Abstract
Rationale: Simvastatin inhibits inflammatory responses in vitro and in murine models of lung inflammation in vivo. As simvastatin modulates a number of the underlying processes described in acute lung injury (ALI), it may be a potential therapeutic option.
Objectives: To investigate in vivo if simvastatin modulates mechanisms important in the development of ALI in a model of acute lung inflammation induced by inhalation of lipopolysaccharide (LPS) in healthy human volunteers.
Methods: Thirty healthy subjects were enrolled in a double-blind, placebo-controlled study. Subjects were randomized to receive 40 mg or 80 mg of simvastatin or placebo (n = 10/group) for 4 days before inhalation of 50 μg LPS. Measurements were performed in bronchoalveolar lavage fluid (BALF) obtained at 6 hours and plasma obtained at 24 hours after LPS challenge. Nuclear translocation of nuclear factor-κB (NF-κB) was measured in monocyte-derived macrophages.
Measurements and Main Results: Pretreatment with simvastatin reduced LPS-induced BALF neutrophilia, myeloperoxidase, tumor necrosis factor-α, matrix metalloproteinases 7, 8, and 9, and C-reactive protein (CRP) as well as plasma CRP (all P < 0.05 vs. placebo). There was no significant difference between simvastatin 40 mg and 80 mg. BALF from subjects post-LPS inhalation induced a threefold up-regulation in nuclear NF-κB in monocyte-derived macrophages (P < 0.001); pretreatment with simvastatin reduced this by 35% (P < 0.001).
Conclusions: Simvastatin has antiinflammatory effects in the pulmonary and systemic compartment in humans exposed to inhaled LPS.
Clinical trial registered with www.controlled-trials.com (ISRCTN21056528).
Keywords: cytokines, matrix metalloproteinases, endotoxin, nuclear factor-κB, simvastatin, acute lung injury
AT A GLANCE COMMENTARY
Scientific Knowledge on the Subject
Pharmacologic therapies have not proven to be effective for acute lung injury (ALI). Experimental data suggest simvastatin has potential as a treatment for ALI. It is unknown if simvastatin reduces pulmonary inflammation in vivo in humans.
What This Study Adds to the Field
Simvastatin pretreatment has antiinflammatory effects in the pulmonary compartment in a model of ALI induced by inhaled lipopolysaccharide in humans.
The development of acute lung injury (ALI) is characterized by macrophage-mediated (1) and neutrophil-mediated (2) injury associated with the release of inflammatory cytokines and proteases, particularly matrix metalloproteinases (MMPs) (3). MMPs are inhibited in vivo by the tissue inhibitors of metalloproteinases (TIMPs) and the balance between MMPs and their inhibitors is critical in determining pathological outcomes (4). The uncontrolled local inflammatory response in ALI contributes to alveolar epithelial and capillary endothelial barrier damage, exudation of protein-rich edema fluid into the alveolar space leading to the development of noncardiogenic pulmonary edema (5). An associated excessive systemic inflammatory response is implicated in the development of multiple organ failure related to ALI (6).
Hydroxyl-methylglutaryl coenzyme A reductase inhibition with statins is a promising potential new therapeutic option in ALI as they modulate a number of the underlying processes described in ALI. Plasma TNF-α concentrations fall with simvastatin therapy in patients with hypercholesterolemia and coronary artery disease (7). In vitro statins reduce macrophage MMP production (8, 9). Simvastatin reduces endothelial permeability in vitro (10) and in an animal model of lung injury after intratracheal LPS instillation (11). In addition, statins attenuate lung injury in vivo in animal models including ischemia-reperfusion (12), peritonitis (13), and aerosolized LPS (11, 14). Most (15–17) but not all (18) observational studies have suggested a benefit of statins in patients with pneumonia, supporting a potential role in modulating pulmonary inflammation. Moreover, simvastatin, at a dose of 80 mg for 4 days, attenuated the systemic inflammatory response to intravenous lipopolysaccharide (LPS) challenge in healthy human subjects (19). However, no previous study has examined if simvastatin can reduce LPS-induced pulmonary inflammation in vivo in humans. Inhalation of low-dose LPS has been used in healthy humans as an in vivo model of pulmonary inflammation without causing adverse events. Reflecting findings in ALI, LPS inhalation results in a local subclinical alveolar and systemic inflammatory response (20–22).
The objective of the present study was to investigate if a clinically relevant dose of simvastatin reduces pulmonary and systemic inflammation induced by LPS inhalation in humans.
Some of the results of these studies have been previously reported in the form of abstracts (23–25).
METHODS
Subjects
Thirty healthy subjects (age 25.8 ± 5.5 yr) were recruited by advertising. Screening consisted of a history and physical examination, routine blood investigation, ECG, and spirometry. Further details of the exclusion criteria are provided in the online supplement. The study was approved by the local research ethics committee, and written informed consent was obtained from all subjects before enrollment in the study.
Study Design
This was a randomized, double-blind, placebo-controlled clinical trial. Randomization to simvastatin 40 mg, 80 mg, or placebo (1:1:1) was performed by an independent clinical trials pharmacist using Prisym clintrial (Prisym, Wokingham, UK). When an eligible subject was recruited, the clinical trials pharmacist allocated the subject to the designated treatment group, maintaining blinding. Blinding of the simvastatin tablets and placebo was achieved by encapsulation with a gelatin capsule. The simvastatin capsule contained the simvastatin tablet with lactose powder. The placebo capsule contained lactose powder only. Both the simvastatin and placebo study drugs had an identical appearance. Subjects took the study medication for 4 days before inhalation of LPS. On the morning of Day 4, 1 hour after the study medicine was taken under direct observation by the study team, subjects inhaled LPS.
LPS (Escherichia coli serotype O26:B6; Sigma Chemicals, Poole, Dorset, UK) was dissolved in endotoxin-free sterile 0.9% saline and inhaled via an automatic inhalation–synchronized dosimeter nebulizer (Spira, Hameenlinna, Finland) as described in the online supplement. The total dose of inhaled LPS was 50 μg. This dose has previously been demonstrated to induce a local alveolar and systemic inflammatory response (21, 22).
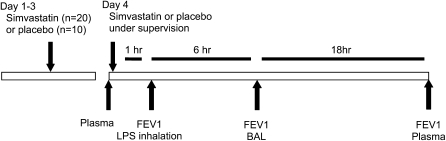
Blood was collected on Day 4 before the subject took the final dose of the study drug and at 24 hours after LPS inhalation. Bronchoalveolar lavage (BAL) was performed 6 hours after LPS inhalation. BAL and processing of bronchoalveolar lavage fluid (BALF) and blood were performed as described in the online supplement. The study design is summarized in Figure 1.
Figure 1.
Study design. Subjects were randomized to receive 40 mg simvastatin (n = 10), 80 mg simvastatin (n = 10), or placebo (n = 10) for 4 days before LPS inhalation. Bronchoaveolar lavage (BAL) was undertaken at 6 hours after lipopolysaccharide (LPS) inhalation and plasma was collected before subjects took the Day 4 medication under direct observation of the study team, 1 hour before LPS inhalation and at 24 hours after LPS inhalation.
Assays
Plasma concentrations of simvastatin and its main active metabolite, simvastatin acid, were measured on Day 4 before the subject took the final dose of study drug, which was administered under supervision (1 h before LPS inhalation), as previously described (26). Additional assay details are provided in the online supplement. Myeloperoxidase (MPO) (27), neutrophil elastase:α-1-antitrypsin (NE:α-1-AT) complex (28), TIMPs and C-reactive protein (CRP) (R&D Systems; Abingdon, UK) were measured by ELISA. LPS concentration was measured in BALF using the limulus ameobocyte lysate chromogenic endpoint assay (29). Total protein concentration was assayed using the Qubit protein assay kit (Invitrogen; Paisley, UK). Cytokines and chemokines (IL-1ra, IL-1β, TNF-α, IL-6, IL-8, IL-10 and MCP-1) and MMPs (MMP-1, 2, 3, 7, 8, 9, 12 and 13) were measured using a cytometric bead array (R&D Systems; Abingdon, UK). These MMPs were chosen because they are the most important expressed pulmonary MMPs (30).
Flow Cytometric Analysis
Cell suspensions (2.5 × 105 BAL cells) were washed twice with phosphate buffered saline/1% bovine serum albumin and resuspended in the binding buffer supplied with the annexin V-FITC (fluorescein isothiocyanate) (Pharmingen; Oxford, UK). Cell suspensions were then labeled with annexin V-FITC (AV) and propidium iodide (PI) (Pharmingen). Flow cytometry was performed as previously described (31). Full experimental details are provided in the online supplement.
Nuclear Factor-κB Measurement
Monocytes were isolated from peripheral blood of healthy volunteers by centrifugation across a Ficoll-Paque gradient and adherence and matured into monocyte-derived macrophages (MDMs) as previously described (32). Full experimental details are provided in the online supplement. Cytoplasmic and nuclear extracts were prepared using a Perbio N-PER nuclear and cytoplasmic extraction kit as previously described (32), and protein content was quantified. Relative concentration of NF-κB in 5 μg nuclear protein was measured using the TransAM NF-B p65 transcription factor assay kit (Active Motif; Rixensart, Belgium), according to the manufacturer's instructions (32).
In Vitro Effect of Simvastatin on LPS-induced MMP Secretion
In vitro studies were performed to examine the effect of simvastatin pretreatment on LPS-induced MMP secretion by neutrophils, MDMs, and alveolar epithelial cells. Full experimental details are provided in the online supplement.
Statistical Analysis
Data are expressed as mean (SD) or median (interquartile range [IQR]). The a priori analysis plan was to compare the combined simvastatin and placebo groups. A secondary analysis to determine if there was a dose-dependent response was also planned. Data were tested for normality and analyzed by unpaired t tests or Mann-Whitney U test as appropriate. A χ2 or Fisher's exact test was used to compare proportions. Data were analyzed using GraphPad Prism (version 4.02, GraphPad Software; San Diego, CA). A P value of 0.05 was considered significant.
RESULTS
There were no differences in baseline parameters, including age or sex, between the groups randomized to receive placebo or simvastatin (Table 1). There was no difference between the 40 and 80 mg simvastatin groups for any of the outcome measures. The data for the combined simvastatin group is presented. There were no significant changes in FEV1 and FVC, oxygenation saturation measured by pulse oximetry, or vital signs over the course of the study. In the simvastatin-treated group, there was a significant reduction in mean (SD) change in plasma cholesterol concentrations compared with the placebo group in which plasma cholesterol was unchanged (−0.63 [0.27] vs. 0.01 [0.38] mmol/L in the placebo-treated group; P = 0.0001).
TABLE 1.
BASELINE CHARACTERISTICS OF VOLUNTEERS IN THE DIFFERENT GROUPS
| Placebo (n = 10) | Simvastatin (n = 20) | |
|---|---|---|
| Age, years | 25.8 (4.49) | 25.8 (6.01) |
| Sex, male:female, n | 5:5 | 9:11 |
| Height, m | 1.68 (0.08) | 1.69 (0.08) |
| Weight, kg | 74.17 (9.58) | 68.13 (10.58) |
| Baseline FEV1, L | 3.88 (0.73) | 3.60 (0.67) |
| Baseline FVC, L | 4.58 (0.92) | 4.27 (0.81) |
Statistical significance was P > 0.05 for all comparisons between placebo and simvastatin groups.
Plasma concentrations of simvastatin and its main active metabolite, simvastatin acid, were detectable in all subjects receiving simvastatin and were below the limit of detection in subjects receiving the placebo. Mean (SD) plasma concentrations of simvastatin and simvastatin acid were 4.7 (9.5) and 1.1 (1.4) ng/ml in the simvastatin group, respectively. No severe or unexpected adverse events occurred in either group. Additional details on the procedure for adverse-event monitoring and adverse events are provided in the online supplement. LPS was detectable in BALF, confirming that LPS was delivered to the distal airspace. There was no difference in LPS concentrations between the two groups (data not shown).
Effects of Simvastatin on LPS-induced Pulmonary Neutrophil Accumulation
Simvastatin pretreatment reduced neutrophilia in the alveolar space after LPS inhalation (P = 0.05 vs. placebo). There was no significant reduction in the total cell count, macrophages, or lymphocytes (Table 2).
TABLE 2.
EFFECTS OF SIMVASTATIN ON LIPOPOLYSACCHARIDE-INDUCED BRONCHOALVEOLAR LAVAGE FLUID CELL COUNTS
| Placebo (n = 10) | Simvastatin (n = 20) | P Value | |
|---|---|---|---|
| Total cells, × 105/ml | 15.2 (10.3–49.8) | 10.7 (4.6–17.4) | 0.2 |
| Neutrophils | 8.5 (4.4–16.2) | 3.0 (1.8–8.1) | 0.05 |
| Macrophages | 7.0 (3.1–19.1) | 5.1 (2.1–13.0) | 0.48 |
| Lymphocytes | 1.1 (0.6–3.2) | 0.9 (0.2–1.6) | 0.37 |
Healthy human volunteers inhaled 50 μg lipopolysaccharide (LPS). Simvastatin or placebo was administered for 4 days before LPS inhalation. Total and differential cell counts were determined in bronchoaveolar lavage fluid 6 hours after inhalation of LPS.
Values are medians (interquartile range).
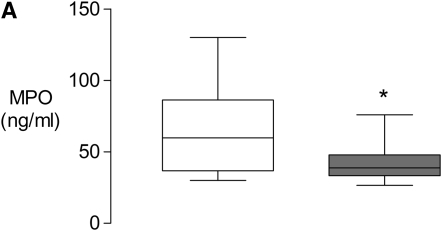
Simvastatin decreased MPO concentrations (P = 0.04 vs. placebo; Figure 2A). The neutrophil releases NE during lung inflammation. NE, which is a neutrophil serine protease, has high affinity for α-1-AT, a serine protease inhibitor present at high concentrations in the respiratory tract. NE forms a covalent complex with α-1-AT. Therefore, elevated NE:α-1-AT complex levels reflect an increase in activated neutrophil numbers in the lung. Simvastatin also decreased the concentrations of NE:α-1-AT complex although this difference did not reach statistical significance (P = 0.07; Figure 2B).
Figure 2.
Effect of simvastatin on lipopolysaccharide (LPS)-induced neutrophil recruitment. Healthy human volunteers inhaled 50 μg LPS. Simvastatin or placebo was administered for 4 days before LPS inhalation. Bronchoaveolar lavage fluid (BALF) was obtained 6 hours after inhalation of LPS, and supernatants were analyzed for (A) myeloperoxidase and (B) neutrophil elastase:α-1-antitrypsin complex (NE: α-1-AT). Open bars = placebo; solid bars = simvastatin. Data are shown for the 10 subjects in the placebo group and the 20 subjects in the combined simvastatin group. Data are medians (IQR). * P < 0.05 versus placebo.
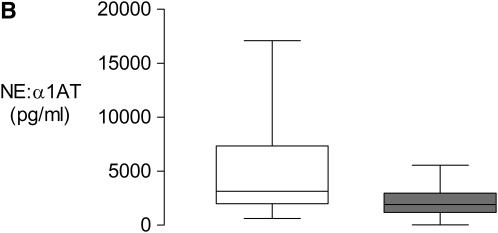
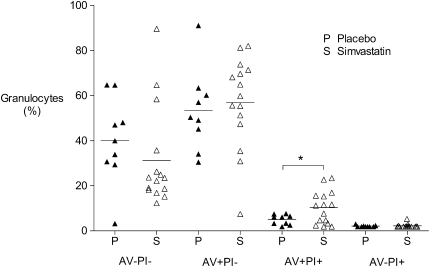
Effects of Simvastatin on Pulmonary Neutrophil Apoptosis
Pretreatment with simvastatin significantly increased the mean (SD) number of neutrophils in late apoptosis, as identified by cells labeled with annexin V-FITC (AV) and propidium iodide (PI) (AV+PI+), compared with placebo, (10.3% [7.3] vs. 5.0% [2.2]; P = 0.05 vs. placebo). There was a high incidence of early apoptosis (AV+PI−). Although not significant there was a small increase in the percentage of granulocytes in early apoptosis (P = 0.7) as well as a reduction in viable cells (AV−PI−) compared with placebo (P = 0.3). There were no significant differences in necrotic (AV−PI+) granulocyte numbers (P = 0.7; Figure 3). Data were available for 9 subjects in the placebo group and 15 subjects in the simvastatin group. Additional details are provided in the online supplement.
Figure 3.
Effect of simvastatin on neutrophil apoptosis. Healthy human volunteers inhaled 50 μg lipopolysaccharide (LPS). Simvastatin or placebo was administered for 4 days before LPS inhalation. Bronchoaveolar lavage fluid (BALF)was obtained 6 hours after inhalation of LPS. Neutrophil apoptosis analyzed by flow cytometry for BAL cells labeled with either annexin V (AV) or propidium iodide (PI). Cells labeled with neither AV nor PI (AV−/PI−) are viable, cells labeled with AV only (AV+/PI−) indicate early apoptosis, cells labeled with AV and PI (AV+/PI+) indicate those in late stage apoptosis, and cells labeled with PI only (AV−/PI+) indicate necrotic cells. Data are shown as individual points; the horizontal lines represent mean values. Data are available for 9 subjects in the placebo group and 15 subjects in the simvastatin group. *P < 0.05 versus placebo.
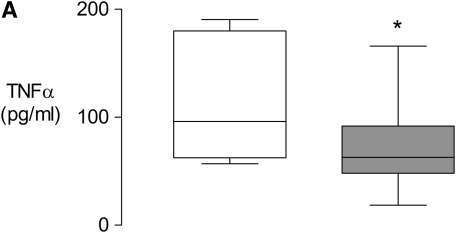
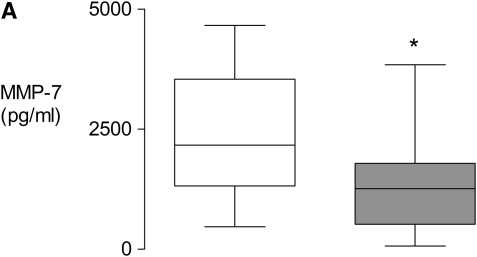
Simvastatin Reduces LPS-induced TNF-α Concentration
There were no differences in mean (SD) BALF protein concentrations between placebo-treated or simvastatin-treated subjects (0.265 [0.070]) vs. 0.235 [0.083] mg/ml, respectively; P = 0.3 vs. placebo). Simvastatin reduced TNF-α concentrations in BALF after LPS challenge (P = 0.04; Figure 4A). Simvastatin also decreased IL-1β but this did not reach statistical significance (P = 0.07; Figure 4B). There was no significant decrease in other cytokines and chemokines measured (data not shown).
Figure 4.
Simvastatin inhibits lipopolysaccharide (LPS)-induced tumor necrosis factor (TNF)-α concentration. Healthy human volunteers inhaled 50 μg LPS. Simvastatin or placebo was administered for 4 days before LPS inhalation. Bronchoaveolar lavage fluid (BALF) was obtained 6 hours after inhalation of LPS and supernatants were analyzed for (A) TNF-α and (B) IL-1β. Data are shown for the 10 subjects in the placebo group and the 20 subjects in the combined simvastatin group. Open bars = placebo; solid bars = simvastatin. Data are medians (interquartile range). *P < 0.05 versus placebo.
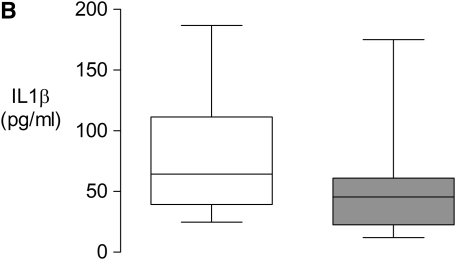
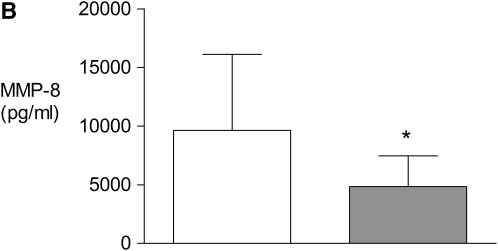
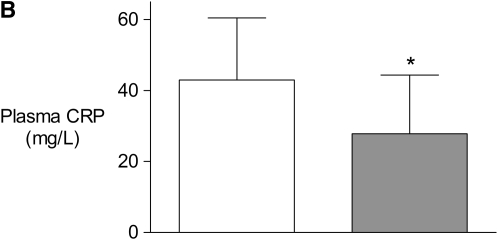
Simvastatin Reduces LPS-induced MMP Concentration
Simvastatin reduced MMP-7 (P = 0.03 vs. placebo; Figure 5A), MMP-8 (P = 0.007; Figure 5B) and MMP-9 (P = 0.04; Figure 5C) concentrations in BALF after LPS challenge. Simvastatin also decreased mean (SD) MMP-2 but this was not significant (560 [298] vs.725 [392] pg/ml in the placebo-treated group; P = 0.2). Other measured MMPs were not detectable. Simvastatin did not affect median (interquartile range) TIMP-1 (4,600 [2,800–8,000] vs. 3,480 [2,800–5,780] pg/ml in the placebo-treated group; P = 0.3) or mean (SD) TIMP-2 (1,337 [621] vs.1217 [439] pg/ml in the placebo-treated group; P = 0.5) concentrations in BALF after LPS challenge.
Figure 5.
Simvastatin inhibits lipopolysaccharide (LPS)-induced matrix metalloproteinase (MMP) concentration. Healthy human volunteers inhaled 50 μg LPS. Simvastatin or placebo was administered for 4 days before LPS inhalation. Bronchoaveolar lavage fluid (BALF) was obtained 6 hours after inhalation of LPS and supernatants were analyzed for (A) MMP-7, (B) MMP-8, and (C) MMP-9. Data are shown for the 10 subjects in the placebo group and the 20 subjects in the combined simvastatin group. Open bars = placebo; solid bars = simvastatin. Data for MMP-7 are medians (interquartile range). *P < 0.05 versus placebo.
In in vitro pretreatment with simvastatin had no effect on LPS-induced neutrophil MMP-8/MMP-9 secretion or epithelial cell MMP-7/MMP-9 secretion. In contrast, in MDMs, simvastatin significantly reduced LPS-induced MMP-9 secretion with a trend to a reduction in MMP-7 secretion. Additional data are provided in the online supplement.
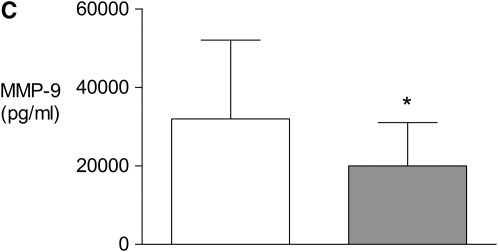
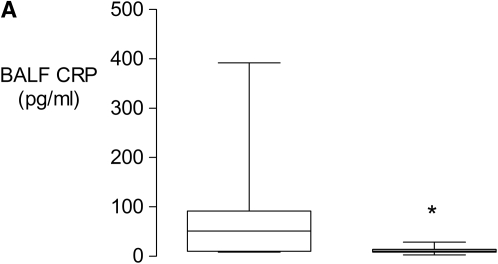
Simvastatin Decreases Pulmonary and Systemic LPS-induced CRP Production
Simvastatin inhibited the increase in BALF CRP after LPS challenge (P = 0.01; Figure 6A). In addition, the increase in plasma CRP after LPS challenge was significantly attenuated by pretreatment with simvastatin (P = 0.03; Figure 6B).
Figure 6.
Simvastatin inhibits lipopolysaccharide (LPS)-induced pulmonary and systemic C-reactive protein (CRP) production. Healthy human volunteers inhaled 50 μg LPS. Simvastatin or placebo was administered for 4 days before LPS inhalation. CRP was measured in bronchoaveolar lavage fluid (BALF) obtained at (A) 6 hours and in plasma obtained at (B) 24 hours after LPS inhalation. Data are shown for the 10 subjects in the placebo group and the 20 subjects in the combined simvastatin group. Open bars = placebo; solid bars = simvastatin. Data for BALF CRP are medians (interquartile range). *P < 0.05 versus placebo.
Simvastatin Decreases LPS-induced NF-κB Translocation in Macrophages
Stimulation of MDMs with BALF from LPS-challenged subjects induced nuclear translocation of NF-κB by approximately threefold (P < 0.001). BALF from subjects pretreated with simvastatin induced significantly less nuclear translocation of NF-κB. Pretreatment of MDMs with 5 μM simvastatin for 4 hours, followed by stimulation with BALF from the placebo group, also attenuated the induction of nuclear NF-κB (Figure 7; P < 0.001).
Figure 7.
Simvastatin pretreatment reduces nuclear NF-κB translocation. Healthy human volunteers inhaled 50 μg lipopolysaccharide (LPS). Simvastatin or placebo was administered for 4 days before LPS inhalation. Monocyte-derived macrophages (MDMs) were pretreated with 5 mM simvastatin or medium control for 4 hours before stimulation with pooled bronchoaveolar lavage fluid (BALF) from subjects who had been pretreated with statin or placebo. Cells were lysed at 1 hour, and relative nuclear concentrations of the p65 subunit of NF-κB were measured. Data represent duplicate readings from MDMs from three separate volunteers, *P = 0.0001 for control versus placebo BALF, **P = 0.03 for placebo BALF versus simvastatin BALF, #P = 0.03 for placebo BALF versus simvastatin + placebo BALF.
DISCUSSION
Several studies have documented the beneficial effects of statins in vitro and in vivo in experimental animal models of pulmonary inflammation (11–13). This is the first study to investigate the effects of a statin in vivo on LPS-induced pulmonary inflammation in humans. Simvastatin was found to have several antiinflammatory effects. In particular, there was a reduction in neutrophil numbers and activity in the alveolar space that is mediated, at least in part, by increased neutrophil apoptosis. We also demonstrated reduced alveolar concentrations of TNF-α and MMP-7, 8, and 9, and showed a reduction in both BALF and plasma CRP. We propose that, in addition to the reduction in neutrophil numbers and activity, these effects are also mediated, in part, by reduced macrophage NF-κB nuclear translocation in the presence of simvastatin.
Reflecting findings in ALI, the inhalation of nebulized LPS in the healthy human results in a local alveolar inflammation characterized by neutrophilic influx and an increase in proinflammatory cytokines in BALF as well as an associated systemic inflammatory response (20–22). Furthermore, macrophages have been identified as a major source of inflammatory proteins in response to inhaled LPS in the human lung (20) and respond vigorously to LPS in vitro (33–35).
In this study, simvastatin reduced the number of neutrophils in the lungs after LPS inhalation. It is likely that the reduction of pulmonary neutrophils is related to both reduced influx and increased apoptosis. Interestingly, we demonstrated a reduction in BALF MMP-7 in response to simvastatin. MMP-7 has been shown to be necessary to create the chemokine gradient required for neutrophil influx to the lung in animal models of ALI (36). We have also shown that simvastatin increased neutrophil apoptosis in the alveolar compartment. This is the first description of an increase in pulmonary neutrophil apoptosis in vivo in humans in response to statin treatment. In contrast to necrosis, neutrophil apoptosis limits inflammation. During apoptosis, neutrophil secretory processes are shut down, and the intact senescent neutrophil is removed by macrophages. As this process does not trigger the release of proinflammatory mediators, there is decreased alveolar inflammation (37). This data is in keeping with data showing that statins induce neutrophil apoptosis in vitro (38) and in the systemic circulation following cardiopulmonary bypass (39). This increase in alveolar neutrophil apoptosis may be related to reduced pulmonary CRP concentrations. CRP can inhibit neutrophil apoptosis (40) and plasma CRP has been suggested to have a role in the delayed neutrophil apoptosis seen in cystic fibrosis (41). Importantly, decreased pulmonary neutrophilia occurred along with increased neutrophil apoptosis. This indicates that the induction of neutrophil apoptosis by simvastatin does not overcome the capacity to clear apoptotic cells. This is in keeping with data that statins augment clearance of apoptotic neutrophils (42). Whereas apoptosis measurement by annexin V and propidium iodide staining is unique in that it specifically allows the identification of early- and late-stage apoptosis as well as necrotic cells, a limitation of this data is that only a single method to measure neutrophil apoptosis was used, which may not be regarded as definitive.
Furthermore, there was decreased neutrophilic inflammation as measured by decreased BALF MPO and MMP-8, which is secreted only by neutrophils. In addition, NE:α-1-AT complex was decreased, although this failed to reach statistical significance. These findings extend previous findings from experimental animal models in which simvastatin decreased pulmonary neutrophilia and neutrophil activity in LPS (11), and ischemia reperfusion (12, 43) induced pulmonary inflammation.
Simvastatin reduced the release of TNF-α induced by LPS inhalation. This is the first study to find this effect in the pulmonary compartment in humans, although previous animal studies have demonstrated that statins attenuate TNF-α release in BALF after intratracheal administration of LPS in mice (44). TNF-α is characteristically induced in, and secreted by, LPS-stimulated alveolar macrophages (33, 35) and is NF-κB–dependent (45).
Simvastatin also reduced the release of MMP-7, 8, and 9 induced by LPS inhalation without any reduction in TIMP-1 and TIMP-2. The decrease in unopposed protease activity mediated by MMP concentrations will reduce matrix degradation and resulting epithelial and endothelial injury. In our in vitro experiments (see online supplement) statins inhibited only LPS-induced MMP secretion by macrophages. Broad spectrum MMP inhibition has attenuated acute lung inflammation in acute experimental models (46). This is the first study to find that statins reduce MMP production associated with pulmonary inflammation in vivo, although statins have been shown to reduce MMP-7 (47) and MMP-9 (8, 9, 48) secretion by human monocyte-derived macrophages in vitro.
As well as reducing pulmonary inflammation, pretreatment with simvastatin was found to decrease the systemic inflammatory responses induced by LPS inhalation as measured by plasma CRP. This is in keeping with a previous report that demonstrated pretreatment with simvastatin decreased the systemic increase in CRP induced by intravenous administration of LPS (19). The current data extend these findings to confirm that simvastatin has a systemic antiinflammatory effect following an insult initiated in the pulmonary compartment. This has potential implications for the treatment of ALI, given that pneumonia is one of the most common initiating stimuli in the development of ALI and that an associated excessive systemic inflammatory response is implicated in the development of multiple organ failure associated with ALI (6).
LPS stimulates the induction of several inflammatory genes via the NF-κB pathway (49), and inhaled LPS is known to cause alveolar macrophage activation (20). In addition, LPS stimulation of AMs is known to induce NF-κB–dependent TNF-α and IL-1β secretion (34, 35), particularly in comparison with other potential sources in the inflamed alveolus (33). Our data suggest that simvastatin specifically reduces TNF-α (and IL-1β), and it also reduced secretion of two key macrophage-derived proteases (MMP-7/MMP-9) in vivo. In vitro we were able to demonstrate little induction of MMPs in either neutrophils or epithelial cells in response to LPS (see online data supplement). However, there was induction of MMP-7/MMP-9 in macrophages, with a tendency to reduction in MMP-7 and a marked reduction in MMP-9 in response to statin pretreatment. These data suggest that, in addition to simvastatin reducing neutrophil inflammation, it may also specifically modulate macrophage activation.
This led us to investigate the activation of NF-κB in MDMs by BALF in an in vitro model. We found that simvastatin reduced macrophage NF-κB activation in this complex cytokine environment, and thus identifying an important potential mechanism for the observed antiinflammatory effect of simvastatin in vivo. This is in keeping with previous data showing statins prevent NF-κB activation (50). It is important to note that other key macrophage-derived cytokines, including IL-8 and MCP-1, were not reduced in response to simvastatin in the in vivo model. These are characteristically NF-κB–dependent and the failure to show a down-regulation of these in response to simvastatin may relate to the timing of the lavage or may indicate that proinflammatory transcriptional regulators other than NF-κB are important in LPS-induced inflammation but are not inhibited by simvastatin.
As with all experimental models, the use of LPS inhalation as a model of pulmonary inflammation has limitations; it is a short-term noninfectious model associated with a relatively low degree of inflammation. However, despite these issues, the model has clear advantages to allow potentially effective therapies to be readily investigated in vivo in humans to inform subsequent clinical trials in patients. Only a single time-point 6 hours after LPS inhalation was examined; therefore, a kinetic analysis of the effect of simvastatin on pulmonary inflammatory mediators is not possible. Previous studies (20, 22, 51) have demonstrated both neutrophil recruitment and inflammatory protein release 6 hours after LPS inhalation. Given the relatively invasive nature of bronchoscopy and BAL it was not possible, for ethical reasons, to extend the number of time-points. Plasma samples were obtained at 24 hours and did show decreased CRP levels in simvastatin-treated subjects. Whereas an additional control arm using inhaled saline would have demonstrated the inflammatory effect of LPS in normal subjects, as this model to induce alveolar inflammation was already well documented (20, 22), and as the aim of our study was to investigate the effect of simvastatin on alveolar inflammation in vivo, from a scientific and ethical point of view we did not feel it was necessary to include an inhaled saline group as an additional control arm in this study. Although we have postulated that decreased macrophage NF-κB activation is a potential mechanism for the antiinflammatory effects of simvastatin, we did not investigate other potential mechanisms, such as transcriptional regulators other than NF-κB or modulation of adhesion molecule expression. In this study we investigated the effects of pretreatment with simvastatin before LPS inhalation. Although statin therapy may be potentially useful as a preventative strategy, additional studies are required to determine if simvastatin has antiinflammatory effects in the lung if administered after the inflammatory process has already been initiated. Furthermore, as the mode of action among statins is similar, and pleiotropic antiinflammatory actions have been demonstrated for most statins in vitro (52), it is likely that these effects will be similar within this group of drugs; however, further studies are needed to confirm this.
Pretreatment with 80 mg simvastatin for 4 days decreased the systemic inflammation induced by intravenous administration of LPS (19); therefore, based on this data, the current study used a pretreatment for 4 days. As a preventative strategy for patients at risk of ALI, such a short pretreatment course would be practical. More recent data indicate a single dose of 80 mg of simvastatin can reduce CRP levels in patients with stable angina within 48 hours (53). However, it is uncertain if a beneficial effect on pulmonary inflammation could be achieved with a shorter duration of pretreatment than 4 days. In addition, based on previous data (19) and animal data comparing 5 or 20 mg/kg of simvastatin where only the higher dose was effective in attenuating lung injury (11), 80 mg of simvastatin was used to obtain proof of the principle of effect. However, in an attempt to determine the effect of a lower dose, we also examined 40 mg of simvastatin. We found that the 40 and 80-mg groups did not differ, although the study was not powered to identify a difference in inflammatory mediators between the two simvastatin groups. Interestingly, there are data demonstrating a similar reduction of CRP in patients with angina using 20 and 40 mg of pravastatin despite a dose-dependent effect in cholesterol (54). This suggests that whereas the cholesterol-lowering effects are dose related, the antiinflammatory effects may be dose independent and might occur at lower doses, although this remains to be proven. In contrast in the only animal study that compared two doses of simvastatin (5 or 20 mg/kg), only the higher dose was effective in attenuating lung injury (11).
Two ongoing phase 2 clinical trials are investigating the prevention (http://www.controlled-trials.com/ISRCTN56543987) and treatment (http://www.controlled-trials.com/ISRCTN70127774) of ALI with 80 mg of simvastatin. These studies will provide evidence of whether 80 mg of simvastatin is safe and effective at improving important surrogate clinical outcomes. Taken together with the findings from our small study, which was unable to demonstrate a difference between the 40-mg and 80-mg simvastatin groups, and in addition, recent data showing that after a single 20-mg dose of atorvastatin very high plasma concentrations were achieved in intensive care patients with sepsis (55), as the adverse effects associated with statins are dose dependent, subsequent studies will be required to determine which dose will be effective while minimizing adverse effects. Several groups, including the National Institutes of Health–sponsored Acute Respiratory Distress Syndrome network and the Irish Critical Care Trials group, are currently considering undertaking multicenter studies of statins in ALI to address these issues.
In conclusion, this double-blind, randomized, placebo-controlled study provides the first proof of principle that simvastatin has important antiinflammatory effects in the pulmonary compartment in humans challenged with aerosolized endotoxin by reducing both neutrophilic and macrophage inflammation. This human study supports the hypothesis that pretreatment with simvastatin might be of benefit in dampening the excessive pulmonary and systemic inflammation associated with ALI. On the basis of these data, as well as other published studies of experimental lung injury, more studies are needed to determine if the use of simvastatin and other statins after the onset of lung inflammation has the same effect as pretreatment with statins. Studies are also needed to determine the effectiveness of other statins on lung inflammation.
Supplementary Material
Acknowledgments
The authors thank the endoscopy staff of the Belfast City Hospital who participated in this study.
Supported by the Intensive Care Society of Ireland, UK Intensive Care Society, Northern Ireland R&D Office, REVIVE, and NHLBI HL51856 (M.A.M.).
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200810-1584OC on March 26, 2009
Conflict of Interest Statement: M.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.T.W.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. C.M.O. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. T.R.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. V.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. D.R.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.A.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. C.C.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.T.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.S.E. has assisted with an advisory board with Gilead and is undertaking contract research for Vectura. D.F.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Frank JA, Wray CM, McAuley DF, Schwendener R, Matthay MA. Alveolar macrophages mediate epithelial barrier dysfunction in ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol 2006;291:L1191–L1198. [DOI] [PubMed] [Google Scholar]
- 2.Perkins GD, Nathani N, McAuley DF, Gao F, Thickett DR. In vitro and in vivo effects of salbutamol on neutrophil function in acute lung injury. Thorax 2007;62:36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Kane CM, Frank JA, McAuley DF. Matrix metalloproteases; a potential role in the pathogenesis of the acute respiratory distress syndrome. In J. L. Vincent, editor. 24th yearbook of intensive care and emergency medicine. Berlin: Springer-Verlag; 2004. pp. 287–300.
- 4.Gipson TS, Bless NM, Shanley TP, Crouch LD, Bleavins MR, Younkin EM, Sarma V, Gibbs DF, Tefera W, McConnell PC, et al. Regulatory effects of endogenous protease inhibitors in acute lung inflammatory injury. J Immunol 1999;162:3653–3662. [PubMed] [Google Scholar]
- 5.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med 2000;342:1334–1349. [DOI] [PubMed] [Google Scholar]
- 6.Ullrich R, Lorber C, Roder G, Urak G, Faryniak B, Sladen RN, Germann P. Controlled airway pressure therapy, nitric oxide inhalation, prone position, and extracorporeal membrane oxygenation (ECMO) as components of an integrated approach to ARDS. Anesthesiology 1999;91:1577–1586. [DOI] [PubMed] [Google Scholar]
- 7.Koh KK, Ahn JY, Jin DK, Han SH, Kim HS, Choi IS, Ahn TH, Shin EK, Jeong EM. Comparative effects of statin and fibrate on nitric oxide bioactivity and matrix metalloproteinase in hyperlipidemia. Int J Cardiol 2004;97:239–244. [DOI] [PubMed] [Google Scholar]
- 8.Bellosta S, Via D, Canavesi M, Pfister P, Fumagalli R, Paoletti R, Bernini F. HMG-CoA reductase inhibitors reduce MMP-9 secretion by macrophages. Arterioscler Thromb Vasc Biol 1998;18:1671–1678. [DOI] [PubMed] [Google Scholar]
- 9.Nagashima H, Aoka Y, Sakomura Y, Sakuta A, Aomi S, Ishizuka N, Hagiwara N, Kawana M, Kasanuki H. A 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, cerivastatin, suppresses production of matrix metalloproteinase-9 in human abdominal aortic aneurysm wall. J Vasc Surg 2002;36:158–163. [DOI] [PubMed] [Google Scholar]
- 10.Jacobson JR, Dudek SM, Birukov KG, Ye SQ, Grigoryev DN, Girgis RE, Garcia JG. Cytoskeletal activation and altered gene expression in endothelial barrier regulation by simvastatin. Am J Respir Cell Mol Biol 2004;30:662–670. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson JR, Barnard JW, Grigoryev DN, Ma SF, Tuder RM, Garcia JG. Simvastatin attenuates vascular leak and inflammation in murine inflammatory lung injury. Am J Physiol Lung Cell Mol Physiol 2005;288:L1026–L1032. [DOI] [PubMed] [Google Scholar]
- 12.Naidu BV, Woolley SM, Farivar AS, Thomas R, Fraga C, Mulligan MS. Simvastatin ameliorates injury in an experimental model of lung ischemia-reperfusion. J Thorac Cardiovasc Surg 2003;126:482–489. [DOI] [PubMed] [Google Scholar]
- 13.Fischetti F, Carretta R, Borotto G, Durigutto P, Bulla R, Meroni PL, Tedesco F. Fluvastatin treatment inhibits leucocyte adhesion and extravasation in models of complement-mediated acute inflammation. Clin Exp Immunol 2004;135:186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fessler MB, Young SK, Jeyaseelan S, Lieber JG, Arndt PG, Nick JA, Worthen GS. A role for hydroxy-methylglutaryl coenzyme a reductase in pulmonary inflammation and host defense. Am J Respir Crit Care Med 2005;171:606–615. [DOI] [PubMed] [Google Scholar]
- 15.Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sorensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia: population-based cohort study of 29,900 patients. Arch Intern Med 2008;168:2081–2087. [DOI] [PubMed] [Google Scholar]
- 16.Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med 2008;121:1002–1007. [DOI] [PubMed] [Google Scholar]
- 17.Mortensen EM, Restrepo MI, Anzueto A, Pugh J. The effect of priorstatin use on 30-day mortality for patients hospitalized with community-acquired pneumonia. Respir Res 2005;6:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majumdar SR, McAlister FA, Eurich DT, Padwal RS, Marrie TJ. Statins and outcomes in patients admitted to hospital with community acquired pneumonia: population based prospective cohort study. BMJ 2006;333:999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steiner S, Speidl WS, Pleiner J, Seidinger D, Zorn G, Kaun C, Wojta J, Huber K, Minar E, Wolzt M, et al. Simvastatin blunts endotoxin-induced tissue factor in vivo. Circulation 2005;111:1841–1846. [DOI] [PubMed] [Google Scholar]
- 20.Maris NA, de Vos AF, Dessing MC, Spek CA, Lutter R, Jansen HM, van der Zee JS, Bresser P, van der Poll T. Antiinflammatory effects of salmeterol after inhalation of lipopolysaccharide by healthy volunteers. Am J Respir Crit Care Med 2005;172:878–884. [DOI] [PubMed] [Google Scholar]
- 21.Michel O, Nagy A, Schroeven M, Duchateau J, Neve J, Fondu P, Sergysels R. Dose–response relationship to inhaled endotoxin in normal subjects. Am J Respir Crit Care Med 1997;156:1157–1164. [DOI] [PubMed] [Google Scholar]
- 22.Maris NA, de Vos AF, Bresser P, van der Zee JS, Meijers JC, Lijnen HR, Levi M, Jansen HM, van der Poll T. Activation of coagulation and inhibition of fibrinolysis in the lung after inhalation of lipopolysaccharide by healthy volunteers. Thromb Haemost 2005;93:1036–1040. [DOI] [PubMed] [Google Scholar]
- 23.Shyamsundar MS, McKeown S, O'Kane C, Craig T, Megarry J, Elborn JS, McAuley DF. Simvastatin reduces systemic inflammation in an in vivo human endotoxaemic model of lung injury; a randomized placebo-controlled clinical trial. J Intensive Care Soc 2007;9:92. [Google Scholar]
- 24.Shyamsundar MS, McKeown S, Craig T, Elborn JS, McAuley DF. Reduction of pulmonary inflammation by simvastatin in an endotoxaemic model of lung injury in humans; a randomized placebo-controlled clinical trial [abstract]. Am J Respir Crit Care Med 2008;177:A77. [Google Scholar]
- 25.McKeown ST, Shyamsundar M, Kane CO, Calfee CS, Brady S, Craig TR, Elborn JS, Matthay MA, McAuley DF. Matrix metalloproteinase (MMP) downregulation by simvastatin in an endotoxaemic model of ALI in humans: a double-blind, placebo-controlled study [abstract]. Am J Respir Crit Care Med 2008;177:A598. [Google Scholar]
- 26.Zhao JJ, Xie IH, Yang AY, Roadcap BA, Rogers JD. Quantitation of simvastatin and its beta-hydroxy acid in human plasma by liquid-liquid cartridge extraction and liquid chromatography/tandem mass spectrometry. J Mass Spectrom 2000;35:1133–1143. [DOI] [PubMed] [Google Scholar]
- 27.McCann CJ, Glover BM, Menown IBA, Moore MJ, McEneny J, Owens CG, Smith B, Sharpe PC, Young IS, Adgey JA. Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponin T. Eur Heart J 2008;29:2843–2850. [DOI] [PubMed] [Google Scholar]
- 28.Greene C, Taggart C, Lowe G, Gallagher P, McElvaney N, O'Neill S. Local impairment of anti-neutrophil elastase capacity in community-acquired pneumonia. J Infect Dis 2003;188:769–776. [DOI] [PubMed] [Google Scholar]
- 29.Venter P, Abraham M, Lues JF, Ivanov I. The influence of sanitizers on the lipopolysaccharide composition of Escherichia coli O111. Int J Food Microbiol 2006;111:221–227. [DOI] [PubMed] [Google Scholar]
- 30.Elkington PTG, Friedland JS. Matrix metalloproteinases in destructive pulmonary pathology. Thorax 2006;61:259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watt AP, Brown V, Courtney J, Kelly M, Garske L, Elborn JS, Ennis M. Neutrophil apoptosis, proinflammatory mediators and cell counts in bronchiectasis. Thorax 2004;59:231–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Kane CM, Boyle JJ, Horncastle DE, Elkington PT, Friedland JS. Monocyte-dependent fibroblast CXCL8 secretion occurs in tuberculosis and limits survival of mycobacteria within macrophages. J Immunol 2007;178:3767–3776. [DOI] [PubMed] [Google Scholar]
- 33.Thorley AJ, Ford PA, Giembycz MA, Goldstraw P, Young A, Tetley TD. Differential regulation of cytokine release and leukocyte migration by lipopolysaccharide-stimulated primary human lung alveolar type II epithelial cells and macrophages. J Immunol 2007;178:463–473. [DOI] [PubMed] [Google Scholar]
- 34.Steurer M, Schläpfer M, Steurer M, Z'graggen BR, Booy C, Reyes L, Spahn DR, Beck-Schimmer B. The volatile anaesthetic sevoflurane attenuates lipopolysaccharide-induced injury in alveolar macrophages. Clin Exp Immunol 2009;155:224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen H, Cowan MJ, Hasday JD, Vogel SN, Medvedev AE. Tobacco smoking inhibits expression of proinflammatory cytokines and activation of IL-1R-associated kinase, p38, and NF-κB in alveolar macrophages stimulated with TLR2 and TLR4 agonists. J Immunol 2007;179:6097–6106. [DOI] [PubMed] [Google Scholar]
- 36.Li Q, Park PW, Wilson CL, Parks WC. Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 2002;111:635–646. [DOI] [PubMed] [Google Scholar]
- 37.Haslett C. Granulocyte apoptosis and its role in the resolution and control of lung inflammation. Am J Respir Crit Care Med 1999;160:S5–S11. [DOI] [PubMed] [Google Scholar]
- 38.Kaneider C, Reinisch CM, Dunzendorfer S, Meierhofer C, Djanani A, Wiedermann CJ. Induction of apoptosis and inhibition of migration of inflammatory and vascular wall cells by cerivastatin. Atherosclerosis 2001;158:23–33. [DOI] [PubMed] [Google Scholar]
- 39.Chello M, Anselmi A, Spadaccio C, Patti G, Goffredo C, Di Sciascio G, Covino E. Simvastatin increases neutrophil apoptosis and reduces inflammatory reaction after coronary surgery. Ann Thorac Surg 2007;83:1374–1380. [DOI] [PubMed] [Google Scholar]
- 40.Khreiss T, Jozsef L, Hossain S, Chan JSD, Potempa LA, Filep JG. Loss of pentameric symmetry of C-reactive protein is associated with delayed apoptosis of human neutrophils. J Biol Chem 2002;277:40775–40781. [DOI] [PubMed] [Google Scholar]
- 41.McKeon DJ, Condliffe AM, Cowburn AS, Cadwallader KC, Farahi N, Bilton D, Chilvers ER. Prolonged survival of neutrophils from patients with Delta F508 CFTR mutations. Thorax 2008;63:660–661. [DOI] [PubMed] [Google Scholar]
- 42.Morimoto K, Janssen WJ, Fessler MB, McPhillips KA, Borges VM, Bowler RP, Xiao YQ, Kench JA, Henson PM, Vandivier RW. Lovastatin enhances clearance of apoptotic cells (efferocytosis) with implications for chronic obstructive pulmonary disease. J Immunol 2006;176:7657–7665. [DOI] [PubMed] [Google Scholar]
- 43.Pirat A, Zeyneloglu P, Aldemir D, Yucel M, Ozen O, Candan S, Arslan G. Pretreatment with simvastatin reduces lung injury related to intestinal ischemia-reperfusion in rats. Anesth Analg 2006;102:225–232. [DOI] [PubMed] [Google Scholar]
- 44.Yao HW, Mao LG, Zhu JP. Protective effects of pravastatin in murine lipopolysaccharide-induced acute lung injury. Clin Exp Pharmacol Physiol 2006;33:793–797. [DOI] [PubMed] [Google Scholar]
- 45.Lo CJ, Fu M, Lo FR, Cryer HG. Macrophage TNF mRNA expression induced by LPS is regulated by sphingomyelin metabolites. Shock 1999;11:411–415. [PubMed] [Google Scholar]
- 46.Foda HD, Rollo EE, Drews M, Conner C, Appelt K, Shalinsky DR, Zucker S. Ventilator-induced lung Injury upregulates and activates gelatinases and EMMPRIN. Attenuation by the synthetic matrix metalloproteinase inhibitor, prinomastat (ag3340). Am J Respir Cell Mol Biol 2001;25:717–724. [DOI] [PubMed] [Google Scholar]
- 47.Furman C, Copin C, Kandoussi M, Davidson R, Moreau M, McTaggiart F, Chapman MJ, Fruchart JC, Rouis M. Rosuvastatin reduces MMP-7 secretion by human monocyte-derived macrophages: potential relevance to atherosclerotic plaque stability. Atherosclerosis 2004;174:93–98. [DOI] [PubMed] [Google Scholar]
- 48.Aikawa M, Rabkin E, Sugiyama S, Voglic SJ, Fukumoto Y, Furukawa Y, Shiomi M, Schoen FJ, Libby P. An HMG-CoA reductase inhibitor, cerivastatin, suppresses growth of macrophages expressing matrix metalloproteinases and tissue factor in vivo and in vitro. Circulation 2001;103:276–283. [DOI] [PubMed] [Google Scholar]
- 49.Guha M, Mackman N. LPS induction of gene expression in human monocytes. Cell Signal 2001;13:85–94. [DOI] [PubMed] [Google Scholar]
- 50.Dichtl W, Dulak J, Frick M, Alber HF, Schwarzacher SP, Ares MP, Nilsson J, Pachinger O, Weidinger F. HMG-CoA reductase inhibitors regulate inflammatory transcription factors in human endothelial and vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 2003;23:58–63. [DOI] [PubMed] [Google Scholar]
- 51.O'Grady NP, Preas HL, Pugin J, Fiuza C, Tropea M, Reda D, Banks SM, Suffredini AF. Local inflammatory responses following bronchial endotoxin instillation in humans. Am J Respir Crit Care Med 2001;163:1591–1598. [DOI] [PubMed] [Google Scholar]
- 52.Craig T, O'Kane CM, McAuley DF. Potential mechanisms by which statins modulate pathogenic mechanisms important in the development of acute lung injury. In J. L. Vincent, editor. 27th yearbook of intensive care and emergency medicine. Berlin: Springer-Verlag; 2007. p.276.
- 53.Li JJ, Wang Y, Nie SP, Zhang CY, Li YS, Hui RT, Zhen X. Reduction of C-reactive protein by a single 80 mg of simvastatin in patients with unstable angina. Clin Chim Acta 2007;376:163–167. [DOI] [PubMed] [Google Scholar]
- 54.Li JJ, Fang CH, Qian HY, Hu WL. Time course of rapid C-reactive protein reduction by pravastatin in patients with stable angina. Angiology 2006;57:1–7. [DOI] [PubMed] [Google Scholar]
- 55.Kruger PS, Freir NM, Venkatesh B, Robertson TA, Roberts MS, Jones M. A preliminary study of atorvastatin plasma concentrations in critically ill patients with sepsis. Intensive Care Med 2008;35:717–721. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.