Abstract
Objectives
To determine how three different physical performance measures (PPM) combine for added utility in predicting adverse health events in elders.
Design
Prospective cohort study.
Setting
Health, Aging, and Body Composition Study.
Participants
3,024 well-functioning older persons (mean age 73.6 years).
Measurements
Timed gait, repeated chair stands and balance (semi- and full-tandem, and single leg stands each held for 30 seconds) tests were administered at baseline. Usual gait speed was categorized to distinguish high and low risk participants using the previously established 1 m/sec cut-point. The same population-percentile (21.3%) was used to identify cut-points for repeated chair stands (17.05 sec) and balance (53 sec) tests. Cox proportional hazard analyses were performed to evaluate the added value of PPM in predicting mortality, hospitalization, and (severe) mobility limitation events over 6.9 years of follow-up.
Results
Risk estimates for developing adverse health-related events were similarly large for each of the three high risk groups considered separately. A greater number of PPM scores at the high risk level was associated with a greater risk of developing adverse health-related events. When all three PPMs were considered, having only one poor performance was sufficient to indicate a highly significant higher risk of (severe) lower extremity and mortality events.
Conclusion
Although gait speed is considered the most important predictor of adverse health events, these findings demonstrate that poor performance on other tests of lower extremity function are equally prognostic. This suggests that chair stand and standing balance performance may be adequate substitutes when gait speed is unavailable.
Keywords: Short Physical Performance Battery, Functional limitation, Death, Hospitalization, Usual gait speed
INTRODUCTION
During the last decade, physical performance measures have gained increased acceptance in the evaluation of functional status of older persons. One of the most commonly used measures of physical performance is the Short Physical Performance Battery (SPPB)1–3. This measure evaluates lower extremity function through tests of gait speed, standing balance, and time to rise from a chair five times. The SPPB not only provides information about physical function, but also predicts major adverse health-related events in the elderly, such as disability1–3, nursing home admission1, and mortality1. This measure also has been associated with several physiological factors, such as inflammation4 and body composition changes5, believed to be involved in the disablement process and which may underlie specific health-related events.
A study by Guralnik and colleagues3 has suggested that timed usual gait, one of the three tasks, provides a predictive value for the onset of disability similar to that obtained for the complete SPPB. However, in that study, the predictive value of usual gait speed was compared with that of the total SPPB for the onset of disability, considering each physical performance measure as a continuous variable. The use of continuous measurements may have limited applicability in clinical settings, where biological markers are typically dichotomized or treated as threshold markers for providing meaningful information.
The present study aims to evaluate the added value of the three tasks included in the SPPB (i.e. usual gait speed, chair stands, and balance tests) for predicting incident adverse health-related events. Analyses will be conducted using dichotomized assessments of physical performance to mirror their potential clinical application.
METHODS
This study uses data from the Health, Aging and Body Composition (Health ABC) study, a prospective cohort study designed to investigate the impact of body composition changes and weight-related health conditions on the functional status of older adults. Participants (n=3,075), aged between 70 and 79 years, were recruited between April 1997 through June 1998, from a list of Medicare beneficiaries residing in the areas surrounding Pittsburgh, PA, and Memphis, TN. Eligibility criteria included: 1) No reported difficulty walking ¼ mile, climbing 10 steps, or performing basic activities of daily living, 2) No life-threatening illness, and 3) No plans to permanently leave the area for three years. Participants were contacted by telephone every 6 months and had annual clinic visits during which health status was assessed and data on interim hospitalizations and major outpatient procedures were collected.
The present study is based on 3,024 participants, after exclusion of 51 participants who had missing baseline values on the physical performance measures. All participants provided written informed consent. The Institutional Review Boards of the clinical sites approved the study protocol.
Physical performance measures
Three physical performance measures were considered in this analysis: usual gait speed, repeated chair stands, and standing balance tests. These measures, easy and quick to administer, have shown good reliability in elders6. The SPPB, based on similar tests, has shown to be predictive of adverse health-related outcomes in older persons1.
Usual gait speed
Participants were asked to stand stationary with their feet behind a starting line marked with tape, then, following the examiner’s command of “Go!”, to walk at their usual pace over a 6-meter course and to stop just past the finish line. Timing was started with the first foot fall and stopped when participant’s first foot completely crossed the 6-meter end line. The faster of two trials (in meters/second) was used for the present analyses.
Repeated chair stands
Participants were asked to stand up five times in a row as quickly as possible from a chair without stopping, keeping arms folded across the chest. Participants had to come to a full standing position each time they stood up, and to sit all the way down each time. Timing was started when examiner said “Go!”, and stopped when the participant sat down for the fifth time. Time (in seconds) or inability to perform the test were used for the present analyses.
Standing balance
Participants were asked to stand in the following three increasingly challenging positions for 30 seconds each: 1) semi-tandem stand, in which participants stand with the side of the heel of one foot touching the big toe of the other foot; 2) tandem stand, in which participants stand with the heel of one foot in front of and touching the toes of the other foot; and 3) single-leg stand, in which participants stand on one leg. The test was stopped when the participant could not hold a stand without support after two attempts. The total amount of time each stand was held, ranging from 0 to 90 seconds, was used for the present analyses.
Outcomes
During the study follow-up, participants were contacted by telephone every 6 months and had a clinical visit every year, during which vital/health status was assessed and data about interim hospitalizations or major outpatient procedures were collected. When an overnight hospitalization or major outpatient procedure was reported, hospital records were collected and the event verified by a Health ABC Disease Adjudicator at each site.
For the present analyses, we explored the additive value of physical performance measures in predicting each of the following outcomes:
Persistent lower extremity limitation. Defined as two consecutive semi-annual reports of having any difficulty either walking ¼ mile or climbing up 10 steps without resting;
Persistent severe lower extremity limitation. Defined as two consecutive semi-annual reports of having a lot of difficulty or not being able to walk ¼ mile or to climb up 10 steps without resting;
Death. Date of death taken from the death certificate;
Hospitalization. Any hospitalization in an acute care unit that occurred during the first year of follow-up.
Physical performance measure cut-points
In a previous paper7, we demonstrated that a usual gait speed (over a 6-meter course) slower than 1 m/sec identified older persons at high risk of health-related events. This gait speed cut-point was identified on the basis of the rates of incident persistent lower extremity limitation events in a random subsample of Health ABC participants. The remaining participants were then used to evaluate the predictive value of the identified cut-point for major health-related events. This cut-point was found to consistently predict health-related events across gender and race (Whites, Blacks) groups7. In the present analyses, we used the 1 m/sec cut-point to dichotomize usual gait speed into high and low risk performance. The balance and chair stand tests were dichotomized using the same percentile (21.3%) as the chosen usual gait speed cut-point. By choosing this same threshold to identify individuals at increased risk of health-related events, we determined equal distributions of the three physical performance measures of interest, consequently allowing fair comparisons.
An alternative approach using ROC curves analysis was also considered to categorize the physical performance measures (results available on request). In the ROC curve analysis, the true-positive rate (sensitivity) is plotted against the false-positive rate (1-specificity) across a range of values from a diagnostic test. Cut-points of 1.175 m/sec for usual gait speed, 77.0 sec for balance test, and 14.5 sec for chair stand test were identified by maximizing the sum of sensitivity and specificity derived on the basis of the persistent lower extremity limitation outcome.
Covariates
Covariates included sociodemographic variables (age, sex, race, study site, smoking, alcohol consumption, education), health indicators (Body Mass Index -BMI, defined as body weight divided height squared), Modified Mini-Mental State (3MS) examination score8, and physical activity -calculated using the Harvard Alumni study9 variable based on walking and exercise expenditure in kcal/week), and comorbidity (adjudicated presence of coronary heart disease, congestive heart failure, diabetes, hypertension, osteoarthritis, peripheral artery disease, cerebrovascular disease, depression, and pulmonary disease). The presence of clinical conditions at baseline was ascertained using algorithms mirroring those adopted in the Cardiovascular Health Study10 and based on self-report of physician diagnoses, current medications, and measures obtained in the clinical examination.
Statistical analyses
Unadjusted and adjusted Cox proportional hazards analyses were performed to assess hazard rate ratios (HR) and 95% confidence intervals (95%CI) for incident outcome events according to the defined risk groups for each physical performance measure (low risk groups considered as reference groups). Analyses also considering continuous variables for the physical performance measures, rescaled as previously described11, were also performed. Then, analyses were repeated to evaluate HR (and 95%CI) for incident outcome events according to the number of physical performance measures in the high risk category (participants with no physical performance measure in the high risk group served as the reference group). Analyses were adjusted for age, sex, race and those variables showing a significant (p<0.10) correlation with physical performance measures and/or outcome variables. The proportional hazard assumption was tested for all the variables of interest 1) using log minus log plots (to verify whether they were approximately parallel for all levels of each categorical explanatory variable), and 2) including interaction terms between time and the variables under consideration (to verify the statistical significance) as part of the Cox proportional models.
To evaluate the predictive value of categorized physical performance measures for health-related events, sensitivity, specificity, predictive values and likelihood ratios were also calculated.
For the persistent (severe) lower extremity limitation outcome, days to event were determined from the baseline assessment visit date to the date of the first of two successive reports of difficulty. For those participants who did not develop functional limitation, follow-up time was censored to the last contact or death date. For the mortality outcome, days to event were determined from the baseline assessment visit date to the date of death. For the hospitalization outcome, follow-up time was defined as the time from the baseline visit to the first hospitalization date (for those who had one) or was censored at one year of follow-up or death date if occurred within the first year (for those with no hospitalizations).
RESULTS
Mean age of the sample population (n=3,024) was 73.6 years (SD ± 2.9), 51.6% were women, and 41.2% were Black. Median follow-up duration was 6.9 years. Main sociodemographic characteristics of the sample population are described in Table 1.
Table 1.
Main baseline characteristics of the study participants.
| Mean ± SD, or % (n=3,024) |
|
|---|---|
| Sociodemographics | |
| Age (years) | 73.6 ± 2.9 |
| Sex (Women) | 51.6 |
| Race (White) | 58.8 |
| Site (Memphis) | 50.0 |
| Smoking | |
| Never | 43.8 |
| Former | 46.0 |
| Current | 10.2 |
| Alcohol consumption | |
| Never | 28.1 |
| Former | 22.2 |
| Current | 49.7 |
| Education | |
| Less than High School | 24.9 |
| High School graduate | 32.7 |
| Post-secondary | 42.4 |
| Health indicators | |
| Body Mass Index | 27.4 ± 4.8 |
| Modified Mini Mental State Examination score | 90.1 ± 8.2 |
| Physical activity | |
| 0 kcal/week | 12.8 |
| 1–499 kcal/week | 39.3 |
| 500–999 kcal/week | 17.3 |
| 1000–1499 kcal/week | 10.2 |
| 1500–1999 kcal/week | 5.8 |
| ≥ 2000 kcal/week | 14.7 |
| Clinical conditions | |
| Coronary heart disease | 16.7 |
| Congestive heart failure | 1.3 |
| Diabetes | 14.9 |
| Hypertension | 60.9 |
| Osteoarthritis | 28.4 |
| Peripheral artery disease | 5.2 |
| Cerebrovascular disease | 7.2 |
| Depression | 2.0 |
| Pulmonary disease | 4.1 |
| Physical performance measures | |
| 6-meter walk test (m/sec) | 1.18 ± 0.23 |
| Chair stand test (sec) | 14.28 ± 4.01 |
| Unable to complete the chair stand test | 3.0 |
| Balance test (sec) | 67.61 ± 23.35 |
Physical activity: walking and exercising expenditure (in kcal/week) according to the Harvard Alumni study variable
Spearman’s analyses were performed to evaluate the correlations among the continuous variables of the physical performance measures. Usual gait speed and chair stand tests showed the strongest correlation (r=−0.413; p<0.001). Significant, but weaker correlations were reported between the balance and usual gait speed tests (r=0.310; p<0.001), and between the balance and chair stand tests (r=−0.271; p<0.001).
In the sample population the 1 m/sec cut-point for usual gait speed corresponded to the 21.3 percentile. The same percentile was used to identify the cut-points to categorize chair stand (high risk group: ≥17.1 sec) and standing balance test (high risk group: ≤53.0 sec). Cross-tabulations and unadjusted odds ratios of dichotomous physical performance measures are reported in Table 2.
Table 2.
Cross-sectional relationships (all p values <0.001) between low results at the physical performance tests. Results are expressed as n (%).
| Balance test | ||
|---|---|---|
| Gait speed test | Low risk | High risk |
| ≥ 1 m/sec (low risk) | 1969 (65.1) | 411 (13.6) |
| <1 m/sec (high risk) | 412 (13.6) | 232 (7.7) |
| Unadjusted odds ratio: 2.70 (95%CI 2.23–3.27) |
||
| Gait speed test | ||
| Chair stand test | Low risk | High risk |
| <17 sec (low risk) | 2015 (66.6) | 361 (11.9) |
| ≥ 17 sec (high risk) | 365 (12.1) | 283 (9.4) |
| Unadjusted odds ratio: 4.33 (95%CI 3.57–5.24) |
||
| Chair stand test | ||
| Balance test | Low risk | High risk |
| ≥ 53 sec (low risk) | 1975 (65.3) | 406 (13.4) |
| <53 sec (high risk) | 401 (13.3) | 242 (8.0) |
| Unadjusted odds ratio: 2.94 (95%CI 2.42–3.56) | ||
The predictive values for adverse health-related events using the identified cut-points for each physical performance measure were evaluated (Table 3). Unadjusted and adjusted Cox proportional hazard analyses showed that participants in the high risk group for usual gait speed, repeated chair stands, or standing balance were more likely to experience persistent (severe) lower extremity limitation, death and hospitalization events. The risk estimates for developing adverse health-related events were rather similar across the three physical performance measures evaluated (e.g. persistent lower extremity limitation - high risk group for usual gait speed HR 1.53, 95%CI 1.35–1.74; high risk group for standing balance test HR 1.58, 95%CI 1.40–1.78; high risk group for repeated chair stands test HR 1.59, 95%CI 1.41–1.78; all p values <0.001). The chair stand test was less strongly associated with new hospitalizations than the other two performance measures after adjustment for potential confounders (HR 1.20, 95%CI 0.97–1.49; p=0.09).
Table 3.
Hazard ratios (and 95%CI) and event rate for persistent (severe) functional limitation, mortality and hospitalization according to the physical performance tests results.
| Event rate Events/Participants (Rate of events per 100 participant- years) | Unadjusted HR (95%CI) | p | Adjusted*HR (95%CI) | p | |
|---|---|---|---|---|---|
| Persistent lower extremity limitation | |||||
| Usual gait speed ≥ 1 m/sec (low risk) | 1015/2379 (9.40) | 1 (Reference) | 1 (Reference) | ||
| Usual gait speed < 1 m/sec (high risk) | 468/643 (25.03) | 2.49 (2.23–2.78) | <0.001 | 1.53 (1.35–1.74) | <0.001 |
| Usual gait speed (continuous)† | 0.56 (0.53–0.60) | <0.001 | 0.70 (0.65–0.74) | <0.001 | |
| Balance test ≥ 53 sec (low risk) | 1047/2380 (9.84) | 1 (Reference) | 1 (Reference) | ||
| Balance test < 53 sec (high risk) | 436/642 (21.49) | 2.08 (1.86–2.33) | <0.001 | 1.58 (1.40–1.78) | <0.001 |
| Balance test (continuous)† | 0.70 (0.67–0.73) | <0.001 | 0.79 (0.75–0.83) | <0.001 | |
| Chair stand test <17 sec (low risk) | 1043/2376 (9.80) | 1 (Reference) | 1 (Reference) | ||
| Chair stand test ≥ 17 sec (high risk) | 440/646 (21.69) | 2.10 (1.88–2.35) | <0.001 | 1.59 (1.41–1.78) | <0.001 |
| Chair stand test (continuous)† | 0.66 (0.63–0.70) | <0.001 | 0.76 (0.72–0.80) | <0.001 | |
| Persistent severe lower extremity limitation | |||||
| Usual gait speed ≥ 1 m/sec (low risk) | 452/2379 (3.70) | 1 (Reference) | 1 (Reference) | ||
| Usual gait speed < 1 m/sec (high risk) | 249/643 (9.03) | 2.45 (2.10–2.86) | <0.001 | 1.52 (1.28–1.82) | <0.001 |
| Usual gait speed (continuous)† | 0.57 (0.53–0.62) | <0.001 | 0.73 (0.67–0.80) | <0.001 | |
| Balance test ≥ 53 sec (low risk) | 447/2380 (3.66) | 1 (Reference) | 1 (Reference) | ||
| Balance test < 53 sec (high risk) | 254/642 (9.18) | 2.51 (2.15–2.93) | <0.001 | 1.85 (1.56–2.19) | <0.001 |
| Balance test (continuous)† | 0.66 (0.62–0.71) | <0.001 | 0.75 (0.70–0.81) | <0.001 | |
| Chair stand test <17 sec (low risk) | 464/2376 (3.83) | 1 (Reference) | 1 (Reference) | ||
| Chair stand test ≥ 17 sec (high risk) | 237/646 (8.36) | 2.20 (1.88–2.57) | <0.001 | 1.62 (1.37–1.91) | <0.001 |
| Chair stand test (continuous)† | 0.65 (0.61–0.69) | <0.001 | 0.77 (0.71–0.83) | <0.001 | |
| Death | |||||
| Usual gait speed ≥ 1 m/sec (low risk) | 464/2380 (3.00) | 1 (Reference) | 1 (Reference) | ||
| Usual gait speed < 1 m/sec (high risk) | 189/644 (4.77) | 1.63 (1.37–1.93) | <0.001 | 1.49 (1.23–1.80) | <0.001 |
| Usual gait speed (continuous)† | 0.75 (0.70–0.82) | <0.001 | 0.79 (0.72–0.86) | <0.001 | |
| Balance test ≥ 53 sec (low risk) | 465/2381 (3.01) | 1 (Reference) | 1 (Reference) | ||
| Balance test < 53 sec (high risk) | 188/643 (4.71) | 1.59 (1.34–1.88) | <0.001 | 1.35 (1.12–1.62) | 0.002 |
| Balance test (continuous)† | 0.79 (0.74–0.84) | <0.001 | 0.84 (0.78–0.91) | <0.001 | |
| Chair stand test <17 sec (low risk) | 468/2376 (3.04) | 1 (Reference) | 1 (Reference) | ||
| Chair stand test ≥ 17 sec (high risk) | 185/648 (4.58) | 1.53 (1.29–1.81) | <0.001 | 1.40 (1.17–1.68) | <0.001 |
| Chair stand test (continuous)† | 0.81 (0.75–0.87) | <0.001 | 0.83 (0.77–0.90) | <0.001 | |
| Hospitalization within the first year of follow-up | |||||
| Usual gait speed ≥ 1 m/sec (low risk) | 360/2380 (16.39) | 1 (Reference) | 1 (Reference) | ||
| Usual gait speed < 1 m/sec (high risk) | 131/644 (22.55) | 1.38 (1.13–1.68) | <0.001 | 1.26 (1.00–1.58) | 0.05 |
| Usual gait speed (continuous)† | 0.83 (0.76–0.90) | <0.001 | 0.83 (0.75–0.93) | 0.001 | |
| Balance test ≥ 53 sec (low risk) | 356/2381 (16.17) | 1 (Reference) | 1 (Reference) | ||
| Balance test < 53 sec (high risk) | 135/643 (23.44) | 1.45 (1.19–1.77) | <0.001 | 1.39 (1.12–1.72) | 0.003 |
| Balance test (continuous)† | 0.84 (0.78–0.91) | <0.001 | 0.85 (0.78–0.93) | <0.001 | |
| Chair stand test <17 sec (low risk) | 365/2376 (16.65) | 1 (Reference) | 1 (Reference) | ||
| Chair stand test ≥ 17 sec (high risk) | 126/648 (21.58) | 1.30 (1.06–1.59) | 0.01 | 1.20 (0.97–1.49) | 0.09 |
| Chair stand test (continuous)† | 0.90 (0.83–0.98) | 0.02 | 0.93 (0.85–1.03) | 0.15 | |
Adjusted for age, sex, race, site, smoking, alcohol consumption, education, body mass index, Modified Mini Mental State Examination score, physical activity, coronary heart disease, congestive heart failure, diabetes, hypertension, osteoarthritis, peripheral artery disease, cerebrovascular disease, depression, pulmonary disease
Continuous measures ranging from 0 (worst performance) to 1 (best performance) and then rescaled according to specific standard deviations (usual gait speed 0.128; balance test 0.255; chair stand test 0.164).
Significant race interactions (both p values for interaction terms <0.01) were found for the relationship between number of high risk physical performance measures and onset of mobility limitation outcomes. The hazard ratios associated with number of high physical performance measures were highly significant in both race groups (p values for trend <0.001), but lower in Blacks (e.g. persistent lower extremity limitation - one physical performance measure: HR 1.32, 95%CI 1.09–1.59; two physical performance measures: HR 1.66, 95%CI 1.33–2.07; three physical performance measures: HR 2.18, 95%CI 1.67–2.85) compared to Whites (one physical performance measure: HR 1.81, 95%CI 1.52–2.14; two physical performance measures: HR 2.56, 95%CI 2.02–3.24; three physical performance measures: HR 3.92, 95%CI 2.60–5.92). No race interaction was detected for the other outcomes. No significant sex interaction was found between number of high risk physical performance tests and onset of any outcome evaluated.
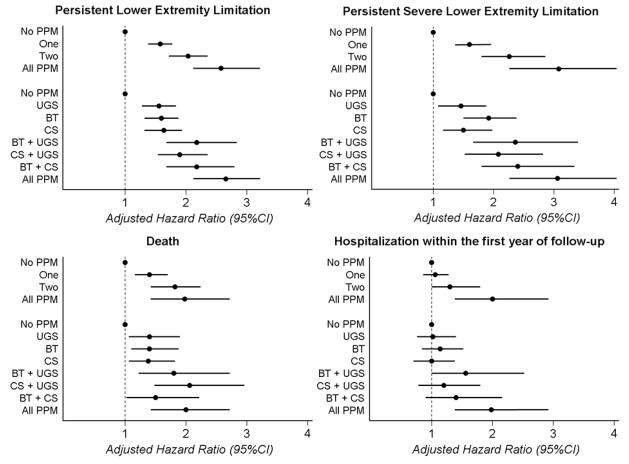
The added value of each additional physical performance measure to the prediction of adverse health-related events was also investigated using Cox proportional hazard models (Figure 1). For each outcome there was a monotonic increase in the event rate with an increasing number of functional criteria. Any single criterion was associated with a significantly higher risk of all outcomes except for hospitalization. In this case, two or more criteria predicted a new hospitalization in the following year.
Figure 1.
Adjusted* hazard ratios (and 95%CI) for persistent (severe) functional limitation, hospitalization and mortality according to the physical performance measures (PPM; usual gait speed [UGS], balance test [BT] and chair stands [CS] test) in the high risk group.
* Adjusted for age, gender, race, site, smoking, alcohol consumption, education, body mass index, Modified Mini Mental State Examination score, physical activity, coronary heart disease, congestive heart failure, diabetes, hypertension, osteoarthritis, peripheral artery disease, cerebrovascular disease, depression, pulmonary disease
In Table 4 (and Supplemental Table), we also presented sensitivity, specificity, predictive values and likelihood ratios for different combinations of physical performance measures at high risk for health-related events. Each single measure of physical performance was characterized by a high specificity (higher than 80%) and low sensitivity (lower than 30%).
Table 4.
Specificity, sensitivity, positive predictive value, and likelihood ratios for persistent (severe) functional limitation, mortality and hospitalization according to the physical performance measures (PPM; usual gait speed [UGS], balance test [BT] and chair stands [CS] test) in the high risk group.
| PPM in the high risk group | Event rate n/N (*) | Sensitivity | Specificity | Positive predictive value | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|---|---|
| Persistent lower extremity limitation | ||||||
| No PPM | 625/1707 (7.53) | Reference | Reference | Reference | Reference | Reference |
| UGS | 170/268 (18.46) | 0.21 | 0.92 | 0.63 | 2.57 | 0.86 |
| BT | 175/308 (14.73) | 0.22 | 0.89 | 0.57 | 2.00 | 0.88 |
| CS | 145/261 (14.54) | 0.19 | 0.90 | 0.56 | 1.94 | 0.90 |
| BT + UGS | 73/93 (31.74) | 0.10 | 0.98 | 0.78 | 5.76 | 0.91 |
| CS + UGS | 107/144 (25.36) | 0.15 | 0.97 | 0.74 | 4.42 | 0.88 |
| BT + CS | 70/103 (22.29) | 0.10 | 0.97 | 0.68 | 3.40 | 0.93 |
| All PPM | 118/138 (39.86) | 0.16 | 0.98 | 0.86 | 8.75 | 0.86 |
| Persistent severe lower extremity limitation | ||||||
| No PPM | 256/1707 (2.83) | Reference | Reference | Reference | Reference | Reference |
| UGS | 76/268 (5.94) | 0.23 | 0.88 | 0.28 | 1.96 | 0.87 |
| BT | 91/308 (6.22) | 0.26 | 0.87 | 0.30 | 2.02 | 0.85 |
| CS | 62/261 (4.85) | 0.20 | 0.88 | 0.24 | 1.62 | 0.92 |
| BT + UGS | 41/93 (11.36) | 0.14 | 0.97 | 0.44 | 3.99 | 0.89 |
| CS + UGS | 53/144 (8.60) | 0.17 | 0.94 | 0.37 | 2.91 | 0.88 |
| BT + CS | 43/103 (9.75) | 0.14 | 0.96 | 0.42 | 3.62 | 0.89 |
| All PPM | 79/138 (15.77) | 0.24 | 0.96 | 0.57 | 6.04 | 0.80 |
| Death | ||||||
| No PPM | 296/1707 (2.65) | Reference | Reference | Reference | Reference | Reference |
| UGS | 65/268 (3.79) | 0.18 | 0.87 | 0.24 | 1.43 | 0.94 |
| BT | 77/308 (3.89) | 0.21 | 0.86 | 0.25 | 1.47 | 0.92 |
| CS | 61/262 (3.63) | 0.17 | 0.88 | 0.23 | 1.37 | 0.95 |
| BT + UGS | 30/93 (5.54) | 0.09 | 0.96 | 0.32 | 2.15 | 0.95 |
| CS + UGS | 43/144 (4.85) | 0.13 | 0.93 | 0.30 | 1.90 | 0.94 |
| BT + CS | 30/103 (4.60) | 0.09 | 0.95 | 0.29 | 1.87 | 0.96 |
| All PPM | 51/139 (6.20) | 0.15 | 0.94 | 0.37 | 2.50 | 0.91 |
| Hospitalization within the first year of follow-up | ||||||
| No PPM | 250/1707 (15.83) | Reference | Reference | Reference | Reference | Reference |
| UGS | 42/268 (16.87) | 0.14 | 0.87 | 0.16 | 1.07 | 0.90 |
| BT | 49/308 (17.38) | 0.16 | 0.85 | 0.16 | 1.09 | 0.98 |
| CS | 39/262 (16.18) | 0.13 | 0.87 | 0.15 | 1.02 | 0.99 |
| BT + UGS | 24/93 (29.27) | 0.09 | 0.95 | 0.26 | 1.94 | 0.96 |
| CS + UGS | 25/144 (19.08) | 0.09 | 0.92 | 0.17 | 1.20 | 0.98 |
| BT + CS | 22/103 (23.66) | 0.08 | 0.95 | 0.21 | 1.54 | 0.97 |
| All PPM | 40/139 (33.90) | 0.14 | 0.94 | 0.29 | 2.17 | 0.92 |
Rate of events per 100 participant-years; n/N=number of events/number of participants
When analyses were repeated considering physical performance measures categorized according to cut-points derived from ROC curves analysis, similar findings were obtained (data available on request). However, in this alternative approach, the predictive value of the chair stand test was consistently lower than the other physical performance measures.
DISCUSSION
To our knowledge, this is the first study to systematically evaluate the added value of using up to three dichotomized physical performance measures in the prediction of several adverse health-related events. The present analyses were specifically aimed at evaluating whether differences in the predictive value for events were present among the three components of the SPPB (i.e. timed usual gait speed, repeated chair stands and standing balance). Our findings demonstrate that poor performance on any one of these three commonly administered performance tests present similar predictive values for major events, although slow usual gait speed and balance test showed the most consistent results. When the three physical performance measures were considered together, a direct association between the number of impaired tests and risk of events was reported. However, having only a single physical performance measure at high risk was significantly and strongly associated with risk of persistent (severe) lower extremity limitation and mortality outcomes. When all three measures were considered together, a significant prediction of hospitalization events could only be reached when all tests showed poor results. No combination of physical performance tests was clearly superior in the prediction of events, and different results were reported for different outcomes. Interestingly, each single physical performance test was characterized by a high specificity for all the study outcomes. This finding clearly confirm the importance of all these measures in the screening process of older persons by 1) correctly identifying negative cases, and 2) consequently avoiding further (and sometime burdensome) investigations in low risk individuals.
It has been suggested that timed gait alone predicts disability nearly as well as the full SPPB3 when the physical performance measures are considered as continuous variables, a rare practice in a clinical setting. Whether this observation would hold when performances on tests were examined as dichotomous variables as it is frequently done in clinical settings with most biological markers, was unknown. The present analyses evaluated the added value of physical performance measures for the prediction of health-related events after categorization into high and low risk groups. Our findings showed that timed usual gait speed, standing balance and repeated chair stand tests have similar utility in identifying subjects who will develop events.
However, the combination of the three measures leads to only a marginal gain in the prediction of physical disability and mortality outcomes. These results confirm that the timed usual gait speed (but also the balance and chair stand tests) is almost as good as the complete SPPB in identifying older persons at risk of physical disability events3. Therefore, even though gait speed is considered the most important predictor of several adverse health events, these findings demonstrate that poor performance on other tests of lower extremity function are equally prognostic. Therefore, chair stand and standing balance performance may be adequate substitutes when gait speed is unavailable. This is particularly valuable and applicable to studies that do not or can not include gait testing due to lack of space.
Our findings from Cox proportional hazard models show that single measures of physical performance are less predictive of hospitalization events compared to physical disability and mortality outcomes, though the simultaneous evaluation of all three physical performance tests does provide significant risk prediction. This finding may be explained in two different ways. First, physical performance measures were originally developed with physical disability as the “gold standard” outcome. Therefore, the stronger association with incident physical disability (and mortality as correlate of overall health status) compared to hospitalization is not unexpected. Second, even if our hospitalization outcome was defined on the basis of overnight hospital stays, it is likely to be an heterogenous outcome, composed of severe as well as mild clinical cases, and clinical events that might not be function related (e.g. plastic surgery).
Despite strong evidence that physical performance measures play an important role in the evaluation of older persons, their clinical use is still very limited12;13. Several problems may inhibit wider usage. Some physical performance measures are time consuming and need special equipment and/or training. This study explored three physical performance tests that are quick and easy to perform and do not require special equipment or training. A second major issue limiting clinical use of physical performance measures concerns the hard to remember and often population-based cut-points currently available in literature2;14–19. Previously7, we identified a cut-point for the 6-meter walking speed (1 m/sec) for a study sample aged 70–79 years based on subsequent risk of functional limitation. The delineation of an easy to remember cut-point for gait speed will hopefully encourage systematic assessment of gait speed in older persons. In the present study, we dichotomized performance on the balance and chair stand tests on the basis of the population-percentile corresponding to the newly established usual gait speed cut-point, to allow a fair comparison across the different tests.
Using this approach7, we found that inability to complete the chair stand test within 17 seconds identified participants at high risk of functional limitation. This cut-point is very similar to those suggested by previous papers in which 16.320, 16.521, or 16.72;3;6 seconds cut-points were used to identify participants scoring one point (on a scale ranging from 0 to 4, whereas higher result is indicative of better performance) in the SPPB score.
The standing balance test in the SPPB consists of three 10-second long tasks: the side-by-side, the semi-tandem, and the full tandem position2. The 30 seconds that participants were asked to hold each progressively more difficult stand and the final one-leg stand evaluation make the version used here more challenging for older persons. The original balance test is a relatively easy task of physical performance and it is often successfully completed by a high percentage of older persons22. The cut-point we identified approximately corresponds to the inability to hold a one-leg stand. Thus, it might be easy to remember and may facilitate the implementation of this measure. This means that, instead of the three tasks evaluating the standing balance, it may be sufficient only to ask the subject attempt only the one-leg stand to identify persons at high risk of adverse health-related events.
All cut-points identified have been shown to predict several adverse health-related events, such as (severe) mobility limitation, hospitalization, and death. These findings confirm results from previous studies1;15;23 and strengthen the recommendation to consider these measures as indicators of age-related body changes and/or markers of (sub)clinical disease.
In our analyses we found significant race interactions in the relationships between number of high risk physical performance tests and onset of persistent (severe) lower extremity limitation. Interestingly, these race differences were observed for the mobility limitation outcomes, only. These findings, consistent with a previous study7, may suggest that the relationship between the SPPB and onset of mobility limitation is more affected by the presence of potential confounders compared to the mortality and hospitalization outcomes. The use of additional measures may be particularly desirable in Black older adults to obtain a better evaluation of risk of mobility disability events.
The Health ABC population consists of well-functioning non-disabled persons, aged 70 to 79 years. Thus, the cut-points identified for usual gait speed, chair stands, and standing balance tests likely represent normative values. These values may also serve as targets for interventions aimed toward improving physical performance and provide useful parameters to evaluate intervention efficacy in reducing risk of health-related events. Most studies evaluating change over time in functional performance have only described improvements in physical performance16;24–26, and not whether meaningful thresholds have been obtained. It is also noteworthy that our results may be useful for evaluating older persons in which a disabling process is not yet clinically evident, providing basis for the development of a “real” preventive program.
Some limitations of the present study should be mentioned. Although a loss of information may occur when continuous variables are dichotomized, the provision of cut-points is essential for promoting the use of physical performance measures for the screening and evaluation of older persons. The three components of the SPPB administered to the Health ABC study participants were slightly modified from the original version1 to provide more challenging tests to a well-functioning and selected older population. It might be argued that these modifications may limit the applicability of the present results to the original version of the SPPB. However, given the similar nature of the Health ABC subtasks compared to the original ones, we believe that this potential issue may not significantly limit the export of our results. Further studies should expand our findings to different age groups and evaluate whether interventions aimed at improving physical performance measures24–26 are able to prevent adverse health-related outcomes. Our choice to define the cut-points for the considered physical performance measures on the basis of a previously validated cut-point7 and the population distribution might be arguable. However, alternative analyses (available on request) using cut-points based on specificity and sensitivity of the physical performance measures for predicting persistent lower extremity limitation were performed and led to similar results.
In conclusion, our findings demonstrate that dichotomized physical performance measures (i.e. usual gait speed, chair stand, and balance tests), which may facilitate use of these measures in clinical practice, provide similar predictive values for adverse health-related events when considered separately. Participants with poor results for all three measures had a higher risk of incident functional limitation, hospitalization and death compared to those with normal values on all of them. Estimating risk for incident physical disability and mortality may not require administration of all three physical performance tests, since a single measure provides significant prediction. However, the predictive value does increase with an increasing number of tests. The value of this increasing predictive ability may be offset by increasing the complexity of administering and interpreting multiple tests in a clinical setting.
Supplementary Material
Acknowledgments
This work was supported by the National Institute on Aging (contract numbers N01-AG-6-2106, N01-AG-6-2101, and N01-AG-6-2103), and by the University of Florida Institute on Aging and the Claude D. Pepper Older Americans Independence Center (NIH grant 1P30AG028740). This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging.
Footnotes
AUTHORS CONTRIBUTIONS
Matteo Cesari: study concept and design; analysis and interpretation of data; preparation of manuscript.
Stephen B Kritchevsky: study concept and design; acquisition of subjects and data; analysis and interpretation of data; preparation of manuscript.
Anne B Newman: study concept and design; acquisition of subjects and data; interpretation of data; preparation of the manuscript.
Eleanor M Simonsick: acquisition of subjects and data; critical review of the manuscript; preparation of the manuscript.
Tamara B Harris: acquisition of subjects and data; interpretation of data; critical review of the manuscript.
Brenda W Penninx: study concept and design; critical review of the manuscript.
Jennifer S Brach: acquisition of subjects and data; critical review of the manuscript.
Frances A Tylavsky: interpretation of data; critical review of the manuscript.
Suzanne Satterfield: acquisition of subjects and data; critical review of the manuscript.
Doug C Bauer: acquisition of subjects and data; critical review of the manuscript.
Susan M Rubin: acquisition of subjects and data; critical review of the manuscript.
Marjolein Visser: interpretation of data, critical review of the manuscript.
Marco Pahor: study concept and design; analysis and interpretation of data; critical review of the manuscript; preparation of manuscript.
References
- 1.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J Gerontol A Biol Sci Med Sci. 2000;55A:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cesari M, Penninx BWJH, Pahor M, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004;59A:M242–M248. doi: 10.1093/gerona/59.3.m242. [DOI] [PubMed] [Google Scholar]
- 5.Hicks GE, Simonsick EM, Harris TB, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the Health, Aging and Body Composition study. J Gerontol A Biol Sci Med Sci. 2005;60:882–887. doi: 10.1093/gerona/60.7.882. [DOI] [PubMed] [Google Scholar]
- 6.Ostir GV, Volpato S, Fried LP, et al. Reliability and sensitivity to change assessed for a summary measure of lower body function - Results from the Women’s Health and Aging Study. J Clin Epidemiol. 2002;55:916–921. doi: 10.1016/s0895-4356(02)00436-5. [DOI] [PubMed] [Google Scholar]
- 7.Cesari M, Kritchevsky SB, Penninx BWJH, et al. Prognostic value of usual gait speed in well-functioning elders - Results from the Health, Aging and Body Composition (Health ABC) study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 8.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 9.Washburn RA, Smith KW, Goldfield SRW, et al. Reliability and physiologic correlates of the Harvard Alumni Activity Survey in a general population. J Clin Epidemiol. 1991;44:1319–1326. doi: 10.1016/0895-4356(91)90093-o. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 11.Cesari M, Pahor M, Bartali B, et al. Antioxidants and physical performance in elderly persons: the Invecchiare in Chianti (InCHIANTI) study. Am J Clin Nutr. 2004;79:289–294. doi: 10.1093/ajcn/79.2.289. [DOI] [PubMed] [Google Scholar]
- 12.Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 13.Guralnik JM, Branch LG, Cummings SR, et al. Physical performance measures in aging research. J Gerontol. 1989;44:M141–M146. doi: 10.1093/geronj/44.5.m141. [DOI] [PubMed] [Google Scholar]
- 14.Rantanen T, Guralnik JM, Ferrucci L, et al. Compairments as predictors of severe walking disability in older women. J Am Geriatr Soc. 2001;49:21–27. doi: 10.1046/j.1532-5415.2001.49005.x. [DOI] [PubMed] [Google Scholar]
- 15.Markides KS, Black SA, Ostir GV, et al. Lower body function and mortality in Mexican American elderly people. J Gerontol A Biol Sci Med Sci. 2001;56A:M243–M247. doi: 10.1093/gerona/56.4.m243. [DOI] [PubMed] [Google Scholar]
- 16.Onder G, Penninx BWJH, Lapuerta P, et al. Change in physical performance over time in older women: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 2002;57A:M289–M293. doi: 10.1093/gerona/57.5.m289. [DOI] [PubMed] [Google Scholar]
- 17.Shinkai S, Watanabe S, Kumagai S, et al. Walking speed as a good predictor for the onset of functional dependenca in a Japanese rural community population. Age Aging. 2000;29:441–446. doi: 10.1093/ageing/29.5.441. [DOI] [PubMed] [Google Scholar]
- 18.Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: the role of physical performance. J Am Geriatr Soc. 1995;43:603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- 19.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 20.Melzer D, Lan TY, Guralnik JM. The predictive validity for mortality of the index of mobility-related limitation. Results from the EPESE study. Age Ageing. 2003;32:619–625. doi: 10.1093/ageing/afg107. [DOI] [PubMed] [Google Scholar]
- 21.Ostir GV, Markides KS, Black SA, et al. Lower body functioning as a predictor of subsequent disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 1998;53:M491–M495. doi: 10.1093/gerona/53a.6.m491. [DOI] [PubMed] [Google Scholar]
- 22.Cesari M, Onder G, Russo A, et al. Comorbidity and physical function - Results from the ilSIRENTE study. Gerontology. 2005;52:24–32. doi: 10.1159/000089822. [DOI] [PubMed] [Google Scholar]
- 23.Woo J, Ho SC, Yu ALM. Walking speed and stride length predicts 36 months dependency, mortality, and institutionalization in Chinese aged 70 and older. J Am Geriatr Soc. 1999;47:1257–1260. doi: 10.1111/j.1532-5415.1999.tb05209.x. [DOI] [PubMed] [Google Scholar]
- 24.Fiatarone MA, O’Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330:1769–1775. doi: 10.1056/NEJM199406233302501. [DOI] [PubMed] [Google Scholar]
- 25.Fiatarone MA, Marks EC, Ryan ND, et al. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263:3029–3034. [PubMed] [Google Scholar]
- 26.Chandler JM, Duncan PW, Kochersberger G, et al. Is lower extremity strength gain associated with improvements in physical performance and disability in frail, community-dwelling elders? Arch Phys Med Rehabil. 1998;79:24–30. doi: 10.1016/s0003-9993(98)90202-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.