Abstract
A sore throat, which is most commonly viewed as a minor ailment, can be a manifestation of a life-threatening disorder known as Lemierre’s syndrome caused by Fusobacterium necrophorum. We report a new case of Lemierre’s syndrome that occurred in an otherwise healthy 18-year-old woman, who initially presented with fever and sore throat. The diagnosis was not made until a week later when blood cultures became available. This syndrome should be suspected until proven otherwise in any patient with signs of pharyngitis, a painful swollen neck, and pulmonary symptoms. By presenting this curable, but potentially life-threatening case of Lemierre’s syndrome, we hope to increase the awareness of the early clinical manifestations of Lemierre’s syndrome and to emphasize the importance of careful physical examination with special attention to the neck. Clinicians should be aware that exclusion of streptococcal infection in a patient with severe tonsillar infection does not exclude a bacterial cause.
KEY WORDS: pharyngitis, sore throat, Lemierre’s syndrome, Fusobacterium necrophorum
Fusobacterium necrophorum is an obligate anaerobe and is believed to be a member of the normal flora of the human oropharyngeal, gastrointestinal, and urogenital tracts. It has been well recognized as the most common cause of Lemierre’s syndrome (LS), a life-threatening septicemia illness with metastatic abscesses secondary to a septic thrombophlebitis of the internal jugular vein following an initial acute sore throat. Although sore throat is an initial presenting feature of LS, not until recently has increasing evidence suggested that F. necrophorum is a cause of recurrent sore throat and persistent sore throat syndrome. F. necrophorum is considered by some to be the second most common cause of bacterial sore throat after group A beta hemolytic streptococci.1–4
Lemierre’s syndrome, which also is known as postanginal septicemia and a form of necrobacillosis, was first reported by Lemierre in 1936.5 Classic LS is characterized by four criteria, which include primary infection in the oropharynx, septicemia documented by at least one positive blood culture, clinical or radiographic evidence of internal jugular vein thrombosis, and at least one metastatic focus.6 We present a case of LS in an 18-year-old otherwise healthy woman with pharyngitis followed by parapharyngeal abscess, internal jugular vein thrombophlebitis, and septic pulmonary emboli, whose illness was caused by a unique species of Fusobacterium, namely, F. nucleatum. A high degree of clinical suspicion is necessary for early diagnosis. Frequent early symptoms are sore throat, fever, and a painful swelling in the neck, typically along the anterior border of the sternocleidomastoid muscle. This syndrome should be suspected until proven otherwise in any patient with signs of pharyngitis, a painful swollen neck, and pulmonary symptoms. Awareness of this illness, its early clinical manifestations, and careful physical examination with special attention to the neck are essential for prompt diagnosis. Clinicians should be aware that exclusion of streptococcal infection in a patient with severe tonsillar infection does not exclude a bacterial cause.
CASE REPORT
A previously healthy 18-year-old white woman was transferred to our facility because of septic shock. She had presented to another hospital’s emergency department one week earlier complaining of sore throat, fever, nausea, vomiting, and generalized weakness where she was diagnosed with pharyngitis and treated symptomatically. Rapid strep test was performed and was negative.
During the next week, her symptoms worsened and fever persisted. She returned to the outlying hospital, where she was admitted for treatment of presumed sepsis. She was then transferred to our hospital for higher level of care.
Upon arrival, she was in acute respiratory distress, appeared toxic, and complained of right-sided pleuritic chest pain. Vital signs included: blood pressure of 102/58 mmHg, heart rate 110/min, respiratory rate 47/min, temperature 98.0, SaO2 of 90% on 5 L binasal canula. Oropharynx was normal. Neck was supple. Chest examination disclosed tachypnea, labored breathing, and bilateral rales with decreased breath sounds and dullness to percussion in the bases. Initial laboratory testing revealed a white blood cell count of 7,400/mm3, Hgb 9.5 g/dl, Hct 26.5%, platelets 42,000/mm3. ABG showed pH of 7.43, pCO2 28, pO2 63, on 40% FIO2. Chest x-ray showed bilateral infiltrates and pleural effusions. IV fluids and broad-spectrum antibiotics were initiated.
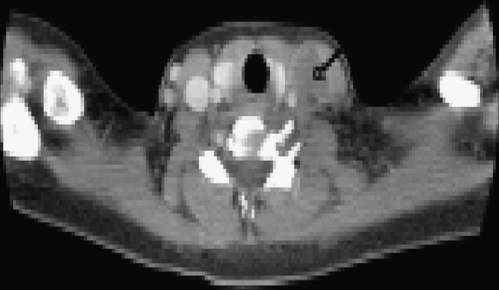
Computed tomography (CT) of the chest revealed a large cavity with air-fluid level in right lower lobe, which is consistent with lung abscess (Fig. 1). Thoracentesis was performed and 600 ml of purulent fluid was drained and sent for culture. A pigtail chest tube was placed for continued drainage. An echocardiogram showed no valvular abnormalities. Repeat physical examination revealed a tender, fluctuant mass on her left neck. CT scan of the neck showed a 3-cm abscess medial to the sternocleidomastoid and suggested jugular vein occlusion (Fig. 2). Doppler ultrasound of the neck confirmed a thrombosis in left internal jugular vein. Blood cultures from the other facility grew F. nucleatum. A diagnosis of LS was established.
Figure 1.
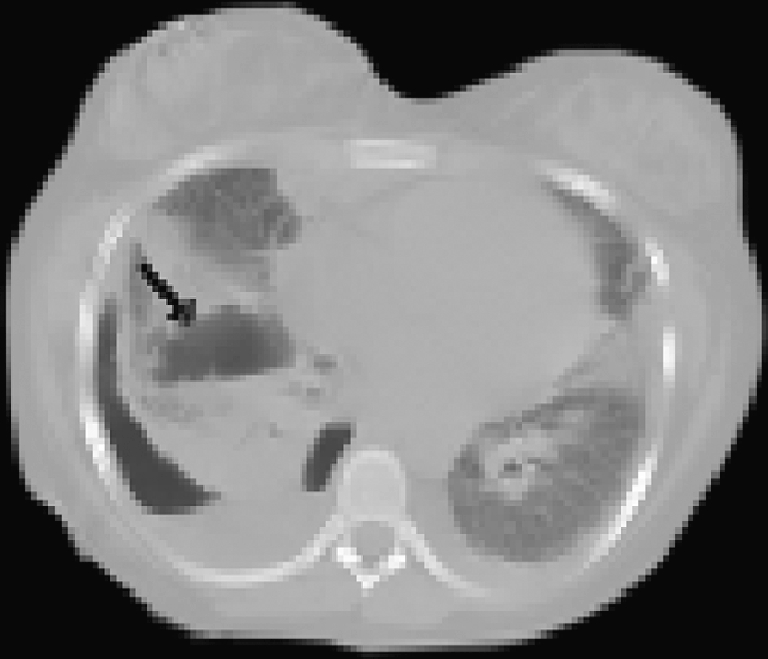
CT scan of chest. A large cavity with air-fluid level is noted in the right lower lobe consistent with lung abscess.
Figure 2.
CT scan of neck. A 3-cm abscess medial to the sternocleidomastoid on the left neck is noted. Findings also suggest a jugular vein occlusion.
The patient was switched to penicillin G intravenously and began to improve. Pigtail chest tube was discontinued due to minimal drainage. However, 1 week after admission, the patient developed left-sided pleuritic chest pain and fever. Repeat chest CT scan revealed a large, loculated, pleural fluid collection containing air in the right hemithorax, large bilateral pleural effusions, and bilateral cavitary pulmonary nodules. Bilateral chest tubes were again placed. The left-sided effusion soon resolved, but the drainage of the right effusion was unsuccessful. Cardiothoracic surgery was consulted and decortication was performed. After surgery, the patient continued to improve while taking penicillin therapy. She was discharged home after 3 weeks’ hospitalization and taking oral amoxicillin. She continued amoxicillin for another 3 weeks.
DISCUSSION
Lemierre’s syndrome was first reported in 1936 as a severe oropharyngeal infection followed by septic thrombophlebitis of the internal jugular vein and disseminated metastatic infection.5 Lemierre’s syndrome had substantial incidence during first half of the 20th century. After the introduction of antibiotics, only a small number of cases were reported during the next 30 years, and it came to be characterized as a “forgotten” disease.7,8 Moore et al. examined the English literature published from 1988–2002 and found that only 40 cases, in addition to their own case, have met the criteria set by Sinave for classic LS.6,9 However, its incidence appears to be increasing. Hagelskjaer et al. reported an overall incidence of 0.8 cases per million per year during 1990–1995 and 3.6 cases per million per year during 1998–2001 with an incidence of 14.4 cases per million per year in youngsters aged 15–24 years in Denmark.10 This increase has been attributed to increasing awareness of the disease, improved anaerobic diagnostic facilities, restriction of antibiotic use for simple sore throat, and antibiotic resistance.1,11
During the preantibiotic era, LS was associated with approximately a 90% mortality rate.5 Hagelskjaer et al. reported an overall mortality rate of 9% during 1998–2001.11 Although potentially fatal if the diagnosis is missed, the condition is highly curable when appropriate antibiotic therapy is administered promptly, making early diagnosis paramount.12–14
Although blood cultures are the “gold standard” for the diagnosis, a clinician’s awareness of the early clinical manifestations of LS and need for early imaging are essential for prompt diagnosis. Frequent early symptoms are sore throat, fever, and painful swelling in the neck, typically along the anterior border of the sternocleidomastoid muscle. This syndrome should be suspected until proven otherwise in any patient with signs of pharyngitis, a painful swollen neck, and pulmonary symptoms.15 Contrast-enhanced CT of the neck is the modality of choice to establish the diagnosis of thrombophlebitis of the internal jugular vein.16 The diagnosis often is missed until an anaerobic gram-negative rod is isolated from blood culture or another sterile site. In our case, we missed the critical sign of the subtle swollen neck during the initial physical examination, resulting in the delay of the imaging of the neck and the correct diagnosis. Most patients have evidence of metastatic complications by the time of diagnosis, as seen in our case.
The putative sequence of events after throat infection with Fusobacterium species was well illustrated in Riordan’s review article: exposure of F. necrophorum causes tonsillitis, which leads to peritonsillar abscess and thrombophlebitis of tonsillar vein. The infection then spreads through lateral pharyngeal space to internal jugular vein causing septic thrombophlebitis, followed by the development of Fusobacterium bacteremia, and finally the occurrence of classic LS/postanginal septicemia with metastatic foci in lung or other sites.11 Pulmonary septic emboli are the most common metastatic infection. These emboli often develop into empyema and pulmonary abscesses, which was seen in our patient.
The time interval between the occurrence of the primary infection and that of suppurative thrombophlebitis of the internal jugular vein with sequelae is usually 4 to 8 days, but can be as long as 2 weeks.17
Fusobacterium organisms are anaerobic, nonmotile, gram-negative bacilli. Fusobacterium has several pathogenic strains, the most notable of which are F. necrophorum and F. nucleatum. F. necrophorum is the species that is responsible for 90% of LS cases and appears to be responsible for 10% of all acute sore throats1 and 21% of all recurring sore throats,2 with the remainder caused by group A streptococci or viruses. F. nucleatum is known for causing typical dental plaque on human teeth as well as involvement in periodontal diseases. It has been reported to cause atypical forms of LS.18,19 To the best of our knowledge, only one case of classic LS caused by F. nucleatum has been reported in English language medical literature since 1988.20
F. necrophorum has been regarded by many people, including Lemierre himself, as a secondary invader, rather than the initiator of throat infection. However, increasing evidence is strongly suggestive that F. necrophorum subspecies funduliforme has a causative role in nonstreptococcal tonsillitis, particularly recurrent infection. Clinicians should be aware that exclusion of streptococcal infection in a patient with severe tonsillar infection does not exclude a bacterial cause.
F. necrophorum is usually sensitive to penicillin G. However, penicillin-resistant organisms have been reported. Therefore, beta lactamase-resistant antibiotics, which provide excellent anaerobic coverage, are becoming more popular. Penicillin, metronidazole, and clindamycin are the most frequently used drug therapy. Most authors would not advocate clindamycin or penicillin alone. Metronidazole in combination with penicillin was recommended by most authors to provide reliable anaerobic coverage and coverage for mixed infection involving organisms, such as oral streptococci.9,11 There is no consistency concerning duration of therapy. A total of 6 weeks of antibiotic therapy seems to be the consensus, including 7–14 days of IV antibiotics, followed by an additional 2–4 weeks of oral antibiotics depending on the severity of the infection.6 In our case, single-agent penicillin G was administered, which may have contributed to the prolonged recovery.
Other therapies include anticoagulation and ligation of the thrombosed vessels. Ligation or excision of the thrombosed internal jugular vein was the only available therapeutic option in Lemierre’s day, although this is rarely needed today. It should be considered in the case of uncontrolled sepsis and ongoing evidence of septic emboli despite appropriate medical therapy.18 Anticoagulation is controversial. It is generally not recommended, except in the case of retrograde extension of the thrombus to the cavernous sinus.21 Anticoagulation was not used in our patient.
CONCLUSIONS
Due to the increased incidence of LS in the recent past and the significance of the high morbidity and potential for mortality with delayed treatment, it is essential that physicians be aware of the clinical manifestations of LS. A high index of suspicion is needed to make the diagnosis. A thorough physical examination with emphasis on the neck, early imaging of the neck, and blood culture must be obtained and early proper antibiotic coverage must be initiated to adequately treat and prevent serious complications in these patients. Clinician should be aware that exclusion of streptococcal infection in a patient with severe tonsillar infection does not exclude a bacterial cause. Early treatment could prevent more serious systemic infection, such as LS.
Acknowledgments
The manuscript has not been simultaneously submitted elsewhere. The abstract was presented as a poster presentation at the National Society of General Internal Medicine conference, April 2008, Pittsburgh, PA. This manuscript was prepared solely by the authors listed and the authors listed on the manuscript have contributed sufficiently to the article to be included as authors.
The authors thank Dr. Huan-You Wang for a critical review of this manuscript.
Disclosure of financial support This work was not funded by any internal or external source.
Conflict of Interest None disclosed.
Statement of proprietary interest The authors hereby state that there are no commercial or proprietary interests of any type of drug, device, or equipment mentioned in this study. None of the authors has any financial interest of this study.
References
- 1.Aliyu SH, Marriott RK, Curran MD, et al. Real-time PCR investigation into the importance of Fusobacterium necrophorum as a cause of acute pharyngitis in general practice. J Med Microbiol. 2004;53:1029–1035. doi: 10.1099/jmm.0.45648-0. [DOI] [PubMed] [Google Scholar]
- 2.Batty A, Wren MWD. Prevalence of Fusobacterium necrophorum and other upper respiratory tract pathogens isolated from throat swabs. Br J Biomed Sci. 2005;62:66–70. doi: 10.1080/09674845.2005.11732687. [DOI] [PubMed] [Google Scholar]
- 3.Jensen A, Hagelskjaer Kristensen L, Prag J. Detection of Fusobacterium necrophorum subsp. funduliforme in tonsillitis in young adults by real-time PCR. Clin Microbiol Infect. 2007;13:695–701. doi: 10.1111/j.1469-0691.2007.01719.x. [DOI] [PubMed] [Google Scholar]
- 4.Amess JA, O’Neill W, Giollariabhaigh CN, Dytrych JK. A six-month audit of the isolation of Fusobacterium necrophorum from patients with sore throat in a district general hospital. Br J Biomed Sci. 2007;64:63–65. doi: 10.1080/09674845.2007.11732757. [DOI] [PubMed] [Google Scholar]
- 5.Lemierre A. On certain septicemias due to anaerobic organisms. Lancet. 1936;1:701–703. doi: 10.1016/S0140-6736(00)57035-4. [DOI] [Google Scholar]
- 6.Sinave CP, Hardy GJ, Fardy PW. The Lemierre’s syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Med (Baltimore) 1989;68:85–94. [PubMed] [Google Scholar]
- 7.Shah SA, Ghani R. Lemierre’s syndrome: a forgotten complication of oropharyngeal infection. J Ayub Med Coll Abbottabad. 2005;17:30–33. [PubMed] [Google Scholar]
- 8.Koay CB, Heyworth T, Burden P. Lemierre syndrome: a forgotten complication of acute tonsillitis. J Laryngol Otol. 1995;109:657–661. doi: 10.1017/s0022215100130956. [DOI] [PubMed] [Google Scholar]
- 9.Moore BA, Dekle C, Werkhaven J. Bilateral Lemierre’s syndrome: a case report and literature review. Ear Nose Throat J. 2002;81:234–252. [PubMed] [Google Scholar]
- 10.Hagelskjær Kristensen L, Prag J. Lemierre’s syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis. 2008;27:779–789. doi: 10.1007/s10096-008-0496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riordan T. Human infection with Fusobacterium necrophorum (necrobacillosis), with a focus on Lemierre’s syndrome. Clin Microbiol Rev. 2007;20:622–659. doi: 10.1128/CMR.00011-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chirinos JA, Lichtstein DM, Garcia J, Tamariz LJ. The evolution of Lemierre’s syndrome: report of 2 cases and review of the literature. Med (Baltimore) 2002;81:458–465. doi: 10.1097/00005792-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Brown LM, Wallwork B. Lemierre’s- the sinister sore throat. J Laryngo Otol. 2007;121:692–694. doi: 10.1017/S0022215106003951. [DOI] [PubMed] [Google Scholar]
- 14.Sherer Y, Mishal J, Leibovici O. Early antibiotic treatment may prevent complete development of Lemierre’s syndrome: experience from 2 cases. Scand J Infect Dis. 2000;32:706–707. doi: 10.1080/003655400459711. [DOI] [PubMed] [Google Scholar]
- 15.Fleskens AJ, Scheltinga MR, Eerten PV, Verhoef LH, Pasmans HL, Vreugdenhil G. Sore throat and a swollen neck: Lemierre’s syndrome until proven otherwise. Ned Tijdschr Geneeskd. 2006;150:2461–2466. [PubMed] [Google Scholar]
- 16.Nguyen-Dihg KV, Masot-Dupuch K, Portier F, Lamblin B, Lasjaunias P. Lemierre syndrome: usefulness of CT in detection of extensive occult thrombophlebitis. J Neuroradiol. 2002;29:132–135. [PubMed] [Google Scholar]
- 17.Dool H, Soetekouw R, Zanten MV, Grooters E. Lemierre’s syndrome: three cases and a review. Eur Arch Otorhinolaryngol. 2005;262:651–654. doi: 10.1007/s00405-004-0880-3. [DOI] [PubMed] [Google Scholar]
- 18.Roux K, Seve P, Gomard E, et al. Lemierre’s syndrome variant: hepatic abscesses and hepatic venous thrombosis due to Fusobacterium nucleatum septicemia [in French] Rev Med Intern. 2006;27:482–486. doi: 10.1016/j.revmed.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Williams MD, Kerber CA, Tergin HF. Unusual presentation of Lemierre’s syndrome due to Fusobacerium nucleatum. J Clin Microbiol. 2003;41:3445–3448. doi: 10.1128/JCM.41.7.3445-3448.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sena S, Rosenfeld DL, Santos S, Keller I. Jugular thrombophlebitis complicating bacterial pharyngitis (Lemierre’s syndrome) Pediatr Radiol. 1996;26:141–144. doi: 10.1007/BF01372094. [DOI] [PubMed] [Google Scholar]
- 21.Riordn T, Wilson M. Lemierre’s syndrome: more than a historical curiosa. Postgrad Med J. 2004;80:328–334. doi: 10.1136/pgmj.2003.014274. [DOI] [PMC free article] [PubMed] [Google Scholar]