Abstract
Delirium is a very common medical condition encountered throughout the world and, undoubtedly, is one of the most frequent reasons psychiatrists are consulted by primary care physicians. Recognizing delirium and treating the underlying medical cause are the first steps in the management of this potentially fatal syndrome. The selection of an appropriate medication to target the perceptual, behavioral, and cognitive abnormalities is crucial. In addition to several of the older, typical antipsychotics, which have been found to be effective for the treatment of delirium, some of the newer, atypical antipsychotic agents have been demonstrated to be efficacious. This paper will review both the typical and atypical antipsychotics with the best evidence for efficacy and safety in the treatment of delirium. Finally, environmental treatments are discussed to present the full armamentarium of therapeutic options available to the practicing clinician.
Keywords: delirium, antipsychotics, epidemiology, somatic treatment
Introduction
Delirium is best described as a disturbance of consciousness with reduced attention, changes in cognition, and perceptual disturbances. Delirium is more common than may be predicted as 10 to 15 percent of medically ill inpatients can be delirious, and 30 to 50 percent of acutely ill geriatric patients are delirious at any given time in the hospital. Patients without delirium in the hospital have a two-percent mortality rate, with an additional three-percent mortality at three months after discharge. The mortality rate in delirious patients in the hospital has been found to be 11 percent, with 11 percent mortality at three months after discharge.1
Delirium reflects brain dysfunction that is almost always due to identifiable systemic or cerebral disease or to drug intoxication or withdrawal states. The disturbance is caused by the direct physiological consequences of a general medical condition.2,3 The onset of delirium is typically rapid and is characterized by a fluctuating course throughout the day with disturbances in consciousness and cognition (Table 1).
TABLE 1.
Core and common features of delirium are present in all DSM IV subtypes of delirium
| Core features of delirium are present in all DSM-IV subtypes of delirium. Common features of delirium may be present in all DSM-IV subtypes of delirium. | |
THE CORE FEATURES INCLUDE:
| |
COMMON FEATURES INCLUDE:
| |
Risk factors for delirium include greater severity of physical illness, older age, and baseline cognitive impairment.3 In particular, burn victims, postoperative and sensory-deprived patients, and patients with human immunodeficiency virus (HIV), head injury, seizures, renal failure, hepatic failure, or cardiac failure are at risk for delirium.4 Recognizing delirium, which may be subtle in less agitated forms, is particularly important as it may be the only evidence of a life-threatening condition.5 Differentiating delirium from dementia is of paramount importance and can be accomplished by noting the temporal pattern of the condition, as well as the attention span of the patient. Delirium differs from dementia in that delirium is characterized by fluctuations in the mental status of the patient (e.g., alertness, orientation), whereas dementia is characterized by a static mental status. Delirium is typically more acute in onset and may be rapidly fatal if not reversed, whereas dementia has a longer and more insidious course. It should be noted that it can be very difficult to distinguish delirium from dementia, especially when the condition is comorbid as is common in the elderly population.
Prompt treatment of delirium is crucial as this syndrome has a significant mortality rate. As a first step, the physician should search for contributing causes, obtain a complete history, including a careful review of medication usage and illicit drug history, and perform full physical and neurological exams. Laboratory tests with neuroimaging studies and a lumbar puncture may be necessary. The most basic treatment principals begin with identifying and treating the causal or contributing medical conditions. If the patient is being treated with sedatives or other medications affecting the central nervous system, the physician should discontinue these agents. The exception to this rule is the patient who is delirious due to sedative-hypnotic or alcohol withdrawal.2
Neuropathogenesis
The list of illnesses, medications, and conditions that can cause delirium is extensive. Nonetheless, there is great controversy over how the brain becomes trapped in this altered state of consciousness. Both cortical and subcortical dysfunction have been implicated by regional cerebral blood flow studies, single photon emission computed tomography, positron-emission tomography, electroencephalogram, and evoked potentials.7
Among the neurotransmitters most strongly implicated in delirium pathogenesis are acetylcholine and dopamine. While decreased acetylcholine activity is presumed to play a role in delirium, hyperactivity in the dopamine system is also a strong etiologic candidate. Less certain is the role of serotonin and gamma-aminobutyric acid (GABA) in which an either increased or decreased activity of these neurotransmitters may be involved in delirium pathogenesis. Finally, excess glutamate activity or decreased histamine activity also may be etiologic factors in delirium (Figure 1).7
FIGURE 1.
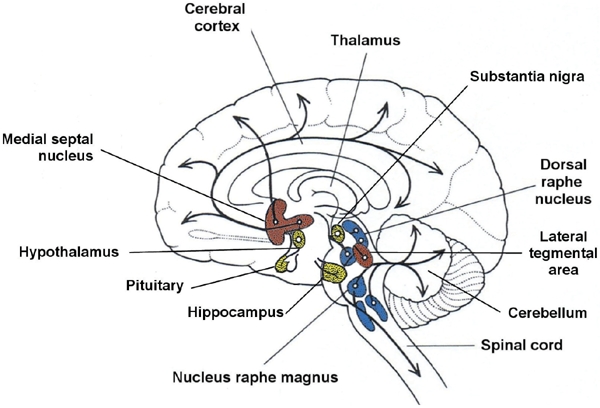
Cholinergic (red), dopaminergic (yellow), and serotonergic (blue) projection systems in the brain.
A complete list of all the possible causes of delirium would be very difficult and lengthy to compile due to the variety of causes potentially responsible for the condition. The most frequent causes of delirium include infectious disease, particularly of the central nervous system, cardiovascular compromise, endocrine abnormalities, trauma, and metabolic derangements from toxins, electrolyte imbalance, or withdrawal states. Some of the more common causes and etiologic factors are expanded upon and summarized in Table 2.
TABLE 2.
The differential diagnosis for delirium using the mnemonic “I WATCH DEATH”
| Adapted with permission from The American Psychiatric Press Textbook of Consultation-Liaison Psychiatry. Washington, DC: American Psychiatric Press, Inc., 1996. | |
| INFECTION | Encephalitis, meningitis, syphilis, HIV, sepsis |
| WITHDRAWAL | Alcohol, barbiturates, sedative-hypnotics |
| ACUTE METABOLIC | Acidosis, alkalosis, electrolyte disturbance, hepatic failure, renal failure |
| TRAUMA | Closed-head injury, heat stroke, postoperative, severe burns |
| CNS PATHOLOGY | Abscess, hemorrhage, hydrocephalus, subdural hematoma, seizures, stroke, infection, tumors, metastases, vasculitis |
| HYPOXIA | Anemia, carbon monoxide poisoning, hypotension, pulmonary or cardiac, cardiac failure |
| DEFICIENCIES | Vitamin B12, folate, niacin, thiamin |
| ENDOCRINOPATHIES | Hyper/hypoadrenocorticism, hyper/hypoglycemia, myxedema, hyperparathyroidism |
| ACUTE VASCULAR | Hypertensive encephalopathy, stroke, arrhythmia, shock |
| TOXINS OR DRUGS | Medications, illicit drugs, pesticides, solvents |
| HEAVY METALS | Lead, manganese, mercury |
Key:
- CNS—
central nervous system
- HIV:
human immunodeficiency virus
Pharmacologic Treatment Options
With regard to the pharmacological management of delirium, antipsychotics are the drugs of choice and should be administered at the lowest adequate dosages. For more threatening agitation, a combination of antipsychotics and benzodiazepines along with ventilatory support has been utilized.8
Haloperidol, a typical antipsychotic, is the most frequently used and best studied antipsychotic medication for delirium due to its few anticholinergic side effects, few active metabolites, and small likelihood of causing sedation. Most studies have used doses of haloperidol from 0.25 to 0.50mg every four hours for the elderly or seriously medically compromised patients to doses of 2 to 3mg per day in healthier patients. For very agitated patients, bolus doses of 5 to 10mg per hour intravenously have been used in hospital settings.9,10 The main outcome measures for these studies were the Brief Psychiatric Rating Scale, Schedule for Affective Disorders Scale, Clinical Dementia Rating Scale, and the Behavioral Syndromes Scale for Dementia. A study with haloperidol, chlorpromazine, and lorazepam groups have demonstrated improvements in the mental status as measured by the Delirium Rating Scale in the haloperidol and chlorpromazine groups but not the lorazepam groups.11 A criticism of this study is that the mean doses of haloperidol and chlorpromazine were low 1.4mg per day and 36mg per day respectively, while the dose of lorazepam was more moderate at 4.6mg per day. As mentioned in a review paper on delirium by Pae, et al., in a larger, placebo-controlled study comparing haloperidol to olanzapine, an atypical antipsychotic discussed in more detail later, little difference between active medication groups but superiority to placebo was demonstrated.12,13 In this study, low to moderate doses of haloperidol and olanzapine were used, 4.5mg versus 7.1mg respectively, and the instrument measure was the Delirium Rating Scale. The size of the active medication groups for haloperidol and olanzapine were 72 versus 74 patients with 29 patients receiving placebo and the mean time to improvement being 3.4 days versus 2.8 days and 5.2 days for those receiving placebo.
Other typical antipsychotics have been the subject of investigation for treatment of delirium (acute organic mental syndrome), but many of these studies are 20 to 30 years old and do not always utilize diagnostic nomenclature compatible with contemporary medical practice. In the 1980s, a single blind study of haloperidol and thiothixene on 14 patients showed that both drugs were effective in relieving delirium with a possible slight advantage for thiothixene as measured by the Brief Psychiatric Rating Scale.14 The dose of haloperidol was between 4.8 and 15mg and the thiothixene dose was between 2 and 7mg per day.
Earlier studies from the 1970s of thiothixene, loxapine, and thioridazine are difficult to incorporate into the evidence base given their admitted diagnostic heterogeneity and small sample sizes. One double-blind, placebo-controlled study of thiothixene dosed at 2 to 5mg up to three times a day failed to find superiority of the drug for chronic organic brain syndrome. The outcome measures of this study were the Brief Psychiatric Rating Scale and Nursing Observational Scale for Inpatient Evaluation.15 Another study contained two individual, double-blind trials of loxapine versus thioridazine for the treatment of chronic organic brain syndromes. One of these studies found loxapine at 10 to 150mg per day to be superior to thioridazine at 150 to 750mg per day for the treatment of chronic organic brain syndrome while the other demonstrated equal efficacy. The outcome measures were the Brief Psychiatric Rating Scale and Nursing Observational Scale for Inpatient Evaluation along with the Clinical Global Impressions Scale.16 Finally, one case report describes a patient who did not respond to higher-dose olanzapine, 20mg per day, but did respond to lower-dose loxapine, 45mg per day. Because rating scales for delirium were not utilized, equivalent doses of these medications were not established, and olanzapine is particularly sedating at higher doses, this case report is difficult to interpret.17
A brief case series of four patients with HIV-associated delirium demonstrated that molindone in doses of 40 to 140mg per day was effective in controlling delirium in each of the patients treated. Caution should be applied in coming to a conclusion from this report as the patients were on other typical antipsychotics at times, such as haloperidol and thioridazine, and no delirium rating scales were utilized.18 The evidence for use of typical antipsychotics in delirium is presented in Table 3.
TABLE 3.
Evidence for the use of typical antipsychotics in delirium
| STUDY | TYPE OF EVIDENCE | COMMENTS |
|---|---|---|
| Molindone (Fernandez F, Levy JK) n=4 | Case study | Molindone safe and effective |
| Loxapine versus olanzapine (Kreiger D, et al.) n=1 | Case study | Loxapine superior to olanzapine |
| Loxapine versus thioridazine (Versiani M, et al.) n=40 (20 patients per group) | RCT | Loxapine superior to thioridazine in one trial of a two-part study but equivalent in other part |
| Thiothixine verus haloperidol (Peterson LG, Bognar B) n=14 (8 and 6 patients respectively) | RCT | Haloperidol superior to thiothixene |
| Haloperidol, chlorpromazine, and lorazepam (Breitbart W, et al.) n=30 (11, 13, and 6 patients in each respective group) | RCT | Only study selected by Cochrane Collaboration. Both haloperidol and chlorpromazine superior to lorazepam |
| Haloperidol, olanzapine, and placebo (Hu X, Deng W, Yang H) n=175 (72, 74, and 29 patients in each respective group) | RCT | Haloperidol equivalent to olanzapine and both superior to placebo |
KEY:
- RCT—
randomized, controlled trial
With the advent of atypical antipsychotics and their decreased risk of extrapyramidal side effects, there has been increased interest in using these agents for delirium. After clozapine, which clearly has serious limitations (lethal agranulocytosis) to its use for any disorder other than refractory schizophrenia or schizoaffective disorder, risperidone was the next atypical antipsychotic approved for use in the United States. An early case report in two patients with hypoxic brain injury demonstrated the potential capability of risperidone to be effective in treating delirium.19 After this, five separate studies in patients with a variety of underlying medical illnesses demonstrated the effectiveness of risperidone at doses ranging from 0.75mg per day to 3.1mg per day in the treatment of delirium with the majority of patients showing moderate to marked improvement of their delirium on the Clinical Global Impressions Scale, Brief Psychiatric Rating Scale, and Trzepacz Delirium Rating Scale. Common side effects of risperidone included sedation, dizziness, and extrapyramidal symptoms (EPS). The average length of treatment in these studies was approximately one week.20–24 In a small case series conducted in Israel, three elderly patients were administered risperidone and subsequently developed delirium. One of these patients was also receiving lithium at a therapeutic level, another was in the middle of a course of electroconvulsive therapy (ECT) treatment, and the last was mildly hyponatremic and receiving fluvoxamine and diuretics along with the risperidone. Clearly, other etiological factors for the delirium could have been operative.25 A double-blind trial of risperidone and haloperidol demonstrated equivalence in treatments in efficacy and response rates. The mean daily dose of risperidone was 1.02mg and the mean daily dose of haloperidol was 1.71mg.26 The Trzepacz Delirium Rating Scale was again the main rating scale utilized. One large double-blind, placebo-controlled study using risperidone for the treatment of delirium in doses of 0.5mg to 4.0mg per day did not demonstrate efficacy for this agent. Nonetheless, a major confounding factor was the fact that the Positive and Negative Symptom Scale was used to measure delirium though this scale is not a measure of delirium specifically and measures multiple other aspects of mental functioning.27
Olanzapine would appear to have sufficient evidence to sustain a claim for delirium treatment. An early case report of the successful treatment of delirium in a cancer patient with olanzapine appeared in the literature in 1998.28 In two open trials of hospitalized patients using similar doses of olanzapine, the outcome was a 50-percent reduction in the Delirium Rating Scale and a marked reduction in the Memorial Delirium Assessment Scale.29,30 Two other studies of olanzapine at mean doses of 4.5mg per day to 8.2mg per day demonstrated comparable reductions in delirium when measured against haloperidol at mean doses of 4.5mg per day to 5.1mg per day on the Delirium Rating Scale and Memorial Delirium Assessment Scale. The peak response time of both groups was similar at nearly seven days. In addition, those on olanzapine had less extrapyramidal side effects and less sedation than the haloperidol group.31,32
Quetiapine, with its very low incidence of extrapyramidal side effects, should be an attractive choice for the delirious elderly patient if proven clinically efficacious. Two sets of case reports with two patients each demonstrated quetiapine to be safe and effective for the treatment of delirium at doses of 50 to 100mg per day within one week of initiation. One of these reports utilized the Delirium Rating Scale and Mini Mental Scale Examination as rating scales while the other used no rating scales.33,34 When compared to haloperidol, delirious patients on quetiapine showed similar improvements on the Delirium Rating Scale but quetiapine was better tolerated.35 Four open-label trials of between 12 and 22 patients using quetiapine at 25 to 200mg per day demonstrated the effectiveness of this agent in almost all patients after approximately seven days of treatment with much improved Delirium Rating Scales, Mini Mental Scale Examination scales, and Clinical Global Impression scales.36–39
The two latest additions to the antipsychotic armamentarium, ziprasidone and aripiprazole, have less information published regarding delirium. A case report of a delirious 34-year-old HIV-positive man with possible cryptococcal meningitis had to be abandoned due to cardiac side effects. Ziprasidone treatment, initiated at 20mg per day and then titrated up to 100mg per day, led to an improvement in the delirium as demonstrated by a significant reduction in the Delirium Rating Scale. Nonetheless, there is too little information to draw a definitive conclusion.40 A case report in the anesthesiology literature reported the successful use of ziprasidone for delirium. Ziprasidone was given intravenously at 20mg after a failed course of haloperidol and then tapered orally over the course of a week. The patient improved but there were no details given on the doses of the taper or if any rating scale was used to measure the delirium.41
Aripiprazole, the newest atypical antipsychotic, likewise, has evidence of its usefulness in the treatment of delirium with two case studies each having two patients given 15 to 30mg of the agent per day and utilizing the Delirium Rating Scale and Mini Mental Scale Examination as rating scales.42,43 A case series examining 14 patients with delirium of varying etiologies treated with 5 to 15mg of aripiprazole per day demonstrated the efficacy of this agent in nearly all patients treated. The response time ranged from several days to two weeks and was gauged with the Delirium Rating Scale and Clinical Global Impressions Scale.44 The evidence for use of atypical antipsychotics in delirium is presented in Table 4.
TABLE 4.
Evidence for the use of atypical antipsychotics in delirium
| STUDY MEDICATION | AUTHOR | N | STUDY DESIGN | RESULTS |
|---|---|---|---|---|
| Risperidone | Sipahimalani A, et al. | 2 | Case report | Risperidone safe and effective |
| Risperidone | Ravona-Springer, et al. | 3 | Case series | Risperidone thought to play a role in the etiology of delirium |
| Risperidone | Sipahimalani A, et al. | 11 | Case series | Risperidone safe and effective |
| Risperidone | Furmaga KM, et al. | 7 | Open trial | Risperidone safe and effective |
| Risperidone | Horikawa N, et al. | 10 | Open trial | Risperidone safe and effective |
| Risperidone | Mittal D, et al. | 10 | Open trial | Risperidone safe and effective |
| Risperidone | Parellada E, et al. | 64 | Open trial | Risperidone safe and effective |
| Risperidone | Hans CS, et al. | 12 vs. 12 | Double blind trial of risperidone vs. haloperidol | Risperidone equivalent to haloperidol |
| Risperidone | Naber D, et al. | 815 | Double blind placebo-controlled trial of risperidone | Risperidone not superior to placebo |
| Olanzapine | Passik SD, et al. | 1 | Case report | Olanzapine safe and effective |
| Olanzapine | Breitbart, et al. | 79 | Open trial | Olanzapine safe and effective |
| Olanzapine | Kim, et al. | 20 | Open trial | Olanzapine safe and effective |
| Olanzapine | Sipahimalani A, et al. | 11 vs. 11 | Open trial | Olanzapine equivalent to haloperidol |
| Olanzapine | Skrobik YK, et al. | 28 vs. 45 | Open trial | Olanzapine equivalent to haloperidol |
| Quetiapine | Torres R, et al. | 2 | Case report | Quetiapine safe and effective |
| Quetiapine | Al-Samarri S, et al. | 2 | Case report | Quetiapine safe and effective |
| Quetiapine | Schwartz TL, et al. | 11 vs. 11 | Retrospective chart review | Quetiapine equivalent to haloperidol |
| Quetiapine | Pae CU, et al. | 22 | Open trial | Quetiapine safe and effective |
| Quetiapine | Kim KY, et al. | 12 | Open trial | Quetiapine safe and effective |
| Quetiapine | Sasaki Y, et al. | 12 | Open trial | Quetiapine safe and effective |
| Quetiapine | Maneeton N, et al. | 17 | Open trial | Quetiapine safe and effective |
| Ziprasidone | Leso L, Schwartz TL | 1 | Case report | Ziprasidone effective but PVC’s limit use (medically ill, immunocompromised patient) |
| Ziprasidone | Young CC, Lugan E | 1 | Case report | Ziprasidone safe and effective |
| Aripiprazole | Alao AO, et al. | 2 | Case report | Aripiprazole safe and effective |
| Aripiprazole | Alao AO, Moskowitz L | 2 | Case report | Aripiprazole safe and effective |
| Aripiprazole | Straker DA, et al. | 14 | Case series | Aripiprazole safe and effective |
Despite the fact that antipsychotics are useful for the treatment of delirium, these medications are associated increased risk of mortality in elderly patients with dementia, a common comorbid condition. One recent study documents the risk of a serious adverse event, defined as an event leading to acute care hospital admission or death, to be 2.4 times more likely for patients on typical antipsychotics than placebo and 1.9 times more likely for patients on atypical antipsychotics than placebo.45
Nonpharmacological treatments for delirium also exist and should not be overlooked in treating this serious condition. It should be recognized, however, that nonpharmacological treatments are adjuncts to, not substitutes for, prompt pharmacological treatment for delirium. The patient should be provided a quiet environment free of excess stimulation and be reoriented frequently.
While providing a safe environment for the recovering patient is crucial, the patient should not be either overly stimulated or actively ignored. At the most basic level, the room that the patient is placed in should be well lit, moderately furnished, and contain a clock and a calendar. Contact with family and staff is helpful. Providing extra supportive physical care, such as nutrition and fluid intake, may be necessary. The use of physical restraints should be limited for diagnostic testing, performing procedures, and patient or staff safety. Document carefully and frequently in the chart the use and rationale for employing physical restraints.
Summary
Delirium is a common medical condition likely to be encountered on the wards in any hospital. Several typical antipsychotics have been demonstrated to be effective but have the potential problems of extrapyramidal side effects and cardiac conduction delays. Atypical antipsychotics are effective for delirium and are associated with less extrapyramidal side effects. While there is little in the way of head to head trials of typical antipsychotics versus atypical antipsychotics for the treatment of delirium, those that do exist seem to suggest equivalence.46,47 Haloperidol continues to be the “gold standard” medication for the treatment of delirium, but atypical antipsychotics may supplant the typical antipsychotics due to their effective and safe management of this condition.48 Numerous studies support the assertion that risperidone, olanzapine, and quetiapine have the best data for the treatment of delirium among the atypical antipsychotics.49
Acknowledgments
The author would like to thank Brandon Cox, BA, for his assistance with graphic artwork and technology.
References
- 1.Pompei P, Foreman M, Rudberg MA, et al. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc. 199442(8)809–815 [DOI] [PubMed] [Google Scholar]
- 2.Gleason OC.Delirium. Am Fam Physician. 200367(5)1027–1034 [PubMed] [Google Scholar]
- 3.Kaplan HI, Sadock BJ.Kaplan HI.Delirium, dementia, and amnestic and other cognitive disorders and mental disorders due to a general medical condition. Synopsis of Psychiatry. Eighth Edition. Philadelphia, PA: Lippincott, Williams, and Wilkins; 1998320–328 [Google Scholar]
- 4.Schwartz TL, Masand PS.The role of atypical antipsychotics in the treatment of delirium. Psychosomatics. 200243(3)171–174 [DOI] [PubMed] [Google Scholar]
- 5.Jacobson S, Schreibman B.Behavioral and pharmacologic treatment of delirium. Am Fam Physician. 199756(8)2005–2012 [PubMed] [Google Scholar]
- 6.Wise MG, Trzepacz PT.Wise MG, Rundell JR.Delirium (Confusional States). The American Psychiatric Press Textbook of Consultation-Liaison Psychiatry. Washington D.C: American Psychiatric Press Publishing; 2005257–272 [Google Scholar]
- 7.Trzepacz PT, Meagher DJ.Levensen JL.Delirium. Textbook of Psychosomatic Medicine. Washington, DC: American Psychiatric Publishing, Inc.,200591–130 [Google Scholar]
- 8.Heckers S, Stern TA.Herman JB.Delirium. The Massachusetts General Hospital Psychiatry Update and Board Preparation, Second Edition.New York, NY: McGraw-Hill Publishing Company; 200443–47 [Google Scholar]
- 9.Trzepacz P.(chair). Practice Guidelines for the Treatment of Patients With Delirium, in American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2002. Washington, DC: American Psychiatric Association; 200229–60 [Google Scholar]
- 10.Devanand DP, Marder K, Michaels KS, et al. A randomized, placebo-controlled dose-comparison trial of haloperidol for psychosis and disruptive behaviors in Alzheimer’s disease. Am J Psychiatry. 1998155(11)1512–1520 [DOI] [PubMed] [Google Scholar]
- 11.Breitbart W, Marotta R, Platt M, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium of hospitalized AIDS patients. Am J Psychiatry. 1996153(2)231–237 [DOI] [PubMed] [Google Scholar]
- 12.Hu X, Deng W, Yang H.A prospective random control study compraison of olanzapine and haloperidol in senile delirium [Chinese]. Chong’qing Med J. 200481234–1237 [Google Scholar]
- 13.Pae C, Marks DM, Han C, et al. Delirium: where do we stand? Curr Psychiatry Rep. 200810240–248 [DOI] [PubMed] [Google Scholar]
- 14.Peterson LG, Bongar B.Navane versus haldol: treatment of acute mental syndromes in the general hospital. Gen Hosp Psychiatry. 198911(6)412–417 [DOI] [PubMed] [Google Scholar]
- 15.Rada RT.Kellner R: Thiothixene in the treatment of geriatric patients with chronic organic brain syndrome. J Am Geriatr Society. 197624(3)105–107 [DOI] [PubMed] [Google Scholar]
- 16.Versiani M, da Silva JAR, Mundin FD.Loxapine versus thioridazine in the treatment of organic psychosis. J Int Med Res. 19808(22)22–30 [DOI] [PubMed] [Google Scholar]
- 17.Krieger D, Hansen K, McDermott C, et al. Loxapine versus olanzapine in the treatment of delirium following traumatic brain injury. Neuro Rehabilitation. 200318(3)205–208 [PubMed] [Google Scholar]
- 18.Fernandez F, Levy JK.The use of molindone in the treatment of psychotic and delirious patients infected with the human immunodeficieny virus. Gen Hosp Psychiatry. 199315(1)31–35 [DOI] [PubMed] [Google Scholar]
- 19.Sipahimalani A, Masand PS.Use of risperidone in delirium. Ann Clin Psychiatry. 19979(2)105–107 [DOI] [PubMed] [Google Scholar]
- 20.Sipahimalani A, Sime RM, Masand PS.Treatment of delirium with risperidone. Int J Geriatric Psychopharmacol. 1997124–26 [Google Scholar]
- 21.Furmaga KM, DeLeon OA, Sinha SB, et al. Psychosis in medical conditions. Gen Hosp Psychiatry. 199719(3)223–228 [DOI] [PubMed] [Google Scholar]
- 22.Horikawa N, Yamazaki T, Miyamoto K, et al. Treatment for delirium with risperidone. Gen Hosp Psychiatry. 200325(4)289–292 [DOI] [PubMed] [Google Scholar]
- 23.Mittal D, Jimerson NA, Neely EP, et al. Risperidone in the treatment of delirium: results from a prospective open-label trial. J Clin Psychiatry. 200465(5)662–667 [DOI] [PubMed] [Google Scholar]
- 24.Parellada E, Baeza I, de Pablo J, et al. Risperidone in the treatment of patients with delirium. J Clin Psychiatry. 200465(3)348–353 [DOI] [PubMed] [Google Scholar]
- 25.Ravona-Springer R, Dolberg O, Hirschmann S, et al. Delirium in elderly patients treated with risperidone: a report of three cases. J Clin Psychopharmacol. 199818(2)171–172 [DOI] [PubMed] [Google Scholar]
- 26.Han CS, Kim YK.A double-blind trial of risperidone and haloperidol for the treatment of delirium. Psychosomatics. 200445(4)297–301 [DOI] [PubMed] [Google Scholar]
- 27.Naber D, Greenspan A, Schreiner A.Efficacy and safety of risperidone in the treatment of elderly patients suffering from organic brain disease (organic brain syndrome): results from a double-blind, randomized, placebo-controlled clinical trial. Psychopharmacology. 2007191(4)1027–1029 [DOI] [PubMed] [Google Scholar]
- 28.Sipahimalani A, Masand PS.Olanzapine in the treatment of delirium. Psychosomatics. 199839(5)422–430 [DOI] [PubMed] [Google Scholar]
- 29.Breitbart W, Tremblay A, Gibson C.An open trial of olanzapine for the treatment of delirium in hospitalized cancer patients. Psychosomatics. 200243(3)175–182 [DOI] [PubMed] [Google Scholar]
- 30.Kim KS, Pae CU, Chae JH, et al. An open pilot trial of olanzapine for felirium in the Korean population. Psychiatry Clin Neurosci. 200155(5)515–519 [DOI] [PubMed] [Google Scholar]
- 31.Passik SD, Cooper M.Complicated delirium in a cancer patient successfully treated with olanzapine. J Pain Symptom Management. 199917(3)219–223 [DOI] [PubMed] [Google Scholar]
- 32.Skrobik YK, Bergeron N, Dumont M, et al. Olanzapine versus haloperidol: treating delirium in a critical care setting. Intensive Care Med. 200430(3)444–449 [DOI] [PubMed] [Google Scholar]
- 33.Torres R, Mittal D, Kennedy R.Use of quetiapine in delirium: case reports. Psychosomatics. 200142(4)347–349 [DOI] [PubMed] [Google Scholar]
- 34.Al-Samarrai S, Dunn J, Newmark T, et al. Quetiapine for treatment-resistant delirium. Psychosomatics. 200344(4)350–351 [DOI] [PubMed] [Google Scholar]
- 35.Schwartz TL, Masand PS.Treatment of delirium with quietapine. J Clin Psychiatry. 20002(1)10–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pae CU, Lee SJ, Lee CU, et al. A pilot trial of quetiapine for the treatment of patients with delirium. Hum Psychopharmacol. 200419(2)125–127 [DOI] [PubMed] [Google Scholar]
- 37.Kim KY, Bader GM, Kotylar V, et al. Treatment of delirium in older adults with quetiapine. J Geriatr Psychiatry Neurol. 2003;16((1)):31. doi: 10.1177/0891988702250533. [DOI] [PubMed] [Google Scholar]
- 38.Sasaki Y, Matsuyama T, Inoue S, et al. A prospective, open-label, flexible-dose study of quetiapine in the treatment of delirium. J Clin Psychiatry. 200364(11)1316–1321 [DOI] [PubMed] [Google Scholar]
- 39.Maneeton B, Maneeton N, Srisurapanont M.An open-label study of quetiapine for delirium. J Med Assoc Thai. 200790(10)2158–2162 [PubMed] [Google Scholar]
- 40.Leso L, Schwartz TL.Ziprasidone treatment of delirium. Psychosomatics. 200243(1)61–62 [DOI] [PubMed] [Google Scholar]
- 41.Young CC, Lujan E.Intravenous ziprasidone for treatment of delirium in the intensive care unit. Anesthesiology. 2004101(3)794–795 [DOI] [PubMed] [Google Scholar]
- 42.Alao AO, Soderberg M, Pohl EL, et al. Aripiprazole in the treatment of delirium. Int J Psychiatry Med. 200535(4)429–433 [DOI] [PubMed] [Google Scholar]
- 43.Alao AO, Moskowitz L.Aripiprazole and felirium. Ann Clin Psychiatry. 200618(4)267–269 [DOI] [PubMed] [Google Scholar]
- 44.Straker DA, Shapiro PA, Muskin PR.Aripiprazole in the treatment of delirium. Psychosomatics. 200647(5)385–391 [DOI] [PubMed] [Google Scholar]
- 45.Rochon PA, Normand S, Gomes T, et al. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Int Med. 2008168(10)1090–1096 [DOI] [PubMed] [Google Scholar]
- 46.Ozbolt LB, Paniagua MA, Kaiser RM.Atypical antipsychotics for the treatment of delirious elders. J Am Med Direct Assoc. 20089(1)18–28 [DOI] [PubMed] [Google Scholar]
- 47.Rea RS, Battistone S, Fong JJ, et al. Atypical antipsychotics versus haloperidol for treatment of delirium in acutely ill patients. Pharmacotherapy. 200727(4)588–594 [DOI] [PubMed] [Google Scholar]
- 48.Conn DK, Lieff S.Diagnosing and managing delirium in the elderly. Can Fam Physician. 200147101–108 [PMC free article] [PubMed] [Google Scholar]
- 49.Boettger S, Breitbart W.Aytpical antipsychotics in the management of delirium: a review of the emperical literature. Palliat Support Care. 20053(3)227–238 [DOI] [PubMed] [Google Scholar]


