Abstract
Objective
Classification of menopausal status often relies on self-report and is centrally important to research and clinical practice. This study was designed to assess the validity of self-reported hysterectomy and oophorectomy.
Design
A validation study of self-reported surgical menopause was conducted using survey data and electronic medical records from women enrolled in the Breast Cancer Screening Program within an integrated group practice in Washington State. Sensitivity of self-reported surgical history was estimated from questionnaire data among women with a history of hysterectomy (N = 1,935) and/or oophorectomy (N = 1,010) per medical records. Positive predictive values were quantified by reviewing medical records for a subset of women who self-reported a hysterectomy and/or oophorectomy (N = 122).
Results
Women self-reported hysterectomy history with great accuracy (sensitivity = 91%, positive predictive value = 97%), but were less accurate in reporting oophorectomy history (sensitivity of bilateral oophorectomy = 64%, positive predictive value = 100% and 73% for bilateral and unilateral oophorectomy, respectively). Among women self-reporting a unilateral oophorectomy, 19% had had both ovaries removed.
Conclusion
Self-report is a valid data collection tool for hysterectomy history, but care should be taken in querying for and interpreting self-reported oophorectomy history for determining menopausal status.
Keywords: hysterectomy, menopause, oophorectomy, sensitivity, validity, positive predictive value
INTRODUCTION
Biologically, menopause is defined as the permanent cessation of ovulation, marked by the end of menstruation.1,2 Classification of women as premenopausal or postmenopausal, and the identification of the age at which a woman underwent menopause, are centrally important to many epidemiologic studies, because risk factors for disease may vary with menopausal status.3-6 The menopausal transition is a gradual and dynamic process, differing in duration, timing, and symptomatology between women.1,2 Classification of menopausal status can, therefore, be rather complicated in epidemiologic studies and in clinical practice, not only because of the gradual transition, but also because many women have a hysterectomy without an oophorectomy, making it difficult to know when women transition through menopause because of the absence of menstrual bleeding.7
There exists a great deal of variation between epidemiologic studies with respect to classifying menopausal status and the detail of information collected on which such classification is based. One common challenge arises in the population of women with a surgically-induced menopause, particularly women who experienced cessation of menses at the time of a simple hysterectomy (i.e., without bilateral oophorectomy). Epidemiologic studies wishing to classify the menopausal status of women with a history of hysterectomy and / or oophorectomy commonly take an approach of grouping together all such women as ‘surgically postmenopausal’8 or, alternatively, consider all women with a prior bilateral oophorectomy to be postmenopausal and consider women with a prior hysterectomy (without bilateral oophorectomy) to be postmenopausal only if they have attained a particular age or have initiated use of hormone replacement therapy.9 Classification of menopausal status based on this information is dependent on the ability of women to accurately report their surgical history, and the ability of study questionnaires to accurately capture such information.
Prior studies have implicated the use of self-reported bleeding history and timing surrounding the natural menopausal transition as a potential source of differential misclassification10 and recall bias.11 Reliance on self-reported surgical history may further introduce bias to menopausal status classification if women are unable to accurately self-report their surgical history. Few prior studies have attempted to assess the accuracy of self-report of surgical menopause, but have been limited to the validation of recent surgical menopause.12-14
In this study, we assess the validity of self-reported hysterectomy and oophorectomy through comparison of medical records and self-reported surgical histories. Through medical record review and linkage of surgical records with breast cancer screening questionnaires, we estimate the sensitivity and positive predictive value (PPV) of self-reported hysterectomy and oophorectomy history.
METHODS
The present study uses data from questionnaires completed by women enrolled in the Breast Cancer Screening Program within Group Health’s integrated group practice, based in western Washington State.15 Women who receive a screening or diagnostic mammogram at any Group Health facility are asked to complete a brief questionnaire, including questions on known breast cancer risk factors such as reproductive history and family history. The questionnaire also inquires about the timing of a woman’s last menstrual period and, among women no longer experiencing menstrual cycles, the reason for and timing of cessation of menses.16 Specifically, all women who report that their menstrual periods have stopped are asked to specify why their menstrual periods stopped, with a number of ordered options provided (Figure 1). Electronic medical records are available for all Group Health enrollees and include information on prior surgeries performed at Group Health facilities, as well as some historical information regarding procedures performed before Group Health enrollment and self-reported medical history.
FIGURE 1.
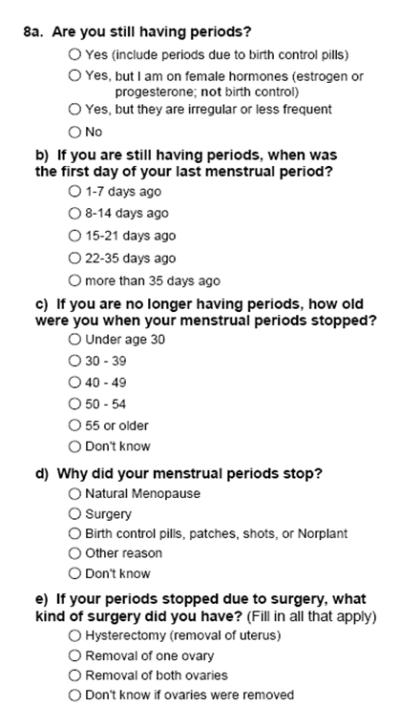
Questionnaire items for the determination of self-reported menopausal status in the Breast Cancer Risk Factor Questionnaire16
We undertook two different examinations using these data to assess: 1) the sensitivity of self-reported surgical history by reviewing the questionnaire responses of women with a surgical history identified from electronic procedure codes, and 2) the positive predictive value of self-reported surgical history by reviewing the medical records of women who self-reported a surgical menopause. Analyses presented here are restricted to women who underwent surgical menopause prior to age 50.
Sensitivity of self-report
Using electronic outpatient procedures data as well as Current Protocol Terminology (CPT) (00846, 00944, 01962-3, 56308, 58150, 58152, 58180, 58200, 58210, 58260, 58275, 58280, 58550, 58942) and International Classification of Disease 9th Revision (ICD-9) inpatient procedure codes (65.6, 68.3-68.7, 68.9) from Group Health medical records, we generated a list of Group Health members who had received a hysterectomy and/or bilateral oophorectomy between 1996-2003 at an age less than 50 years. This list was linked to records of women who had completed a breast cancer screening questionnaire to identify women who had completed a questionnaire following their surgery. We identified 1,996 women with a hysterectomy and/or bilateral oophorectomy before age 50 who had subsequently completed one or more questionnaire. Overall, records for 1,935 hysterectomies and 1,010 bilateral oophorectomies were linked to completed questionnaires. A total of 949 (48%) women had undergone both surgeries, 986 (49%) women had undergone hysterectomy alone, and 61 (3%) had undergone bilateral oophorectomy alone.
We estimated the sensitivity of self-reported hysterectomy and bilateral oophorectomy history as the proportion of women with a documented surgery who, on subsequent screening questionnaires, self-reported surgery as a reason why their menstrual periods had stopped. Sensitivity was calculated in three ways: 1) based on the most recently completed questionnaire, 2) based on the first questionnaire completed after the documented surgery, and 3) based on the set of questionnaires completed at least five years after surgery, with one questionnaire randomly selected from each individual who had completed more than one questionnaire in that time frame.
Sensitivity of self-reported unilateral oophorectomy was not assessed because few women underwent this surgery in the Group Health system over the study period and because unilateral oophorectomy itself would not be expected to cause the cessation of menstrual periods.
Positive predictive value (PPV) of self-report
Based on questionnaire data from women receiving mammograms at Group Health in 2005, we identified a total of 9,770 women who self-reported a surgical menopause prior to age 60. We used stratified random sampling to select 200 women for medical record review, stratifying on the type of surgery reported to identify a study sample with equal number of women reporting surgical menopause attributable to different combinations of hysterectomy and oophorectomy history. The women included in this random sample were not significantly different from the overall population of women self-reporting a surgical menopause with respect to age at the time of survey or self-reported age at menopause. The analysis presented here was restricted to the subset of this abstracted population with a self-reported surgical menopause occurring prior to age 50 (N=122, 61%), including: 22 women with a hysterectomy alone, 18 women with a hysterectomy and one ovary removed, 22 women with a hysterectomy and both ovaries removed, 17 women with a hysterectomy and unknown oophorectomy status, 13 women with a unilateral oophorectomy only, 17 women with a bilateral oophorectomy only, and 13 women with menopause attributed to another or unspecified surgery.
We reviewed electronic medical records for information to confirm or refute self-reported surgical history, starting with surgical and pathology reports from menopausal surgeries (available for 13% of women). In the absence of surgical or pathology reports, we attempted to locate information from transcribed results of pelvic imaging and pelvic physical exams indicating the presence or absence of the uterus and ovaries (37%). If no information was available from these sources, we attempted to locate information in transcribed medical histories (43%), understanding that medical histories were likely to be self-reported. In the absence of information from all of these sources, surgical history was recorded as indeterminable from the medical records (9%). When available, we recorded the date of reported surgeries.
Based on self-report and information extracted from medical records, we calculated the PPV of self-reported hysterectomy, unilateral oophorectomy, and bilateral oophorectomy, excluding women whose surgical history was indeterminable from medical records. We conducted sensitivity analyses to assess the impact of various assumptions on PPV estimates, re-calculating the PPV under different scenarios: 1) excluding women with information from transcribed medical histories only, 2) assuming all women with missing information had no surgical history, and 3) assuming all women with missing information had correctly self-reported their surgical history.
RESULTS
Sensitivity of self-report
Sensitivity estimates were substantially higher for hysterectomy (91%) than bilateral oophorectomy (64%) (Table 1). The sensitivity of self-reported hysterectomy was similar regardless of whether women underwent a bilateral oophorectomy (Table 2). However, the sensitivity of self-reported bilateral oophorectomy was higher among women who had also undergone a hysterectomy compared to women who had undergone an oophorectomy alone (65% versus 49%). Among women who underwent both procedures before age 50, 59% reported both surgeries as reasons why their periods stopped, 31% reported only their hysterectomy, 3% reported only their bilateral oophorectomy, and 7% reported neither surgery as the reason for the cessation of menses. Approximately 62% of women who had undergone a bilateral oophorectomy without hysterectomy over the study period reported that their menstrual periods had ceased subsequent to a hysterectomy, the majority of whom also self-reported a bilateral oophorectomy. Only 23 (1%) of women who had undergone a hysterectomy and 13 (1%) of women who had undergone bilateral oophorectomy reported a natural menopause. Sensitivity estimates for both hysterectomy and bilateral oophorectomy were substantially lower among women who underwent these surgeries between ages 50-59 years (67% and 43%, respectively). No appreciable differences were observed between sensitivity estimates based on questionnaires completed at least five years following surgery and estimates based on the first questionnaire completed after surgery.
TABLE 1.
Sensitivity of self-reported surgical menopause among women with a prior hysterectomy and/or oophorectomy performed between 1996-2003, western Washington State, USA*
| Known Surgery* | ||
|---|---|---|
| Hysterectomy (N = 1,935) |
Bilateral Oophorectomy (N = 1,010) |
|
| Self-report of surgery† | ||
| Yes | 1,757 | 645 |
| No | 127 | 350 |
| Don’t Know / Missing | 51 | 15 |
| Surgery-specific sensitivity | 91% | 64% |
Documented surgical history from procedure codes in electronic medical records taken as the gold standard for comparison.
Self-report taken from most recently completed breast cancer risk factor questionnaire in or before 2005.
TABLE 2.
Self-reported reasons for cessation of menses among women with a known surgical history, western Washington State, USA, 2005*†‡
| Known Surgical History* |
|||
|---|---|---|---|
| Hysterectomy only N (%) |
Bilateral oophorectomy only N (%) |
Hysterectomy + bilateral oophorectomy N (%) |
|
| Self-Report | |||
| Still menstruating | 21 (2) | 2 (3) | 1 (0.1) |
| Natural menopause | 10 (1) | 0 (0) | 13 (1) |
| Hysterectomy | 887 (90) | 38 (62) | 870 (92) |
| Removal of 1 ovary | 100 (10) | 7 (11) | 17 (2) |
| Removal of 2 ovaries | 81 (8) | 30 (49) | 615 (65) |
| Other reason | 16 (2) | 1 (2) | 14 (1) |
| Don’t know | 1 (0.1) | 0 (0) | 3 (0.3) |
Known surgical history derived from procedure codes in electronic medical records.
Numbers do not sum to total and columns %’s sum to >100% due to allow ance for multiple responses perperson.
Based on responses from most recently completed breast cancer risk factor questionnaire during or prior to 2005.
Positive predictive value (PPV) of self-report
Information in medical records pertaining to history of menopausal surgeries was sparse (Table 3): surgical / pathology reports could be located for only 10% of self-reported hysterectomies and 19% of reported oophorectomies (unilateral and bilateral). In 6% of women who self-reported a hysterectomy there was no mention in medical records as to the presence or absence of a uterus; there was no mention as to the presence or absence of ovaries in 21% of women who self-reported an oophorectomy. When it was possible to locate information in medical records relevant to a woman’s surgical history, that information was almost always in agreement with self-reported surgical history. The PPVs for self-report of hysterectomy and oophorectomy were high, ranging from 73-100% (Table 4).
TABLE 3.
Sources of information* for verification of self-reported surgical history among women reporting prior hysterectomy and/or oophorectomy, western Washington State, USA, 2005
| Information Source from Medical Records* | |||||
|---|---|---|---|---|---|
| Total Sample N |
Surgical / pathology report N (%) |
Transcribed notes — pelvic imaging / pelvic exam N (%) |
Transcribed medical history N (% ) |
No information in record N (%) |
|
| Self-Reported Surgery | |||||
| Hysterectomy | 79 | 8 (10) | 28 (35) | 38 (48) | 5 (6) |
| Bilateral oophorectomy | 39 | 8 (21) | 9 (23) | 12 (31) | 10 (26) |
| Unilateral oophorectomy | 31 | 5 (16) | 7 (23) | 14 (45) | 5 (16) |
Sources are mutually exclusive and hierarchical with surgical/pathology report as the first level of evidence, followed by transcribed notes from pelvic imaging/exam, and medical history.
TABLE 4.
Positive predictive value (PPV) of self-reported hysterectomy and oophorectomy by reported type, western Washington State, USA , 2005
| Results of Medical Record Review | ||||||
|---|---|---|---|---|---|---|
| Agreement* N |
Disagreement† N |
Indeterminable‡ N |
Total | PPV (Range)§ | PPV (Range)# | |
| Self-Reported Surgery | ||||||
| Hysterectomy | 72 | 2 | 5 | 79 | 97.3% (91.1, 97.5 ) | 94.0% (82.9,95.1) |
| Bilateral oophorectomy | 29 | 0 | 10 | 39 | 100.0 % (74.4,100.0 ) | 100.0 % (63.0,100.0) |
| Unilateral oophorectomy | 19 | 7 | 5 | 31 | 73.1% (61.3,83.9) | 75.0%(53.9,82.4) |
Agreement indicates that confirmation of self-report was located in at least one information source.
Disagreement indicates that information located in medical records contradicted self-reported surgical history.
Indeterminable indicates that no information to either support or refute self-report could be located inmedical records.
PPV calculation excludes women with “indeterminable” results. PPV range indicates the range of values possible had disagreement (lower bound) or agreement (upper bound) been observed for all women with “indeterminable” results.
PPV calculation excludes women with “indeterminable” results and those with information from only transcribed medical histories. PPV range indicates the range of values possible had disagreement (lower bound) or agreement (upper bound) been observed for all women with “indeterminable” results.
The PPV for a self-report of hysterectomy was high regardless of how missing data were treated (97%). The PPV for self-reported oophorectomy was also high, but differed according to the number of ovaries reportedly removed (100% for bilateral and 73% for unilateral). Information contrary to self-report was located in medical records for 2 women who self-reported a hysterectomy and 7 women who reported a unilateral oophorectomy (1 whose records indicated that both ovaries were still intact and 6 whose records indicated that both ovaries had been surgically removed). There was good agreement between the self-reported timing of cessation of menses and surgery data recorded in medical records, and estimates did not vary markedly according to whether women reported surgical menopause less than 15 years or at least 15 years prior to completing the questionnaire (results not shown). Estimated PPVs changed only marginally when women with validation from transcribed medical histories were excluded (Table 4). PPV estimates were not impacted by including data from women aged 50-59 at the time of menopause included in the original abstracted dataset (results not shown).
DISCUSSION
Our results suggest that the sensitivity and PPV of self-reported history of hysterectomy are high, implying that self-report is a valid means of collecting hysterectomy history. Approximately 91% of women who underwent a hysterectomy at an age less than 50 years reported that surgery as a reason why their menstrual periods had ceased on subsequent screening questionnaires; only 3% of women who self-reported a hysterectomy on their questionnaire had information in their medical records to suggest the continued presence of an intact uterus. We found no difference in the sensitivity of self-reported hysterectomy by history of bilateral oophorectomy, and no evidence to suggest that PPV or sensitivity of hysterectomy varied with time in the five to nine years following surgery.
With respect to bilateral oophorectomy, we observed a high PPV (100%) but low sensitivity (64%), suggesting underreporting of this surgery. Less than two-thirds of women with a documented bilateral oophorectomy performed before age 50 years reported on subsequent screening questionnaires that their menstrual periods had ceased due to a bilateral oophorectomy. PPV analyses found the validity of self-reported unilateral oophorectomy to be lower than for bilateral oophorectomy, and suggest that a substantial proportion of women who self-report having had a unilateral oophorectomy have actually had both ovaries removed. Greater than 60% of women who underwent a bilateral oophorectomy without hysterectomy over the study period self-reported cessation of menses resulting from a hysterectomy; while we cannot rule out the possibility that these women received a hysterectomy prior to the study period, the underreporting of bilateral oophorectomy as a cause of menopause remains concerning given that young women who receive a simple hysterectomy (i.e., without bilateral oophorectomy) may continue to experience ovarian cycling until bilateral oophorectomy, even in the absence of menstruation. However, given that some women may have already been postmenopausal at the time of surgery, underreporting of these surgeries does not necessarily imply underreporting of oophorectomy as a reason for cessation of menses.
There are several limitations inherent to the present study, mostly related to the design of the study questionnaire and the availability of information in medical records. With respect to our sensitivity analyses, we were not able to rule out the possibility that natural menopause, or menopause due to another reason, had preceded the documented surgery. Specifically, the questionnaire asked women to report the reason why their menstrual periods had ceased with no separate question inquiring on history of hysterectomy or oophorectomy. If women who did not self-report their documented surgeries failed to do so because they had undergone natural menopause before their surgery, our estimates of sensitivity will be conservatively low. Given that, in the absence of bilateral oophorectomy, approximately 80% of Caucasian U.S. women remain hormonally premenopausal through age 49,17 we attempted to minimize this conservative bias by restricting the present analysis to women aged less than 50 at the time of surgery. In fact, we observed that only 13% of women who had undergone a hysterectomy and did not report that surgery as a reason for their cessation of menses reported a natural menopause. Thus, while the proportion of women included here who will have undergone natural menopause prior to surgery is not negligible, we anticipate that the bias to sensitivity estimates due to inclusion of these women should be small.
Additionally, because our sensitivity estimates were limited to surgeries performed in 1996-2003 and women with surgeries prior to age 50, it is difficult to extrapolate to women with less recent surgical procedures. It is possible that the sensitivity of self-report wanes with time since surgery, although we found no difference in sensitivity estimates based on questionnaires completed at least five years following surgery and estimates based on the first questionnaires completed post-surgery.
There are several possible reasons for the observed underreporting / misreporting of oophorectomy history: 1) women may not know if / how many ovaries they have had removed, 2) women may have forgotten if / how many ovaries they have had removed, and 3) women may not understand that having both of their ovaries removed would result in the cessation of menses or, if they have also had a hysterectomy, may not understand the additional relevance of having their ovaries removed. Underreporting may also reflect issues with the design of the screening questionnaire if the wording and ordering of possible reasons for cessation of menses led fewer women to report their history of oophorectomy.
The primary limitation of our PPV estimations was the scarcity of information in medical records, even for women with surgeries reportedly performed in the past 15 years. There was no mention as to the presence or absence of ovaries in medical records of 21% of women who self-reported an oophorectomy, and such information had to be gleaned from transcribed medical histories for 37% of such women. Using information from medical histories in the absence of more concrete evidence may have biased estimates of PPV for menopausal surgeries, although PPV estimates did not markedly change after excluding women for whom the only source of information was a medical history.
We estimate a higher PPV for self-reported hysterectomy than previously suggested Brett et al.12 In a medical record review of 452 participants in the National Health and Nutrition Examination Survey (NHANES) who had reported no history of hysterectomy at baseline but reported a hysterectomy in a follow-up interview (1982-84, 1986, or 1987), confirmation from hospital records could be located for only 298 (66%). The fact that we observed a larger PPV than this study may suggest improved awareness among women with regards to understanding the nature of the procedure or increasing documentation in medical records; it may also reflect the fact that the present study was conducted in an integrated group practice setting where access to medical records is likely more complete.
CONCLUSIONS
Despite study limitations, this analysis provides suggestive evidence that self-report of history of hysterectomy is valid and sensitive. This finding is reassuring given the relevance of hysterectomy to disease risk and to the determination of menopausal status. Prior studies have suggested that, in the absence of bilateral oophorectomy, women who undergo a hysterectomy experience a more rapid loss of ovarian function following surgery relative to women of a similar age who do not undergo hysterectomy, which would translate to an earlier average age at menopause.18,19 This study does, however, raise concerns regarding the completeness of self-report for oophorectomy history. We estimate that almost 20% of women who self-report a unilateral oophorectomy will have had both ovaries removed. We also found that less than two-thirds of women who had undergone a bilateral oophorectomy before age 50 reported that surgery as a reason why they had undergone menopause. Misreporting and underreporting of oophorectomy history are particularly relevant to the classification of menopausal status in epidemiologic studies: regardless of hysterectomy status, women with at least one ovary may continue ovulating up to the age of natural menopause while hormone cycling will cease after the removal of both ovaries. Thus, women with a bilateral oophorectomy who self-report having had only one or no ovaries removed may be misclassified as premenopausal or of unknown menopausal status. As epidemiologists, we often weigh the cost-benefit of having longer questionnaires to more accurately ascertain exposures or potential covariates. Given the importance of menopausal status to many outcomes including breast cancer and cardiovascular disease, it may be important to inquire, in separate questions, whether or not women have ever had a hysterectomy, whether or not they have ever had surgery to remove both ovaries, the timing of such surgical procedures, and whether or not they underwent these surgical procedures prior to experiencing the cessation of menstrual periods.
More that 600,000 hysterectomies are performed every year in the U.S., and it is estimated that approximately 20% of U.S. white women aged 40-49 have received a hysterectomy, with approximately 50% of these women also having had both ovaries removed.20 Given the widespread prevalence of these surgeries, and their relevance to disease risk and to the determination of menopausal status, knowing the validity of self-reported surgical history is an important step to developing a broad set of rules for classifying menopausal status in epidemiologic studies using self-reported data. The limitations encountered in this analysis support the need for more detailed, specific questions regarding menopausal surgeries in epidemiologic studies, and highlight the lack of adequate reporting of prior menopausal surgeries in medical records. In the context of these limitations, estimates of PPV and sensitivity of self-reported surgical history from this analysis indicate that women are able to recall and report their history of hysterectomy with great accuracy and able to recall and report their history of bilateral and unilateral oophorectomy with only moderate accuracy.
Acknowledgements
The authors acknowledge contributions to this project made by: Robert Reid, MD, PhD; Erin Aiello Bowles, MPH; Karla Kerlikowske, MD; Diana L. Miglioretti, PhD; Laura Ichikawa, MS; Patricia Carney, PhD; Deborah Seger, MS; Dawn Fitzgibbons, MPH; and Malia Oliver, MPH.
This work was funded by a cooperative agreement from the National Cancer Institute (U01CA63731, PI: DSM Buist).
REFERENCES
- 1.Soules MR, Sherman S, Parrott E, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW) Fertil Steril. 2001;76:874–878. doi: 10.1016/s0015-0282(01)02909-0. [DOI] [PubMed] [Google Scholar]
- 2.Lasley BL, Santoro N, Randolf JF, et al. The relationship of circulating dehydroepiandrosterone, testosterone, and estradiol to stages of the menopausal transition and ethnicity. J Clin Endocrinol Metab. 2002;87:3760–3767. doi: 10.1210/jcem.87.8.8741. [DOI] [PubMed] [Google Scholar]
- 3.Huang Z, Hankinson SE, Colditz GA, et al. Dual effects of weight and weight gain on breast cancer risk. JAMA. 1997;278:1407–1411. [PubMed] [Google Scholar]
- 4.Gierach GL, Johnson BD, Merz CN Bairey, et al. Hypertension, menopause, and coronary artery disease risk in the Women’s Ischemia Syndrome Evaluation (WISE) Study. J Am Coll Cardiol. 2006;47:S50–S58. doi: 10.1016/j.jacc.2005.02.099. [DOI] [PubMed] [Google Scholar]
- 5.Gaudet MM, Britton JA, Kabat GC, et al. Fruits, vegetables, and micronutrients in relation to breast cancer modified by menopause and hormone receptor status. Cancer Epidemiol Biomarkers Prev. 2004;13:1485–1494. [PubMed] [Google Scholar]
- 6.Slattery ML, Ballard-Barbash R, Edwards S, et al. Body mass index and colon cancer: an evaluation of the modifying effects of estrogen (United States) Cancer Causes Control. 2003;14:75–84. doi: 10.1023/a:1022545017867. [DOI] [PubMed] [Google Scholar]
- 7.Sauza AZ, Fonseca AM, Izzo WM, et al. Ovarian histology and function after total abdominal hysterectomy. Obstet Gynecol. 1986;68:847–849. [PubMed] [Google Scholar]
- 8.Brambilla DJ, McKinlay SM, Johannes CB. Defining the perimenopause for application in epidemiologic investigations. Am J Epidemiol. 1994;140:1091–1095. doi: 10.1093/oxfordjournals.aje.a117209. [DOI] [PubMed] [Google Scholar]
- 9.Johnson BD, Merz CN, Braunstein GD, et al. Determination of menopausal status in women: the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study. J Womens Health (Larchmt) 2004;13:872–887. doi: 10.1089/jwh.2004.13.872. [DOI] [PubMed] [Google Scholar]
- 10.Morabia A, Flandre P. Misclassification bias related to definition of menopausal status in case-control studies of breast cancer. Int J Epidemiol. 1992;21:222–228. doi: 10.1093/ije/21.2.222. [DOI] [PubMed] [Google Scholar]
- 11.Rockhill B, Colditz GA, Rosner B. Bias in breast cancer analyses due to error in age at menopause. Am J Epidemiol. 2000;151:404–408. doi: 10.1093/oxfordjournals.aje.a010220. [DOI] [PubMed] [Google Scholar]
- 12.Brett KM, Madans JH. Hysterectomy use: the correspondence between self-reports and hospital records. Am J Public Health. 1994;84:1653–1655. doi: 10.2105/ajph.84.10.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colditz GA, Stampfer MJ, Willett WC, et al. Reproducibility and validity of self-reported menopausal status in a prospective cohort study. Am J Epidemiol. 1987;126:319–325. doi: 10.1093/aje/126.2.319. [DOI] [PubMed] [Google Scholar]
- 14.Irwin KL, Wingo PA, Lee NC. Agreement of self-reported ovarian number following gynecologic surgery with medical record reports. J Clin Epidemiol. 1990;43:181–187. doi: 10.1016/0895-4356(90)90182-o. [DOI] [PubMed] [Google Scholar]
- 15.Taplin SH, Ichikawa L, Buist DS, et al. Evaluating organized breast cancer screening implementation: the prevention of late-stage disease? Cancer Epidemiol Biomarkers Prev. 2004;13:225–234. doi: 10.1158/1055-9965.epi-03-0206. [DOI] [PubMed] [Google Scholar]
- 16.Breast Cancer Surveillance Consortium Group Health Cooperative Risk Factor Questionnaire 2.2: sample standardized questionnaire. [(Accessed 27 July 2007)]; Updated 2006 September. Available from: www.breastscreening.cancer.gov/data/questionnaires/ssq_ghc_pat.pdf.
- 17.Gold EB, Bromberger J, Crawford S, et al. Factors association with age at natural menopause in a multiethnic sample of midlife women. Am J Epidemiol. 2001;153:865–874. doi: 10.1093/aje/153.9.865. [DOI] [PubMed] [Google Scholar]
- 18.Farquhar CM, Sadler L, Harvey SA, Stewart AW. The association of hysterectomy and menopause: A prospective cohort study. BJOG. 2005;112:956–962. doi: 10.1111/j.1471-0528.2005.00696.x. [DOI] [PubMed] [Google Scholar]
- 19.Chang SH, Kim CS, Lee KS, et al. Premenopausal factors influencing ovarian failure and early menopause. Maturitas. 2007;58:19–30. doi: 10.1016/j.maturitas.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Merrill RM. Impact of hysterectomy and bilateral oophorectomy on race-specific rates of corpus, cervical, and ovarian cancers in the United States. Ann Epidemiol. 2006;16:880–887. doi: 10.1016/j.annepidem.2006.06.001. [DOI] [PubMed] [Google Scholar]


