Abstract
Background
Modern biomonitoring has expanded beyond its origins in occupational medicine to cover a wide variety of diagnostic procedures and assessments of environmental pollution, ranging from exposure to heavy metals and chemicals to the effects of pesticides and environmental tobacco smoke. In biomonitoring, the overall pollutant load and hazardous exposure of an organism is quantitatively determined, by monitoring the pollutants themselves, their metabolic products and/or conjugates with protein or DNA, in either serum, urine or other body fluids, as well as tissue samples in exceptional circumstances.
Methods
A selective survey of the current literature is exemplified by our recent scientific and clinical experience.
Results
Biomonitoring is an excellent way to monitor potentially hazardous substances, especially for the assessment of systemic uptake from chronic exposure and the evaluation of subsequent health risks. Investigative biomonitoring can highlight incidental/accidental intoxication in individuals and provide new categories of problematic pollutants relevant to the general population.
Conclusions
In combination with diagnostic procedures, biomonitoring provides an important contribution to the rational assessment of currently recorded pollutants and resulting health risks. It is as an evaluation tool available in daily practice as well as in health and environmental research applications. Legislation is already implemented that incorporates biomonitoring within the remit of specified occupational health screening.
Keywords: biomonitoring, hazardous exposure, noxious substance, environmental pollution, environmental medicine
Exposure to noxious substances can be expected in many areas of work. If there is a causal connection between work-related exposure and disease, we are dealing with a work-related disease. Legislators have defined some of these diseases as occupational diseases. These are neurological or systemic disturbances to health—for example, from metals or solvents—or diseases of the skin or respiratory tract, triggered by irritant or allergenic substances. About four million chemical substances have been synthesized; many of these can trigger disease, but have not been incorporated into the law on occupational diseases. The latter include pyrethroids, PCB, phthalates, and passively inhaled cigarette smoke. According to a current study, 8% of nonsmokers in the USA are still exposed to passively inhaled smoke at the workplace (1).
In addition, these and many other noxious substances in the general environment may act on man. They have a decisive influence on the overall pollutant load for the organism and cause several illnesses. These noxious substances may be incorporated by inhalation and/or cutaneous contact, as well as orally. More than 4500 cases of acute or chronic intoxication are reported annually in Germany (2). The unreported figure is presumably higher, as correlative background information is often unknown. As these cases are generally not restricted to specific localizations or specific groups of individuals, in potential cases, a detailed medical history must be taken and diagnostic procedures initiated (3, 4). For example, the toxic and carcinogenic effect of agricultural chemicals or polycyclic aromatic hydrocarbons, either indoors or outside, can lead to systemic disturbances or lesions of the skin and/or respiratory organs (5). If the pollutants interact with particularly sensitive individuals, such as children, the old, or vulnerable persons, even small quantities may cause neurological or other damage or anomalies. Because of the increasing globalization of the exchange of goods, the general population in Germany is now being exposed again to hazards which have long been prohibited, but which are now being introduced with the products from low wage countries. Examples of this include benzene and insecticides such as lindane (our own unpublished data; [6]).
When individuals take up noxious substances, this leads to internal lesions, which can be measured objectively. To recognize whether a subject is suffering from integrated exposure to a hazardous substance, or even accidental intoxication, standardized analytical procedures for the diagnostic investigation of biological materials have become established and these are subsumed under the term "biomonitoring." Taken together with clinical experience and epidemiological studies, the personal data from biomonitoring permits an evaluation of the noxious substances taken up. For example, population-orientated studies have provided data on lead, PCB or phthalate loads in Germany (7, 8, 9).
The aim of the present article is to describe the possibilities open to biomonitoring in the clarification of potential acute or chronic intoxications. New developments will also be described, such as effect biomonitoring, which correlates with the health risk. It quite often happens that assumptions about intoxications from environmental toxins can be disproved with the help of qualified biomonitoring.
Health risk from incorporated environmental pollutants
There are two measurement strategies in environmental and occupational medicine used to record the health risk to the general population and to exposed employees. Either the pollutant can be measured in the air—also known as air monitoring or ambient monitoring—or the internal exposure can be quantified—which is known as biomonitoring. Both ambient monitoring and biomonitoring are of established value in diagnosis and complement each other. To obtain an approximate assessment of the risk, it is often of decisive importance first to determine the type and degree of possible contamination with ambient monitoring. Under experimental conditions in the laboratory and applying the principles of pharmacokinetics, a relationship can be established between the air concentration of inhalable substances and the internal load. The conditions at the workplace do not allow the air concentration to be directly deduced from the concentration of the pollutant or its metabolites in the biological material. Thus, individual risk assessment should not be restricted to compliance with air limit values (10). Measurements of pollutants in the air, soil, house dust, and in other media can only indicate that individuals may be exposed and/or serve to characterize the toxins on site.
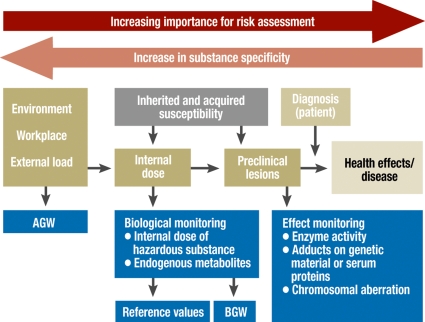
In addition, animal studies do not produce data on health risks which can be transferred one to one to humans, as there are considerable discrepancies between the species, due to differences in genetic, anatomical, motoric, physiological, and metabolic characteristics. In contrast to analyses of hazardous substances in the air, biomonitoring affords a rational possibility of measuring the pollutant dose in an organism (10). This covers uptake through inhalation, through the skin or through the intestines, and thus gives the real internal load. Thus biomonitoring is a unique way of recording and quantifying environmental and occupational loads (figure 1). Internal exposure can trigger different reactions or changes in each individual and these are defined as preclinical lesions (figure 1).
Figure 1.
From external to internal dose. AGW, workplace limit value; BGW, biological guidance value
Definition of biomonitoring
Biomonitoring was originally defined as "systematic standardized measurement of a substance or its metabolites in body fluids (including blood and urine) of exposed persons" (3, 4, 11). This classical exposure monitoring (table) is now complemented by additional biomonitoring analyses (3, 4).
Table. Examples of biomonitoring parameters.
| Selection of biomonitoring parameters (exposure markers) | Matrix | BGW/EKA | Reference value (source) | BLW/HMB-II/BAT Carcinogenesis category | Units |
| Metals | |||||
| Aluminium | (U) | 200 | 15 (b) | 60 µg/g creatinine (BAT) | µg/L |
| Lead | (B) | 400 (300, w<45y) | 90 (70, w<45y) (a) | 400 (100, w<45y) (blw), 250 (hbm-ii), cancer cat.2 | µg/L |
| Nickel | (U) | EKA*1 | 3 (a) | Cancer cat. 1 | µg/L |
| Mercury | (U) | 100 | 1.4 (a) | Cancer cat. 3B 20 µg/g creatinine (HBM-II) | µg/L |
| Organic solvents and their metabolic products | |||||
| Benzene | (B) | EKA*2 | 0.001 (b) | Cancer cat. 1 | mg/L |
| o-Cresol (parameter for toluene) | (U) | 3 | Cancer cat. 3A | mg/L | |
| Mandelic acid/phenylglyoxylic acid(parameters for styrene) | (U) | 600 | mg/g creatinine | ||
| Methanol | (U) | 30 | mg/L | ||
| Methylhippuric (toluric) acid (parameter for xylene) | (U) | 2000 | mg/L | ||
| t-t-muconic acid (parameter for benzene) | (U) | EKA*2 | mg/L | ||
| Toluene | (B) | 1 | 0.005 (b) | mg/L | |
| Xylenes | (B) | 1.5 | 0.003 (b) | mg/L | |
| Pesticides | |||||
| γ-Hexachlorcyclohexane (lindane) | (B) | 25 | 0.1 (a) | Cancer cat. 4 | µg/L |
| Hexachlorobenzene | (S) | 150 (BAT), | µg/L | ||
| (B) | 0.5 (a) | Cancer cat. 4 | |||
| PCB153 | (B) | 0.8 (a) | µg/L | ||
| Pentachlorophenol | (S) | EKA*3 | 12 (a) | 70 (HBM-II), Cancer cat. 2 | µg/L |
| Other hazardous substances | |||||
| Isocyanate: 4,4'-MDI, 1,5-NDI, 2,4-TDI, 2,6-TDI, 1,6-HDI, IPDI | (U) | 10 (for 4,4'-MDI) | 4,4'-MDI: Cancer cat 4; | µg/L | |
| 1,5-NDI: Cancer cat 3B; | |||||
| 2,4-TDI: Cancer cat 3A; | |||||
| 2,6-TDI: Cancer cat 3A | µg/g creatinine | ||||
IBAT, BLW, HBM-II, and EKA values are only given when there is no BGW value and/or these values differ from the BGW: Reference values: m, 20-29 Y. Abbreviations: U: urine; B: whole blood;
S: serum; Source for limit values: BGW: biological limit value (14c, www.baua.de); BLW: biological guidance value; EKA: exposure equivalents for carcinogenic substances (16); reference values:
a) www.uni-duesseldorf.de/awmf/II/002-024;
c) www.cdc.gov; more biomonitoring parameters: www.uke.uni-hamburg.de/Institute/Arbeitsmedizin
*1, EKA for nickel (nickel as metal oxide, carbonate or sulfide): 15 µg/L (U) is equivalent for 0.10 mg/m3 nickel (air)
*2, EKA for 0.005mg/L benzene (B) and 2 mg/L t-t-muconic acid (U) is equivalent for 1 ppb (3.3 mg/m3) benzene (air)
*3, EKA for pentachlorophenol: 17 µg/L (S) is equivalent for 0.001 mg/m3 (air)
Biochemical effect monitoring includes studies of the formation of protein and DNA adducts, the binding products of chemically reactive substances such as acrylamide, a component of intensely heated foods. Biological effect monitoring includes additional monitoring at the subcellular level, such as changes in enzymatic activity or the formation of micronuclei.
Although the toxicological significance of effect biomonitoring is clearly greater than that of exposure biomonitoring, its substance specificity is lower, as different hazardous substances can trigger the same biological effect. Moreover, some of the limit values for exposure biomonitoring do not reflect the links between the air concentration of the hazardous substance and the internal dose, but consider the frequency and intensity of adverse reactions and internal exposure. The new developments in effect biomonitoring have been able to fill in gaps in the clarification of a potential association between exposure and the development of disease. To improve the characterization of possible risks to health, dose monitoring (= exposure biomonitoring) should be complemented by studies of biological effects (= effect biomonitoring) (figure 1).
Legal principles, establishing reference and limit values
Biomonitoring is an established component of occupational health surveillance (12). The current draft of the Ordinance on Occupational Medical Care (ArbMedVV) has already been passed by the German cabinet. This creates transparency with respect to the obligatory and available investigations and enhances the right to request investigations (13). The Ordinance on Hazardous Substances (GefStoffV) refers to the technical rules for hazardous substances (TRGS). These reflect the current status of the technical safety, occupational medical, and occupational scientific requirements for the hazardous substances (14a). Biomonitoring has been implemented in this legal regulatory system for some years. TRGS 710 (14b) gives a detailed description of the constellations under which biomonitoring is prescribed and when it is only recommended. The aim is to record the load and risk to health of the employees, to compare the analytical values with evaluation values, and to suggest suitable measures to protect health at the workplace from the effects of chemical substances. Biomonitoring makes it possible for the occupational physician to evaluate the occupational medical conditions of the employees or at the workplace and thus to document the success or failure of measures to reduce emissions. The rules of professional associations (such as the German G2 "Work with Lead or its compounds"), together with occupational and environmental medical guidelines contain specific practical instructions.
Reference values for the general population have replaced the previous term of "normal values," to make it clear that these are primarily statistical ranges, taken from a group of healthy subjects. The reference values are only of descriptive character and are certainly not fixed, as they can be influenced by age, region, life style, or other factors. The DFG (German Research Foundation) Senate committee to examine working materials is currently developing biological reference values for working materials hazardous to health (biologische Arbeitsstoffreferenzwerte, BAR).
Both national and international limit values have been established and these are now both extensive and complex (table). The currently binding limits in Germany (14c) are implemented through the GefStoffV. The TRGS 903 includes the so-called biological limit values (biologische Grenzwerte, BGW): "A specific biological limit value is the limit value for the concentration of a substance, its metabolite or of an indicator of preclinical lesions in the corresponding material, derived from toxicological and occupational medical data, at which the health of an employee is generally not impaired." (Gefstoff V §3 Section 8).
BGWs are conceived as the maximal values for healthy individuals with a 5-day working week and an 8-hour day and are generally given for blood and/or urine, after considering the characteristic activity of the substance. The workplace limit value (Arbeitsplatzgrenzwert, AGW) signifies the concentrations of a hazardous substance in the air at the workplace which do not impair health. The AGW is weighted for time, like the BGW. The legal principles for health care are currently being revised by the committee for hazardous substances (14d) and the Federal Government’s scientific advisory committee for global environmental change (15). For carcinogenic substances, the committee is developing new risk limit values, each with an acceptance and a tolerance risk, and is also developing additional criteria for the classification of risks (15).
Evaluation of analytical data
Biomonitoring data are generally interpreted with the help of reference and limit values. If no BGW is available, the interpretation should be based on a comparison of the analytical values with the recommendations in the scientific literature, such as the BLW (biologischer Leitwert, biological guidance value) or the BAT value (biologischer Arbeitsstoff-Toleranzwert, biological working material tolerance value) of the DFG Senate committee to examine working materials (16, 17, 18) (table). In occupational medicine, evaluation of the biomonitoring results can be supported by the reference values for the general population and the workplace-related limit values (BGW; BAT) (19). Human biomonitoring limit values (HBMs) have been published by the committee on human biomonitoring (20). They are toxicologically based and include environmental evaluation of chemical loads. It must be borne in mind that even compliance with limit values of this sort does not guarantee safety for particularly sensitive persons, especially if there is an allergic reaction.
Metabolism of foreign substances and toxicokinetics
The selection of the biomonitoring parameter for each case must be based on the specific toxic effect of the foreign substance and should permit an estimate of the exposure, after allowing for the half-life (table).
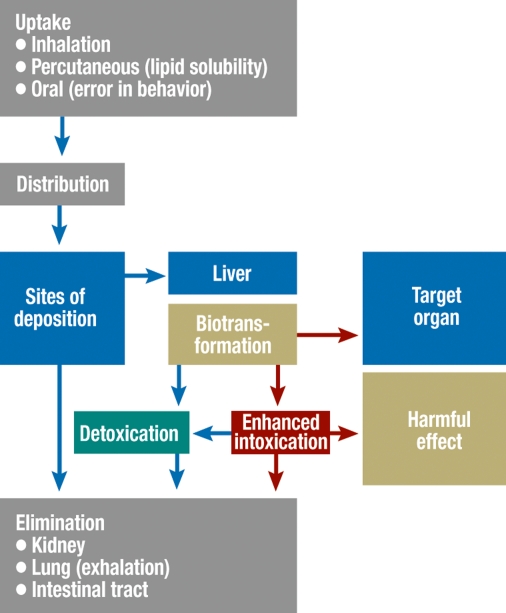
Biomonitoring is based on knowledge of the metabolic pathway of a hazardous substance in the organism (xenobiotic metabolism) and its toxicokinetics. All toxic materials are metabolized in the body—to different extents and at different rates (figure 2). The breakdown products are mostly taken up more rapidly by the kidneys than the starting compounds. The toxic substances are distributed according to the set patterns for toxins and regulated by a complex system. Phase I and II enzymes play an important role. Their primary function is to render foreign compounds harmless and/or to facilitate their elimination. Not all metabolic processes decrease the toxicity of foreign substances. They may even initially form highly toxic compounds. If reaction products of this sort are known and can be measured, they are used as biomarkers.
Figure 2.
Metabolism
If biomonitoring is systematically performed, it reflects changes in the level of exposure, for example, in the environmental air or in food. These changes may either be considered for individuals or for specially exposed groups of people at special risk, for example, varnishers exposed to solvent or children exposed to PCB. Biomonitoring is now used in various population screening studies and this has led to its being of increasing importance outside occupational medicine. For example, it is used in monitoring the health of people living near waste disposal sites, users of drinking water contaminated with lead, and marksmen (3, 7– 9).
Environmental and work-related lead load
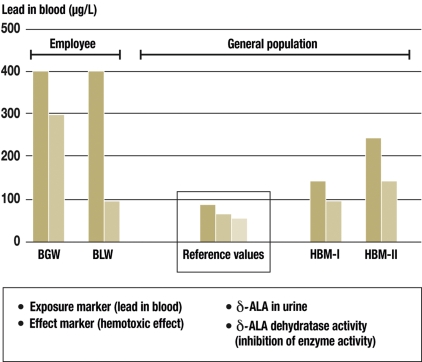
A classical example of biomonitoring is the determination of biomarkers for environmental and work-related lead exposure. The most important effect is lead’s hemotoxic activity, triggered by its inhibition of haem synthesis. Figure 3 summarizes the resulting biomarkers which can be recorded, together with their current reference values.
Figure 3.
Exposure markers. BGW, biological limit value; BLW, biological guidance value; HBM, human biomonitoring limit value
Acute and chronic intoxication with benzene analogues
Benzene analogues (the solvents toluene, the xylenes, and styrene) can be taken up by inhalation or cutaneously. Acute intoxication is marked by CNS depression. There is no specific clinical presentation for the chronic effects of toluene, the xylenes, or styrene. The most striking features are neurological and psychological disturbances and alcohol intolerance. It must be remembered that patients have generally been exposed to a mixture of solvents, and not just a single substance. This makes evaluation more difficult (21).
Environmental exposure to tobacco smoke
Passive smoking is the most common environmental exposure to hazardous substances. Passive smoking essentially consists of sidestream smoke, meaning the smoke released by the heat of the burning cigarette into the environment. Tobacco smoke contains many poisonous and carcinogenic substances. The smoke of an average cigarette contains more than 4800 different chemical compounds, including toxins such as hydrocyanic acid, ammonia and carbon monoxide. More than 70 of these substances have been shown to be carcinogenic. Passive smoking leads to potentially fatal chronic diseases, including chronic obstructive pulmonary disease (COPD), stroke, and pulmonary and laryngeal cancer (22, 23).
Cotinine is an important breakdown product of nicotine. As the half-life of nicotine is about 2.5 h, cotinine can serve as a reliable parameter to determine the current smoker status (24). Its concentration in urine correlates well with the quantity of nicotine taken up. The average cotinine value for nonsmokers is 2 µg/g creatinine; the reference value is 16 µg/g creatinine. The cotinine value for active smokers is 105 to 2993 µg/g creatinine and the level of cotinine excretion permits an estimate of the number of cigarettes smoked.
Interpretation of diagnostic laboratory data
A simple comparison between a biomonitoring value and a reference value does not allow any specific conclusion about the risk to health or any illness. This requires examination of all available analytical data in context with the clinical findings. It is important to bear in mind when interpreting biomonitoring data that the biologically effective dose and early detection of health impairment are not only influenced by the type and dose of incorporation of foreign materials, but also other factors, such as physical exertion, hormonal status, nutrition, drug and alcohol abuse, and nicotine abuse (box). Paradoxical effects (idiosynchratic reactions) may occur, as well as potentiating, additive, and subadditive effects. Paradoxical effects increase with age. The subject’s general condition and habituation to toxic substances may also greatly influence the magnitude of the effect and must be considered during the interpretation of the findings.
Box. Factors influencing the sensitivity to hazardous substances.
-
Biological (individual) factors
Genetic factors (such as polymorphisms)
Toxicokinetics
Metabolism and elimination of the hazardous substances (phase I and phase II, phase III)
Sex and age
Smoking status / alcohol abuse
Hormonal effects
Constitutional health (and diseases)
-
Environmental factors
Stress
Nutritional status
Climate
Individual susceptibility to a specific substance (either genetic or acquired) is an additional aspect, which is often neglected. Many people exhibit genetically based deviations from the normal reaction to toxic substances. This can lead to increased or decreased activity of the enzymes responsible for the metabolism of foreign substances. For example, the terms slow and rapid inactivators are used. These terms apply to oxidation from phase I and to the enzymes which catalyze acetylation. This is a phase II conjugation reaction, in which an acetyl group is transformed into toxic substance, resulting in limitations to an organism’s ability to respond to the challenge of exposure.
Genetic susceptibility markers often provide surprising causal explanations for atypical reactions to environmental toxins. Because of ethical reservations, they will not be a permitted component of biomonitoring at the workplace in Germany. They are currently only used to advise patients and employers with specific interests and for scientific studies. For example, susceptibility markers can record enzyme polymorphisms and immunomodulation, providing additional evidence for a potential increase in the risk of illness, relevant to occupational or environmental medicine (3, 25).
Practical aspects
Biomonitoring can be used to measure hazardous substances, independently of whether they were taken up by inhalation, through the skin, or orally (10, 25, e1). Effect biomonitoring also allows the assessment of health risks from anthropogenic substances which trigger organ or systemic reactions. The available analytical methods for urine and/or blood samples must be used specifically, together with a detailed medical history, in diagnosis, which might have to be performed by a specialist (e2). Indications should be guided by any present symptoms consistent with possible exposure to a hazardous substance. The time of sampling (interval after exposure) is also relevant. It is particularly important that the time of blood or urine sampling should be given for highly volatile hazardous substances. The correct choice of sample vessels is also essential. For example, headspace vials must be used for blood tests for residues of solvents such as benzene and its analogues.
Reliability of the analytical procedures
Biomonitoring is only of practical value if it employs analytical methods which have been validated with respect to specificity, limit of detection, reliability, and routine use (11). Sound knowledge of the metabolism of the foreign substance and of its toxicokinetics is also required. Internal and external quality assurance is also an essential component of biomonitoring in environmental and occupational medicine. As part of external quality assurance, the German Society for Occupational and Environmental Medicine (Deutsche Gesellschaft für Arbeits- und Umweltmedizin, DGAUM) organizes interlaboratory comparisons twice yearly, in accordance with the German Medical Association’s guideline of 16 January 1987, 16 October 1987, and 24 August 2001. This "German external quality assessment" currently includes more parameters and participants than any other external quality assessment schemes in the world (www.g-equas.de).
Acknowledgments
Translated from the original German by Rodney A. Yeates, M.A., Ph.D.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measurements: New York City, 2002-2003. Am J Public Health. 2005;95:1016–1023. doi: 10.2105/AJPH.2004.058164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ärztliche Mitteilungen von BfR 2006. www.bfr.bund.de/cm/aerztliche_mitteilungen_bei_vergiftungen_2006.pdf
- 3.Angerer J, Ewers U, Wilhelm M. Human Biomonitoring: state of the art. Int J Hyg Env Health. 2007;210:201–228. doi: 10.1016/j.ijheh.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 4.Bader M, Wrbitzky R. Biomonitoring in der arbeitsmedizinischen Diagnostik. Dtsch Med Wochenschr. 2007;132:485–486. doi: 10.1055/s-2007-970374. [DOI] [PubMed] [Google Scholar]
- 5.Angerer J, Mannschreck C, Gündel J. Biological monitoring and biochemical effect monitoring of exposure to polycyclic aromatic hydrocarbons. Int Arch Occup Environ Health. 1997;70:365–377. doi: 10.1007/s004200050231. [DOI] [PubMed] [Google Scholar]
- 6.Baur X, Ollesch T, Budnik LT, Finger S, Matz G. Begasungsmittel und toxische Industriechemikalien in Importcontainern. Zbl Arbeitsmed Umweltmed. 2007;57:89–104. [Google Scholar]
- 7.Wilhelm M, Pesch A, Rostek U, Begerow J, Schmitz N, Idel H, Ranft U. Concentrations of lead in blood, hair and saliva of German children living in three different areas of traffic density. Sci Total Environ. 2002;297:109–118. doi: 10.1016/s0048-9697(02)00101-8. [DOI] [PubMed] [Google Scholar]
- 8.Wittsiepe J, Fürst P, Schrey P, Lemm F, Kraft M, Eberwein G, Winneke G, Wilhelm M. PCDD/ and dioxin-like PCB in human blood and milk from German mothers. Chemosphere. 2007;67:286–294. doi: 10.1016/j.chemosphere.2006.05.118. [DOI] [PubMed] [Google Scholar]
- 9.Koch HM, Drexler H, Angerer J. An estimation of the daily intake of di(2-ethylhexyl)phthalate (DEHP) and other phthalates in the general population. Int J Hyg Environ Health. 2003;206:77–83. doi: 10.1078/1438-4639-00205. [DOI] [PubMed] [Google Scholar]
- 10.Angerer J, Bolt HM, Brüning T, et al. Über das Biomonitoring, den Unwillen Gesundheitsrisiken rational abzuschätzen und die Lust an radikalen Maßnahmen. Umweltmed Forsch Prax. 2004;9:61–64. [Google Scholar]
- 11.Angerer J, Schaller KH, editors. Analysis of hazardous substances in biological materials/biomonitoring methods, vols. 1-10. Methodensammlung der DFG zur Prüfung gesundheitsschädlicher Arbeitsstoffe. Wiley-VCH Verlag: Weinheim; 1985-2007. [Google Scholar]
- 12.Giesen T. Ärztliche Untersuchung im Arbeitsverhältnis. Arbeitsmed Sozialmed Umweltmed. 2007;42:646–655. [Google Scholar]
- 13.Bundesministerium für Arbeit und Soziales. Verordnung zur arbeitsmedizinischen Vorsorge. www.bmas.de/portal/30018/
- 14.Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Ausschuss für Gefahrstoffe, a) www.baua.de/prax/ags/trgs.htm, b) Technische Regel für Gefahrstoffe 710. www.baua.de/nn_16802/de/Themen-von-A-Z/Gefahrstoffe/TRGS/pdf/TRGS-710.pdf?, c) TRGS 903: Verzeichnis der biologischen Grenzwerte http://www.baua.de/nn_16810/de/Themen-von-A-Z/Gefahrstoffe/TRGS/pdf/TRGS-903.pdf? [25.08.2008], d) Risikowerte und Exposition-Risiko-Beziehungen für Tätigkeit mit krebserzeugenden Gefahrstoffen. www.baua.de/nn_78674/de/Themen-von-A-Z/Gefahrstoffe/TRGS/pdf/Bekanntmachung-910.pdf [25.08.2008]
- 15.Smola A, Klein H. Risikobasiertes Grenzwertkonzept für krebserzeugende Stoffe Gefahrstoffe - Reinhaltung der Luft. 2008;68 [Google Scholar]
- 16.Deutsche Forschungsgemeinschaft. Maximale Arbeitsplatzkonzentration und Biologische Arbeitsstofftoleranzwerte MAK- und BAT-Werte-Liste. Mitteilung 44. Weinheim: Wiley-VCH; 2008. [Google Scholar]
- 17.Deutsche Forschungsgemeinschaft. Biological monitoring-prospects in occupational and environmental medicine. In: Angerer J, editor. Weinheim: Wiley-VCH; 2002. [Google Scholar]
- 18.Deutsche Forschungsgemeinschaft Gesundheitsschädliche Arbeitsstoffe. Toxikologisch-arbeitsmedizinische Begründungen von MAK-Werten. Weinheim: Wiley-VCH Verlag; 1972-2006. [Google Scholar]
- 19.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgegesellschaften e.V. Umweltmedizinische AWMF Leitlinie: Human biomonitoring. www.uni-duesseldorf.de/AWMF/ll/002-024.htm. [Google Scholar]
- 20.Schulz C, Angerer J, Ewers U., Kolossa-Gehring M. The German Human Biomonitoring Commission. Int J Hyg Environ Health. 2007;210:375–384. doi: 10.1016/j.ijheh.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 21.Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V. Leitlinie: Benzol-Analoga. www-dgaum.med.uni-rostock.de/leitlinien/benzol.htm.
- 22.California Environmental Protection Agency. Health effects of exposure to environmental tobacco smoke. Sacramento, California: California Environmental Protection Agency; 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deutsches Krebsforschungszentrum. Passivrauchen—ein unterschätztes Gesundheitsrisiko. Heidelberg: Deutsches Krebsforschungszentrum,; 2005. [Google Scholar]
- 24.Heinrich-Ramm R, Wegner R, Garde AH, Baur X. Cotinine excretion (tobacco smoke biomarker) of smokers and non-smokers: comparison of GC/MS and RIA results. Int J Hyg Environ Health. 2002;205:493–499. doi: 10.1078/1438-4639-00173. [DOI] [PubMed] [Google Scholar]
- 25.Angerer J, Bird MG, Burke TA, et al. Strategic biomonitoring initiatives: moving the science forward. Toxicol Sci. 2006;93:3–10. doi: 10.1093/toxsci/kfl042. [DOI] [PubMed] [Google Scholar]
- e1.Schulz C, Conrad A, Becker K, Kolossa-Gehring M, Seiwert M. 20 years of German Environmental Survey (GerES): human biomonitoring and trends over time. Int J Hyg Environ Health. 2007;210:271–297. doi: 10.1016/j.ijheh.2007.01.034. [DOI] [PubMed] [Google Scholar]
- e2.Herr C, Otterbach I, Nowak D, Homberg C, Eikmann T, Wiesmüller GA. Clinical Environmental Medicine. Dtsch Arztebl Int. 2008;105(30):523–531. doi: 10.3238/arztebl.2008.0523. [DOI] [PMC free article] [PubMed] [Google Scholar]