study of fall risk prevalence.
Lack of uniformity in risk assessment tools and inter-rater reliability can complicate comparisons of inpatient populations between and within hospitals. However, for the last 5 years, all inpatients in the VHA Medical Centers in Florida and Puerto Rico, which comprises the VHA Sunshine Network (VISN 8), are assessed for fall risk using one tool – the MFS (Morse 1997). Using a uniform fall risk assessment tool across medical centers has made this prevalence study possible, as well as the targeting and sharing of fall intervention programs to patient profiles based on severity of risk.
Coordinating with the facilities’ nurse managers, the fall program coordinators developed a plan to conduct the prevalence study. Over a 2-day period, every inpatient in the 6 medical centers was to be assessed using the MFS. The patients’ primary nurse or associate nurse (registered nurses only) rated each patient by MFS, and gave the scores to the nurse managers. All patients were rated during the day shift. Two days later, the nurse managers submitted the raw MFS scores for each patient to the VISN 8 data manager. Nurse managers reported their data by unit, and each of 99 units was categorized by type of care services into acute/critical care (medical, surgical, intensive care, and rehabilitation units) or long-term care. While patients in all open wards/units were to be included, patient MFS data from 4 units, 3 acute/critical care and 1 long-term care unit were not reported, and thus excluded from analysis. Upon receipt of the data, the data manager entered all data by unit by VHA medical center into a central database. All data were cleaned prior to data analysis. Data results examined the relationship between age and MFS scores, and type of ward/unit, using the Pearson coefficient and analysis of variance.
Results
A total of 1819 patients in 96 units were assessed for their fall risk score during the 2-day period. As seen in Table 2, the average age of the patients was 69 years of age with the youngest being 19 and the oldest being 107 years old. The mean MFS for these patients was 49. The frequency distribution for MFS is shown in Figure 1.
Table 2.
Age and Morse score descriptive statistics
| n | Min | Max | Median | Mean | SD | |
|---|---|---|---|---|---|---|
| Age | 1789 | 19 | 107 | 72 | 69.31 | 12.8023 |
| Morse Score | 1819 | 0 | 125 | 50 | 49.07 | 24.1422 |
Figure 1.
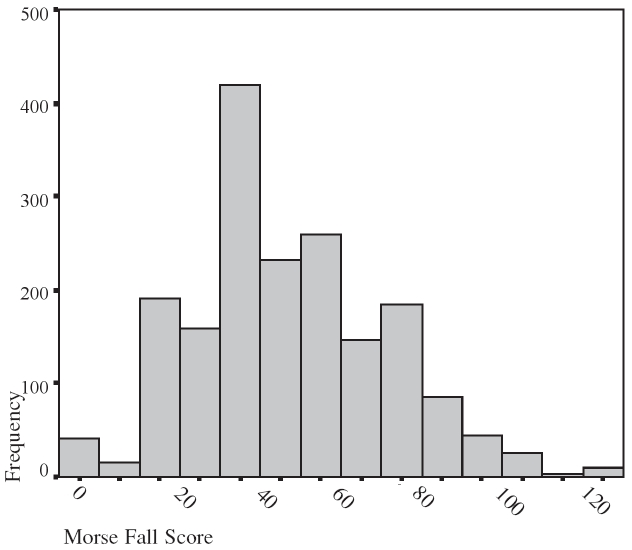
Frequency distribution of Morse scores.
Age alone was not highly correlated with the MFS (r=0.288, p<0.01) although the relationship was statistically significant. As the patient’s age increased, the mean MFS also tended to increase in an approximately linear manner. This association is graphically represented in Figure 2.
Figure 2.
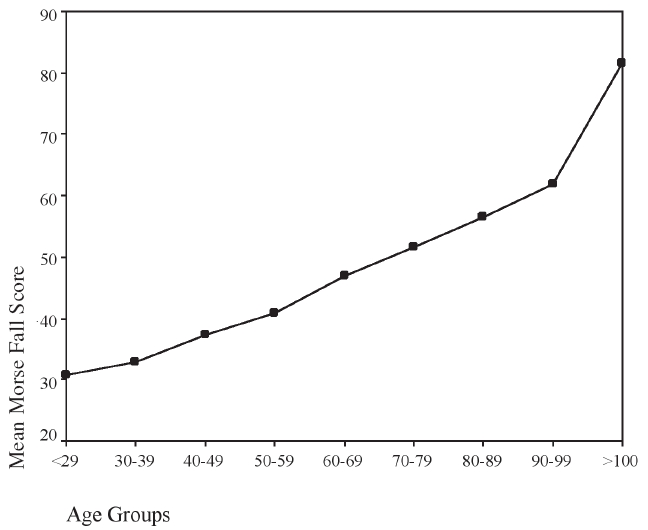
Distribution of Morse Fall Score among age groups.
Age and the MFS also varied significantly according to the type of ward/unit (Table 3). The mean age in the acute/critical units was 66 years old. This was significantly different (p<0.001) than the 73 year mean age in the long-term care units. The mean MFS of 50.75 in long-term care was significantly higher (p=0.002) than the mean MFS of 47.3 in the acute/critical care.
Table 3.
Age and Morse score by type of unit
| Unit type | n | Mean | SD | |
|---|---|---|---|---|
| Age * | Acute/critical care | 865 | 65.56 | 12.9113 |
| Long-term care | 924 | 72.82 | 11.6585 | |
| Morse Fall Score ** | Acute/critical care | 883 | 47.30 | 25.6385 |
| Long-term care | 936 | 50.75 | 22.5256 |
t= −12.5, p<0.0001
t= −3.1, p=0.002
Abbreviations: SD, standard deviation.
Discussion
It was not surprising to find that older patients and those in long term care settings are at higher risk for anticipated physiological falls (Table 3). However, the large standard deviation (25.64) around the mean (47.3) for acute/critical care settings suggests that a large number of patients in this setting of care are at very high risk for anticipated physiological falls. Greater attention to development of appropriate fall prevention strategies for these settings of care is warranted.
The results of this fall risk prevalence study validate the high fall risk status of our inpatient veterans as determined by the MFS. These findings support our ongoing commitment to the implementation and evaluation of fall prevention interventions throughout our acute care and long term care units. We believe that our clinical fall teams are positively impacting patient safety as fall prevention experts and resources throughout our VISN.
Falls are under-reported, but are receiving increased national attention due to rising fall-related injury rates leading to death, loss of independence associated with aging (OMI 1999; Oliver et al 2000; Agostini et al 2001). Healthcare providers have come to learn that many falls can be prevented through accurate and systematic assessment and patient-specific interventions (GPFOP 2001).
The severity of fall-related injuries can be reduced with the proper use of protective strategies. However, a clear understanding of fall definition and type between clinicians is critical, and then meaningful fall assessment protocols and fall reduction intervention programs can be individualized to meet patients’ needs and tested for overall effectiveness. While patient falls and fall-related injuries have been the focus of traditional quality assurance programs for over 3 decades, prioritized organizational safety improvements continue to target reducing fall rates and fall-related injuries.
While research on preventing patient falls is widely available, a major challenge is implementing use of valid, reliable instruments into practice, which are needed for evidenced-based fall prevention interventions. This study describes the process and outcomes of a multi-institutional patient safety effort in hospitals and long term care facilities within the VHA system, designed to determine veterans’ fall risk profiles as part of a major commitment towards reducing falls and fall-related injuries among inpatients/residents.
Relevance of findings and future recommendations
Fall prevention programs have targeted those at-risk patients in acute-care or long-term care facilities. Our study findings support our premise that almost all inpatient veterans are at risk for anticipated physiological falls. The findings of this study support the need for development of patient-specific interventions and fall prevention programs throughout the continuum of healthcare.
Assessing patients for their fall risk is more important than summing up a score and the success of fall prevention programs is more important than counting overall fall rates. Fall rates must be analyzed by type of fall and effectiveness of interventions must be linked to level of fall risk. We are morally driven to help our patients avoid unnecessary suffering – such as a preventable fall. A strong financial incentive also exists for healthcare institutions to reduce the economic burden of patient falls and injuries. Nurse staff support is essential to successful patient safety programs. Without strong administrative leadership and commitment, no injury prevention program can succeed.
We believe that patients with the highest risk scores are our most vulnerable population. This population probably experiences repeat falls and may have already sustained a fall-related injury. Because falls are under-reported, we can not rely only on self-reports of fall occurrence. Instead, we can use clinical findings, based on valid and reliable fall risk assessment, to diagnose the type of fall an at-risk-patient may have, along with the severity of risk. This diagnosis can be extended to population cohorts within clinical settings so that appropriate fall prevention programs are implemented at the point of entry into our healthcare. We must protect patients from falls and injuries while in our care.
More than fall rates: type of falls
We recommend that institutions move to analyzing falls according to the three categories described by Morse (1997). If the majority of falls are anticipated physiological falls, the focus should be on protecting the patient from falling by implementing all possible interventions for these high-risk patients. We also believe that more focused research is needed on the patient who experiences repeat falls, determining the effectiveness of team communication and care planning redesign.
Based on the results of this study and other portions of our fall prevention program, we recommend that hospitals wishing to improve patient safety and reduce falls and fall-related injuries: 1) adopt consistent, valid, reliable measures of fall risk across all settings of care; 2) acquire added resources (technology and staffing) to protect the high-risk, vulnerable populations most likely to be injured upon a fall; and 3) implement universal fall prevention programs to protect the patient from falling from the point of entry into the healthcare system; 4) establish research programs to test fall prevention interventions (direct, indirect, and environmental) on patient safety; and 5) evaluate usefulness of MFS guidelines for at-risk categories based on scores.
VHA’s leadership and commitment to patient safety is unparalleled. This project reflects the cooperative efforts of staff, administrators, quality managers, and researchers to promote our veterans’ freedom, independence and safety.
Footnotes
Disclosure
The study was supported by NPI 02-006-1: VISN-wide Deployment of an Evidence Based Fall Prevention Program: VISN 8 and VISN 22.
References
- Agostini J, Baker D, Bogardus S. Prevention of falls in hospitalized and institutionalized older people. In: Shojania K, Duncan B, McDonald K, et al., editors. Making health care safer: a critical analysis of patient safety practices. San Francisco: University of California at San Francisco (UCSF) – Stanford University Evidence-based Practice Center; 2001. [Google Scholar]
- Amlung SR, Miller WL, Bosley LM. The 1999 national pressure ulcer prevalence survey: a benchmarking approach. Adv Skin Wound Care. 2001;14:297–301. doi: 10.1097/00129334-200111000-00012. [DOI] [PubMed] [Google Scholar]
- Anderson V.2004Fear of falling senior citizens face serious injury, death from losing balance [online]Accessed April 10, 2004. The Atlanta Journal and Constitution E1URL: http://www.proquest.com/
- Anonymous Statistics reveal incidence of falling in the elderly. Ophthalmology Times. 2003;28(20):68. [Google Scholar]
- Brainsky A, Glick H, Lydick E, et al. The economic cost of hip fractures in community-dwelling older adults: a prospective study. J Am Geriatr Soc. 1997;45:281–7. doi: 10.1111/j.1532-5415.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- [CDC] Centers for Disease Control and Prevention 2005Falls and hip fractures among older adults [online]. Accessed 11 September 2005. URL: http://www.cdc.gov/ncipc/factsheets/falls.htm
- Doweiko D. Prevention program cut patient falls by 10% Hosp Case Manage. 2000;8(38):43–4. [PubMed] [Google Scholar]
- [DVA] Department of Veterans Affairs . Department of Veterans Affairs; Washington, DC, USA: 1996. Fall prevention guidelines. [Google Scholar]
- Englander F, Hodson TJ, Terregrossa RA, et al. Economic dimensions of slip and fall injuries. J Forensic Sc. 1996;41:733–46. [PubMed] [Google Scholar]
- [GPFOP] Guideline for the Prevention of Falls in Older Persons J Am Geriatr Soc. 2001;49:664–72. [PubMed] [Google Scholar]
- [HHS] Health and Human Services 2004Falls prevention interventions in the medicare population [online]Accessed 11 September 2005. URL: http://www.cdc.gov/ncipc/falls/fallprev.pdf
- Ignatavicius D. Do you help staff rise to the fall-prevention challenge? Nurs Manage. 2000;31:27–31. [PubMed] [Google Scholar]
- Johnson M, Cusick A, Chang S. Home-screen: a short scale to measure fall risk in the home. Public Health Nurs. 2001;18:169–77. doi: 10.1046/j.1525-1446.2001.00169.x. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan J, Donaldson MS, editors. To err is human: building a safer health system. Washington DC: Nat Acad Press; 2000. [PubMed] [Google Scholar]
- Morse J. Preventing patient falls. Thousand Oaks CA: SAGE; 1997. [Google Scholar]
- Oliver D, Hopper A, Seed P. Do hospital fall prevention programs work? A systematic review. J Am Geriatr Soc. 2000;48:1679–89. doi: 10.1111/j.1532-5415.2000.tb03883.x. [DOI] [PubMed] [Google Scholar]
- [OMI] Office of the Medical Inspector, Veterans Health Administration . VHA patient safety event registry: first nineteen months of reported cases: summary and analysis. Washington DC: VHA; 1999. [Google Scholar]
- Rubenstein L, Josephson K, Robbins A, et al. Falls in the nursing home. Ann Intern Med. 1994;121:442–51. doi: 10.7326/0003-4819-121-6-199409150-00009. [DOI] [PubMed] [Google Scholar]
- Rubenstein L, Powers C, MacLean C, et al. 2001Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders Ann Intern Med 135(8 Pt 2)686–93. [DOI] [PubMed] [Google Scholar]


