Abstract
Background:
The BODE index was recently validated as a multidimensional tool for the evaluation of patients with COPD. The influence of gender on the BODE index has not been studied.
Hypothesis:
The contribution of each component of the disease to the BODE index may differ according to gender.
Methods:
We evaluated age, forced expiratory volume in one second (FEV1), Modified Medical Research Council (MMRC) score, 6-min walk distance (6MWD), and body mass index (BMI) in 52 men and 52 women with COPD and the same BODE index. We compared the studied parameters between men and women and then performed a multiple regression analysis by gender.
Results:
We found statistically significant differences between men and women in all parameters: FEV1 % (55 ± 17 vs 63 ± 18, p < 0.001), MMRC [1 (0–2) vs 1 (1–2) p = 0.03], BMI [28 (26–30) vs 25 (22–30), p = 0.05], and 6MWD [546 (451–592) vs 462 (419–520), p = 0.001]. Multiple regression analysis revealed that each component of the BODE index had different weight (β standardized coefficient) in men and women respectively: FEV1% (0.74 vs 0.62), MMRC (0.31 vs 0.48), BMI (−0.09 vs −0.17), and 6MWD (0.13 vs 0.10).
Conclusions:
The contribution of each component to the BODE index differs by gender in subjects with similar BODE scores. Long term longitudinal studies will help determine the significance of our findings.
Keywords: Gender, COPD, BODE index
Introduction
Chronic Obstructive Pulmonary Disease (COPD), is characterized by poorly reversible airflow limitation and is predicted to be the third leading cause of death world-wide by 2020 (Murray and Lopez 1997). According to recent COPD disease surveillance in the United States there was a five-fold increase in female COPD-related mortality between 1971 and 2000 and in 2000 for the first time, more women died from COPD than men (Mannino et al 2002).
The risk of death in patients with COPD is often graded with the use of a single physiological variable, the forced expiratory volume in one second (FEV1) (Siafakas et al 1995). However, a multidimensional evaluation of disease severity and prognosis: the BODE index (Body mass index, degree of airway Obstruction, Dyspnea and Exercise capacity) has been recently validated in a population of predominantly male COPD patients as a better independent predictor of respiratory and overall mortality than FEV1% (Celli et al 2004). Another study (Celli et al 2005) of 816 patients with COPD investigating the prognostic significance of 40 potential staging variables identified 3 key elements of a multidimensional grading system that proved to be useful in the evaluation of the disease.
We have recently identified gender differences in the clinical presentation of the disease in FEV1% matched populations (de Torres et al 2005). We also observed that the main components of the disease evaluated by the BODE index (body mass index [BMI], Modified Medical Research Council [MMRC], and 6-min walk distance [6MWD]) were different in men and women.
We therefore postulated that the relative weight each component has on the total BODE score could differ by gender. To prove this hypothesis we planned this cross sectional comparative study of 52 men and 52 women with the same BODE index and investigated the relative contribution of each of the components to the total BODE index.
Methods
This matched case series study, recruited women and men with COPD attending an outpatient pulmonary clinic at Hospital Universitario Ntra Sra de Candelaria; a tertiary referral center in Santa Cruz de Tenerife, Spain from January 2000 to March 2006. Patients with any degree ofseverity were included if they had smoked ≥10 pack years, and had a post-bronchodilator FEV1/forced vital capacity (FVC) of < 0.7 after 400 μg of inhaled albuterol. Patients were excluded if they had a history of asthma, bronchiectasis, tuberculosis, or other confounding diseases. The patients were clinically stable (no exacerbations for at least 2 months) at the time of the evaluation and were part of the BODE international multicenter study (Celli et al 2004). The Institutional Ethics Committee approved the study, and all patients signed an informed consent.
We evaluated the following parameters in the study sample: age, spirometry (FEV1, FVC, FEV1/FVC), dyspnoea by the MMRC, BMI (weight in kilograms divided by height in meters2), and the 6MWD test. Postbronchodilator FEV1% of predicted, FVC% of predicted and FEV1/FVC values were determined using the European Community for Steel and Coal reference values for Spain (Quanjer 1983) and using a Jaegger 920 MasterLab® Body Box. The MMRC (Brooks 1982) is a dyspnoea scale that ranges from 0 (dyspnoea only with intense physical activity), to 4 (dyspnoea with minimal activity such as getting dressed). The 6MWD test was performed according to published ATS recommendations (ATS 2002).
Patients were matched from an initial sample of 111 males and 52 females with COPD. We were able to match every female patient with a corresponding male with identical BODE index. When more than one male matched, we randomly chose the patient to be included in the final sample. A blinded investigator performed case matching.
Statistical analysis
We describe each variable using mean ± SD or median (25th percentile-75th percentile) depending on distribution. We compared differences between men and women with student t test or Mann-Whitney’s U test depending on distribution. We then performed a multiple regression analysis with BODE index as the dependent variable and those parameters included in the index as predictors. A p value ≤ 0.05 was considered statistically significant. The analysis was performed with SPSS® (software version 12, Chicago, IL, USA).
Results
The clinical characteristics of the patients participating in the study are described in Table 1. Female participants were younger, had better lung function, higher dyspnoea scores, and worse nutritional status and exercise capacity than men. The distribution of patients classified by the GOLD staging system was gender dependent, but no differences were found in the classification by BODE index quartiles.
Table 1.
Clinical characteristics of patients
| Clinical parameter | Men (n = 52) | Women (n = 52) | p Value |
|---|---|---|---|
| Age (yrs) | 63 ± 8 | 55 ± 11 | < 0.001* |
| FEV1% of predicted | 55 ± 17 | 63 ± 18 | 0.03* |
| FVC % of predicted | 86 ± 17 | 93 ± 23 | 0.03* |
| FEV1/FVC | 50 ± 10 | 56 ± 10 | 0.005* |
| MMRC (points) | 1 (0–2) | 1 (1–2) | 0.035* |
| BMI (Kg/m2) | 28 (26–30) | 25 (22–30) | 0.05* |
| 6MWD (m) | 546 (451–592) | 462 (419–520) | 0.001* |
| GOLD Stage (%) | |||
| I | 7 | 19 | 0.32 |
| II | 54 | 54 | |
| II | 33 | 25 | |
| IV | 6 | 2 | |
| BODE quartiles (%) | |||
| 1st (0–2) | 71 | 71 | 0.78 |
| 2nd(3–4) | 25 | 25 | |
| 3rd(5–6) | 4 | 4 | |
| 4th(7–10) | 0 | 0 |
Note: Expressed as mean ± SD or median (25–75th percentiles); p ≤ 0.05 considered statistically significant.
Abbreviations: BMI, body mass index; BODE, Body mass index, degree of airway Obstruction, Dyspnea and Exercise capacity; GOLD, global obstructive lung disease; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; MMRC, Modified Medical Research Council; SD, standard deviation; 6MWD, 6-minute walk distance.
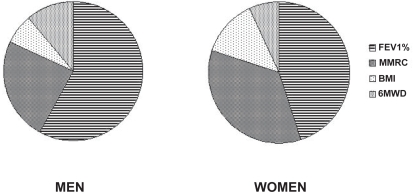
Table 2 shows a description of the variables and points values used for the computation of the BODE index. Table 3 shows the results of the lineal regression analysis by gender with BODE index as the dependent variable and its components as independent predictors of its score. There were gender differences in the relative weight that each component of the BODE index had on the total score. This is shown in Figure 1 where each component represents the percentage of the total BODE score. MMRC and BMI contributed most to the overall score in women, while FEV1% and 6MWD were more significant in men.
Table 2.
Variables and points values used for the computation of the BODE index
| Variable | Points of BODE index | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| FEV1% of predicted | ≥65 | 50–64 | 36–49 | ≤35 |
| 6MWD (m) | ≥350 | 250–349 | 150–249 | ≤149 |
| MMRC | 0–1 | 2 | 3 | 4 |
| BMI | >21 | ≤21 | ||
Note: Total possible values range from 0 to 10.
Abbreviations: BMI, body mass index; BODE, Body mass index, degree of airway Obstruction, Dyspnea and Exercise capacity; FEV1, forced expiratory volume in one second; MMRC, Modified Medical Research Council; 6MWD, 6-minute walk distance.
Table 3.
Results of the lineal regression analysis by gender with BODE index
| Variable | Men | Women |
|---|---|---|
| FEV1% | 0.75 | 0.62 |
| MMRC | 0.30 | 0.49 |
| BMI | −0.09 | −0.17 |
| 6MWD | 0.13 | 0.11 |
Note: R2=0.98 for men and R2=0.99 for women; All standardized coefficients with p < 0.001.
Abbreviations: BMI, body mass index; BODE, Body mass index, degree of airway Obstruction, Dyspnea and Exercise capacity; FEV1, forced expiratory volume in one second; MMRC, Modified Medical Research Council; 6MWD, 6-minute walk distance.
Figure 1.
Percentage of relative weight of each of the parameters over the total BODE index.
Abbreviations: BMI, body mass index; BODE, Body mass index, degree of airway Obstruction, Dyspnea and Exercise capacity; FEV1, forced expiratory volume in one second; MMRC, Modified Medical Research Council; 6MWD, 6-minute walk distance.
Discussion
COPD is now considered a respiratory disease with important systemic consequences (Agusti et al 2003). Several studies have shown that there are different independent clinical parameters that help predict survival in patients with COPD (Anthonisen et al 1986; Nishimura et al 2002; Pinto-Plata et al 2004; Vestbo et al 2005). This independent relationship has been confirmed in a factor analysis performed in a large cohort of patients. Indeed, the FEV1, degree of dyspnoea, and exercise capacity, provide independent information regarding the degree of compromise in patients with COPD (Ries et al 1991). Recently Celli and colleagues (2004) combined these three variables with BMI and developed a multi-dimensional score reflecting 3 important dimensions of the disease: airflow limitation (FEV1%), symptoms (MMRC), and systemic manifestations (BMI and 6MWD). The BODE index predicts respiratory and overall mortality better than FEV1. These findings suggest that the clinical evaluation of all patients with COPD should include the BODE index. Unfortunately, one important limitation recognized in the Celli study was the small number of women participants (only 17 patients out of 625). Therefore, including the BODE index as an integral part of the evaluation of female patients with COPD is questionable. Another recent study by a group of experts in the disease (Celli et al 2005) studied over 40 potential staging variables in a population of 816 COPD patients participating in drug trials, evaluating them according to sensitivity to change, measured reproducibly, independence of the information they provide, and prognostic value. They performed principal component analysis and identified 6 independent groups: pulmonary function (including FEV1), symptoms of cough and sputum, dyspnoea, health status, bronchodilator reversibility, and BMI. They selected 3 variables (FEV1, MMRC, and BMI) and elaborated a multidimensional score that proved to be useful in predicting outcome.
We have recently found (de Torres et al 2005) that men and women with the same FEV1% show differences in the clinical presentation of the disease. We found significant differences in all the components of the BODE index. Women had worse dyspnoea, exercise capacity, and nutritional status at an earlier stage of the disease.
Our present study shows that the proportional weight of each component over the total score of the index differs in men and women with COPD. Furthermore, the order of importance of these domains is not the same in the two genders. The individual weight of each variable was gender specific: the contribution of FEV1% and 6MWD was greater in men while MMRC and BMI had a greater impact in women’s BODE indices. This finding is very interesting because it might imply fundamental differences in the expression and perception of respiratory disease in men and women. This observation supports the need to adequately assess every dimension of COPD beyond respiratory impairment. In addition, the results support the use of the BODE index, because it takes into account respiratory symptoms and the systemic implications of this illness beyond airflow limitation incorporating them into a single expression of important clinical value.
The BODE index addresses gender specific limitations of spirometry or the GOLD (Global Obstructive Lung Disease) classification which are heavily dependent on the severity of airflow limitation and largely ignore symptoms and systemic consequences of COPD such as nutritional status. Indeed, while classification of disease severity based on airflow limitation might be best suited to male patients with COPD, we run the risk of underestimating the burden of disease in female patients by ignoring the important contribution of BMI and dyspnoea in these patients. Reliance on the BODE index helps address these issues by incorporating those other domains that are more frequently altered in women with the disease.
The importance of nutritional status in patients with COPD has been reported. Mortality sharply increases when BMI falls below 21 (Vestbo et al 2005). We found lower BMIs for a given BODE score in female patients when compared with their matched male controls. In fact, BMI had greater relative weight in women over the total BODE index score than men. This implies that a nutritional evaluation is especially important in women with COPD, and should be included alone or integrated in a composite index in the standard assessment of female patients with this disease.
Our women with COPD walked a shorter distance in the 6MWD test. This finding has been previously reported elsewhere (Celli et al 2005). When we take into consideration their predictive values according to the European predictive equation (Troosters et al 1999) we see that these fall within the normal range for both men and women. The novel finding of the present study was the greater relative importance that this has in the multisystemic component of the disease in men.
The main limitation of our study is its cross-sectional design. We still do not know how the different quartiles of the BODE index reflect the evolution and survival of the disease in a population of women with COPD. Furthermore, we do not know whether interventions shown to improve the BODE index and survival of male patients with COPD such as lung volume reduction surgery (LVRS) (Imfeld et al 2006) or pulmonary rehabilitation (Cote and Celli 2005), have the same effects in women. Another limitation is that our study includes patients mainly in GOLD stages II and III or in the lower quartiles of the BODE index. We do not know if the same findings apply to other populations not included in this study, including patients with higher BODE indices.
In conclusion, we have demonstrated that the relative weight of each component of the BODE index differs by gender. Perception of disease and nutritional status has a more important role in women with COPD when a multidimensional evaluation of the disease is performed. We believe the BODE index, might be particularly useful in assessing COPD severity in women because it takes into account those aspects of the disease most relevant to this population for a given degree of airflow obstruction. Since the BODE index was validated primarily in a population of men with COPD, one can only hope that future longitudinal studies might prove it to be even more useful in the evaluation of women with COPD.
References
- Agustí AGN, Noguera A, Sauleda J, et al. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003;21:347–60. doi: 10.1183/09031936.03.00405703. [DOI] [PubMed] [Google Scholar]
- Anthonisen NR, Wright EC, Hodgkin JE. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986;133:14–20. doi: 10.1164/arrd.1986.133.1.14. [DOI] [PubMed] [Google Scholar]
- [ATS] ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS Statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–17. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- Brooks SM. Surveillance for respiratory hazards. ATS News. 1982;8:12–16. [Google Scholar]
- Celli BR, Calverley PM, Rennard SI, et al. Proposal for a multidimensional staging system for chronic obstructive pulmonary disease. Respir Med. 2005;99:1546–54. doi: 10.1016/j.rmed.2005.03.019. [DOI] [PubMed] [Google Scholar]
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J. 2005;26:630–6. doi: 10.1183/09031936.05.00045505. [DOI] [PubMed] [Google Scholar]
- de Torres JP, Casanova C, Hernandez C, et al. Gender and COPD in patients attending a pulmonary clinic. Chest. 2005;128:2012–16. doi: 10.1378/chest.128.4.2012. [DOI] [PubMed] [Google Scholar]
- Imfeld S, Bloch KE, Weder W, et al. The BODE index after lung volume reduction surgery correlates with survival. Chest. 2006;129:873–8. doi: 10.1378/chest.129.4.873. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, et al. Chronic pulmonary disease surveillance - United States, 1971–2000. Respir Care. 2002;47:1184–99. [PubMed] [Google Scholar]
- Murray CJL, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- Nishimura K, Izumi T, Tsukino M, et al. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121:1434–40. doi: 10.1378/chest.121.5.1434. [DOI] [PubMed] [Google Scholar]
- Pinto-Plata VM, Cote C, Cabral, et al. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J. 2004;23:28–33. doi: 10.1183/09031936.03.00034603. [DOI] [PubMed] [Google Scholar]
- Quanjer PH. Standardized lung function testing. Report of the Working Party for the European Community for Steel and Coal. Bull Eur Physiopath Respir. 1983;19(supp 5):22–7. [Google Scholar]
- Ries AL, Kaplan RM, Blumberg E. Use of factor analysis to consolidate multiple outcome measures in chronic obstructive pulmonary disease. J Clin Epidemiol. 1991;44:497–503. doi: 10.1016/0895-4356(91)90212-r. [DOI] [PubMed] [Google Scholar]
- Siafakas NM, Vermeire P, Pride NB, et al. on behalf of the Task Force Optimal assessment and management of chronic obstructive pulmonary disease (COPD) Eur Respir J. 1995;8:1398–420. doi: 10.1183/09031936.95.08081398. [DOI] [PubMed] [Google Scholar]
- Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J. 1999;14:270–4. doi: 10.1034/j.1399-3003.1999.14b06.x. [DOI] [PubMed] [Google Scholar]
- Vestbo J, Prescott E, Almdal T, et al. 2005Body mass, fat free body mass and prognosis in COPD patients from a random population sample Am J Respir Crit Care Med September15[Epub]. [DOI] [PubMed] [Google Scholar]