Abstract
Objective:
Many patients present to their physician with depression as their primary symptom. However, depression may mask other comorbid disorders. This article presents diagnostic criteria and treatment recommendations (and monitoring) pertaining to the diagnosis of adult attention deficit hyperactivity disorder (ADHD), which may be missed in patients who present with depressive symptoms, or major depressive disorder (MDD). Other co-occurring conditions such as anxiety, substance use, and bipolar disorder are briefly discussed.
Methods:
A panel of psychiatrist-clinicians with expertise in the area of child and adolescent ADHD and mood disorders, adult mood disorders, and adult ADHD was convened. A literature search for recommendations on the diagnosis and treatment of co-occurring conditions (MDD, anxiety symptoms, and substance use) with adult ADHD was performed. Based on this, and the panel’s clinical expertise, the authors developed a diagnostic algorithm and recommendations for the treatment of adult ADHD with co-occurring MDD.
Results:
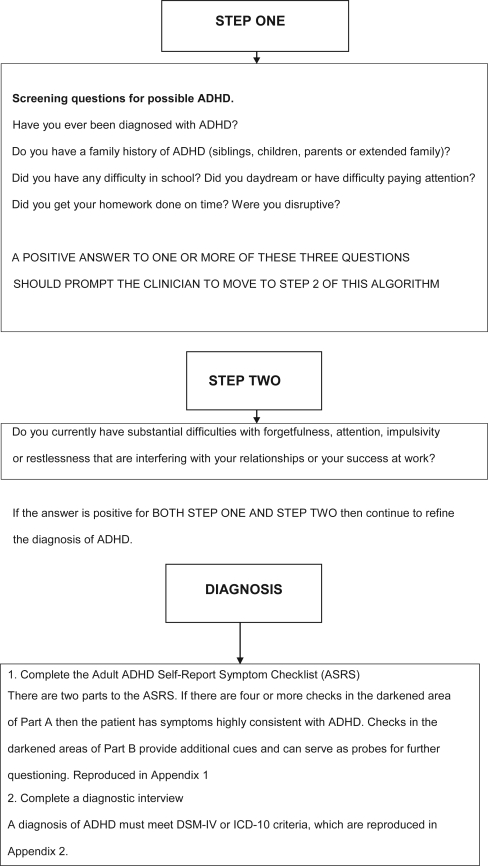
Little information exists to assist clinicians in diagnosing ADHD co-occurring with other disorders such as MDD. A three-step process was developed by the panel to aid in the screening and diagnosis of adult ADHD. In addition, comorbid MDD, bipolar disorder, anxiety symptoms, substance use and cardiovascular concerns regarding stimulant use are discussed.
Conclusion:
This article provides clinicians with a clinically relevant overview of the literature on comorbid ADHD and depression and offers a clinically useful diagnostic algorithm and treatment suggestions.
Keywords: ADHD, adult, treatment, diagnosis, substance use disorder, depression
Introduction
Attention deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder of childhood associated with substantial cognitive, family, social, behavioral, and academic impairment. ADHD in childhood occurs in an estimated 3%–7% of school-aged children.1–4 The National Comorbidity Survey Replication Study found 36% of adults who met the criteria for ADHD as children continued to meet the diagnostic criteria as adults.5–7 The overall prevalence of adults who meet the diagnosis of ADHD was 4.4%.8 The Cross National Prevalence study estimated an average adult ADHD prevalence of 3.4% with lower income countries reporting a lower prevalence (1.9%) than higher income countries (4.2%). The survey states few cases are treated for ADHD but in many cases treatment is given for comorbid disorders.9
Many clinicians are familiar with making a diagnosis of ADHD in young people but find that making a diagnosis of ADHD in adults presents challenges. First, the Diagnostic and Statistical Manual (DSM) requirement of onset prior to age seven relies on the memory of the informant and retrospective accounts of symptoms are notoriously inaccurate.10,11 In addition, the ancillary information such as school reports that is helpful in diagnosing childhood ADHD is frequently not available for adults.
Furthermore, the presentation of ADHD in adults may be obfuscated by outcomes of the chronic illness such as demoralization and substance misuse.12–16 Finally, adults often underreport their symptoms. This might be due to the lifelong presence of the symptoms, which are now considered part of their personal style rather than abnormal or due to the adaptations they have made to accommodate their symptoms, such as careful job selection.
Clinicians who treat children with ADHD do not usually follow their patients into adulthood, and those who treat adults are not always familiar with the diagnosis or usual management.4 Hence, in the opinion of the panel, clinicians treating adults might assume affected individuals have, by adulthood, grown out of the disorder. The panel also suggested clinicians treating adults may be more familiar with mood and anxiety symptoms. As a result, they may tend to make a mood or anxiety disorder diagnosis rather than attribute the presenting symptoms to ADHD. Some adult patients present with self-identified ADHD, and this may arouse suspicion among clinicians concerned these patients are either malingering or susceptible to media influence.4 Clinicians may also be concerned that patients are seeking treatment as a way to obtain medications they can misuse or abuse. Although some clinicians have challenged the validity of the diagnosis, the evidence supports the existence of adult ADHD.5–8 Until recently, adult ADHD was not included in medical school curricula or in postgraduate medical training and many health providers are therefore unfamiliar with the diagnosis and management of adult ADHD, in particular when it occurs in conjunction with psychiatric disorders such as major depressive disorder (MDD).
This article reviews the available literature pertaining to the diagnosis of adult ADHD and recommends diagnostic criteria and treatment guidelines based on consensus by the panel. In addition, comorbid depression, bipolar disorder, anxiety symptoms, substance use, and cardiovascular concerns regarding stimulant use are discussed with a view to providing consensus guidance on how to manage these patients.
Methods
In 2007, the Canadian Psychiatric Association’s (CPA) needs assessment identified ADHD as an area warranting professional attention. In partnership with the CPA, the Office of Continuing Medical Education and Professional Development (CME and PD) at the University of Calgary, and Partners In Psychiatry sent survey invitations to psychiatrists and family practitioners. In all, 517 Canadian physicians responded to the survey. Results indicate family physicians and psychiatrists have a desire for more knowledge regarding ADHD including adult ADHD and comorbidities.
In response, a group of Canadian psychiatrists with clinical experience in the diagnosis and treatment of adult ADHD, adult MDD and childhood ADHD/MDD were invited by Janssen-Ortho Inc., to address the issue of diagnosis and management of adult ADHD co-occurring with Major Depressive Disorder and provide some guidance for other key psychiatric illnesses (eg, anxiety disorder, substance use, bipolar disorder). Members of the panel identified the clinically relevant diagnostic and treatment issues and critically reviewed the available literature. The panel synthesized relevant information obtained from the literature review and reached consensus on clinically relevant information arising from the review. The panel, via teleconference or email, discussed areas of disagreement until consensus was reached. A “first draft” of an academic paper was developed by a professional writer from the consensus discussion and the literature and was reviewed by all panel members, followed by revisions and a final consensus on the manuscript by all members of the panel. Janssen Ortho Inc. employees observed the first expert panel meeting, reviewed the literature and gave input into the article.
Literature review
A search of the literature was performed in March 2008 and repeated in August 2008. The databases EmBase, Medline, and Psychinfo were searched over the period of 1990–2008; keywords: ADHD adult, depression, comorbid, bipolar disorder and ADHD, ADHD and substance use, ADHD and depressive disorder differentiation.
Key learning issue #1: ADHD persists into adulthood
Historical teachings that ADHD rarely persists into adulthood are not supported by the research data. A longitudinal study of 85 children with ADHD found that 4% continued to meet diagnostic criteria for ADHD as adults.17 Another study of 104 boys with ADHD found that 11% had disabling ADHD in adulthood.17,18 Other studies have reported that 60% of children with ADHD will exhibit sub-clinical symptoms of ADHD4,6,19–22 in adulthood. ADHD is best understood as a childhood-onset neurodevelopmental disorder that may persist into adulthood.19
Adult ADHD prevalence estimates vary from 1%–6% depending on the populations studied (community versus clinic), the edition of Diagnostic and Statistical Manual (DSM) used, and whether the assessment was based on self or observer report. As well, differing definitions of persistence were employed. Persistence may be defined as continuing to meet the full DSM criteria, or continuing to experience functional impairment due to the ADHD symptoms.8,19,22,23 The most recent estimate of the prevalence of adult ADHD from the National Comorbidity Survey Replication (USA) was 4.4%.8
Many adults living with ADHD were not diagnosed or effectively treated as children.2,13,24 Early clinical work on adult ADHD was driven by self-referrals of adults who had symptoms of restlessness, impulsivity, and difficulty concentrating as well as psychosocial disability, as demonstrated by lower socioeconomic status or shorter job tenure.4,25 These adults met criteria for childhood onset ADHD but had never received this diagnosis.
The DSM-IV-TR ADHD symptoms of inattention in children include “often has difficulty sustaining attention in tasks or play activities; often seems not to be listening when spoken to directly; often does not follow through on instructions; often has difficulty organizing tasks and activities; often loses things necessary for tasks or activities; often is distracted easily by extraneous stimuli and is often forgetful in daily activities.” Symptoms of inattention in adults with ADHD include difficulty sustaining attention when reading or doing paperwork; distractibility and forgetfulness; poor concentration; poor time management; difficulty finishing tasks; and misplacing things.26
A similar migration occurs with hyperactive symptoms as a child with ADHD transitions into adulthood. The DSM-IV-TR symptoms of hyperactivity in children include “often fidgets with hands or feet or squirms in seat; often runs about or climbs excessively in situations in which it is inappropriate; often has difficulty playing or engaging in leisure activities quietly; often ‘on the go’ or often acts as if ‘driven by a motor’; and often talks excessively.”
In adults, symptoms of hyperactivity can present as feelings of restlessness or of being overwhelmed; choosing active jobs that require a lot of energy; working at multiple jobs; and talking excessively.26
As for impulsivity, childhood symptoms that present as “often blurts out answers before questions have been completed; often has difficulty awaiting turn; and often interrupts or intrudes on others (in conversation, in games)”, shift in adults and present as changing jobs impulsively; driving too fast; being involved in traffic accidents; irritability; and being quick to anger.
Studies have since shown that childhood ADHD, if not effectively treated, increases the short- and long-term risk for many negative personal, social, family, vocational and health outcomes. These include cognitive difficulties (eg, inattention, disinhibition, slowed reaction time) which are associated with both ADHD and depression, interpersonal problems, school failure, failure to graduate,27–31 substance misuse/abuse,13,24 legal difficulties, automobile accidents, workplace accidents, unemployment or underemployment,13,24,28 lower socioeconomic status, family and marital difficulties,29,32 low self esteem, demoralization, and comorbid MDD.33–36 Biederman and colleagues found an increased incidence of alcohol (27%) and drug (18%) dependency compared to controls (13% and 6%, p < 0.01 and p < 0.001, respectively) and statistically significant rates of separation and divorce in adults with untreated ADHD (28%) compared to controls (15%, p < 0.01).37
Key learning issue #2: ADHD and heritability
ADHD is highly heritable. Twin studies show the heritability of ADHD to be 0.80, indicating a substantial genetic effect, almost as high as that of schizophrenia (Table 1).38
Table 1.
Heritability of psychiatric disorders, respiratory disorders, and cancers
| Heritability | Reference | |
|---|---|---|
| ADHD | 0.80 | Faraone 200036 |
| Schizophrenia | 0.83–0.87 | Cardno et al 199981 |
| Asthma | 0.38 | Palmer et al 200182 |
| Prostate cancer | 0.42 | Palmer et al 200182 |
| Colorectal cancer | 0.35 | Palmer et al 200182 |
| Breast cancer | 0.27 | Palmer et al 200182 |
Abbreviation: ADHD, adult attention deficit hyperactivity disorder.
There is some evidence that heritability is greater for ADHD that persists into young adulthood than for ADHD that remits in adolescence.38–40 A prospective four-year follow-up of ADHD diagnosed boys assessed in mid-adolescence found that of those with persistent ADHD, the parental prevalence was 16.5% compared to 10.8% in those who had remitted. Similar results have been reported for ADHD in siblings.38
Children of parents with ADHD have up to a sevenfold increase in their risk for developing ADHD compared with children of non-ADHD parents.41 Although no single gene has been implicated in determining the expression of ADHD, recent studies have explored the effects of genes involved in the activities of dopamine receptors and transporter systems.6,12–16,41
Key learning issue #3: ADHD and comorbid depression
The literature search found strong evidence for the comorbidity of depression and ADHD but little in the way of tools to differentially diagnose and treat the disorders.6,7,34,36,42–48 Comorbid depression occurs frequently in adult ADHD (see Table 2). According to the National Comorbidity Survey Replication study,8 the prevalence of MDD in adults with ADHD was 18.6% (SE 4.2) compared to 7.8% (SE 0.4) in non-ADHD respondents (OR 2.7). A more impressive, albeit less frequent, relationship was found for dysthymia (12.8% vs 1.9%, OR 7.5). Other investigators have reported similar results.5–7,24 The converse is also true. ADHD is found frequently in adult probands with depressive disorders. Reported rates range from 9%–16%.6,7,36,46
Table 2.
Prevalence of depression comorbid with ADHD
| Reference | Prevalence of depression with ADHD |
|---|---|
| Biederman et al 200855 | 40.7% |
| Able et al 200721 | 31.0% |
| Kessler et al 20068 | 18.6% |
| Sobanski 200612 | 30%–50%a |
| Torgersen et al 200633 | 9% (Lifetime prevalence of 53%) |
| Fischer et al 200642 | 26% |
Note: aOne or more past episodes of depression.
Abbreviation: ADHD, adult attention deficit hyperactivity disorder.
When ADHD and a depressive disorder present concurrently, individuals have been noted to be at a numerically greater risk (vs ADHD alone) for poorer long-term outcome (ie, negative social and vocational outcomes)49 and a higher numerical risk of suicide in children and adolescents.50,51 There is a greater cost to society and individuals when ADHD occurs concurrently with depression.52–54 For example, patients with ADHD comorbid with another psychiatric disorder have been found to be more often unemployed than patients with ADHD alone, 34.5% versus 6.7%, respectively, although this was not a statistically significant finding possibly due to a small sample size.48 Biederman and colleagues recently published an article that followed 123 young females with ADHD and 122 female controls for five years into adolescence/early adulthood. 40.7% of females with ADHD at baseline had MDD with moderate to severe impairment while only 11% of the controls had MDD. At the five-year follow-up time point, 65% (80/123) of females with ADHD had MDD compared to 20.5% of controls. Even after adjustment for comorbid conditions, the relationship between ADHD and MDD was still significant (95% confidence interval 1.5–4.2; p < 0.01).55
Few studies have directly addressed the functional consequences for adults with comorbid ADHD and depression. This is unsurprising considering it is only recently that ADHD has been considered a valid diagnosis for adults and work elucidating the relationships between ADHD and other psychiatric disorders is in its early stages. Studies in the pediatric setting have found that depressed children with ADHD were significantly less socially competent than children with ADHD who were not depressed or community controls.56 Other earlier research conducted in young people suggests that the combination of affective and attention deficit disorders may increase the risk for completed suicide,57 increased suicidality,55 lead to poorer academic outcomes58 and psychiatric hospitalization.55
Clinically, it is necessary to consider the possibility of comorbid depression in individuals diagnosed with ADHD and vice versa. However, it is important to carefully differentiate between the presence of a depressive syndrome and the presence of depressive symptoms that may arise secondarily to the demoralization or other negative emotional effects experienced by individuals as a consequence of ADHD.58–61 This distinction has important therapeutic considerations. ADHD-associated demoralization may be most parsimoniously treated with interventions primarily focused on addressing ADHD symptoms while treatment of a comorbid depressive disorder may require interventions for both disorders concurrently.60 The presence of concentration and memory problems, restlessness, irritability, anhedonia, and chronic difficulty getting and staying asleep may mimic depression. The panel concluded that it is not typical for ADHD in the absence of a mood disorder to be associated with a fixed, depressed affect or suicidal thoughts. The majority of patients with ADHD maintain mood stability despite the social and occupational difficulties inherent to the disorder.
In summary, the onset of ADHD is pre-pubertal and persists into adulthood with up to 60% of those adults initially diagnosed with ADHD as children reporting clinically significant symptoms of ADHD in adulthood. In the view of the panel, individuals who suffer from ADHD may not have been identified or effectively treated in childhood and may present for the first time to mental health care providers as adults, perhaps with complaints of depression or anxiety. In many of these individuals, their clinical presentation may be confounded by the secondary consequences of undiagnosed and untreated ADHD.
ADHD is heritable.38–40 The clinician should discuss the hereditary nature of ADHD and in the opinion of the panel; it is recommended that parents and/or children of the patient be screened for ADHD. Furthermore, although substantive data on this issue are not currently available, the panel concurs that effective treatment of parental ADHD may be expected to improve outcomes in the treatment of their children with ADHD.
Lastly, depression co-occurs with adult ADHD in 9%–50% of cases and complicates the assessment and management of the patient.8,14,24,34,45
Diagnosing and treating ADHD comorbidity with depression assessment
There is limited information in the literature to help guide the clinician in assessing patients with comorbid conditions for ADHD and recommendations are made based on the panel’s clinical experience. The panel recommends, as part of a new patient interview, a general screen for the assessment of possible ADHD, even when there are other psychiatric presentations. The quick screen includes three questions:
Have you ever been diagnosed with ADHD?
Do you have a family history of ADHD?
Did you have any difficulty in school?
Patients who screen positive for a previous diagnosis of ADHD, a family history of ADHD or reports of school difficulties characterized by behavioral or learning problems should undergo a more comprehensive review of current ADHD symptoms. This review should cover the three components of the ADHD spectrum:
Inattention.
Hyperactivity.
Impulsivity.
If symptoms are described, a more detailed review of the syndromal components of ADHD should follow. In addition, patients should be evaluated for the presence of functional impairment arising from these symptoms. As many clinicians have had limited training in the assessment and diagnosis of ADHD, the use of a validated screening aid such as the Adult Symptom Rating Scale (ASRS) (see http://www.med.nyu.edu/psych/psychiatrist/adhd.html)62 may be useful. The ASRS may be used as part of the clinical interview or it can be completed at home after the interview, with corroboration from a parent, spouse, or close friend. In addition to its utility as a screening aid, the ASRS can also provide a useful baseline measure of symptom severity. The ASRS has not been validated as an evaluation tool to monitor symptom change, however, because the questions closely map the 18 items of the DSM-IV criteria, the panel suggests that the ASRS can be repeated during treatment to evaluate the outcome of an intervention.
The panel has developed an algorithm (Figure 1) to assist physicians in their diagnostic evaluation of any patient suspected of having ADHD, including patients with comorbidities like depression. Screening questions including mood, anxiety, psychotic and personality pathology are an essential part of any psychiatric interview. Likewise, a review of past and current medical history is important to rule out the impact of medical illness in the development or maintenance of any psychiatric disorder.
Figure 1.
Screening assessment.
Panel recomendations on treatment
Psychostimulants (such as methylphenidate and amphetamine salts) and atomoxetine have been approved for the treatment of pediatric and adult ADHD in the United States and Canada. No pharmacological treatment for adult ADHD has been approved in the European Union (except for Ritalin LA in Norway). The antidepressants recommended for the treatment of major depression in this article are also approved for use in the United States, Canada and other countries. There are no antidepressants specifically indicated for MDD comorbid with ADHD.
ADHD treatment guidelines have focused primarily on pediatrics. Guidelines regarding the treatment of adult ADHD have appeared in the literature and online,63–65 however with limited information regarding practical pharmacotherapy treatment guidelines for co-occurring depression and ADHD.66–70
This article focuses on pharmacotherapy; however, Weiss and colleagues conducted a literature search for empirical studies of psychological treatment for adults with ADHD. Their search revealed five empirical, short-term studies, which demonstrated, moderate to large effect sizes. However, there were inconsistencies in selection of control groups and measures of outcomes.71
ADHD with comorbid depression
The panel recommends clinicians use the guiding principle of treating the most severe or functionally impairing condition first. If moderate-severe MDD is the most pressing clinical issue, then treatment for depression should be initiated first. Clinicians may follow relevant clinical practice guidelines (in Canada, these would be CANMAT guidelines, see http://www.canmat.org).72 There has been increased focus by regulatory bodies on the risk of suicide in children and adolescents and patients should be monitored for indicators of potential suicidal ideation. Treatment of the depression may result in amelioration of the symptoms of frustration, anxiety, or irritability. Some cognitive symptoms such as concentration may also be improved with antidepressant treatment. Once the depression has improved, the patient should be re-evaluated for symptoms of ADHD and if necessary treatment for ADHD should be initiated. In the course of treating the depression, if a patient does not respond adequately to an antidepressant medication, consideration should be given to re-evaluating both the depression and ADHD diagnosis and, if appropriate, initiating ADHD treatment. Treatment goals must be established in collaboration with the patient and should include improving both symptoms and psychosocial functioning.
Combining medications used to treat depression and ADHD may result in drug-drug interactions of a pharmacodynamic nature (ie, the medication’s effect on the body as evinced by competition for receptor binding) or pharmacokinetic nature (ie, the body’s effect on the medication as evinced by fatty foods slowing absorption of medications leading to higher plasma levels), although this is infrequent and there are no absolute contraindications except co-administration of psychostimulants or atomoxetine with monoamine oxidase inhibitors. A careful review of co-administered medications for potential drug–drug interactions is strongly advised. There is insufficient data available to determine the best combination of antidepressant and ADHD treatment.70 The choice of treatment should be guided by clinical experience, knowledge of the pharmacokinetics of the various treatment options and other practical issues. Any of the ADHD agents may have behavioral side effects;73 hence there is a need to monitor the patient’s depressive state. Psychostimulants have been used as an augmentation strategy for treatment-resistant depression though with limited evidence for success.74,75
The panel recommends if ADHD is the primary disabling condition and associated with mild depression, the ADHD should be treated first. As mentioned previously, ADHD is often accompanied by distress, demoralization or mild depressive symptoms. These depressive symptoms may improve with ADHD treatment alone. The panel recommends a long acting psychostimulant as first-line treatment for ADHD that is accompanied by distress, demoralization or mild depressive symptoms. The choice of agent should also be influenced by patient preference and risk profile. Once the patient has been initiated on ADHD treatment, the depressive features should be reassessed at subsequent visits to determine if treatment for depression is warranted.
If both depression and ADHD are deemed equally clinically relevant and functionally impairing the treatments may be initiated at close proximity. However, starting two treatments simultaneously should be avoided if possible because if there are tolerability or efficacy issues, it will be difficult to determine which agent is responsible.
Additional diagnostic and treatment challenges
ADHD, anxiety symptoms, and anxiety disorders
An anxiety disorder (eg, obsessive compulsive disorder [OCD], post-traumatic stress disorder [PTSD], panic disorder [PD], generalized anxiety disorder [GAD]) and ADHD may co-occur and, in the opinion of the panel the same rules apply here as for major depression: the most severe or functionally impairing condition should be treated first. However, patients with depression co-occurring with ADHD may present with anxiety symptoms that do not meet the criteria for an anxiety disorder. Using simple screening questions for anxiety disorders when anxiety symptoms are present is necessary to determine how to properly manage these patients. Similar to depression, many patients with an anxiety disorder have difficulty with concentrating, memory, restlessness, and irritability, which are not associated with an underlying attention deficit disorder. Some clues that the attention issue is paramount include the presence of symptoms less likely to be associated with anxiety such as stimulus-seeking behavior, disinhibition, or difficulty with time management.
Bipolar spectrum disorder
Bipolar disorder may occur comorbidly with ADHD, and has been reported to have an incidence of approximately 20% in adults with ADHD.8 Due to this possible relationship, patients with bipolar disorder should be screened for the possible presence of ADHD. This should be conducted during an euthymic phase as many symptoms of hypomania/mania also occur in ADHD. Any patient who experiences acute symptoms typical of mania or hypomania (eg, decreased need for sleep, increased energy, markedly inappropriate or erratic behavior, irritability, grandiosity, or psychotic symptoms) should be considered bipolar until proven otherwise. ADHD shares several of these symptoms, but is a chronic disorder unlikely to present with acute exacerbations and mood states are congruent.
ADHD treatment and risk of substance use
Clinicians are often concerned that treating individuals with psychostimulants leads to substance misuse, abuse or diversion. The National Comorbidity Survey Replication study reports a 12-month incidence of comorbidity with substance use disorder of between 9.5% and 25.4%.8 Conversely, 15%–25% of adults with substance use disorders present with ADHD.76 Although not all studies have shown the same results, the weight of information suggests that the risk of substance use disorders developing among individuals prescribed psychostimulant medication for ADHD is reduced,77 with some evidence that the treatment of ADHD may itself reduce the long-term risk for development of substance abuse disorders. A recent study suggested there was no protective effect associated with the treatment of ADHD; however patients treated with psychostimulants were no more likely to abuse substances than non-ADHD controls when they reached young adulthood.78
For patients with a history of substance abuse or dependence, the panel advises the use of short-acting stimulants should be avoided due to the possibility of misuse or diversion. Long-acting stimulants are effective and relatively well tolerated for this patient population. Diversion does not appear to be an issue with atomoxetine. However, its onset of action is longer than the long-acting stimulants. If a patient exhibits comorbid substance abuse, then appropriate psychosocial substance abuse interventions should be implemented together with treatments for ADHD. Some patients actively abusing substances may present with attention, behavior and self-control problems that mimic ADHD. Depending on the nature and acuity of the substance abuse, the diagnosis of ADHD should be deferred until the substance abuse problems have stabilized, even with a positive childhood history.
Panel recommendations for treatment and monitoring
It is important to educate patients about the expected onset of treatment effects and the duration of treatment. The choice of medication for ADHD and depression is based on many factors including the patient’s informed choice, time of day when the impairment is most problematic, risk of substance abuse, the presence of other comorbid disorders, medication tolerability, history or likelihood of compliance, and cost. For optimal clinical management the panel suggests that it may take 7–10 days (sometimes sooner) to titrate to the appropriate dose of a psychostimulant to achieve maximal symptomatic improvement.79,80 Onset of response with atomoxetine may occur as early as two weeks; however, as noted in two identical 10 week studies, longer periods of time after obtaining the maximal dose appear to be required to obtain optimal response.81
At every treatment point, patients should be systematically evaluated regarding their symptoms of both ADHD and depression, including a review of side effects and psychosocial functioning. Patient administered scales, which are helpful for both diagnosis and for monitoring response to treatment include the ASRS for ADHD and the Patient Health Questionnaire-9 (PHQ-9) (see http://www.depressionprimarycare.org/clinicians/toolkits/materials/forms/phq9/) for depression. The panel recommends monitoring of pulse and blood pressure at initiation of treatment, at dose changes and periodically, at regular intervals, thereafter. The introduction of medication will usually lead to symptom improvement, but symptomatic remission along with functional recovery is an endpoint that usually requires both medication and psychosocial interventions. It is unlikely that either ADHD or depression will remit if both disorders are not considered in the treatment plan.
Absence of improvement of ADHD
If there has been no substantial improvement in ADHD symptoms after at least two weeks at the maximal tolerable dose of the first medication, a trial of an agent from another class is warranted (eg, methylphenidate switched to mixed amphetamine salts or vice versa), or to a medication outside the psychostimulant class (eg, atomoxetine). If a second trial does not significantly alleviate symptoms, reevaluation of the diagnosis and potential comorbidities should be completed. If the ADHD diagnosis is confirmed and no untreated comorbid conditions are evident, consultation with an ADHD treatment specialist, if available, should be sought.
Adults with ADHD should be encouraged to address elements in their life that may contribute to improved treatment outcomes. These include decreasing the consumption of caffeine-containing beverages (eg, coffee, tea, colas, etc); improve sleep hygiene (regular bedtime, stimulus decreasing activities prior to bed, quiet and cool sleeping environment); and daily exercise or relaxation activities.
Cardiovascular concerns about stimulant use in adults
The American Heart Association and the American Academy of Pediatrics have recently clarified a clinical concern regarding cardiac risk and need for cardiac evaluation with respect to prescribing medication for ADHD.82 The associations both agreed that medications used to treat ADHD have not been shown to cause heart conditions nor have they been demonstrated to cause sudden cardiac death. However, some of these medications can “increase or decrease heart rate and blood pressure” although this is not usually considered to be dangerous.
The joint advisory also clarified the AHA/AAP position on the necessity of ordering ECGs before treating ADHD. The advisory read that it is, “… prudent to carefully assess children for heart conditions who need to receive treatment with drugs for ADHD.” As well, they recommended obtaining a patient and family health history and conducting a physical exam focused on cardiovascular disease risk factors before treatment with medications for ADHD. The joint statement said that acquiring an electrocardiogram (ECG) should be at the physician’s judgment, and it is not mandatory to obtain one. The statement went on to suggest that, “… treatment of ADHD should not be withheld because an ECG is not done.”82 While these recommendations were made with respect to children, it is the opinion of the panel that the same should hold true for adults being treated with ADHD medication (ie, treatment should not be withheld in the absence of an ECG). Central nervous system stimulant medications should be used with caution in adults with pre-existing cardiovascular or cerebrovascular conditions and should not be used in symptomatic cardiovascular disease or in people with known structural abnormalities.83 The recommendations above are applicable to stimulants and nonstimulant treatments for ADHD, including atomoxetine.
The panel recommends that if after having conducted the AHA recommended investigations, the physician is uncomfortable with prescribing treatment for ADHD due to possible cardiac risk: a referral to a cardiologist is warranted. Treatment should not be avoided due to potential risk, but may be delayed until a cardiology opinion is obtained. It is the panel’s opinion that heart rate and blood pressure should be assessed before treatment commences, following each dose change, and as clinically indicated.
Summary
Although not well appreciated by many clinicians, adult ADHD is a complex and relatively common psychiatric disorder that has substantial impact on social, personal, and vocational functioning and wellness.13,24,28–31 ADHD frequently may present comorbidly with depressive disorders, which worsens the morbidity of both disorders.6,7,34,36,42–47 Individuals with comorbid ADHD and depression should have both disorders identified, diagnosed and treated to optimize outcomes. To summarize, the panel recommends a general screen for adult ADHD for all new patients presenting in a physician’s office. Symptoms of adult ADHD may overlap those of affective disorders or be “hidden” by the more severe condition. Tests for ADHD and MDD are tools that may improve diagnostic consideration of these conditions and may also be used to evaluate symptom improvement if indicated. Clinically, the first intervention is to treat the condition with the greatest impact on patient function. If the patient presents with suicidal ideation, then an assessment for MDD should occur and if MDD is confirmed, treatment should begin. If the patient presents with deficits in function due to the inability to concentrate at work, complete tasks, or forgetfulness as the most severe presenting condition in addition to a mild depression, and the diagnostic assessment leads to adult ADHD, then the ADHD should be treated first.
Some patients may present with attention, behavioral and self-control problems that mimic ADHD but are due to actively abusing substances. Depending on the nature and acuity of the substance abuse, the diagnosis and treatment of ADHD should be deferred until the substance abuse problems have stabilized.
Conclusion
This article provides clinicians with a clinically relevant overview of the literature pertaining to comorbid ADHD and depression and offers a clinically useful diagnostic algorithm and treatment suggestions. Appropriate diagnosis and application of effective treatments, in the opinion of the panel can be expected to substantially improve both short- and long-term outcomes for patients with comorbid ADHD and depression. Further research is needed to clarify what are the best tolerated and effective medication combinations for comorbid depression and ADHD.
Acknowledgments
Janssen-Ortho Inc. funded the first expert meeting. The authors did not receive payment for writing this article. Dr D McIntosh reports having received lecture and consulting fees from: Janssen-Ortho Inc., Astra Zeneca, Lilly, NovoNordisc, GlaxoSmithKline, Lundbeck, Servier, SanofiAventis, and Shire. Dr S Kutcher reports having received lecture and consulting fees from Janssen-Ortho Inc. and is a faculty member at the Lundbeck Institute. Dr A Levitt reports having received lecture and consulting fees from: Janssen-Ortho Inc., Eli Lilly, and Pfizer. Dr M Rosenbluth reports having received lecture and consulting fees from: Janssen-Ortho Inc, Astra Zeneca, Lilly, GlaxoSmithKline, Lundbeck, Wyeth, Biovail, Organon, and Pfizer. Dr A Fallu reports having received lecture and consulting fees from: Janssen-Ortho Inc, Shire, Eli Lilly, and Lundbeck. C Binder is an employee of Janssen-Ortho Inc. The authors thank Marian P. Smith for assisting with reference searches and medical writing.
Appendix 1
Adult ADHD Self-Report Scale (ASRS-v1.1) symptom checklist instructions
The questions on the back page are designed to stimulate dialogue between you and your patients and to help confirm if they may be suffering from the symptoms of attention-deficit/hyperactivity disorder (ADHD).
Description: The symptom checklist is an instrument consisting of the eighteen DSM-IV-TR criteria. Six of the eighteen questions were found to be the most predictive of symptoms consistent with ADHD. These six questions are the basis for the ASRS v1.1 Screener and are also Part A of the symptom checklist. Part B of the symptom checklist contains the remaining twelve questions.
Instructions
Symptoms
Ask the patient to complete both Part A and Part B of the symptom checklist by marking an X in the box that most closely represents the frequency of occurrence of each of the symptoms.
Score Part A. If four or more marks appear in the darkly shaded boxes within Part A then the patient has symptoms highly consistent with ADHD in adults and further investigation is warranted.
The frequency scores on Part B provide additional cues and can serve as further probes into the patient’s symptoms. Pay particular attention to marks appearing in the dark shaded boxes. The frequency-based response is more sensitive with certain questions. No total score or diagnostic likelihood is utilized for the twelve questions. It has been found that the six questions in Part A are the most predictive of the disorder and are best for use as a screening instrument.
Impairments
Review the entire symptom checklist with your patients and evaluate the level of impairment associated with the symptom.
Consider work/school, social and family settings.
Symptom frequency is often associated with symptom severity, therefore the symptom checklist may also aid in the assessment of impairments. If your patients have frequent symptoms, you may want to ask them to describe how these problems have affected the ability to work, take care of things at home, or get along with other people such as their spouse/significant other.
History
Assess the presence of these symptoms or similar symptoms in childhood. Adults who have ADHD need not have been formally diagnosed in childhood. In evaluating a patient’s history, look for evidence of early-appearing and long-standing problems with attention or self-control. Some significant symptoms should have been present in childhood, but full symptomology is not necessary.
Adult ADHD Self-Report Scale (ASRS-v1.1) Symptom Checklist
| Patient name | Today’s date | ||||
|---|---|---|---|---|---|
| Please answer the questions below, rating yourself on each of the criteria shown using the scale on the right side of the page. As you answer each question, place an X in the box that best describes how you have felt and conducted yourself over the past 6 months. Please give this completed checklist to your healthcare professional to discuss during today’s appointment. | Never | Rarely | Sometimes | Often | Very often |
| 1. How often do you have trouble wrapping up the final details of a project, once the challenging parts have been done? | |||||
| 2. How often do you have difficulty getting things in order when you have to do a task that requires organization? | |||||
| 3. How often do you have problems remembering appointments or obligations? | |||||
| 4. When you have a task that requires a lot of thought, how often do you avoid or delay getting started? | |||||
| 5. How often do you fidget or squirm with your hands or feet when you have to sit down for a long time? | |||||
| 6. How often do you feel overly active and compelled to do things, like you were driven by a motor? | |||||
| part A | |||||
| 7. How often do you make careless mistakes when you have to work on a boring or difficult project? | |||||
| 8. How often do you have difficulty keeping your attention when you are doing boring or repetitive work? | |||||
| 9. How often do you have difficulty concentrating on what people say to you, even when they are speaking to you directly? | |||||
| 10. How often do you misplace or have difficulty finding things at home or at work? | |||||
| 11. How often are you distracted by activity or noise around you? | |||||
| 12. How often do you leave your seat in meetings or other situations in which you are expected to remain seated? | |||||
| 13. How often do you feel restless or fidgety? | |||||
| 14. How often do you have difficulty unwinding and relaxing when you have time to yourself? | |||||
| 15. How often do you find yourself talking too much when you are in social situations? | |||||
| 16. When you’re in a conversation, how often do you find yourself finishing the sentences of the people you are talking to, before they can finish them themselves? | |||||
| 17. How often do you have difficulty waiting your turn in situations when turn taking is required? | |||||
| 18. How often do you interrupt others when they are busy? | |||||
| Part B | |||||
The value of screening for adults with ADHD
Research suggests that the symptoms of ADHD can persist into adulthood, having a significant impact on the relationships, careers, and even the personal safety of your patients who may suffer from it.1–4 Because this disorder is often misunderstood, many people who have it do not receive appropriate treatment and, as a result, may never reach their full potential. Part of the problem is that it can be difficult to diagnose, particularly in adults.
The Adult ADHD Self-Report Scale (ASRS-v1.1) symptom checklist was developed in conjunction with the World Health Organization (WHO), and the Workgroup on Adult ADHD that included the following team of psychiatrists and researchers:
-
Lenard Adler, MD
Associate Professor of Psychiatry and Neurology
New York University Medical School
-
Ronald C. Kessler, PhD
Professor, Department of Health Care Policy
Harvard Medical School
-
Thomas Spencer, MD
Associate Professor of Psychiatry
Harvard Medical School
As a healthcare professional, you can use the ASRS v1.1 as a tool to help screen for ADHD in adult patients. Insights gained through this screening may suggest the need for a more in-depth clinician interview. The questions in the ASRS v1.1 are consistent with DSM-IV criteria and address the manifestations of ADHD symptoms in adults. Content of the questionnaire also reflects the importance that DSM-IV places on symptoms, impairments, and history for a correc diagnosis.4
The checklist takes about five minutes to complete and can provide information that is critical to supplement the diagnostic process.
References
- 1.Schweitzer JB, et al. Med Clin North Am. 2001;85(3):10–11. [Google Scholar]
- 2.Barkley RA. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 2nd ed. 1998. [Google Scholar]
- 3.Biederman J, et al. Am J Psychiatry. 1993;150:1792–1798. doi: 10.1176/ajp.150.12.1792. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders Fourth EditionText Revision. Washington, DC: American Psychiatric Association; 200085–93. [Google Scholar]
Appendix 2
ICD-10 Criteria for Diagnosis of Hyperkinetic Disorders.
Reproduced with permission from: World Health Organization. The ICD-10 Classification of mental and behavioural disorders: Diagnostic Criteria for Research. Geneva: Author, 1993, p155–157.
F90. Hyperkinetic disorders.
Note: The research diagnosis of hyperkinetic disorder requires the definite presence of abnormal levels of inattention, hyperactivity, and restlessness that are pervasive across situations and persistent over time and that are not caused by other disorders such as autism or affective disorders.
G1. Inattention. At least six of the following symptoms of inattention have persisted for at least six months, to a degree that is maladaptive and inconsistent with the developmental level of the child:
often fails to give close attention to details, or makes careless errors in schoolwork, work, or other activities;
often fails to sustain attention in tasks or play activities;
often appears not to listen to what is being said to him or her;
often fails to follow through on instructions or to finish schoolwork, chores, or duties in the workplace (not because of oppositional behaviour or failure to understand instructions);
is often impaired in organizing tasks and activities;
often avoids or strongly dislikes tasks, such as homework, that require sustained mental effort;
often loses things necessary for certain tasks or activities, such as school assignments, pencils, books, toys, or tools;
is often easily distracted by external stimuli;
is often forgetful in the course of daily activities.
G2. Hyperactivity. At least three of the following symptoms of hyperactivity have persisted for at least 6 months, to a degree that is maladaptive and inconsistent with the developmental level of the child:
often fidgets with hands or feet or squirms on seat;
leaves seat in classroom or in other situations in which remaining seated is expected;
often runs about or climbs excessively in situations in which it is inappropriate (in adolescents or adults, only feelings of restlessness may be present);
is often unduly noisy in playing or has difficulty in engaging quietly in leisure activities;
exhibits a persistent pattern of excessive motor activity that is not substantially modified by social context or demands.
G3. Impulsivity. At least one of the following symptoms of impulsivity has persisted for at least 6 months, to a degree that is maladaptive and inconsistent with the development level of the child:
often blurts out answers before questions have been completed;
often fails to wait in lines or await turns in games or group situations;
often interrupts or intrudes on others (eg, butts into others’ conversations or games);
often talks excessively without appropriate response to social constraints.
G5. Onset of the disorder is no later than the age of 7 years. G5. Pervasiveness. The criteria should be met for more than a single situation, eg, the combination of inattention and hyper-activity should be present both at home and at school, or at both school and another setting where children are observed, such as a clinic. (Evidence for cross-situationality will ordinarily require information from more than one source; parental reports about classroom behaviour, for instance, are unlikely to be sufficient).
G6. The symptoms in G1–G3 cause clinically significant distress or impairment I social, academic, or occupational functioning.
G7. The disorder does not meet the criteria for pervasive developmental disorders (F84.-), manic episode (F30.-), depressive episode (F32.-), or anxiety disorders (F41.-).
Comment
Many authorities also recognise conditions that are sub-threshold for hyperkinetic disorder. Children who meet criteria in other ways but do not show abnormalities of hyperactivity/impulsiveness may be recognized as showing attention deficit; conversely, children who fall short of criteria for attention problems but meet criteria in other respect may be recognized as showing activity disorder. In the same way, children who meet criteria for only one situation (eg, only the whom or only the classroom) may be regarded as showing a home-specific or classroom-specific disorder. These conditions are not yet included in the main classification because of insufficient empirical predictive validation, and because many children with sub-threshold disorders show other syndromes (such as oppositional defiant disorder, F91.3) and should be classified in the appropriate category.
F90.0 Disturbance of activity and attention.
The general criteria for hyperkinetic disorder (F90) must be met, but not those for conduct disorders (F91.-).
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Bird HR, Canino G, Rubio-Stipec M, et al. Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico. Arch Gen Psychiatry. 1988;45:1120–1126. doi: 10.1001/archpsyc.1988.01800360068010. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JC, Williams S, McGee R, et al. DSM-III disorders in pre adolescent children: prevalence in a large sample from the general population. Arch Gen Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- 4.Spencer T, Biederman J, Wilens TE, Faraone SV. Adults with attention-deficit/hyperactivity disorder; a controversial diagnosis. J Clin Psychiatry. 1998;59(Suppl 7):59–68. [PubMed] [Google Scholar]
- 5.Kessler RC, Adler LA, Barkley R, et al. Patterns and predictors of attention deficit/hyperactivity disorder persistence into adulthood: Results from the National Comorbidity Survey Replication. Biol Psychiatry. 2005;57:1442–1451. doi: 10.1016/j.biopsych.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cumyn L, Kolar D, Keller A, Hechtman L. Current issues and trends in the diagnosis and treatment of adults with ADHD. Expert Rev Neurotherapeutics. 2007;7:1375–1390. doi: 10.1586/14737175.7.10.1375. [DOI] [PubMed] [Google Scholar]
- 7.Alpert JA, Maddocks A, Nierenberg AA, et al. Attention deficit hyperactivity disorder in childhood among adults with major depression. Psychiatry Res. 2006;62:213–219. doi: 10.1016/0165-1781(96)02912-5. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of Adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fayyad F, De Graaf R, Kessler R, et al. Cross–national prevalence and correlates of adult attention–deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402–409. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- 10.Mannuzza S, Klein RG, Klein DF, Bessler A, Shrout P. Accuracy of adult recall of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 2002;159:1882–1888. doi: 10.1176/appi.ajp.159.11.1882. [DOI] [PubMed] [Google Scholar]
- 11.Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder; are late onset and subthreshold diagnoses valid? Am J Psychiatry. 2006;163:1720–1729. doi: 10.1176/ajp.2006.163.10.1720. [DOI] [PubMed] [Google Scholar]
- 12.Asherson P, Chen W, Craddock B, Taylor E. Adult attention-deficit hyperactivity disorder: recognition and treatment in general adult psychiatry. Br J Psychiatry. 2007;190:4–5. doi: 10.1192/bjp.bp.106.026484. [DOI] [PubMed] [Google Scholar]
- 13.Goodman DW. The consequences of attention-deficit/hyperactivity disorder in adults. J Psychiatr Pract. 2007;13:318–327. doi: 10.1097/01.pra.0000290670.87236.18. [DOI] [PubMed] [Google Scholar]
- 14.Sobanski E. Psychiatry co-morbidity in adults with attention deficit/hyperactivity disorder (ADHD) Eur Arch Psychiatr Clin Neurosci. 2006;256:26–31. [Google Scholar]
- 15.Biederman J. Impact of comorbidity in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2004;65(Suppl 3):3–7. [PubMed] [Google Scholar]
- 16.Murphy KR, Adler LA. Assessing attention-deficit/hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry. 2004;65(Suppl 3):12–17. [PubMed] [Google Scholar]
- 17.Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155:493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- 18.Mannuzza S, Shenker R, Bonagura N, Malloy P, Giampino TL, Addalli KA. Hyperactive boys almost grown up, V: replication of psychiatric status. Arch Gen Psychiatry. 1991;48:77–83. doi: 10.1001/archpsyc.1991.01810250079012. [DOI] [PubMed] [Google Scholar]
- 19.Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol. 2002;111:279–289. [PubMed] [Google Scholar]
- 20.Weiss G, Hechtman LT. Hyperactive children grown up. New York: Guilford; 1993. [Google Scholar]
- 21.Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry. 2000;39:1424–1431. doi: 10.1097/00004583-200011000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Biederman E, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder impact of remission definition and symptom type. Am J Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- 23.Murphy K, Barkley RA. Prevalence of DSM-IV symptoms of ADHD in adult licensed drivers: Implications for clinical diagnosis. J Atten Disord. 1996;1:147–161. [Google Scholar]
- 24.Able SL, Johnston JA, Adler LA, Swindle RW. Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychol Med. 2007;37:97–107. doi: 10.1017/S0033291706008713. [DOI] [PubMed] [Google Scholar]
- 25.Young S, Toone B. Attention deficit hyperactivity disorder in adults: clinical issues. A report from the first NHS clinic in the UK. Couns Psych Q. 2000;13:313–319. [Google Scholar]
- 26.Adler L, Cohen J. Diagnosis and evaluation of adults with attention- deficit/hyperactivity disorder. Psychiatr Clin N Am. 2004;27:187–201. doi: 10.1016/j.psc.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Fischer M, Barkley RA, Smallish L, Fletcher K. Executive functioning in hyperactive children as young adults: attention, inhibition, response perseveration, and the impact of comorbidity. Dev Neuropsychol. 2005;27:107–133. doi: 10.1207/s15326942dn2701_5. [DOI] [PubMed] [Google Scholar]
- 28.Nadeau K. Career choices and workplace challenges for individuals with ADHD. J Clin Psychiatry. 2005;61:549–563. doi: 10.1002/jclp.20119. [DOI] [PubMed] [Google Scholar]
- 29.Adler L, Cohen J. Diagnosis and evaluation of adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27:187–201. doi: 10.1016/j.psc.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Biederman J, Faraone S, Spencer T, et al. Functional impairments in adults with self-reports of diagnosed ADHD: a controlled study of 1001 adults in the community. J Clin Psychiatry. 2006;67:524–540. doi: 10.4088/jcp.v67n0403. [DOI] [PubMed] [Google Scholar]
- 31.Barkley RA, Fischer M, Edelbrock CS, et al. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Clarke S, Heussler H, Kohn M. Attention deficit disorder: not just for children. Int Med J. 2005;35:721–725. doi: 10.1111/j.1445-5994.2005.00987.x. [DOI] [PubMed] [Google Scholar]
- 33.Weiss G, Hechtman L, Milroy T, et al. Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry. 1985;24:211–220. doi: 10.1016/s0002-7138(09)60450-7. [DOI] [PubMed] [Google Scholar]
- 34.Gittelman R, Mannuzza S, Shenker R, et al. Hyperactive boys almost grown up, I: psychiatric status. Arch Gen Psychiatry. 1985;42:937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- 35.Cantwell D, Hanna G. Attention deficit hyperactivity disorder. In: Tasman A, Hales R, Frances A, editors. Review of Psychiatry, 8. Washington, DC: American Psychiatric Press; 1989. pp. 134–161. [Google Scholar]
- 36.Torgersen T, Gjervan B, Rasmussen K. ADHD in adults: a study of clinical characteristics, impairment and comorbidity. Nord J Psychiatry. 2006;60:38–43. doi: 10.1080/08039480500520665. [DOI] [PubMed] [Google Scholar]
- 37.Biederman J, Faraone SV, Spencer T, et al. Patterns of psychiatric comorbidity, cognition and psychosocial functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:1792–1798. doi: 10.1176/ajp.150.12.1792. [DOI] [PubMed] [Google Scholar]
- 38.Faraone SV. Genetics of childhood disorders: XX. ADHD, Part 4: IS ADHD genetically heterogeneous? J Am Acad Child Adolesc Psychiatry. 2000;39:1455–1457. doi: 10.1097/00004583-200011000-00022. [DOI] [PubMed] [Google Scholar]
- 39.Faraone SV, Biederman J, Monuteaux M. Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet Epidemiol. 2000;18:1–16. doi: 10.1002/(SICI)1098-2272(200001)18:1<1::AID-GEPI1>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 40.Faraone SV, Biederman J. Do attention deficit hyperactivity disorder and major depression share familial risk factors? J Nerv Ment Dis. 1997;185:533–541. doi: 10.1097/00005053-199709000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Moss SB, Nair R, Vallarino A, Wang S. Attention deficit/hyperactivity disorder in adults. Prim Care Clin Office Pract. 2007;34:445–473. doi: 10.1016/j.pop.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Biederman J. Attention-deficit/hyperactivity disorder: a life-span perspective. J Clin Psychiatry. 1998;59(Suppl 7):4–16. [PubMed] [Google Scholar]
- 43.Riordan HJ, Flashman LA, Saykin AJ, Frutiger SA, Carroll KE, Huey L. Neuropsychological correlates of methylphenidate treatment in adult ADHD with and without depression. Arch Clin Neuropsychol. 1999;14:217–233. [PubMed] [Google Scholar]
- 44.Milberger S, Biederman J, Faraone SV, Murphy J, Tsuang MT. Attention deficit hyperactivity disorder and comorbid disorders: Issues of overlapping symptoms. Am J Psychiatry. 1995;152:1793–1799. doi: 10.1176/ajp.152.12.1793. [DOI] [PubMed] [Google Scholar]
- 45.Fischer M, Barkley R, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnormal Child Psychol. 2002;60:463–475. doi: 10.1023/a:1019864813776. [DOI] [PubMed] [Google Scholar]
- 46.Spencer TJ, Faraone SV, Michelson D, et al. Atomoxetine and adult attention-deficit/hyperactivity disorder: The effects of comorbidity. J Clin Psychiatry. 2006;67:415–420. doi: 10.4088/jcp.v67n0312. [DOI] [PubMed] [Google Scholar]
- 47.Katz LJ, Wood DS, Goldstein G, Auchenbach RC, Geckle M. The utility of neuropsychological tests in evaluation of attention-deficit hyperactivity disorder (ADHD) versus depression in adults. Assessment. 1998;5:45–51. doi: 10.1177/107319119800500107. [DOI] [PubMed] [Google Scholar]
- 48.Rostain AL. Adult ADHD and depressive disorders: prevalence, significance and clinical presentation. CNS Spectr. 2008;13(5 Suppl 8):8–10. doi: 10.1017/s1092852900002959. [DOI] [PubMed] [Google Scholar]
- 49.Sobanski E, Bruggeman D, Alm B, et al. Psychiatric comorbidity and functional impairment in a clinically referred sample of adults with attention-deficit/hyperactivity disorder (ADHD) Eur Arch Psychiatry Clin Neurosci. 2007;257:371–377. doi: 10.1007/s00406-007-0712-8. [DOI] [PubMed] [Google Scholar]
- 50.Biederman J, Faraone SV, Spencer T, Wilens T, Mick B, Lapey B. Gender differences in adults with attention-deficit hyperactivity disorder. Psychiatry Res. 1994;53:13–29. doi: 10.1016/0165-1781(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 51.Lewinsohn PM, Rohde P, Seeley JR. Psychosocial characteristics of adolescents with a history of suicide attempt. J Am Acad Child Adolesc Psychiatry. 1993;32:60–68. doi: 10.1097/00004583-199301000-00009. [DOI] [PubMed] [Google Scholar]
- 52.Fischer AG, Bau CHD, Grevet EH, et al. The role of comorbid major depressive disorder in the clinical presentation of adult ADHD. J Psychiatr Res. 2007;41:991–996. doi: 10.1016/j.jpsychires.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 53.Secnik K, Swensen A, Lage MJ. Comorbidities and costs of adult patients diagnosed with attention-deficit hyperactivity disorder. Pharmacoeconomics. 2005;23:93–102. doi: 10.2165/00019053-200523010-00008. [DOI] [PubMed] [Google Scholar]
- 54.Biederman J, Faraone SV, Monuteaux MC, Bober M, Cadogen E. Gender effects on attention-deficit/hyperactivity disorder in adults, revisited. Biol Psychiatry. 2004;55:692–700. doi: 10.1016/j.biopsych.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 55.Biederman J, Ball S, Monuteaux M, et al. New insights into the comorbidity of ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry. 2008;47:426–434. doi: 10.1097/CHI.0b013e31816429d3. [DOI] [PubMed] [Google Scholar]
- 56.Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: a multisource, multimethod assessment of clinical, social and academic functioning. J Atten Disord. 2005;8:195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- 57.Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide. Arch Gen Psychiatry. 1988;45:581–588. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- 58.Biederman J, Faraone SV, Keenan K, Tsuang MT. Evidence of familial association between attention deficit disorder and major affective disorders. Arch Gen Psychiatry. 1991;48:633–642. doi: 10.1001/archpsyc.1991.01810310051009. [DOI] [PubMed] [Google Scholar]
- 59.Mangelli L, Fava GA, Grandi S, et al. Assessing demoralization and depression in the setting of medical disease. J Clin Psychiatry. 2005;66:391–394. doi: 10.4088/jcp.v66n0317. [DOI] [PubMed] [Google Scholar]
- 60.Biederman J, Mick E, Faraone SV. Depression in attention deficit hyperactivity disorder (ADHD) children: “true” depression or demoralization? J Affect Disord. 1998;47:113–122. doi: 10.1016/s0165-0327(97)00127-4. [DOI] [PubMed] [Google Scholar]
- 61.Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36:733–742. doi: 10.1046/j.1440-1614.2002.01086.x. [DOI] [PubMed] [Google Scholar]
- 62.Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 63.Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA). Canadian ADHD Practice Guidelines 2007/2008. Accessed on Dec 12, 2008. Available from: http://www.caddra.ca/english/phys_guide.html
- 64.Kolar D, Keller A, Golfinopoulos M, Cumyn L, Syer C, Hechtman L. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008;4:389–403. doi: 10.2147/ndt.s6985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gibbins C, Weiss M. Clinical recommendations in current practice guidelines for diagnosis and treatment of ADHD in adults. Curr Psychiatry Rep. 2007;9:420–426. doi: 10.1007/s11920-007-0055-1. [DOI] [PubMed] [Google Scholar]
- 66.Hornig-Rohan M, Amsterdam JD. Venlafaxine versus stimulant therapy in patietns with dual diagnosis ADD and depression. Progr NeuroPsychopharmacol Biol Psychiatry. 2002;26:585–589. doi: 10.1016/s0278-5846(01)00312-8. [DOI] [PubMed] [Google Scholar]
- 67.Biederman J, Mick E, Surman C, et al. Impact of psychiatric comorbidity and concomitant use of antidepressants on the efficacy of OROS® MPH in adults with ADHD: a randomized double-blind study. Poster NR 358. Presented at the 160th Annual Meeting of the American Psychiatric Association; May 21, 2007; San Diego, CA. [Google Scholar]
- 68.Myronuk LDS, Weiss M. Combined treatment with moclobemide and methylphenidate for comorbid major depression and adult attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 16:468–469. doi: 10.1097/00004714-199612000-00018. [DOI] [PubMed] [Google Scholar]
- 69.Findling RL. Open-label treatment of comorbid depression and attentional disorders with co-administration of serotonin reuptake inhibitors and psychostimulants in children, adolescents and adults. J Child Adolesc Psychopharmacol. 1996;6:165–175. doi: 10.1089/cap.1996.6.165. [DOI] [PubMed] [Google Scholar]
- 70.Spencer TJ. Treatment of adult ADHD and comorbid depression. CNS Spectr. 2008;13(Suppl 8):14–16. doi: 10.1017/s1092852900002972. [DOI] [PubMed] [Google Scholar]
- 71.Weiss M, Safren S, Solanto MV, et al. Research forum on psychological treatment of adults with ADHD. J Atten Disord. 2008;11:642–651. doi: 10.1177/1087054708315063. [DOI] [PubMed] [Google Scholar]
- 72.Canadian Network for Mood and Anxiety Treatment (CANMAT) Clinical Guidelines for the Treatment of Depressive Disorders. Canadian Psychiatric Association and CANMAT. 2001 Cited on Dec 12, 2008. Available from: http://www.canmat.org/
- 73.Food and Drug Administration FDA directs ADHD drug manufacturers to notify patients about cardiovascular adverse events and psychiatric adverse events [Press Release]. February 21, 2007. Cited on Dec 12, 2008. Available from http://www.fda.gov/bbs/topics/news/2007/new01568.html
- 74.Ravindran AV, Kennedy SH, O’Donovan C, Fallu A, Camacho F, Binder CE. Osmotic-release oral system methylphenidate augmentation of antidepressant monotherapy in major depressive disorder: results of a doubleblind randomized, placebo-controlled trial. J Clin Psychiatry. 2008;69:87–94. doi: 10.4088/jcp.v69n0112. [DOI] [PubMed] [Google Scholar]
- 75.Patkar AA, Masand PS, Pae C-U, et al. A randomized, double-blind placebo-controlled trial of agumentation with an extended release formulation of methylphenidate in outpatients with treatment-resistant depression. J Clin Psychopharmacol. 2006;26:653–656. doi: 10.1097/01.jcp.0000246212.03530.fd. [DOI] [PubMed] [Google Scholar]
- 76.Wigal SB, Wigal TL. Special considerations in diagnosing and treating attention-deficit/hyperactivity disorder. CNS Spectr. 2007;12(6 Suppl 9):1–14. doi: 10.1017/s1092852900026092. [DOI] [PubMed] [Google Scholar]
- 77.Faraone SV, Wilens T. Does stimulant treatment lead to substance abuse disorders? J Clin Psychiatry. 2003;64(Suppl 11):9–13. [PubMed] [Google Scholar]
- 78.Biederman J, Monuteaux MC, Spencer T, Wilens TE, MacPherson HA, Faraone SV. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. Am J Psychiatry. 2008;165:597–603. doi: 10.1176/appi.ajp.2007.07091486. [DOI] [PubMed] [Google Scholar]
- 79.Medori R, Ramos-Quiroga JA, Casas M, et al. A randomized, placebo-controlled trial of three fixed dosages of prolonged-release OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2008;63:981–989. doi: 10.1016/j.biopsych.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 80.McCracken JT, Biederman J, Greenhill LL, et al. Analog classroom assessment of a once-daily mixed amphetamine formulation, SlI381 (Adderall XR) in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42:673–683. doi: 10.1097/01.CHI.0000046863.56865.FE. [DOI] [PubMed] [Google Scholar]
- 81.Michelson D, Adler L, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo-controlled studies. Biol Psychiatry. 2003;53:112–120. doi: 10.1016/s0006-3223(02)01671-2. [DOI] [PubMed] [Google Scholar]
- 82.American Heart Association, American Academy of Pediatrics Clarification of statement on cardiovascular evaluation and monitoring of children and adolescents with heart disease receiving medications for ADHD [Press Release]. May 16, 2008. Cited Dec 12, 2008. Available from: http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.107.189473/DC1 [DOI] [PubMed]
- 83.Wooltorton E. Medications for attention deficit hyperactivity disorder: cardiovascular concerns. CMAJ. 2006;175:2. doi: 10.1503/cmaj.060718. [DOI] [PMC free article] [PubMed] [Google Scholar]