Abstract
Introduction:
Little is known about osteoporosis in institutionalized older adults. Risk factors such as low body mass index (BMI) have been investigated in female populations, but remain understudied in men. The objective of this study was to examine characteristics of older men residing in a nursing home who received bone mineral density evaluations.
Methods:
57 male Miami Veterans Affairs Medical Center (VAMC) nursing home residents were screened for osteoporosis using a peripheral dual X-ray (pDXA) technique. T-scores were categorized into three groups: normal (0>–1); osteopenic (−1 to −2.49); osteoporotic (<–2.5).
Results:
Average age was 76.2 years (standard deviation = 11.5; range: 48–100). T-scores indicated that 37.3% of the population was normal, 35.6% osteopenic, and 27.1% osteoporotic. 35.6% of patients had normal BMIs, 3.4% were underweight, 47.5% were overweight, and 13.6% were considered obese. There was a high prevalence of overweight and obese individuals (61.1%) in the osteopenic and osteoporotic groups.
Conclusion:
As expected, there was a high prevalence of low bone mass in our population (62%). However, overweight and obese men were more likely to have osteoporosis and osteopenia, contrary to literature and clinical knowledge. This finding may be partially explained by the prevalence of sedentary lifestyle and relative lack of weight-bearing activity in this group of men.
Keywords: osteoporosis, nursing home, aging, body mass index
Introduction
Osteoporosis and osteoporosis-related fractures are conventionally thought to be conditions of older women (Bilezikian 1999). However, osteoporosis and related fractures are also an important health issue of older men. One-third of hip fractures occur in men, and mortality from hip fractures tends to be greater among older men compared with women (Eastel et al 1998; Yeh et al 2002; Drake et al 2003; Finkelstein et al 2003). The near-exclusive focus on osteoporosis in women in the past has delayed progress in understanding male osteoporosis.
Despite the fact that current World Health Organization (WHO) criteria for the diagnosis of osteoporosis strictly apply to white postmenopausal women, these criteria are commonly applied to men as well. At present, there are no published guidelines for osteoporosis screening in older men, although written recommendations have been previously published (Campion et al 2003). Osteoporosis in women is routinely diagnosed by bone mineral density (BMD) testing, while men are often diagnosed only after a fracture occurs.
Most of the information about osteoporosis in the nursing home has been derived from case control and cohort studies involving risk factors for falls or hip fracture in skilled nursing facilities (Colon-Emeric et al 2003). The incidence of hip fractures in institutionalized elderly patients is significantly high, as the risk can be up to six times greater for skilled nursing facility residents compared with community-dwelling older adults (Colon-Emeric et al 2003). Most of the research using nursing home and/or institutionalized patients has been based on primarily female participants.
The Department of Veterans Affairs (VA) nursing homes are unique in that most residents are male. The purpose of this study was to investigate the prevalence of low bone mass (osteopenia or osteoporosis) in our elderly male VA nursing home population and whether treatment strategies were implemented in those with the disease. In addition, this study evaluated the frequency of reporting of osteoporosis, its comorbidities, and known risk factors.
Methods
Fifty-seven Miami VA Medical Center (VAMC) male nursing home residents were evaluated with a calcaneal peripheral X-ray (pDXA) technique (Lunar® Pixi Bone Densitometry, General Electric Healthcare Corporation, Fairfield, CT, USA) in February or March of 2000. Bone mineral density (gm/cm2) was ascertained, and T-scores were categorized into three groups: normal (0 >–1); osteopenic (−1 to −2.49); osteoporotic (<–2.5). The institutional review board at the Miami VAMC approved the retrospective review of these subjects’ medical records. Body mass index (BMI) was calculated using height and weight. BMI scores were classified as: normal (18.5–24.9); overweight (25–29.9); obese (30+); and underweight (<18.5). Patient age was categorized into four age groups (younger than 65, 65–74, 75–84, 85+). Additional characteristics were coded including history of dementia, depression, diabetes and other co-occurring illnesses; death since time of measurement; laboratory markers including albumin, calcium, and creatinine levels; treatment data including calcium replacement and vitamin D, bisphosphonate, and calcitonin use. Additional information on medication use including corticosteroids, heparin, and thyroid replacement was also collected. Chi-square analyses were conducted to compare characteristics of male nursing home residents by BMI rank, T-score classification, and death since measurement. All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) 10.0.
Outcomes
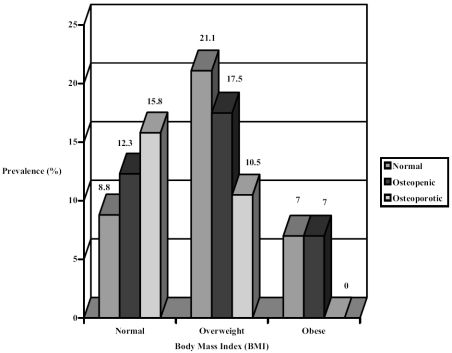
Table 1 illustrates descriptive findings of the sample. T-score rankings indicated that 37.3% of the population was normal, 35.6% osteopenic, and 27.1% osteoporotic. 94.7% of men with osteoporosis by pDXA did not have a clinical diagnosis of osteoporosis at the time of testing. Additionally, 57.1% of those found to have low bone mass were receiving calcium or vitamin D treatment at the time of testing. There were no significant differences in T-score classification or BMI rank by age or ethnicity. There was a high prevalence of overweight and obese individuals (61.1%) in the osteopenic and osteoporotic groups (Figure 1). 58% of male veterans in this cohort died in the four years post-measurement, and of these, 60% were osteopenic or osteoporotic. 71.4% of men who died since measurement had abnormally low albumin levels (p<0.03), but there were no significant differences in albumin level by BMI rank or T-score classification. There were no significant differences in T-score classification by ambulatory status. 18.9% of men had a history of an adult fracture, but no significant differences were found between history of fracture and T-score classification. Over half of our sample had a diagnosis of depression, and men with a diagnosis of depression were significantly more likely to have osteopenia or osteoporosis (p<0.04).
Table 1.
Demographic characteristics of 57 male nursing home residents
| Characteristic | N (%) |
|---|---|
| Age, mean (SD) | 76.2 (11.5) |
| Osteopenia or osteoporosis by age group | |
| 65–74 | 11 (30) |
| 75–84 | 14 (38) |
| ≥85 | 9 (24) |
| Ethnicity | |
| NLW | 37 (65) |
| Black | 12 (21) |
| Latino | 8 (14) |
| BMI rank | |
| Normal (18.5–24.9) | 20 (35) |
| Underweight (<18.5) | 2 (3.5) |
| Overweight (25–29.9) | 27 (47) |
| Obese (>30) | 8 (14) |
| T-score | |
| Normal (≥–1) | 22 (39) |
| Osteopenic (−1 to −2.49) | 19 (33) |
| Osteoporotic (≤–2.5) | 16 (28) |
| Ambulatory status | |
| Independent | 23 (40) |
| WCB | 25 (44) |
| Assistive device | 4 (7.0) |
| Depression diagnosis | |
| Yes | 28 (49) |
| Unable to screen | 16 (28) |
| Dementia diagnosis | 36 (63) |
| Osteoporosis diagnosis | 3 (5.3) |
| Death since measurement | 33 (58) |
Abbreviations: BMI, body mass index; NLW, non-Latino White; SD, standard deviation; WCB, wheelchair-bound.
Figure 1.
Comparison of BMI rank with T-score of 57 male nursing home residents.
Discussion
In our population of elderly male veterans residing in a nursing home care unit, more than half were either osteopenic or osteoporotic. Patients in our male nursing home sample who were identified to have osteopenia or osteoporosis were more likely to be overweight, have dementia, or suffer from depression. One-fifth of the residents were found to have a history of fracture, although there was no association between the fracture and BMI.
Previous reports have been consistent in demonstrating a direct correlation between increasing body weight and high bone mass or low fracture incidence (Turner et al 1998; Guthrie et al 2000; Bakhireva et al 2004). Various studies suggest that low BMI is related to decreased BMD. However, most of these studies were done in postmenopausal women and in community-dwelling older adults (Ravn et al 1999). Body weight is considered one the most powerful predictors of bone status, and adipose tissue plays a substantial role in weight-related protective effects on bone (Thomas 2003). Jagielska (1999) reported that restoration of weight resulted in increase in BMD in anorexic women; low bone mass is considered a common complication of anorexia nervosa. The relationship between increasing body mass and osteoporosis prevention is based on the theory of bone remodeling in which increased body weight causes mechanical stress on bone, which in turn stimulates bone remodeling and promotes bone mineralization. Also, the estrogen level in obese people tends to be higher, which is explained by increased aromatization of testosterone to estrogen in adipose tissue. Hence, an increased level of estradiol is strongly correlated with higher bone density in men (Orwoll 2003). Bioavailable estradiol level is now believed to be a determinant of bone mass and its action essential for normal bone development (Orwoll 2003). In a previous study it was found that the prevalence of osteopenia was higher in VA nursing home patients compared with age-matched and gender-matched community-dwelling counterparts (Nagraj et al 1990). A majority of these nursing home residents weighed less than their ideal body weight.
Obesity in nursing homes is prevalent, contradicting commonly held beliefs that nursing home residents are often underweight and suffer from malnutrition. Older people living in the community usually have significantly higher BMI than those elderly living in institutions (Sibai et al 2003). However, it is also of note that an increase in visceral fat and obesity is common among aging men as they undergo a progressive decrease in androgen production (Wespes and Schulman 2002), which may partially explain our findings.
BMI is a measure of thinness and adiposity. In our study, it was only BMI that was analyzed; body weight and other measures of body size (total weight, height, waist-hip ratio, lean mass, fat mass, percentage fat mass) were not examined. It has been shown in numerous studies that body weight is the most consistent marker of BMD overall among other measures of body size which include BMI (Edelstein and Barrett-Connor 1993; Adami et al 2004). It has been argued that BMI is more frequently associated with increased bone turnover and bone loss. while body weight is a more proximate determinant of the actual bone mass (Iqbal et al 1999; Adami et al 2004). The Epidemiological Study on the Prevalence of Osteoporosis (ESOPO) by Adami et al (2004) found that bone stiffness was positively related to body weight, height, and BMI, but in a multivariate analysis only weight was significantly correlated. In addition, among men, BMD seems to be related to fat-free soft-mass tissue (Coin et al 2000).
Limitations
The results of our study are inconsistent with current literature regarding the influence of body mass on BMD. This discrepancy may be attributed to a number of factors, including the limitations of our methodology, which included the arbitrary screening of willing and available nursing home residents for low bone mass and the subsequent retrospective review of their medical records. The study population was small and is not generalizable to community-based nursing home residents. VA nursing home residents are unique because they are typically male and mostly Caucasian. The corresponding rates of low bone density are higher than reported prevalence rates, and potential contributing factors to the high prevalence of abnormal bone density could not be analyzed due to the limitations of retrospective chart review methodology.
Additional findings of our study are not consistent with current literature. It is well known that a lower BMD translates to a higher fracture rate and is apparently a strong predictor of future fracture risk (Campion and Maricic 2003). Our study found no significant association between history of fracture and T-score classification, although it is difficult to extrapolate to this population due to the variability in ambulatory status. Other risk factors for osteoporosis-related fractures, including functional impairment, previous fractures, and environmental factors could not be analyzed in this study. While weight-bearing exercise may reduce fracture risk, we are not aware of the effect of immobilization on BMD value (Campion and Maricic 2003).
While our osteopenic and osteoporotic patients were more likely to have depression, causality cannot be established with our current methodology, and reports about its association are conflicting. In a cross-sectional study of 1566 Medicare enrollees, Robbins et al (2001) found a significant association between BMD and depressive symptoms, while another study by Whooley et al (2004) found no relation between depression and BMD in community-dwelling older men. The high prevalence of depression in institutionalized older adults may partially explain this finding. Future work will examine the possible relationship between osteoporosis and depressive symptomatology in this population. Currently, the literature shows an association between dementia and falls or hip fracture, but not directly with osteoporosis.
In summary, we found a high prevalence of osteopenia and osteoporosis among male nursing home residents who were more likely to be classified as overweight and obese according to BMI. The abnormal BMD was found to be independent of the ambulatory status and history of fracture among the subjects studied. Overall, osteoporosis is under-recognized and under-treated in this institutionalized population. Additional studies are needed to improve awareness of the risk factors for osteoporosis among institutionalized men in order to screen, diagnose, and treat osteoporosis properly and to prevent its complications.
Acknowledgments and disclosure
The authors would like to acknowledge Juancho Libiran, MD, Rebecca Perez, MD, Stephen Hanff, MD, and Silvina Levis, MD, for their assistance in the preparation of this manuscript. Dr Paniagua is supported in part by the Miami Veterans Affairs Medical Center GRECC and the Division of State, Community, and Public Health, Bureau of Health Professions (BHPr), Health Resources and Services Administration (HRSA), Department of Health and Human Services (DHHS), Geriatric Academic Career Award (1 K01 HP 00118-01). The information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, the BHPR, HRSA, DHHS, or the US Government.
References
- Adami S, Giannini S, Giorgino R, et al. Effect of age, weight and lifestyle factors on calcaneal quantitative ultrasound in premenopausal women: the ESOPO study. Calcif Tissue Int. 2004;74:317–21. doi: 10.1007/s00223-003-0036-2. [DOI] [PubMed] [Google Scholar]
- Bakhireva LN, Barrett-Connor E, Kritz-Silverstein D, et al. Modifiable predictors of bone loss in older men; a prospective study. Am J Prevent Med. 2004;26:436–42. doi: 10.1016/j.amepre.2004.02.013. [DOI] [PubMed] [Google Scholar]
- Bilezikian JP. Osteoporosis in men. J Bone Miner Res. 1999;4:3431–4. [Google Scholar]
- Campion JM, Maricic MJ. Osteoporosis in men. Am Fam Physician. 2003;67:1521–6. [PubMed] [Google Scholar]
- Coin A, Sergi G, Beninca P. Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos Int. 2000;11:1043–50. doi: 10.1007/s001980070026. [DOI] [PubMed] [Google Scholar]
- Colon-Emeric CS, Biggs DP, Schenck AP, et al. Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos Int. 2003;14:484–9. doi: 10.1007/s00198-003-1384-5. [DOI] [PubMed] [Google Scholar]
- Drake WM, Kendler DL, Rosen CJ, et al. An investigation of the predictors of bone mineral density and response to therapy with alendronate in osteoporotic men. J Clin Endoncrinol Metab. 2003;88:5765–9. doi: 10.1210/jc.2002-021654. [DOI] [PubMed] [Google Scholar]
- Eastel R, Boyle IT, Compton J, et al. Management of male osteoporosis: report of the UK Consensus Group. QJM. 1998;91:71–92. doi: 10.1093/qjmed/91.2.71. [DOI] [PubMed] [Google Scholar]
- Edelstein SL, Barrett-Connor E. Relationship between body size and bone mineral density in elderly men and women. Am J Epidemiol. 1993;138:160–9. doi: 10.1093/oxfordjournals.aje.a116842. [DOI] [PubMed] [Google Scholar]
- Finkelstein J, Hayes A, Hunzelman J, et al. The effects of parathyroid hormone, alendronate, or both in men with osteoporosis. New Engl J Med. 2003;349:1216–26. doi: 10.1056/NEJMoa035725. [DOI] [PubMed] [Google Scholar]
- Guthrie JR, Dennerstein L, Wark JD. Risk factors for osteoporosis. Medscape Womens Health. 2000;5:4. [PubMed] [Google Scholar]
- Iqbal F, Michaelson J, Thaler L, et al. Declining bone mass in men with chronic pulmonary disease. Chest. 1999;116:1616–24. doi: 10.1378/chest.116.6.1616. [DOI] [PubMed] [Google Scholar]
- Jagielska G. Osteoporosis in anorexia nervosa: a literature review. Psychiatr Pol. 1999;33:887–96. [PubMed] [Google Scholar]
- Nagraj HS, Gergans GA, Mattson DE, et al. Osteopenia in the men of a Veterans Administration nursing home. Am J Clin Nutr. 1990;51:100–6. doi: 10.1093/ajcn/51.1.100. [DOI] [PubMed] [Google Scholar]
- Orwoll ES. Men, bone and estrogen: unresolved issues. Osteoporos Int. 2003;14:93–8. doi: 10.1007/s00198-002-1332-9. [DOI] [PubMed] [Google Scholar]
- Ravn P, Cizza G, Bjarnason NH, et al. Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Early Postmenopausal Intervention Cohort (EPIC) study group. J Bone Miner Res. 1999;14:1622–7. doi: 10.1359/jbmr.1999.14.9.1622. [DOI] [PubMed] [Google Scholar]
- Robbins J, Hirsch C, Whitmer R, et al. The association of bone mineral density and depression in an older population. J Am Geriatr Soc. 2001;49:732–6. doi: 10.1046/j.1532-5415.2001.49149.x. [DOI] [PubMed] [Google Scholar]
- Sibai A, Zard C, Adra N, et al. Variations in nutritional status of elderly men and women according to place of residence. Gerontology. 2003;49:215–24. doi: 10.1159/000070401. [DOI] [PubMed] [Google Scholar]
- Thomas T. Leptin: a potential mediator for protective effects of fat mass on bone tissue. Joint Bone Spine. 2003;70:18–21. doi: 10.1016/s1297-319x(02)00005-2. [DOI] [PubMed] [Google Scholar]
- Turner LW, Wang MQ, Qiang F, et al. Risk factors for hip fracture among southern older women. South Med J. 1998;91:4338–48. doi: 10.1097/00007611-199806000-00005. [DOI] [PubMed] [Google Scholar]
- Wespes E, Schulman CC. Male andropause: myth, reality, and treatment. Int J Impot Res. 2002;4(Suppl 1):S93–8. doi: 10.1038/sj.ijir.3900798. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Cauley JA, Zmuda JM, et al. Depressive symptoms and bone mineral density in older men. J Geriatr Psychiatry Neurol. 2004;17:88–92. doi: 10.1177/0891988704264537. [DOI] [PubMed] [Google Scholar]
- Yeh S, Phanumas S, Hafner D, et al. Risk factors for osteoporosis in a subgroup of elderly men in a Veterans Administration nursing home. J Invest Med. 2002;50:452–7. doi: 10.1136/jim-50-06-05. [DOI] [PubMed] [Google Scholar]