Abstract
Pathogens must be able to overcome both host defenses and antimicrobial treatment in order to successfully infect and maintain colonization of the host. One way fungi accomplish this feat and overcome intercellular toxin accumulation is efflux pumps, in particular ATP-binding cassette transporters and transporters of the major facilitator superfamily. Members of these two superfamilies remove many toxic compounds by coupling transport with ATP hydrolysis or a proton gradient, respectively. Fungal genomes encode a plethora of members of these families of transporters compared to other organisms. In this review we discuss the role these two fungal superfamilies of transporters play in virulence and resistance to antifungal agents. These efflux transporters are responsible not only for export of compounds involved in pathogenesis such as secondary metabolites, but also export of host-derived antimicrobial compounds. In addition, we examine the current knowledge of these transporters in resistance of pathogens to clinically relevant antifungal agents.
Introduction
Members of the fungal kingdom are found in almost all habitats and exist as saprobes, commensals, and pathogens. Approximately 11,000 plant diseases have been attributed to fungi in over 120 genera [1], while in the clinical setting, the number of invasive fungal infections has increased steadily over the past two decades. Candida sp. is the fourth most common pathogen isolated from blood cultures [2], and other pathogens such as Cryptococcus sp., Aspergillus sp., Fusarium sp., and zygomycetes, have an unacceptably high morbidity and mortality [3]–[5]. In addition, the incidence of mycoses caused by opportunistic fungi is rising [6].
The diverse nature of fungi can be attributed to such factors as increased capacity to utilize a wide range of carbon and nitrogen sources, the capability for rapid growth, and the ability to adapt to otherwise harsh environments. Fungi are constantly bombarded by toxic compounds from external sources. These compounds can be synthesized by other microorganisms to impede the fungus for a competitive advantage to limited resources, synthesized by hosts as a defense mechanism, or may be present in the environment. Regardless of the source, these toxic compounds force the fungus to evolve mechanisms in order to survive. One common method to overcome these antifungal compounds is active efflux, which prevents any intracellular build-up of the compound and, therefore, renders the fungus resistant or tolerant to the otherwise toxic compound.
As research in mycology progresses it is becoming evident that transporters are important factors in pathogenicity. Several transporters have been described as being involved in fungal pathogenicity, including a range of cellular processes such as calcium entry, vescicle transport, stress tolerance, dimorphic switching, capsule synthesis, iron acquition, and virulence factor enzyme activity [7]–[16]. This review will focus on the ATP-binding cassette (ABC) transporters and the major facilitator superfamily (MFS) transporters associated with secondary metabolites, such as mycotoxins, and resistance to natural toxic compounds or antifungal drugs, which have a proven or implicated role in fungal pathogenesis (Table 1).
Table 1. Summary of Transporters Involved in Virulence or Toxin and Drug Efflux.
| Transporter Family | Name | Fungus | Description/Substrate | Amino Acid Length | References |
| ABC Transporters | |||||
| PDR/ABCG | CDR1 | C. albicans | Triazole resistance | 1500 | [60],[72] |
| PDR/ABCG | CDR2 | C. albicans | Triazole resistance | 1499 | [71]–[73] |
| PDR/ABCG | CgCDR1 | C. glabrata | Fluconazole, itraconazole | 1542 | [59] |
| PDR/ABCG | CgCDR2/PDH1 | C. glabrata | Fluconazole, ketoconazole | 1499 | [61],[85] |
| PDR/ABCG | CgSNQ2 | C. glabrata | Fluconazole, itraconazole | 1507 | [62] |
| PDR/ABCG | AFR1 | C. neoformans | Triazole resistance | 1543 | [58] |
| PDR/ABCG | ABC1 | M. grisea | Unknown function | 1619 | [46] |
| PDR/ABCG | GpABC1 | G. pulicaris | Rishitin tolerance | 1491 | [51] |
| PDR/ABCG | Mgatr4 | M. graminicola | Unknown function | 1635 | [49] |
| PDR/ABCG | BcatrB | B. cinerea | Resveratrol tolerance | 1439 | [48],[50] |
| MRP/ABCC | MLT1 | C. albicans | Unknown function, possibly bile | 1606 | [55] |
| MFS Transporters | |||||
| DHA14 | TOXA | C. carbonum | HC-toxin secretion | 548 | [34] |
| DHA14 | TRI12 | F. sporotrichioides | Trichothecene T-2 secretion | 598 | [40] |
| DHA14 | CFP | C. kikuchii | Cercosporin secretion | 607 | [35] |
| DHA12 | CTB4 | C. nicotianae | Cercosporin secretion | 512 | [36] |
| DHA12 | cefT | A. chrysogenum | Cephalosporin secretion | 561 | [42] |
| DHA14 | PEP5 | N. haematococca | Unknown function | 592 | [52] |
| DHA12 | MDR1 | C. albicans | Fluconazole resistance | 564 | [76]–[78] |
| DHA12 | FLU1 | C. albicans | Fluconazole resistance | 610 | [79] |
| DHA12 | CdMDR1 | C. dubliniensis | Fluconazole resistance | 557 | [80],[81] |
| DHA12 | TMP1 | C. albicans | MDR | 561 | [83] |
| DHA12 | TMP2 | C. albicans | MDR | 581 | [83] |
Transporters involved in virulence are in bold.
Overview of Efflux Pumps
The two most extensively studied families of transporters involved in efflux are the ABC transporters and the MFS transporters. Fungi dedicate a large amount of their genome to encoding transporters, as there are approximately ten to 30 genes encoding transporters per megabase of genomic DNA in fungal genomes [17]. The most common type of transporter in all sequenced fungal genomes to date is the MFS transporter. However, members of the ABC transporter superfamily are the most common of the primary transporters (Table 2). Together, these two superfamilies account for approximately half of all the genes encoding transporters in fungal genomes. Despite the importance of these two families of transporters in virulence, there is no apparent correlation between the quantity of these transporters in fungal genomes and the pathogenicity of the fungus (a saprobic isolate versus a pathogenic isolate). For example, Aspergillus nidulans and the closely related human pathogen Aspergillus fumigatus both have 45 ABC transporters encoded in their genomes, and A. nidulans has more MFS transporters than A. fumigatus (Table 2). Also of note, the group known as oomycetes, although not members of the fungal kingdom, but sometimes loosely grouped with fungi, have 4- to 5-fold more ABC transporters than true fungi; however, this difference could be due to the larger genome size of the oomycetes.
Table 2. Number of ABC and MFS Transporters in Sequenced Fungal and Oomycete Genomes.
| Classification | Fungus | ABCa | MFS |
| Oomycetes | Phytophthora infestans | 160 | 102 |
| Phytophthora ramorum | 185 | 113 | |
| Phytophthora sojae | 190 | 109 | |
| Chytridiomycota | Batrachochytrium dendrobatidis | 52 | 23 |
| Zygomycota | Rhizopus oryzae | 44 | 111 |
| Basidiomycota | Ustilago maydis | 38 | 91 |
| Puccinia graminis | 26 | 35 | |
| Cryptococcus neoformans JEC21 | 29 | 192 | |
| C. neoformans H99 | 32 | 159 | |
| Coprinus cinereus | 47 | 95 | |
| Phanerochaete chrysosporium | 56 | 113 | |
| Ascomycota | |||
| Taphrinomycotina | Schizosaccharomyces pombe | 9 | 58 |
| Saccharomycotina | Saccharomyces cerevisiae | 24 | 85 |
| Candida albicans SC5314 | 21 | 85 | |
| Eurotiomycetes | Aspergillus nidulans | 45 | 356 |
| Aspergillus fumigatus | 45 | 275 | |
| Penicillium chrysogenum | 51 | 416 | |
| Coccidioides posadasii C735 | 30 | 146 | |
| Paracoccidioides brasiliensis Pb18 | 28 | 103 | |
| Histoplasma capsulatum | 33 | 86 | |
| Microsporum gypseum | 45 | 178 | |
| Dothideomycetes | Stagonospora nodorum | 46 | 301 |
| Leotiomycetes | Sclerotinia sclerotiorum | 44 | 169 |
| Botrytis cinerea | 51 | 204 | |
| Sordariomycetes | Magnaporthe grisea | 50 | 251 |
| Chaetomium globosum | 41 | 155 | |
| Neurospora crassa | 31 | 141 | |
| Gibberella zeae (Fusarium grmainearium) | 56 | 335 | |
The number of transporters in each genome was calculated from either the genome publication (P. chrysosporium, P. chrysogenum), the TransporterDB (P. infestans, P. ramorum, P. sojae, C. neoformans JEC21, S. pombe, S. cerevisiae, A. nidulans, A. fumigatus, C. posadasii, N. crassa) or from searching the Broad Fungal Genome Initiative Web site (http://www.broad.mit.edu/node/304) for the PFAM domains corresponding to the transporter.
The number of ABC transporters from genomes from the Broad Fungal Genome Initiative includes the number of ABCE and ABCF proteins (usually 4–5 members), as they contain the conserved sequence; however, they are not transporters.
Members of the ABC transporter superfamily are primary efflux transporters, which, as their name implies, hydrolyize ATP for export of the substrate. This superfamily is further broken into five families of transporters (ABCA, ABCB, ABCC, ABCD, and ABCG), of which three families are involved in efflux of toxic compounds. Members of these three families, ABCB, ABCC, and ABCG, also referred to as the multi-drug resistance (MDR), multi-drug resistance–associated protein (MRP), and the pleiotropic drug resistance (PDR) families, respectively, have been extensively studied in Saccharomyces cerevisiae, providing insight into their possible functions in pathogenic fungi [18],[19]. Of the ABC transporter families, the PDR family has the least amount of phylogenetic conservation, demonstrating both gene loss and duplication within yeasts [20] and filamentous fungi, which suggests that members of this family are rapidly evolving from outside selective pressures.
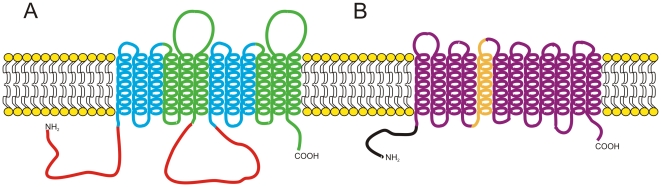
The conserved architecture of ABC transporters is composed of a nucleotide-binding domain (NBD) followed or preceded by six transmembrane-spanning helices creating a transmembrane domain (TMD). These two domains together represent the NBD-TMD6 design of half ABC transporters, which dimerize to form a fully functional protein [21]. Instead of dimerizing, most fungal ABC transporters have evolved to be comprised of two fused NBD-TMD6 half transporters, creating one functional protein (Figure 1) [21],[22].
Figure 1. Schematic representation of the two main fungal transporters responsible for efflux of toxic compounds.
Representation of an ABC transporter of the PDR family (A) and an MFS transporter of the DHA12 family (B). The NBDs of the ABC transporter are depicted in red, while the TMDs important for substrate specificity are colored green and gold for the ABC and MFS transporters, respectively.
The MFS transporters are smaller in size compared to the ABC transporters since they do not require an NBD; however, they still contain 12 or 14 transmembrane-spanning helices (Figure 1). Translocation of the substrate is driven by the proton gradient generated across the plasma membrane [23]. This family is divided into 17 families, of which two, the drug:H+ antiporter (14 spanner) (DHA14) and the drug:H+ antiporter (12-spanner) (DHA12), are involved in efflux of toxic compounds [23].
Transporters in Plant Pathogens
Virulence-associated efflux pumps in plant pathogenic fungi can be classified into two categories. The first class of transporters is responsible for secretion of virulence factors or compounds produced by the fungus. Several fungi synthesize and secrete low molecular weight compounds that are not required for growth. These compounds, termed secondary metabolites, are bioactive and are sometimes involved in virulence [24],[25]. Secondary metabolites are commonly synthesized by clusters of genes that usually include either a polyketide synthase (PKS), nonribsomal peptide synthase (NRPS), or a fusion of both enzymes (PKS-NRPS), which is responsible for the majority of the synthesis of the metabolite [24],[25]. Other accessory proteins within the gene cluster are involved in the secondary metabolite's biosynthesis, and frequently one (or more) gene(s) encoding a transporter is associated with these secondary metabolite gene clusters. Examples of secondary metabolites are the iron sequestering compounds, termed siderophores [26],[27], which are virulence factors for a number of pathogens [28]–[30]; mycotoxins such as penicillin G, gliotoxin, aflatoxin, and lovastatin; and the host-specific and -nonspecific toxins such as T-toxin, victorin, botrydial, AF-toxin, and cercosporin [31].
Phytotoxins produced by fungi that are involved in virulence on a specific host plant, and therefore expand host range, are termed host-specific toxins (HSTs), and while not all plant pathogens produce HSTs, they are important virulence factors for members of the Cochliobolus and Alternaria species [31],[32]. For example, the phytopathogenic fungus Cochliobolus carbonum produces a cyclic tetrapeptide HST, termed HC-toxin, which functions as an inhibitor of histone deacetylases in several organisms and is a virulence factor on maize [33]. The synthesis of this compound is carried out by an NRPS named HTS1 [33], and the locus responsible for the synthesis of this compound contains two genes encoding MFS transporters, termed TOXA and TOXB, postulated to be responsible for efflux of HC-toxin into the host plant cell [34]. In another example, the plant pathogenic Cercospora species produces a host-nonselective toxin, cercosporin, which is also synthesized by a secondary metabolite gene cluster. Cercosporin is exported out of the fungal cell by the cercosporin facilitator protein (CFP) in C. kikuchii and by CTB4 in C. nicotinae [35],[36]. These 12-membrane-spanning MFS transporters appear to be orthologous, and mutants of these genes are reduced in virulence on their host plants. However, the rice pathogen Magnaporthe grisea produces a secondary metabolite via the PKS-NRPS fusion protein termed ACE1 and the surrounding accessory proteins. This cluster contains a gene encoding an MFS transporter (MFS1), although it is not involved in efflux of the ACE1 metabolite as it has a deletion of a single base pair resulting in an early stop codon [37]. Therefore, the ACE1 metabolite must rely on another transporter encoded outside the secondary metabolite gene cluster for export.
Efflux pumps in secondary metabolite gene clusters that are responsible for synthesis of mycotoxins are less well understood. The expression of MFS transporters in mycotoxin secondary metabolite clusters appears not to be controlled by the same transcription factors as the rest of the secondary metabolite cluster but, instead, is induced by the accumulation of the synthesized metabolite [38],[39]. However, the ABC transporter TRI12 in the trichothecene T-2 toxin cluster contains the conserved sequence in the promoter region for binding of the cluster's transcription factor, suggesting it is under the same control as the rest of the gene cluster [40]. Mutants of efflux pumps in secondary metabolite clusters have been constructed, and most of these mutants retain wild-type levels of mycotoxin secretion [38],[39],[41]. However, studies where the efflux pump was expressed in a homologous system or increased in copy number resulted in either efflux of the compound or a corresponding increase in efflux [40],[42], demonstrating that the transporters are actually involved in efflux of the mycotoxin. The most obvious reason why mutants of transporters in secondary metabolite clusters lack a reduction of toxin secretion is due to other transporters with an overlapping substrate range. Supporting this notion, mutants of the ABC transporter atrD in Aspergillus nidulans, although not in a cluster, produce less penicillin than the wild-type, suggesting this transporter is involved in efflux of the compound [43].
The second class of transporters involved in plant virulence is responsible for efflux of molecules produced by the host plant. As a defense mechanism, plants produce antimicrobial compounds. These low molecular weight compounds, termed phytoalexins or phytoanticipins depending on when they are synthesized, have diverse chemical structures. Over 25 years ago, studies conducted on Nectria haematococca MPVI and the pea phytoalexin pisatin suggested that a fungal efflux mechanism is involved in the tolerance to this plant-derived defense compound and, therefore, may be a pathogenicity factor [44],[45]. However, it was not until 15 years later that the first fungal ABC transporter (ABC1) was demonstrated to be a virulence factor in the phytopathogenic fungus M. grisea, the causative agent of rice blast disease [46].
Since that time a number of ABC transporters have been identified as virulence factors on host plants. Most of these transporters are members of the PDR family of ABC transporters (Table 1). A number of phytoalexins and other toxic compounds induce expression of these fungal transporters [46]–[50]; however, only a few have demonstrated the ability to confer tolerance to a known phytoalexin. The ABC transporters BcatrB in Botrytis cinerea and GpABC1 in Gibberella pulicaris provide tolerance to the host plant's phytoalexins, resveratrol and rishitin, respectively [48],[51]. A BcatrB mutant is reduced in pathogenicity on grape leaves [48], while a GpABC1 mutant is essentially nonpathogenic on potato [51]. Few examples of fungal MFS transporters involved in tolerance to phytoalexins exist, although a MFS transporter from N. haematococca is able to confer an increase in pathogenicity on pea when placed in a nonpathogenic pea isolate [52]. This MFS transporter–encoding gene, termed PEP5 for pea pathogenicity, is induced upon exposure to the pea phytoalexin pisatin [53]; however, the mechanism by which PEP5 contributes to virulence remains unknown.
Fungicide resistance is also due to ABC and MFS transporters. Several transporters in the agriculturally relevant fungi B. cinerea and Mycospharella graminicola, as well as the model filamentous fungus A. nidulans, have been reviewed recently [54]. The ABC transporter BcatrB of B. cinerea is also able to provide resistance to the fungicides fenpiclonil and fludioxonil in addition to resveratrol, as referenced above [48],[50].
Transporters Involved in Mammalian Virulence
The most common human pathogenic fungus, C. albicans, has a total of 21 ABC transporters and 85 MFS transporters encoded within its genome (Table 2). A single ABC transporter that is required for full virulence has been identified in C. albicans. This transporter, MLT1, is a vacuolar transporter and a member of the ABCC/MRP family of proteins. Mutants of this transporter are severely defective in invasion of the liver and pancreas in a mouse peritonitis virulence assay and cause less hepatic tissue damage [55]. The exact substrate(s) of this efflux pump are not currently known; however, MLT1 is similar to the bile pigment transporter BPT1 in S. cerevisiae, which is involved in sequestering unconjugated bilirubin and glutathione conjugates in the vacuole [56],[57], suggesting that MLT1 is involved in resistance to similar compounds.
ABC Transporters in Clinical Multi-Drug Resistance
Although not directly involved in virulence, the ability to provide resistance to antifungal compounds does provide a “colonization” advantage to the fungus and, therefore, merits further discussion.
A number of transporters that confer resistance to members of the antifungal class of triazoles have been described. These include the ABC transporters CDR1 and CDR2 in C. albicans; AFR1 in C. neoformans; ABC1 in C. krusei; and CgCDR1, PDH1 (also referred to as CgCDR2), and SNQ2 in C. glabrata [58]–[63]. These transporters are usually able to provide cross-resistance to the antifungal class of triazoles (fluconazole, itraconazole, ketoconazole, voriconazole); however, studies suggest they are not responsible for echinocandin resistance or resistance to the antifungal protein histatin 5 [64],[65]. These transporters are closely related and all belong to the PDR family, which includes the well-characterized PDR5 transporter in S. cerevisiae. The PDR family is one of the largest families of ABC transporters in fungi and is overrepresented when their numbers are compared to other organisms, i.e., there are five and nine ABCG/PDR transporters in humans and Caenorhabditis elegans, respectively [66],[67]. Although initially identified for conferring an MDR phenotype, studies of CDR1 and CDR2, and most likely the orthologous genes in other pathogenic fungi, have demonstrated that their physiological function is the transport of phospholipids and steroids across the membrane [68]–[70].
Of the transporters involved in fluconazole resistance in medically important fungi, CDR1 and CDR2 are the most studied. Despite their high degree of amino acid similarity, there are functional differences between the two. Mutants of CDR2 retain a wild-type level of resistance to fluconazole; however, in a double mutant (ΔCDR1/ΔCDR2) the strain is more susceptible to fluconazole than either single mutant [71]. Other differences in function have been identified, suggesting that the two ABC transporters have separate, but overlapping, roles in the fungus [72]. In addition, there is allelic variation of the genes. Comparison of the CDR2 alleles uncovered two point mutations in equal frequency of an allele in transmembrane helix 12 that were involved in substrate binding and function [73]. Most strains were heterozygous for these CDR2 genes, and further phylogenetic analysis suggested that as many as 33 codon changes between the two alleles may be selectively advantageous [73]. Differences in transmembrane domains are significant, as evidence builds that they are responsible for substrate specificity. Most ABC transporters have been demonstrated to have multiple substrates; thus, it is postulated that substrate binding does not occur in a specific active site, but rather in an active pocket able to accommodate a variety of structurally different compounds [74],[75]. Several amino acids are conserved among these transmembrane helices of fluconazole PDR transporters, where the most conserved helices are 6 and 12.
MFS Transporters in Clinical Multi-Drug Resistance
In addition to ABC transporters, a number of MFS transporters also are responsible for increased resistance to fluconazole. The two best characterized are MDR1 (formally BENr) and FLU1 in C. albicans [76]–[79], and homologs of MDR1 have been implicated in fluconazole resistance in C. dubliniensis [80],[81] and C. tropicalis [82]. Unlike the ABC transporters, the resistance conferred by MFS transporters is more specific for fluconazole than other triazoles, although other substrates have been identified [76],[80]. Of particular importance for MDR1 function is transmembrane domain 5, which harbors a conserved motif important for drug:H+ translocation (Figure 1) [78]. Other MFS transporters (TMP1 and TMP2) confer increased resistance to a number of unrelated antifungal drugs in C. albicans [83]. It should be noted that other transporters may be involved in resistance to antifungals. For example, the Sec14p family member PDR16 transporter in C. albicans is upregulated in fluconazole-resistant clinical isolates, and confers a 2-fold increased resistance to the azole antifungal [84].
Expression of Efflux Pumps in the Multi-Drug Resistance Phenomenon
Pathogenic isolates are able to develop resistance to prescribed antifungal treatment rapidly [85],[86]. While other factors contribute to this increase in resistance, one reason is the increase in transcription of drug transporters [85], [87]–[91]. A shared 22–base pair sequence in the promoters of CaCDR1 and CaCDR2, termed the drug responsive element, serves as the binding site of the Zn(2)-Cys(6) finger transcription factor TAC1 [92],[93]. Although azole-resistant isolates have been demonstrated to sometimes carry an extra copy of the chromosome that has CDR1 and CDR2, the transcript levels did not increase [94], confirming other studies that suggest the increase in transcription is due to either the promoter or trans-acting factors of the CDR genes [95]. Indeed, a second chromosomal rearrangement was identified where resistant isolates frequently harbor duplications of the chromosomal region in which TAC1 resides [96]. Recently, the analogous transcription factors of TAC1 in C. glabrata (CgPDR1 and CgPDR3) have been demonstrated to bind the substrate, promoting the expression of the efflux pumps under its control [97]. Another zinc finger transcription factor (MRR1) is responsible for the overexpression of the MFS transporter encoding gene MDR1 [98]. Two point mutations in MRR1 of azole-resistant isolates were identified as rendering the transcription factor constitutively active [98],[99]. Unlike MDR1, expression of FLU1 in clinically resistant isolates is not increased, and therefore FLU1 is not believed to contribute significantly to resistance to fluconazole [79].
A major difference in the mutations of the major transcription factors that confer fluconazole resistance is the heritability of the resistance phenotype. The CDR1/CDR2 overexpressing C. albicans isolates require the TAC1 fluconazole-resistant transcription factor to be homozygous, as heterogygous isolates retain wild-type levels of fluconazole susceptibility [100]; however, the nature of the point mutations of MRR1, which render the transcription factor constitutively active, functions in a semi-dominant manner, as a single copy of the fluconazole-resistant mutant MRR1 increases fluconazole resistance [98]. Other transcription factors involved in CDR1, CDR2, and MRR1 overexpression have been identified, but their role in clinical resistance is less understood. These transcription factors include CaNdt80 in CDR1 overexpression [101], and Cup1 and Mcm1 in MDR1 overexpression [102],[103]. Recent studies also describe an increase in mRNA stability of CDR1 transcripts in fluconazole-resistant C. albicans isolates that results in an increase in the number of CDR1 transporters [104].
Conclusions
The role of efflux pumps, in particular ABC and MFS transporters, in fungal virulence cannot be understated. These transporters contribute to pathogenesis by 1) transporting HSTs and mycotoxins outside of the cell, 2) removing host-derived compounds that would otherwise inhibit the fungus, and 3) providing resistance to clinical antifungals. This concept is further supported by the vast amount of substrate redundancy already evidenced with the few transporters that have been extensively studied. Considering S. cerevisiae and C. albicans have relatively few ABC and MFS transporters compared to filamentous fungi, and the scope of research already conducted on these important yeast superfamilies, it appears there is much more to be discovered in other fungi.
The redundant nature of the transporters creates difficulty in characterization of the efflux mechanisms, as single deletion mutants sometimes retain a wild-type phenotype, and it is only through multiple mutations of transporters or expression in heterologous systems that the function of the transporters becomes apparent. Although a daunting endeavor, understanding all of the contributing efflux factors of a given antimicrobial will provide a means to circumvent efflux transporters.
Footnotes
The authors have declared that no competing interests exist.
Support was provided by the National Institutes of Health R01 award AI075286 to EM. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Agrios GN. Plant pathology. San Diego: Academic Press; 1997. p. 635. [Google Scholar]
- 2.Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, et al. Nosocomial bloodstream infections in United States hospitals: a three year analysis. Clin Infect Dis. 1999;29:239–244. doi: 10.1086/520192. [DOI] [PubMed] [Google Scholar]
- 3.Singh N, Paterson DL. Aspergillus infections in transplant recipients. Clin Microbiol Rev. 2005;18:44–69. doi: 10.1128/CMR.18.1.44-69.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pukkila-Worley R, Mylonakis E. Epidemiology and management of cryptococcal meningitis: developments and challenges. Expert Opin Pharmacother. 2008;9:551–560. doi: 10.1517/14656566.9.4.551. [DOI] [PubMed] [Google Scholar]
- 5.Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695–704. doi: 10.1128/CMR.00014-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nucci M, Marr KA. Emerging fungal diseases. Clin Infect Dis. 2005;41:521–526. doi: 10.1086/432060. [DOI] [PubMed] [Google Scholar]
- 7.Liu M, Du P, Heinrich G, Cox GM, Gelli A. Cch1 mediates calcium entry in Cryptococcus neoformans and is essential in low-calcium environments. Eukaryot Cell. 2006;5:1788–1796. doi: 10.1128/EC.00158-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu X, Williamson PR. A CLC-type chloride channel gene is required for laccase activity and virulence in Cryptococcus neoformans. Mol Microbiol. 2003;50:1271–1281. doi: 10.1046/j.1365-2958.2003.03752.x. [DOI] [PubMed] [Google Scholar]
- 9.Fan W, Idnurm A, Breger J, Mylonakis E, Heitman J. Eca1, a sarcoplasmic/endoplasmic reticulum Ca2+-ATPase, is involved in stress tolerance and virulence in Cryptococcus neoformans. Infect Immun. 2007;75:3394–3405. doi: 10.1128/IAI.01977-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franke K, Nguyen M, Hartl A, Dahse H-M, Vogl G, et al. The vesicle transport protein Vac1p is required for virulence of Candida albicans. Microbiology. 2006;152:3111–3121. doi: 10.1099/mic.0.29115-0. [DOI] [PubMed] [Google Scholar]
- 11.Cottrell TR, Griffith CL, Liu H, Nenninger AA, Doering TL. The pathogenic fungus Cryptococcus neoformans expresses two functional GDP-mannose transporters with distinct expression patterns and roles in capsule synthesis. Eukaryot Cell. 2007;6:776–785. doi: 10.1128/EC.00015-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eichhorn H, Lessing F, Winterberg B, Schirawski J, Kamper J, et al. A ferroxidation/permeation iron uptake system is required for virulence in Ustilago maydis. Plant Cell. 2006;18:3332–3345. doi: 10.1105/tpc.106.043588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung WH, Sham A, Lian T, Singh A, Kosman DJ, et al. Iron source preference and regulation of iron uptake in Cryptococcus neoformans. PLoS Pathog. 2008;4:e45. doi: 10.1371/journal.ppat.0040045. doi:10.1371/journal.ppat.0040045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramanan N, Wang Y. A high-affinity iron permease essential for Candida albicans virulence. Science. 2000;288:1062–1064. doi: 10.1126/science.288.5468.1062. [DOI] [PubMed] [Google Scholar]
- 15.Heymann P, Gerads M, Schaller M, Dromer F, Winkelmann G, et al. The siderophore iron transporter of Candida albicans (Sit1p/Arn1p) mediates uptake of ferrichrome-type siderophores and is required for epithelial invasion. Infect Immun. 2002;70:5246–5255. doi: 10.1128/IAI.70.9.5246-5255.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith DG, Garcia-Pedrajas MD, Gold SE, Perlin MH. Isolation and characterization from pathogenic fungi of genes encoding ammonium permeases and their roles in dimorphism. Mol Microbiol. 2003;50:259–275. doi: 10.1046/j.1365-2958.2003.03680.x. [DOI] [PubMed] [Google Scholar]
- 17.Ren Q, Chen K, Paulsen IT. TransportDB: a comprehensive database resource for cytoplasmic membrane transport systems and outer membrane channels. Nucleic Acids Research. 2007;35:D274–279. doi: 10.1093/nar/gkl925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sipos G, Kuchler K. Fungal ATP-binding cassette (ABC) transporters in drug resistance detoxification. Curr Drug Targets. 2006;7:471–481. doi: 10.2174/138945006776359403. [DOI] [PubMed] [Google Scholar]
- 19.Rogers B, Decottignies A, Kolaczkowski M, Carvajal E, Balzi E, et al. The pleitropic drug ABC transporters from Saccharomyces cerevisiae. J Mol Microbiol Biotechnol. 2003;3:207–214. [PubMed] [Google Scholar]
- 20.Gbelska Y, Krijger J-J, Breunig KD. Evolution of gene families: the multidrug resistance transporter genes in five related yeast species. FEMS Yeast Research. 2006;6:345–355. doi: 10.1111/j.1567-1364.2006.00058.x. [DOI] [PubMed] [Google Scholar]
- 21.Higgins CF. ABC transporters: from microorganisms to man. Annu Rev Cell Biol. 1992;8:67–113. doi: 10.1146/annurev.cb.08.110192.000435. [DOI] [PubMed] [Google Scholar]
- 22.Saier MH. Tracing pathways of transport protein evolution. Mol Microbiol. 2003;48:1145–1156. doi: 10.1046/j.1365-2958.2003.03499.x. [DOI] [PubMed] [Google Scholar]
- 23.Pao SS, Paulsen IT, Saier MH., Jr Major facilitator superfamily. Microbiol Mol Biol Rev. 1998;62:1–34. doi: 10.1128/mmbr.62.1.1-34.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keller NP, Turner G, Bennett JW. Fungal secondary metabolism - from biochemistry to genomics. Nat Rev Microbiol. 2005;3:937–947. doi: 10.1038/nrmicro1286. [DOI] [PubMed] [Google Scholar]
- 25.Howlett BJ. Secondary metabolite toxins and nutrition of plant pathogenic fungi. Curr Opin Plant Biol. 2006;9:371–375. doi: 10.1016/j.pbi.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Johnson L. Iron and siderophores in fungal-host interactions. Mycol Res. 2008;112:170–183. doi: 10.1016/j.mycres.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 27.Haas H, Eisendle M, Turgeon BG. Siderophores in fungal physiology and virulence. Annu Rev Phytopathol. 2008;46:149–187. doi: 10.1146/annurev.phyto.45.062806.094338. [DOI] [PubMed] [Google Scholar]
- 28.Lee B-N, Kroken S, Chou DYT, Robbertse B, Yoder OC, et al. Functional analysis of all nonribosomal peptide synthetases in Cochliobolus heterostrophus reveals a factor, NPS6, involved in virulence and resistance to oxidative stress. Eukaryot Cell. 2005;4:545–555. doi: 10.1128/EC.4.3.545-555.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oide S, Moeder W, Krasnoff S, Gibson D, Haas H, et al. NPS6, encoding a nonribosomal peptide synthetase involved in siderophore-mediated iron metabolism, is a conserved virulence determinant of plant pathogenic ascomycetes. Plant Cell. 2006;18:2836–2853. doi: 10.1105/tpc.106.045633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schrettl M, Bignell E, Kragl C, Joechl C, Rogers T, et al. Siderophore biosynthesis but not reductive iron assimilation is essential for Aspergillus fumigatus virulence. J Exp Med. 2004;200:1213–1219. doi: 10.1084/jem.20041242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walton JD. Host-selective toxins: agents of compatibility. Plant Cell. 1996;8:1723–1733. doi: 10.1105/tpc.8.10.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friesen TL, Faris JD, Solomon PS, Oliver RP. Host-specific toxins: effectors of necrotrophic pathogenicity. Cell Microbiol. 2008;10:1421–1428. doi: 10.1111/j.1462-5822.2008.01153.x. [DOI] [PubMed] [Google Scholar]
- 33.Walton JD. HC-toxin. Phytochem. 2006;67:1406–1413. doi: 10.1016/j.phytochem.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 34.Pitkin J, Panaccione D, Walton J. A putative cyclic peptide efflux pump encoded by the TOXA gene of the plant-pathogenic fungus Cochliobolus carbonum. Microbiology. 1996;142:1557–1565. doi: 10.1099/13500872-142-6-1557. [DOI] [PubMed] [Google Scholar]
- 35.Callahan TM, Rose MS, Meade MJ, Ehrenshaft M, Upchurch RG. CFP, the putative cercosporin transporter of Cercospora kikuchii, is required for wild type cercosporin production, resistance, and virulence on soybean. Mol Plant-Microbe Interact. 1999;12:901–910. doi: 10.1094/MPMI.1999.12.10.901. [DOI] [PubMed] [Google Scholar]
- 36.Choquer M, Lee M, Bau H, Chung K. Deletion of a MFS transporter-like gene in Cerospora nicotianae reduces cerosporin toxin accumulation and fungal virulence. FEMS Letters. 2007;581:489–494. doi: 10.1016/j.febslet.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 37.Collemare J, Pianfetti M, Houlle A, Morin D, Camborde L, et al. Magnaporthe grisea avirulence gene ACE1 belongs to an infection-specific gene cluster involved in secondary metabolism. New Phytologist. 2008;179:196–208. doi: 10.1111/j.1469-8137.2008.02459.x. [DOI] [PubMed] [Google Scholar]
- 38.Gardiner DM, Jarvis RS, Howlett BJ. The ABC transporter gene in the sirodesmin biosynthetic gene cluster of Leptosphaeria maculans is not essential for sirodesmin production but facilitates self-protection. Fungal Genet Biol. 2005;42:257–263. doi: 10.1016/j.fgb.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Chang P-K, Yu J, Yu J-H. aflT, a MFS transporter-encoding gene located in the aflatoxin gene cluster, does not have a significant role in aflatoxin secretion. Fungal Genet Biol. 2004;41:911–920. doi: 10.1016/j.fgb.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Alexander N, McCormick S, Hohn T. TRI12, a trichothecene efflux pump from Fusarium sporotrichioides: gene isolation and expression in yeast. Mol Gen Genet. 1999;261:977–984. doi: 10.1007/s004380051046. [DOI] [PubMed] [Google Scholar]
- 41.Proctor RH, Brown DW, Plattner RD, Desjardins AE. Co-expression of 15 contiguous genes delineates a fumonisin biosynthetic gene cluster in Gibberella moniliformis. Fungal Genet Biol. 2003;38:237–249. doi: 10.1016/s1087-1845(02)00525-x. [DOI] [PubMed] [Google Scholar]
- 42.Ullan R, Liu G, Casqueiro J, Guitierrez S, Banuelos O, et al. The cefT gene of Acremonium chrysogenum C10 encodes a putative multidrug efflux pump protein that significantly increases cephalosporin C production. Mol Genet Genomics. 2002;267:673–683. doi: 10.1007/s00438-002-0702-5. [DOI] [PubMed] [Google Scholar]
- 43.Andrade A, van Nistelrooy J, Peery R, Skatrud P, de Waard M. The role of ABC transporters from Aspergillus nidulans in protection against cytotoxic agents and in antibiotic production. Mol Gen Genet. 2000;263:966–977. doi: 10.1007/pl00008697. [DOI] [PubMed] [Google Scholar]
- 44.Denny TP, VanEtten HD. Characterization of an inducible, nondegradative tolerance of Nectria haematococca MPVI to phytoalexins. J Gen Microbiol. 1983;129:2903–2913. [Google Scholar]
- 45.Denny TP, Matthews PS, VanEtten HD. A possible mechanism of nondegradative tolerance of pisatin in Nectria haematococca MPVI. Physiol Mol Plant Pathol. 1987;30:93–107. [Google Scholar]
- 46.Urban M, Bhargava T, Hamer JE. An ATP-driven efflux pump is a novel pathogenicity factor in rice blast disease. EMBO J. 1999;18:512–521. doi: 10.1093/emboj/18.3.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zwiers L-H, De Waard MA. Characterization of the ABC transporter genes MgAtr1 and MgAtr2 from the wheat pathogen Mycosphaerella graminicola. Fungal Genet Biol. 2000;30:115–125. doi: 10.1006/fgbi.2000.1209. [DOI] [PubMed] [Google Scholar]
- 48.Schoonbeek H, Del Sorbo G, De Waard MA. The ABC transporter BcatrB affects the sensitivity of Botrytis cinerea to the phytoalexin resveratrol and the fungicide fenpiclonil. Mol Plant-Microbe Interact. 2001;14:562–571. doi: 10.1094/MPMI.2001.14.4.562. [DOI] [PubMed] [Google Scholar]
- 49.Stergiopoulos I, Zwiers L-H, De Waard MA. The ABC transporter MgAtr4 is a virulence factor of Mycosphaerella graminicola that affects colonization of substomatal cavities in wheat leaves. Mol Plant-Microbe Interact. 2003;16:689–698. doi: 10.1094/MPMI.2003.16.8.689. [DOI] [PubMed] [Google Scholar]
- 50.Schoonbeek H, van Nistelrooy J, de Waard MA. Functional analysis of ABC transporter genes from Botrytis cinerea identifies BcatrB as a transporter of eugenol. Eur J Plant Pathol. 2003;109:1003–1011. [Google Scholar]
- 51.Fleissner A, Sopalla C, Weltring K-M. An ATP-binding cassette multidrug-resistance transporter is necessary for tolerance of Gibberella pulicaris to phytoalexins and virulence on potato tubers. Mol Plant-Microbe Interact. 2002;15:102–108. doi: 10.1094/MPMI.2002.15.2.102. [DOI] [PubMed] [Google Scholar]
- 52.Han Y, Liu X, Benny U, Kistler HC, VanEtten HD. Genes determining pathogenicity to pea are clustered on a supernumerary chromosome in the fungal plant pathogen Nectria haematococca. Plant J. 2001;25:305–314. doi: 10.1046/j.1365-313x.2001.00969.x. [DOI] [PubMed] [Google Scholar]
- 53.Liu X, Inlow M, VanEtten HD. Expression profiles of pea pathogenicity (PEP) genes in vivo and in vitro, characterization of the flanking regions of the PEP cluster and evidence that the PEP cluster region resulted from horizontal gene transfer in the fungal pathogen Nectria haematococca. Curr Genet. 2003;44:95–103. doi: 10.1007/s00294-003-0428-x. [DOI] [PubMed] [Google Scholar]
- 54.de Waard MA, Andrade AC, Hayashi K, Schoonbeek H-j, Stergiopoulos I, et al. Impact of fungal drug transporters on fungicide sensitivity, multidrug resistance and virulence. Pest Manag Sci. 2006;62:195–207. doi: 10.1002/ps.1150. [DOI] [PubMed] [Google Scholar]
- 55.Theiss S, Kretschmar M, Nichterlein T, Hof H, Agabian N, et al. Functional analysis of a vacuolar ABC transporter in wild-type Candida albicans reveals its involvement in virulence. Mol Microbiol. 2002;43:571–584. doi: 10.1046/j.1365-2958.2002.02769.x. [DOI] [PubMed] [Google Scholar]
- 56.Petrovic S, Pascolo L, Gallo R, Cupelli F, Ostrow JD, et al. The products of YCF1 and YLL015w (BPT1) cooperate for the ATP-dependent vacuolar transport of unconjugated bilirubin in Saccharomyces cerevisiae. Yeast. 2000;16:561–571. doi: 10.1002/(SICI)1097-0061(200004)16:6<561::AID-YEA551>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 57.Klein M, Mamnun YM, Eggmann T, Schueller C, Wolfger H, et al. The ATP-binding cassette (ABC) transporter Bpt1p mediates vacuolar sequestration of glutathione conjugates in yeast. FEBS Lett. 2002;520:63–67. doi: 10.1016/s0014-5793(02)02767-9. [DOI] [PubMed] [Google Scholar]
- 58.Posteraro B, Sanguinetti M, Sanglard D, La Sorda M, Boccia S, et al. Identification and characterization of a Cryptococcus neoformans ATP binding cassette (ABC) transporter-encoding gene, CnAFR1, involved in the resistance to fluconazole. Mol Microbiol. 2003;47:357–371. doi: 10.1046/j.1365-2958.2003.03281.x. [DOI] [PubMed] [Google Scholar]
- 59.Sanglard D, Ischer F, Calabrese D, Majcherczyk PA, Bille J. The ATP binding cassette transporter gene CgCDR1 from Candida glabrata is involved in the resistance of clinical isolates to azole antifungal agents. Antimicrob Agents Chemother. 1999;43:2753–2765. doi: 10.1128/aac.43.11.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prasad R, Dewergifosse P, Goffeau A, E B. Molecular cloning and characterization of a novel gene of Candida albicans, CDR1, conferring multiple resistance to drugs and antifungals. Curr Genet. 1995;27:320–329. doi: 10.1007/BF00352101. [DOI] [PubMed] [Google Scholar]
- 61.Miyazaki H, Miyazaki Y, Geber A, Parkinson T, Hitchcock C, et al. Fluconazole resistance associated with drug efflux and increased transcription of a drug transporter gene, PDH1, in Candida glabrata. Antimicrob Agents Chemother. 1998;42:1695–1701. doi: 10.1128/aac.42.7.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Torelli R, Posteraro B, Ferrari S, La Sorda M, Fadda G, et al. The ATP-binding cassette transporter-encoding gene CgSNQ2 is contributing to the CgPDR1-dependent azole resistance of Candida glabrata. Mol Microbiol. 2008;68:186–201. doi: 10.1111/j.1365-2958.2008.06143.x. [DOI] [PubMed] [Google Scholar]
- 63.Katiyar SK, TD E. Identification and expression of multidrug resistance related ABC transporter genes in Candida krusei. Medical Mycology. 2001;39:109–116. doi: 10.1080/mmy.39.1.109.116. [DOI] [PubMed] [Google Scholar]
- 64.Helmerhorst EJ, Venuleo C, Sanglard D, Oppenheim FG. Roles of cellular respiration, CgCDR1, and CgCDR2 in Candida glabrata resistance to histatin 5. Antimicrob Agents Chemother. 2006;50:1100–1103. doi: 10.1128/AAC.50.3.1100-1103.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Niimi K, Maki K, Ikeda F, Holmes AR, Lamping E, et al. Overexpression of Candida albicans CDR1, CDR2, or MDR1 does not produce significant changes in echinocandin susceptibility. Antimicrob Agents Chemother. 2006;50:1148–1155. doi: 10.1128/AAC.50.4.1148-1155.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dean M, Rzhetsky A, R A. The human ATP-binding cassette (ABC) transporter superfamily. Genome Res. 2001;11:1156–1166. doi: 10.1101/gr.184901. [DOI] [PubMed] [Google Scholar]
- 67.Sheps JA, Ralph S, Zhao Z, Baillie DL, V L. The ABC transporter gene family of Caenorhabditis elegans has implications for the evolutionary dynamics of multidrug resistance in eukaryotes. Genome Biol. 2004;5:R15. doi: 10.1186/gb-2004-5-3-r15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smriti KS, Dixit BL, Gupta CM, Milewski S, R P. ABC transporters Cdr1p, Cdr2p and Cdr3p of a human pathogen Candida albicans are general phospholipid translocators. Yeast. 2002;19:303–318. doi: 10.1002/yea.818. [DOI] [PubMed] [Google Scholar]
- 69.Cheng G, Yeater KM, LL H. Cellular and molecular biology of Candida albicans estrogen response. Eukaryot Cell. 2006;5:180–191. doi: 10.1128/EC.5.1.180-191.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shukla S, Rai V, Saini P, Banerjee D, AK M, et al. Candida drug resistance protein 1, a major multidrug ATP binding cassette transporter of Candida albicans, translocates fluorescent phospholipids in a reconstituted system. Biochemistry. 2007;46:12081–12090. doi: 10.1021/bi700453e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sanglard D, Ischer F, Monod M, Bille J. Cloning of Candida albicans genes conferring resistance to azole antifungal agents: characterization of CDR2, a new multidrug ABC transporter gene. Microbiology. 1997;143:405–416. doi: 10.1099/00221287-143-2-405. [DOI] [PubMed] [Google Scholar]
- 72.Gauthier C, Weber S, Alarco A-M, Alqawi O, Daoud R, et al. Functional similarities and differences between Candida albicans Cdr1p and Cdr2p transporters. Antimicrob Agents Chemother. 2003;47:1543–1554. doi: 10.1128/AAC.47.5.1543-1554.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Holmes AR, Tsao S, Ong S-W, Lamping E, Niimi K, et al. Heterozygosity and functional allelic variation in the Candida albicans efflux pump genes CDR1 and CDR2. Mol Microbiol. 2006;62:170–186. doi: 10.1111/j.1365-2958.2006.05357.x. [DOI] [PubMed] [Google Scholar]
- 74.Blackmore CG, McNaughton PA, van Veen HW. Multidrug transporters in prokaryotic and eukaryotic cells: physiological functions and transport mechanisms. Mol Membr Biol. 2001;18:97–103. doi: 10.1080/09687680010030200. [DOI] [PubMed] [Google Scholar]
- 75.Borges-Walmsley MI, Walmsley AR. The structure and function of drug pumps. Trends Microbiol. 2001;9:71–79. doi: 10.1016/s0966-842x(00)01920-x. [DOI] [PubMed] [Google Scholar]
- 76.Goldway M, Teff D, Schmidt R, Oppenheim AB, Koltin Y. Multidrug resistance in Candida albicans: disruption of the BENr gene. Antimicrob Agents Chemother. 1995;39:422–426. doi: 10.1128/aac.39.2.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wirsching S, Michel S, Morschhäuser J. Targeted gene disruption in Candida albicans wild-type strains: the role of the MDR1 gene in fluconazole resistance of clinical Candida albicans isolates. Mol Microbiol. 2000;36:856–865. doi: 10.1046/j.1365-2958.2000.01899.x. [DOI] [PubMed] [Google Scholar]
- 78.Pasrija R, Banerjee D, Prasad R. Structure and function analysis of CaMdr1p, a major facilitator superfamily antifungal efflux transporter protein of Candida albicans: identification of amino acid residues critical for drug/H+ transport. Eukaryot Cell. 2007;6:443–453. doi: 10.1128/EC.00315-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Calabrese D, Bille J, Sanglard D. A novel multidrug efflux transporter gene of the major facilitator superfamily from Candida albicans (FLU1) conferring resistance to fluconazole. Microbiology. 2000;146:2743–2754. doi: 10.1099/00221287-146-11-2743. [DOI] [PubMed] [Google Scholar]
- 80.Moran GP, Sanglard D, Donnelly SM, Shanley DB, Sullivan DJ, et al. Identification and expression of multidrug transporters responsible for fluconazole resistance in Candida dubliniensis. Antimicrob Agents Chemother. 1998;42:1819–1830. doi: 10.1128/aac.42.7.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wirsching S, Moran GP, Sullivan DJ, Coleman DC, Morschhauser J. MDR1-mediated drug resistance in Candida dubliniensis. Antimicrob Agents Chemother. 2001;45:3416–3421. doi: 10.1128/AAC.45.12.3416-3421.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Barchiesi F, Calabrese D, Sanglard D, Falconi Di Francesco L, Caselli F, et al. Experimental induction of fluconazole resistance in Candida tropicalis ATCC 750. Antimicrob Agents Chemother. 2000;44:1578–1584. doi: 10.1128/aac.44.6.1578-1584.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sengupta M, Datta A. Two membrane proteins located in the Nag regulon of Candida albicans confer multidrug resistance. Biochem Biophys Res Commun. 2003;301:1099–1108. doi: 10.1016/s0006-291x(03)00094-9. [DOI] [PubMed] [Google Scholar]
- 84.Saidane S, Weber S, De Deken X, St-Germain G, Raymond M. PDR16-mediated azole resistance in Candida albicans. Mol Microbiol. 2006;60:1546–1562. doi: 10.1111/j.1365-2958.2006.05196.x. [DOI] [PubMed] [Google Scholar]
- 85.Sanglard D, Ischer F, Bille J. Role of ATP-binding-cassette transporter genes in high-frequency acquisition of resistance to azole antifungals in Candida glabrata. Antimicrob Agents Chemother. 2001;45:1174–1183. doi: 10.1128/AAC.45.4.1174-1183.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Borst A, Raimer MT, Warnock DW, Morrison CJ, Arthington-Skaggs BA. Rapid acquisition of stable azole resistance by Candida glabrata isolates obtained before the clinical introduction of fluconazole. Antimicrob Agents Chemother. 2005;49:783–787. doi: 10.1128/AAC.49.2.783-787.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.White TC. Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob Agents Chemother. 1997;41:1482–1487. doi: 10.1128/aac.41.7.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Marr KA, Lyons CN, Rustad T, Bowden RA, White TC. Rapid, transient fluconazole resistance in Candida albicans is associated with increased mRNA levels of CDR. Antimicrob Agents Chemother. 1998;42:2584–2589. doi: 10.1128/aac.42.10.2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.White TC, Marr KA, Bowden RA. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin Microbiol Rev. 1998;11:382–402. doi: 10.1128/cmr.11.2.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.White TC, Holleman S, Dy F, Mirels LF, Stevens DA. Resistance mechanisms in clinical isolates of Candida albicans. Antimicrob Agents Chemother. 2002;46:1704–1713. doi: 10.1128/AAC.46.6.1704-1713.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cowen LE, Steinbach WJ. Stress, drugs, and evolution: the role of cellular signaling in fungal drug resistance. Eukaryot Cell. 2008;7:747–764. doi: 10.1128/EC.00041-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Micheli Md, Bille J, Schueller C, Sanglard D. A common drug-responsive element mediates the upregulation of the Candida albicans ABC transporters CDR1 and CDR2 , two genes involved in antifungal drug resistance. Mol Microbiol. 2002;43:1197–1214. doi: 10.1046/j.1365-2958.2002.02814.x. [DOI] [PubMed] [Google Scholar]
- 93.Coste AT, Karababa M, Ischer F, Bille J, Sanglard D. TAC1, transcriptional activator of CDR genes, is a new transcription factor involved in the regulation of Candida albicans ABC Transporters CDR1 and CDR2. Eukaryot Cell. 2004;3:1639–1652. doi: 10.1128/EC.3.6.1639-1652.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Perepnikhatka V, Fischer FJ, Niimi M, Baker RA, Cannon RD, et al. Specific chromosome alterations in fluconazole-resistant mutants of Candida albicans. J Bacteriol. 1999;181:4041–4049. doi: 10.1128/jb.181.13.4041-4049.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lyons CN, White TC. Transcriptional analyses of antifungal drug resistance in Candida albicans. Antimicrob Agents Chemother. 2000;44:2296–2303. doi: 10.1128/aac.44.9.2296-2303.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Selmecki A, Forche A, Berman J. Aneuploidy and isochromosome formation in drug-resistant Candida albicans. Science. 2006;313:367–370. doi: 10.1126/science.1128242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Thakur JK, Arthanari H, Yang F, Pan S-J, Fan X, et al. A nuclear receptor-like pathway regulating multidrug resistance in fungi. Nature. 2008;452:604–609. doi: 10.1038/nature06836. [DOI] [PubMed] [Google Scholar]
- 98.Morschhäuser J, Barker KS, Liu TT, Blaβ-Warmuth J, Homayouni R, et al. The transcription factor Mrr1p controls expression of the MDR1 efflux pump and mediates multidrug resistance in Candida albicans. PLoS Pathog. 2007;3:e164. doi: 10.1371/journal.ppat.0030164. doi:10.1371/journal.ppat.0030164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dunkel N, Blaβ J, Rogers PD, Morschhäuser J. Mutations in the multi-drug resistance regulator MRR1, followed by loss of heterozygosity, are the main cause of MDR1 overexpression in fluconazole-resistant Candida albicans strains. Mol Microbiol. 2008;69:827–840. doi: 10.1111/j.1365-2958.2008.06309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Coste A, Turner V, Ischer F, Morschhauser J, Forche A, et al. A mutation in Tac1p, a transcription factor regulating CDR1 and CDR2, is coupled with loss of heterozygosity at chromosome 5 to mediate antifungal resistance in Candida albicans. Genetics. 2006;172:2139–2156. doi: 10.1534/genetics.105.054767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen C-G, Yang Y-L, Shih H-I, Su C-L, Lo H-J. CaNdt80 is involved in drug resistance in Candida albicans by regulating CDR1. Antimicrob Agents Chemother. 2004;48:4505–4512. doi: 10.1128/AAC.48.12.4505-4512.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rognon B, Kozovska Z, Coste AT, Pardini G, Sanglard D. Identification of promoter elements responsible for the regulation of MDR1 from Candida albicans, a major facilitator transporter involved in azole resistance. Microbiology. 2006;152:3701–3722. doi: 10.1099/mic.0.29277-0. [DOI] [PubMed] [Google Scholar]
- 103.Riggle PJ, Kumamoto CA. Transcriptional regulation of MDR1, encoding a drug efflux determinant, in fluconazole-resistant Candida albicans strains through an Mcm1p binding site. Eukaryot Cell. 2006;5:1957–1968. doi: 10.1128/EC.00243-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Manoharlal R, Gaur NA, Panwar SL, Morschhauser J, Prasad R. Transcriptional activation and increased mRNA stability contribute to overexpression of CDR1 in azole-resistant Candida albicans. Antimicrob Agents Chemother. 2008;52:1481–1492. doi: 10.1128/AAC.01106-07. [DOI] [PMC free article] [PubMed] [Google Scholar]