Abstract
Hepatocellular carcinoma (HCC) has a decisive influence on the prognosis of cirrhotic patients. Although α-fetoprotein (AFP) is a known and specific tumor maker for HCC, it is not suitable for the screening and surveillance of HCC because of its poor predictive value and low sensitivity. The use of imaging modalities is essential for the screening, diagnosis and treatment of HCC. Ultrasound (US) plays a major role among them, because it provides real-time and non-invasive observation by a simple and easy technique. In addition, US-guided needle puncture methods are frequently required for the diagnosis and/or treatment process of HCC. The development of digital technology has led to the detection of blood flow by color Doppler US, and the sensitivity for detecting tumor vascularity has shown remarkable improvement with the introduction of microbubble contrast agents. Moreover, near real-time 3-dimensional US images are now available. As for the treatment of HCC, high intensity focused ultrasound (HIFU) was developed as a novel technology that provides a transcutaneous ablation effect without needle puncture. These advancements in the US field have led to rapid progress in HCC management, and continuing advances are expected. This article reviews the current application of US for HCC in clinical practice.
Keywords: Ultrasound, Contrast agent, Hepatocellular carcinoma, Liver, Surveillance, Treatments
INTRODUCTION
Hepatocellular carcinoma (HCC) is increasing worldwide and is one of the most common carcinomas in the eastern part of Asia[1]. As the prognosis of cirrhotic patients depends on the occurrence and progression of HCC, management of this neoplasm is a major issue in clinical practice. The recent popularization of periodic surveillance and the development of diagnostic capabilities have resulted in the discovery of increasing numbers of patients with small HCC nodules[2,3]. Although tumor markers may be helpful for the diagnosis of HCC, imaging modalities are essential for finding and characterizing this neoplasm[4,5].
On the basis of the continuing development of digital technologies, ultrasound (US) has also shown significant improvements within the last decade[6]. As for grey-scale imaging, tissue harmonic imaging (THI) has improved both lateral resolution and contrast resolution by narrowing the width of the US beam, with the reduction of reverberation and side-lobe artifacts. Since the margin and structure of tumor nodules have become clear, with distinct delineation[7–10], THI has become popular as part of the routine work of grey-scale US examination.
Color Doppler imaging provides real-time evaluation of the hemodynamics in liver tumors, and power Doppler mode has contributed to a better detectability of blood flow[11–15]. However, limitations in the detection of slow flow and vessels located deeply from the skin surface have prevented the wider application of Doppler mode in the evaluation of tumor hemodynamics[16–18]. Furthermore, artifacts caused by respiratory or cardiac motion sometimes affect the precise evaluation of hemodynamic information.
With these backgrounds, US contrast agents have been expected to improve the detectability of blood flow in liver tumors, since the first report about a US contrast agent by Gramiak et al[19]. From the late 1980s to the 1990s, grey-scale contrast-enhanced US with carbon dioxide gained broad attention as an echo-enhancing technique, with high sensitivity for detecting tumor vascularity and high performance for the characterization of liver tumors[20,21]. However, this method requires an arteriography procedure because carbon dioxide is easily soluble in blood. The development of microbubble contrast agents together with peripheral venous injection was expected for practical use. In the late 1990’s, a galactose-based US contrast agent (SHU 508, Levovist) was made available by Schering, Germany[22,23]. It was a long-awaited material that could provide a stable enhancement effect in abdominal organs with a peripheral injection. Subsequently, many microbubble contrast agents have been produced or are currently under development. At present, the application of Doppler mode alone for detecting tumor blood flow is rare, as contrast-enhanced US with microbubble contrast agents provides details of the hemodynamics that are useful for the detection and characterization of liver tumors. Additionally, three-dimensional US images are now easily available due to the development of advanced digital technologies[24,25], and high intensity focused ultrasound (HIFU) was developed as a novel treatment method for tumors[26]. This article reviews the current development and application of US for the diagnosis and treatment of HCC.
SURVEILLANCE FOR HCC
Viral-related and/or alcoholic chronic liver disease is a high-risk factor for developing HCC that limits the prognosis. There is no question about the importance of periodic surveillance for HCC in these high-risk patients[27–29]. Some serum markers are known for HCC, and α-fetoprotein (AFP) is widely used for its diagnosis[30–32]. Ishii et al reported that sensitivity and specificity of AFP was 13.8% and 97.4% at a cut-off value of 200 ng/mL, respectively, and 62.1% and 78.3%, at a cut-off value of 20 ng/mL, respectively[31]. They added that when AFP and another tumor maker, protein induced by vitamin K absence or antagonist II (PIVKA-II), were combined with cut-off values of 40 ng/mL for AFP and 80 mAU/mL for PIVKA-II, sensitivity was 65.5% and specificity was 85.5%. The study by Tong et al showed that the positive predictive value for AFP to detect HCC was only 12% or less for all AFP cut-off values, and the maximum joint sensitivity and specificity as determined by receiver operator characteristic (ROC) analysis were approximately 65% and 90%, respectively. Meanwhile, the positive predictive value for US to detect HCC was 78%, while sensitivity and specificity were 100% and 98%, respectively[33]. They concluded that AFP should not be used as the only test for screening and surveillance for HCC because of its poor predictive value and low sensitivity. Larcos et al also mentioned that US screening was superior to AFP assay for detection of HCC[34]. Novel serum markers with improved sensitivity are awaited for screening tests for HCC.
US is the most common method for the screening of HCC because of its advantages - simple, non-invasive and real-time observation[4,5]. However, there has been a variety of results in the application of US for HCC surveillance (Table 1). Sherman et al reported that US showed a sensitivity of 71.4%, a specificity of 93.8%, with only 14% of positive predictive value, as a screening test in chronic HBsAg carriers[35]. Chalasani et al compared the sensitivity in a screening program between US and computed tomography (CT), and the sensitivity of US (59%) was much lower than that of CT (91%)[36]. Two other studies in the diagnosis of HCC before liver transplantation resulted in similar sensitivity between US and CT, 79.4% for US and 81.6% for CT[37], 58% for US and 53% for CT[38], respectively, with the latter claiming that US is preferable to CT for routine screening of HCC before liver transplantation because of its lower cost. Meanwhile, Teefey et al mentioned that the sensitivity of US (89%) was much higher than CT (67%) and magnetic resonance imaging (MRI, 56%)[39]. Evaluation of the actual sensitivity of US and other imaging techniques from the published studies on screening and surveillance is quite difficult because of the lack of a defined gold standard, as was also noted in the review article by Bolondi[28]. In addition, Chalasani et al described in their study that the lesser steatosis to change liver echogenecity in Asian patients with predominantly viral cirrhosis, leaner body habitus in Japanese patients resulting in better visualization of the liver by US, and differences in US technique between physicians (Japan) and technologists (USA) were the causes for the high detection rates by US in Japanese reports[4,36,40]. Although it is natural that US results depend on the physical size of the patients and the operator’s skill, medical staffs and engineers who engage in US should not accept the current situation. Further technical and technological improvements are required to overcome these problems.
Table 1.
Sensitivity and specificity of US and other imaging modalities for the screening of HCC
| Authors |
US |
Other modalities |
||
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |
| Sherman et al[35] | 71.4 | 93.8 | - | - |
| Chalasani et al[36] | 59 | 93 | 91 (CT) | 96 (CT) |
| 1Yao et al[37] | 79.4 | - | 81.6 (CT) | - |
| 88.9 (MRI) | - | |||
| Gambarin-Gelwan et al[38] | 58 | 94 | 53 (CT) | 94 (CT) |
| 2Teefey et al[39] | 89 | 75 | 67 (CT) | 75 (CT) |
| 56 (MRI) | 81 (MRI) | |||
| 0 (PET) | 88 (PET) | |||
Sensitivity of radiologic procedures in the diagnosis and staging of known HCC before liver transplantation.
The higher value was presented from two data obtained between two observers.
Tumor detectability between US without enhancement and contrast-enhanced spiral CT has been compared in some previous studies. The comparison may not be on an equal footing, as US has now acquired collaboration with microbubble contrast agents. The application of contrast-enhanced CT for screening of HCC would be expensive and invasive, and MRI has the limitation of a low availability rate of the equipment. Although contrast-enhanced US may not be cheap, it is much less invasive and more convenient than contrast-enhanced CT. The establishment of surveillance based on both non-contrast US and contrast-enhanced US may be necessary for the screening procedure of HCC.
According to clinical studies concerning the doubling time of tumor, median days were reported as 117 d (29-398 d) by Sheu et al[27] or 171.6 d (27.2-605.6 d) by Barbara et al[41], and the former study called for a suitable screening interval for the early detection of HCC of 4-5 mo. Solmi et al reported that the percentage of detected unifocal tumors with a diameter less than or equal to 3 cm was significantly higher in the group followed-up every six months by both US and AFP than the group without this follow-up protocol[42]. Depending on the risk factors, a score based on certain clinical findings may be predictive for the doubling time of HCC[41,43]. The latter report recommended a regular US follow-up of a 3- or 6-mo interval according to the risk of HCC development, sex (male), alkaline phosphatase, AFP, γ-glutamyltransferase and albumin[43]. The study by Izzo et al also supported the 6-month surveillance by AFP and US for patients with severe chronic active hepatitis or liver cirrhosis[44]. However, Fasani et al reported that screening with US every six months may be inadequate for early detection of liver cancer in patients with multiple risk factors because multinodular HCC was under detected by US[45]. A tailor-made surveillance interval may be required according to the risk of HCC development.
Bolondi et al examined their surveillance program based on US and AFP at six-month intervals in 313 cirrhotic patients, reporting that the cumulative survival of the 61 patients with liver tumors detected by the surveillance program was significantly longer than that of controls not participating in any specific surveillance program, with incidentally detected HCC, and multivariate analysis showed an association between surveillance and survival[46]. Other studies showed that surveillance based on US and AFP every 6-12 mo improved the survival of patients[47,48].
As described above, the method and appropriate interval of surveillance have been discussed from the aspect of growth speed of HCC, detected number and size of HCC, and the risk of developing HCC. Furthermore, the significance of surveillance is well-supported by the improved survival rate. US should play a main role in the screening procedure of HCC.
DIAGNOSIS OF HCC
Imaging diagnosis of HCC is based on the presentation of characteristic hypervascular appearances in nodules. The European Association for the Study of the Liver (EASL) has documented the diagnostic criteria for HCC in a report for the clinical management of HCC[49]. Nodules larger than 2 cm with an arterial hypervascular pattern by two imaging techniques or by one imaging technique associated with an AFP level higher than 400 ng/mL was considered to be HCC in cirrhotic patients without needing confirmation by a positive biopsy. Four imaging modalities, US, spiral CT, MRI, and angiography, were recommended for evaluation of the vascularity of hepatic nodules in that article.
The advantages of US imaging consist of the simple and non-invasive demonstration of blood flow by real-time observation. US is a unique method that can evaluate blood flow direction under physiological condition. In contrast to focal nodular hyperplasia (FNH) with a centrifugal blood flow appearance (Figure 1), HCC has a characteristic hypervascular appearance with centripetal blood flow, and a basket pattern is one of the typical findings of HCC by color Doppler imaging[50–52]. The clinical application of microbubble contrast agents has resulted in remarkable improvement in blood flow detection by US examination. It was reported that the same enhancement pattern was found between contrast-enhanced harmonic grey-scale imaging with Levovist and contrast-enhanced helical CT in 53 of 61 (87%) HCC nodules[53]. Other studies have also shown over 80% concordance of tumor vascularity[54,55] between contrast-enhanced US with SonoVue (Bracco Diagnostics, Princeton, NJ, USA) and contrast-enhanced helical CT. Thus, the application of Doppler mode alone for detecting tumor blood flow is rare, as the more recent availability of microbubble contrast agents has assisted in overcoming the limitations of Doppler methods.
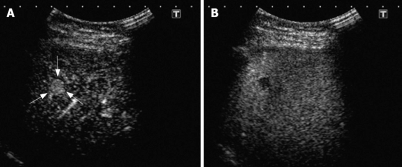
Figure 1.

Contrast-enhanced harmonic imaging with Sonazoid in focal nodular hyperplasia (FNH). The centrifugal blood flow appearance like “spoke-wheel sign” was clearly demonstrated in the center of the nodules (arrows).
The diagnostic performance of contrast-enhanced US is not limited to the demonstration of tumor vascularity. Some microbubble contrast agents have a characteristic property of organ-specific accumulation[56–59]. Although the precise mechanism remains unclear, the reticuloendothelial system (i.e., phagocytosis by Kupffer cells) may be involved in this phenomenon. Both Levovist and Sonazoid (Nycomed-Amersham, Oslo, Norway) accumulate in the liver, and sonograms in this phase (late liver-specific parenchymal phase) are frequently used for the detection or characterization of liver tumors. In contrast, Definity (Bristol-Myers Squibb, N. Billerica, MA, USA) and SonoVue do not accumulate in the liver. The characterization of liver tumors by contrast-enhanced US has been carried out using accumulation images as well as vascular enhancement images (Figure 2A and B).
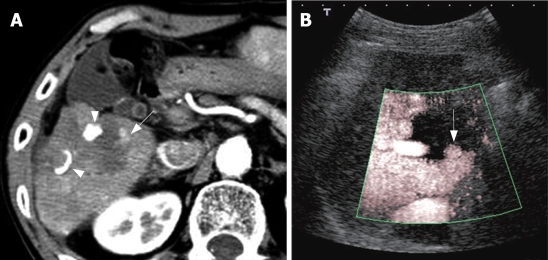
Figure 2.
Contrast-enhanced harmonic imaging with Sonazoid in small HCC (9.8 mm, arrows). A: Early-phase image (22 s after the injection); B: Late-phase image (10 min after the injection). The early-phase image showed positive enhancement and the late-phase image showed negative enhancement in the nodule. These findings could easily diagnose this lesion as HCC.
Concerning the discrimination of malignant versus benign liver lesions by contrast-enhanced US, recent literature has reported sensitivity of 98% to 100% and specificity of 63% to 93% with Levovist[60–63], and sensitivity of 98% and accuracy of 92.7% with SonoVue[64]. Furthermore, in a clinical study with two independent image reviewers, Kim et al[65] described that contrast-enhanced US (agent detecting imaging mode with Levovist) provided a specific diagnosis in 75%-79% of 75 patients with focal hepatic lesions, and that the technique was successful as a confirmatory imaging technique in 63%-72% of the patients.
Hypervascular hepatic lesions do not always reflect the fact that the final diagnosis of the nodule is HCC in heavy drinkers[66], since benign hypervascular nodules sometimes occur in their liver. A recent report has shown that the ring-shaped appearance on liver-specific contrast-enhanced sonograms with Levovist may be a useful sign for the differential diagnosis of benign nodule from HCC in heavy drinkers[67]. Since contrast-enhanced CT hardly differentiates these benign nodules from HCC, this characteristic finding may prevent unnecessary treatments under misdiagnosis. Moreover, it could be expected to lead to a reduction in the application of percutaneous needle biopsy, an invasive procedure, for the precise diagnosis.
Non-hypervascular and/or small (< 2 cm) nodules
Well-differentiated HCC, dysplastic nodule (DN) and regenerative nodule (RN) do not always reveal the specific hypervascular pattern on contrast-enhanced CT such as typical HCC[68–71]. The characterization of such non-hypervascular nodules is very important in clinical practice[72,73] because high-grade DN are considered potentially pre-malignant lesions. However, as these non-hypervascular nodules have Kupffer cell distribution[74,75], observation of the superparamagnetic iron oxide-enhanced (SPIO) MR images or liver-specific images on contrast-enhanced US could not easily characterize them.
According to the EASL report, percutaneous needle biopsy has until now been a standard method for the diagnosis of non-hypervascular hepatic nodules or small hepatic nodules of 1 cm to 2 cm[49], because characterization of these nodules by imaging modalities alone is difficult[76–79]. As for nodules smaller than 1 cm, EASL recommended repeated US observation every 3 mo until the lesion grows to 1 cm, at which point additional diagnostic techniques can be applied[49].
Thanks to the establishment of US-guided needle puncture technique[80], percutaneous needle biopsy has a quite high diagnostic accuracy. Caturelli et al found that the typing accuracy of fine-needle aspiration biopsy was 88.6% for nodules with diameters < 10 mm, 86.2% for nodules with diameters of 11-15 mm, and 91.3% for nodules with diameters of 16-20 mm[81]. Durand et al reported that US-guided FNB diagnosed HCC nodules with a sensitivity of 91%[82]. However, liver biopsy for small nodules always has the possibility of sampling error, and a negative biopsy of a nodule visible with imaging techniques in a cirrhotic liver can never be taken as a criterion to rule out malignancy[83]. Additionally, as rapid progression is rare in these kinds of nodules, repeated observations in their clinical course would determine their management. Therefore contrast-enhanced US can be expected to be an effective diagnostic tool for these non-hypervascular lesions because of its high resolution and non-invasive procedure.
TREATMENT SUPPORT AND EVALUATION OF THERAPEUTIC EFFECT
US-guided treatment
Since the majority of HCC patients have poor liver function and recurrence is not rare, surgical treatment is not always an appropriate choice[2,3,49]. With such backgrounds, percutaneous ethanol injection (PEI)[84–86] and radio-frequency ablation (RFA)[87,88] were developed and came to be widely used in clinical practice as minimally invasive methods[89]. They are now a first-line, favored approach with an efficient therapeutic effect on HCC[90–93].
Treatment for recurrent lesions
Although percutaneous US-guided treatments provide sufficient therapeutic effect, recurrence often plagues many HCC patients. According to long-term study results, cumulative recurrence rates of the treated site of post-PEI lesions were 3.4% at 1 year, 7.1% at 2 years, and 10% at 3 years, and those of the untreated sites in liver were 18.7% at 1 year, 62.1% at 3 years, and 81.7% at 5 years, respectively[94]. Thus, many HCC patients have to receive repeated treatments during their clinical course. In order to minimize adverse effects to the liver, less invasive treatment such as PEI or RFA is preferable for these patients. However, localization of lesions on sonograms is sometimes problematic in patients with cirrhotic liver and/or repeated treatment history[95,96]. Although percutaneous treatment under CT guidance is a well-established technique and a useful method for lesions undetected by US, the method lacks convenience and exposes both patients and physicians to radiation[97–100]. Microbubble contrast agents are also useful in such a case. A recent study showed that contrast-enhanced US with Levovist could localize 24/32 (75%) of HCC lesions that were invisible by non-contrast US[101]. Application of the next-generation US contrast agents, SonoVue and Sonazoid, is expected to improve the localization result.
Evaluation of therapeutic effect
US examination is eligible for the evaluation of the therapeutic effect after percutaneous treatments such as PEI and RFA, because they are usually performed under US guidance. In fact, contrast-enhanced US has come to be frequently applied for evaluation of the therapeutic response in HCC nodules with improved sensitivity and specificity for detecting tumor blood flow (Table 2). According to the results by Bartolozzi et al, color Doppler US with Levovist showed sensitivity of 92%, specificity of 100%, and accuracy of 98% compared to the results of spiral CT and biopsy, in the detection of residual tumor tissue in 47 HCC lesions after PEI[102]. Wen et al examined the efficacy of coded harmonic angio mode with Levovist for detecting residual tumor in 91 HCC nodules about one week after RFA in comparison with contrast-enhanced CT, and they found that sensitivity, specificity, and diagnostic accuracy of US were 95.3%, 100%, and 98.1%, respectively[103]. Meloni et al reported that sensitivity and specificity of pulse inversion harmonic imaging with Levovist were 83.3% and 100%, respectively, for detecting residual non-ablated tumor at 4 mo after treatment in 35 patients with 43 HCC nodules, compared with helical CT findings[104]. Immediate evaluation of the therapeutic effect is often desirable after RFA for the management of HCC, and Choi et al mentioned that diagnostic agreement between power Doppler with Levovist about half or one day after ablation therapy and CT just after ablation was achieved in 100% of the 45 HCC nodules in 40 patients[105]. Another study showed that diagnostic concordance between agent detection imaging with Levovist performed within 24 h after RFA and 1-mo follow-up CT was 99% in 90 patients with 97 HCC nodules[106]. Thus, estimation of the therapeutic response in HCC after percutaneous treatments would become more efficient on the basis of this non-invasive imaging method. Although artificial signals caused by the RFA procedure affect an early detailed observation[105–107], monitoring by contrast-enhanced US during RFA would likely be applied to the assessment of the therapeutic effect as well as the detection of viable tumor.
Table 2.
Assessment of therapeutic response after percutaneous treatment for HCC using contrast-enhanced US
| Author | Treatment | No. of patients/No. of lesions | Results1 (contrast agent) |
| Bartolozzi et al[102] | PEI | 40/47 | Sensitivity 92% |
| Specificity 100% | |||
| Accuracy 98% | |||
| (Levovist) | |||
| Wen et al[103] | RFA | 67/91 | Sensitivity 95.30% |
| Specificity 100% | |||
| Accuracy 98.10% | |||
| (Levovist) | |||
| Meloni et al[104] | RFA | 25/43 | Sensitivity 83.30% |
| Specificity 100% | |||
| (Levovist) | |||
| Choi et al[105] | RFA | 40/45 | Diagnostic agreement 100% |
| (Levovist) | |||
| Kim et al[106] | RFA | 90/94 | Diagnostic concordace2 99% |
| (Levovist) | |||
| Solbiati et al[107] | RFA | 20/203 | Sensitivity 50% |
| Specificity 100% | |||
| Diagnostic agreement 85% | |||
| (Levovist) | |||
| Pompili et al[110] | PEI, RFA, TACE | 47/56 | Sensitivity 87% |
| Combined treatments | Specificity 98.40% | ||
| Diagnostic agreement 94.60% | |||
| (SonoVue) |
Comparison with contrast-enhanced helical CT;
1-mo follow-up CT;
Solitary colorectal liver metastases.
It is well known that contrast-enhanced CT can hardly evaluate intratumoral contrast enhancement when partial retention of iodized oil is present in the tumor after transcatheter arterial chemoembolization (TACE). Therefore, the therapeutic effect of TACE is usually assessed by the distribution of iodized oil in the tumor on non-contrast CT images, though these findings are an indirect presentation. As MRI findings are not affected by the presence of iodized oil, contrast-enhanced MRI is favorable for the assessment of the therapeutic effect after TACE. However, the equipment has not yet come into wide-spread use, the procedure is not convenient, and evaluation of the findings in small lesions is sometimes difficult due to the low resolution and influence of motion artifacts. Contrast-enhanced US has the advantage of not being limited by iodized oil deposition that affects the evaluation of contrast-enhanced CT findings. Some clinical studies have shown the magnitude of contrast-enhanced US for evaluation of the therapeutic effect after TACE[108,109]. According to the report by Pompili et al, contrast-enhanced US with SonoVue resulted in diagnostic agreement in 53/56 cases (94.6%), with 87.0% sensitivity and 98.4% specificity compared with contrast-enhanced CT findings, after non-surgical treatments for HCC[110]. Another study showed that contrast-enhanced US resulted in considerably higher sensitivity in detecting residual tumor blood flow after TACE than dynamic CT or dynamic MRI[111]. Meanwhile, Lim et al described that a reliable assessment of intratumoral blood flow by contrast-enhanced US may not be possible in many instances, particularly in small lesions or in lesions located deep within the liver parenchyma[112]. They concluded that CT is the standard imaging technique for monitoring the effectiveness of TACE and RFA, and contrast-enhanced US and MRI can complement CT in evaluating the therapeutic response. Although the performance of the US examination may depend on the operator’s skill, location of the tumor and system capability, quite a few radiologists and hepatologists may believe that contrast-enhanced US plays a major role in evaluation of the therapeutic effect after TACE. The recent developments in this technology would allow contrast-enhanced US to be positioned as the standard method for evaluation of the therapeutic effect in many HCC patients (Figure 3A and B).
Figure 3.
Assessment of therapeutic response after PEI for HCC. A: Contrast-enhanced CT with dynamic study; B: Contrast-enhanced US (Advanced Dynamic Flow with Levovist). Contrast-enhanced CT showed enhancement appearance which needed additional treatment within the treated area (arrow), and contrast-enhanced US could demonstrate a similar finding. Arrow heads: Lipiodol.
ADVANCED TECHNOLOGY
Recent US systems have provided three-dimensional visualization of the combined tissue structures and color blood-flow appearance under easy handling[24,25]. Additional anatomical information of the tumor with tumor-associated vessels is available at any plane from multiple directions[113–116]. With the remarkable progress in microelectronic technology, the US transducer has achieved full digital specification (Matrix transducer, iu22, Philips) with 3000 elements[117,118]. Including built-in micro-beamforming composed of a 150-computer board, it can visualize “Live 3D”, which presents real-time three-dimensional anatomical views visible from any angle with volume rendering for pyramidal volume (90*70 angles). Contrast-enhanced 3D or 4D ultrasonographies using microbubble contrast agents might become a standard method for the characterization and/or evaluation of the therapeutic effect on liver tumors (Figure 4)[119].
Figure 4.
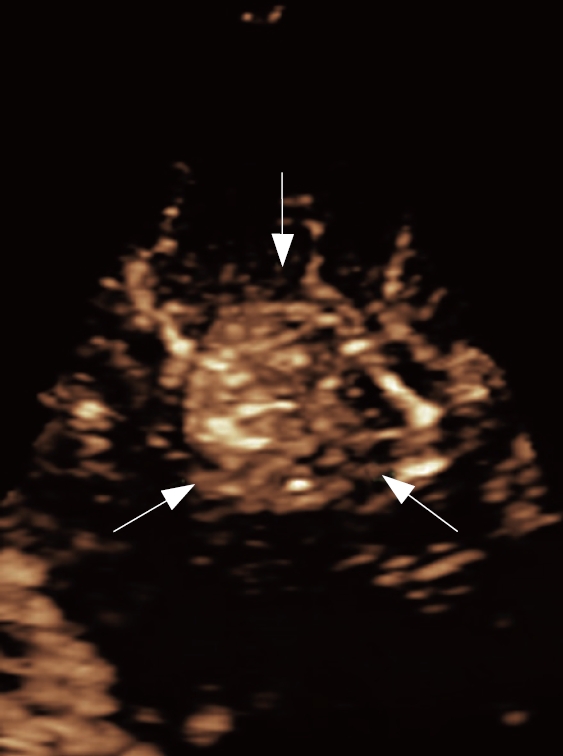
Real-time three-dimensional imaging of HCC (contrast-enhanced LIVE 3D with Sonazoid, iu22, Philips). Abundant tumor vessels were dramatically demonstrated in the HCC nodule. (Arrows: HCC nodule).
HIFU is a novel technology that enables transcutaneous ablation effect without needle puncture[120,121]. While controlling the energy and focusing of US, successful HIFU results in necrosis of the tumor in the focal area with less damage of surrounding tissues. A number of clinical studies have been carried out using HIFU for the treatment of liver tumors as well as breast cancer and myoma uteri. In regard to liver tumors, it was reported that the anti-tumor effect and survival time by HIFU combined with TACE were superior to those by TACE alone in 50 patients with advanced HCC[122]. Although some of the subjects seemed to have a complete ablation effect, the precise effect for complete tumor necrosis by HIFU was not clear in this study. Furthermore, as the background of the HCCs showing sufficient ablation effect was not fully analyzed, it remains to be solved whether HIFU is valuable as a reliable method for curative treatment of small HCC. Nonetheless, this non-invasive method is really expected to be used for HCC treatment, as an alternative to PEI or RFA, because needle puncture is an invasive procedure for cirrhotic patients.
Normal ventilation is one of the serious problems in the completion of HIFU treatment for liver tumor, as movement of the liver may cause ablation failure that results on non-tumor tissue damage and/or incomplete therapeutic effect for the tumor. Wu et al reported that three-dimensional US images were used as a monitor to localize the tumor during HIFU treatment, and changes in echogenicity of the tumor just after the treatment were evaluated by US[122]. Advances in imaging technology for real-time 3D sonography would help the improvement of the therapeutic ability of HIFU.
In conclusion, US has made amazing strides in the last decades because of digital technology progress, and it will continue to grow. The advancement of imaging methods is expected to support the clinical management of patients with HCC.
Peer reviewers: Serdar Karakose, Dr, Professor, Department of Radiology, Meram Medical Faculty, Selcuk University, Konya 42080, Turkey; Manuel Romero-Gómez, MD, Professor, Hepatology Unit, Hospital Universitario de Valme, Ctra de Cádiz s/n, Sevilla 41014, Spain
S- Editor Liu Y L- Editor Alpini GD E- Editor Lu W
References
- 1.Bosch FX, Ribes J, Borras J. Epidemiology of primary liver cancer. Semin Liver Dis. 1999;19:271–285. doi: 10.1055/s-2007-1007117. [DOI] [PubMed] [Google Scholar]
- 2.Okuda K. Hepatocellular carcinoma: recent progress. Hepatology. 1992;15:948–963. doi: 10.1002/hep.1840150532. [DOI] [PubMed] [Google Scholar]
- 3.Okuda K. Hepatocellular carcinoma. J Hepatol. 2000;32:225–237. doi: 10.1016/s0168-8278(00)80428-6. [DOI] [PubMed] [Google Scholar]
- 4.Oka H, Kurioka N, Kim K, Kanno T, Kuroki T, Mizoguchi Y, Kobayashi K. Prospective study of early detection of hepatocellular carcinoma in patients with cirrhosis. Hepatology. 1990;12:680–687. doi: 10.1002/hep.1840120411. [DOI] [PubMed] [Google Scholar]
- 5.Takayasu K, Moriyama N, Muramatsu Y, Makuuchi M, Hasegawa H, Okazaki N, Hirohashi S. The diagnosis of small hepatocellular carcinomas: efficacy of various imaging procedures in 100 patients. AJR Am J Roentgenol. 1990;155:49–54. doi: 10.2214/ajr.155.1.1693808. [DOI] [PubMed] [Google Scholar]
- 6.Kremkau FW. Diagnostic ultrasound: Principles and Instruments. 4th edition. Vol. 155. Philadelphia: WB Saunders; 1993. [Google Scholar]
- 7.Harvey CJ, Albrecht T. Ultrasound of focal liver lesions. Eur Radiol. 2001;11:1578–1593. doi: 10.1007/s003300101002. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro RS, Wagreich J, Parsons RB, Stancato-Pasik A, Yeh HC, Lao R. Tissue harmonic imaging sonography: evaluation of image quality compared with conventional sonography. AJR Am J Roentgenol. 1998;171:1203–1206. doi: 10.2214/ajr.171.5.9798848. [DOI] [PubMed] [Google Scholar]
- 9.Hann LE, Bach AM, Cramer LD, Siegel D, Yoo HH, Garcia R. Hepatic sonography: comparison of tissue harmonic and standard sonography techniques. AJR Am J Roentgenol. 1999;173:201–206. doi: 10.2214/ajr.173.1.10397127. [DOI] [PubMed] [Google Scholar]
- 10.Whittingham TA. Tissue harmonic imaging. Eur Radiol. 1999;9 Suppl 3:S323–S326. doi: 10.1007/pl00014065. [DOI] [PubMed] [Google Scholar]
- 11.Taylor KJ, Ramos I, Morse SS, Fortune KL, Hammers L, Taylor CR. Focal liver masses: differential diagnosis with pulsed Doppler US. Radiology. 1987;164:643–647. doi: 10.1148/radiology.164.3.3039570. [DOI] [PubMed] [Google Scholar]
- 12.Nino-Murcia M, Ralls PW, Jeffrey RB Jr, Johnson M. Color flow Doppler characterization of focal hepatic lesions. AJR Am J Roentgenol. 1992;159:1195–1197. doi: 10.2214/ajr.159.6.1332456. [DOI] [PubMed] [Google Scholar]
- 13.Choi BI, Kim TK, Han JK, Chung JW, Park JH, Han MC. Power versus conventional color Doppler sonography: comparison in the depiction of vasculature in liver tumors. Radiology. 1996;200:55–58. doi: 10.1148/radiology.200.1.8657945. [DOI] [PubMed] [Google Scholar]
- 14.Lencioni R, Pinto F, Armillotta N, Bartolozzi C. Assessment of tumor vascularity in hepatocellular carcinoma: comparison of power Doppler US and color Doppler US. Radiology. 1996;201:353–358. doi: 10.1148/radiology.201.2.8888222. [DOI] [PubMed] [Google Scholar]
- 15.Gaiani S, Volpe L, Piscaglia F, Bolondi L. Vascularity of liver tumours and recent advances in doppler ultrasound. J Hepatol. 2001;34:474–482. doi: 10.1016/s0168-8278(01)00021-6. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell DG. Color Doppler imaging: principles, limitations, and artifacts. Radiology. 1990;177:1–10. doi: 10.1148/radiology.177.1.2204956. [DOI] [PubMed] [Google Scholar]
- 17.Foley WD, Erickson SJ. Color Doppler flow imaging. AJR Am J Roentgenol. 1991;156:3–13. doi: 10.2214/ajr.156.1.1898567. [DOI] [PubMed] [Google Scholar]
- 18.Rubin JM, Bude RO, Carson PL, Bree RL, Adler RS. Power Doppler US: a potentially useful alternative to mean frequency-based color Doppler US. Radiology. 1994;190:853–856. doi: 10.1148/radiology.190.3.8115639. [DOI] [PubMed] [Google Scholar]
- 19.Gramiak R, Shah PM. Echocardiography of the normal and diseased aortic valve. Radiology. 1970;96:1–8. doi: 10.1148/96.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Matsuda Y, Yabuuchi I. Hepatic tumors: US contrast enhancement with CO2 microbubbles. Radiology. 1986;161:701–705. doi: 10.1148/radiology.161.3.3024206. [DOI] [PubMed] [Google Scholar]
- 21.Kudo M, Tomita S, Tochio H, Mimura J, Okabe Y, Kashida H, Hirasa M, Ibuki Y, Todo A. Small hepatocellular carcinoma: diagnosis with US angiography with intraarterial CO2 microbubbles. Radiology. 1992;182:155–160. doi: 10.1148/radiology.182.1.1309216. [DOI] [PubMed] [Google Scholar]
- 22.Schlief R, Staks T, Mahler M, Rufer M, Fritzsch T, Seifert W. Successful opacification of the left heart chambers on echocardiographic examination after intravenous injection of a new saccharide based contrast agent. Echocardiography. 1990;7:61–64. doi: 10.1111/j.1540-8175.1990.tb00349.x. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg BB. Ultrasound contrast agents. London: Martin Dunitz Ltd; 1997. p. 169. [Google Scholar]
- 24.Nelson TR, Pretorius DH. Three-dimensional ultrasound imaging. Ultrasound Med Biol. 1998;24:1243–1270. doi: 10.1016/s0301-5629(98)00043-x. [DOI] [PubMed] [Google Scholar]
- 25.Downey DB, Fenster A, Williams JC. Clinical utility of three-dimensional US. Radiographics. 2000;20:559–571. doi: 10.1148/radiographics.20.2.g00mc19559. [DOI] [PubMed] [Google Scholar]
- 26.Kennedy JE, Ter Haar GR, Cranston D. High intensity focused ultrasound: surgery of the future? Br J Radiol. 2003;76:590–599. doi: 10.1259/bjr/17150274. [DOI] [PubMed] [Google Scholar]
- 27.Sheu JC, Sung JL, Chen DS, Yang PM, Lai MY, Lee CS, Hsu HC, Chuang CN, Yang PC, Wang TH. Growth rate of asymptomatic hepatocellular carcinoma and its clinical implications. Gastroenterology. 1985;89:259–266. doi: 10.1016/0016-5085(85)90324-5. [DOI] [PubMed] [Google Scholar]
- 28.Bolondi L. Screening for hepatocellular carcinoma in cirrhosis. J Hepatol. 2003;39:1076–1084. doi: 10.1016/s0168-8278(03)00349-0. [DOI] [PubMed] [Google Scholar]
- 29.Collier J, Sherman M. Screening for hepatocellular carcinoma. Hepatology. 1998;27:273–278. doi: 10.1002/hep.510270140. [DOI] [PubMed] [Google Scholar]
- 30.Sato Y, Nakata K, Kato Y, Shima M, Ishii N, Koji T, Taketa K, Endo Y, Nagataki S. Early recognition of hepatocellular carcinoma based on altered profiles of alpha-fetoprotein. N Engl J Med. 1993;328:1802–1806. doi: 10.1056/NEJM199306243282502. [DOI] [PubMed] [Google Scholar]
- 31.Izzo F, Cremona F, Delrio P, Leonardi E, Castello G, Pignata S, Daniele B, Curley SA. Soluble interleukin-2 receptor levels in hepatocellular cancer: a more sensitive marker than alfa fetoprotein. Ann Surg Oncol. 1999;6:178–185. doi: 10.1007/s10434-999-0178-1. [DOI] [PubMed] [Google Scholar]
- 32.Ishii M, Gama H, Chida N, Ueno Y, Shinzawa H, Takagi T, Toyota T, Takahashi T, Kasukawa R. Simultaneous measurements of serum alpha-fetoprotein and protein induced by vitamin K absence for detecting hepatocellular carcinoma. South Tohoku District Study Group. Am J Gastroenterol. 2000;95:1036–1040. doi: 10.1111/j.1572-0241.2000.01978.x. [DOI] [PubMed] [Google Scholar]
- 33.Tong MJ, Blatt LM, Kao VW. Surveillance for hepatocellular carcinoma in patients with chronic viral hepatitis in the United States of America. J Gastroenterol Hepatol. 2001;16:553–559. doi: 10.1046/j.1440-1746.2001.02470.x. [DOI] [PubMed] [Google Scholar]
- 34.Larcos G, Sorokopud H, Berry G, Farrell GC. Sonographic screening for hepatocellular carcinoma in patients with chronic hepatitis or cirrhosis: an evaluation. AJR Am J Roentgenol. 1998;171:433–435. doi: 10.2214/ajr.171.2.9694470. [DOI] [PubMed] [Google Scholar]
- 35.Sherman M, Peltekian KM, Lee C. Screening for hepatocellular carcinoma in chronic carriers of hepatitis B virus: incidence and prevalence of hepatocellular carcinoma in a North American urban population. Hepatology. 1995;22:432–438. [PubMed] [Google Scholar]
- 36.Chalasani N, Horlander JC Sr, Said A, Hoen H, Kopecky KK, Stockberger SM Jr, Manam R, Kwo PY, Lumeng L. Screening for hepatocellular carcinoma in patients with advanced cirrhosis. Am J Gastroenterol. 1999;94:2988–2993. doi: 10.1111/j.1572-0241.1999.01448.x. [DOI] [PubMed] [Google Scholar]
- 37.Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33:1394–1403. doi: 10.1053/jhep.2001.24563. [DOI] [PubMed] [Google Scholar]
- 38.Gambarin-Gelwan M, Wolf DC, Shapiro R, Schwartz ME, Min AD. Sensitivity of commonly available screening tests in detecting hepatocellular carcinoma in cirrhotic patients undergoing liver transplantation. Am J Gastroenterol. 2000;95:1535–1538. doi: 10.1111/j.1572-0241.2000.02091.x. [DOI] [PubMed] [Google Scholar]
- 39.Teefey SA, Hildeboldt CC, Dehdashti F, Siegel BA, Peters MG, Heiken JP, Brown JJ, McFarland EG, Middleton WD, Balfe DM, et al. Detection of primary hepatic malignancy in liver transplant candidates: prospective comparison of CT, MR imaging, US, and PET. Radiology. 2003;226:533–542. doi: 10.1148/radiol.2262011980. [DOI] [PubMed] [Google Scholar]
- 40.Tanaka S, Kitamura T, Nakanishi K, Okuda S, Yamazaki H, Hiyama T, Fujimoto I. Effectiveness of periodic checkup by ultrasonography for the early diagnosis of hepatocellular carcinoma. Cancer. 1990;66:2210–2214. doi: 10.1002/1097-0142(19901115)66:10<2210::aid-cncr2820661028>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 41.Barbara L, Benzi G, Gaiani S, Fusconi F, Zironi G, Siringo S, Rigamonti A, Barbara C, Grigioni W, Mazziotti A. Natural history of small untreated hepatocellular carcinoma in cirrhosis: a multivariate analysis of prognostic factors of tumor growth rate and patient survival. Hepatology. 1992;16:132–137. doi: 10.1002/hep.1840160122. [DOI] [PubMed] [Google Scholar]
- 42.Solmi L, Primerano AM, Gandolfi L. Ultrasound follow-up of patients at risk for hepatocellular carcinoma: results of a prospective study on 360 cases. Am J Gastroenterol. 1996;91:1189–1194. [PubMed] [Google Scholar]
- 43.Zoli M, Magalotti D, Bianchi G, Gueli C, Marchesini G, Pisi E. Efficacy of a surveillance program for early detection of hepatocellular carcinoma. Cancer. 1996;78:977–985. doi: 10.1002/(SICI)1097-0142(19960901)78:5<977::AID-CNCR6>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 44.Izzo F, Cremona F, Ruffolo F, Palaia R, Parisi V, Curley SA. Outcome of 67 patients with hepatocellular cancer detected during screening of 1125 patients with chronic hepatitis. Ann Surg. 1998;227:513–518. doi: 10.1097/00000658-199804000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fasani P, Sangiovanni A, De Fazio C, Borzio M, Bruno S, Ronchi G, Del Ninno E, Colombo M. High prevalence of multinodular hepatocellular carcinoma in patients with cirrhosis attributable to multiple risk factors. Hepatology. 1999;29:1704–1707. doi: 10.1002/hep.510290604. [DOI] [PubMed] [Google Scholar]
- 46.Bolondi L, Sofia S, Siringo S, Gaiani S, Casali A, Zironi G, Piscaglia F, Gramantieri L, Zanetti M, Sherman M. Surveillance programme of cirrhotic patients for early diagnosis and treatment of hepatocellular carcinoma: a cost effectiveness analysis. Gut. 2001;48:251–259. doi: 10.1136/gut.48.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sangiovanni A, Del Ninno E, Fasani P, De Fazio C, Ronchi G, Romeo R, Morabito A, De Franchis R, Colombo M. Increased survival of cirrhotic patients with a hepatocellular carcinoma detected during surveillance. Gastroenterology. 2004;126:1005–1014. doi: 10.1053/j.gastro.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 48.Trevisani F, Cantarini MC, Labate AM, De Notariis S, Rapaccini G, Farinati F, Del Poggio P, Di Nolfo MA, Benvegnu L, Zoli M, et al. Surveillance for hepatocellular carcinoma in elderly Italian patients with cirrhosis: effects on cancer staging and patient survival. Am J Gastroenterol. 2004;99:1470–1476. doi: 10.1111/j.1572-0241.2004.30137.x. [DOI] [PubMed] [Google Scholar]
- 49.Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M, Rodes J. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421–430. doi: 10.1016/s0168-8278(01)00130-1. [DOI] [PubMed] [Google Scholar]
- 50.Tanaka S, Kitamura T, Fujita M, Nakanishi K, Okuda S. Color Doppler flow imaging of liver tumors. AJR Am J Roentgenol. 1990;154:509–514. doi: 10.2214/ajr.154.3.2154912. [DOI] [PubMed] [Google Scholar]
- 51.Kudo M, Tomita S, Tochio H, Kashida H, Hirasa M, Todo A. Hepatic focal nodular hyperplasia: specific findings at dynamic contrast-enhanced US with carbon dioxide microbubbles. Radiology. 1991;179:377–382. doi: 10.1148/radiology.179.2.1849661. [DOI] [PubMed] [Google Scholar]
- 52.Golli M, Mathieu D, Anglade MC, Cherqui D, Vasile N, Rahmouni A. Focal nodular hyperplasia of the liver: value of color Doppler US in association with MR imaging. Radiology. 1993;187:113–117. doi: 10.1148/radiology.187.1.8451397. [DOI] [PubMed] [Google Scholar]
- 53.Numata K, Tanaka K, Kiba T, Saito S, Ikeda M, Hara K, Tanaka N, Morimoto M, Iwase S, Sekihara H. Contrast-enhanced, wide-band harmonic gray scale imaging of hepatocellular carcinoma: correlation with helical computed tomographic findings. J Ultrasound Med. 2001;20:89–98. doi: 10.7863/jum.2001.20.2.89. [DOI] [PubMed] [Google Scholar]
- 54.Giorgio A, Ferraioli G, Tarantino L, de Stefano G, Scala V, Scarano F, Coppola C, Del Viscovo L. Contrast-enhanced sonographic appearance of hepatocellular carcinoma in patients with cirrhosis: comparison with contrast-enhanced helical CT appearance. AJR Am J Roentgenol. 2004;183:1319–1326. doi: 10.2214/ajr.183.5.1831319. [DOI] [PubMed] [Google Scholar]
- 55.Bolondi L, Gaiani S, Celli N, Golfieri R, Grigioni WF, Leoni S, Venturi AM, Piscaglia F. Characterization of small nodules in cirrhosis by assessment of vascularity: the problem of hypovascular hepatocellular carcinoma. Hepatology. 2005;42:27–34. doi: 10.1002/hep.20728. [DOI] [PubMed] [Google Scholar]
- 56.Blomley M, Albrecht T, Cosgrove D, Jayaram V, Butler-Barnes J, Eckersley R. Stimulated acoustic emission in liver parenchyma with Levovist. Lancet. 1998;351:568. doi: 10.1016/S0140-6736(05)78554-8. [DOI] [PubMed] [Google Scholar]
- 57.Marelli C. Preliminary experience with NC100100, a new ultrasound contrast agent for intravenous injection. Eur Radiol. 1999;9 Suppl 3:S343–S346. doi: 10.1007/pl00014070. [DOI] [PubMed] [Google Scholar]
- 58.Morel DR, Schwieger I, Hohn L, Terrettaz J, Llull JB, Cornioley YA, Schneider M. Human pharmacokinetics and safety evaluation of SonoVue, a new contrast agent for ultrasound imaging. Invest Radiol. 2000;35:80–85. doi: 10.1097/00004424-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 59.Maruyama H, Matsutani S, Saisho H, Mine Y, Yuki H, Miyata K. Different behaviors of microbubbles in the liver: time-related quantitative analysis of two ultrasound contrast agents, Levovist and Definity. Ultrasound Med Biol. 2004;30:1035–1040. doi: 10.1016/j.ultrasmedbio.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 60.von Herbay A, Vogt C, Haussinger D. Late-phase pulse-inversion sonography using the contrast agent levovist: differentiation between benign and malignant focal lesions of the liver. AJR Am J Roentgenol. 2002;179:1273–1279. doi: 10.2214/ajr.179.5.1791273. [DOI] [PubMed] [Google Scholar]
- 61.Bryant TH, Blomley MJ, Albrecht T, Sidhu PS, Leen EL, Basilico R, Pilcher JM, Bushby LH, Hoffmann CW, Harvey CJ, et al. Improved characterization of liver lesions with liver-phase uptake of liver-specific microbubbles: prospective multicenter study. Radiology. 2004;232:799–809. doi: 10.1148/radiol.2323030596. [DOI] [PubMed] [Google Scholar]
- 62.Dietrich CF, Ignee A, Trojan J, Fellbaum C, Schuessler G. Improved characterisation of histologically proven liver tumours by contrast enhanced ultrasonography during the portal venous and specific late phase of SHU 508A. Gut. 2004;53:401–405. doi: 10.1136/gut.2003.026260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.von Herbay A, Vogt C, Willers R, Haussinger D. Real-time imaging with the sonographic contrast agent SonoVue: differentiation between benign and malignant hepatic lesions. J Ultrasound Med. 2004;23:1557–1568. doi: 10.7863/jum.2004.23.12.1557. [DOI] [PubMed] [Google Scholar]
- 64.Nicolau C, Vilana R, Catalá V, Bianchi L, Gilabert R, García A, Brú C. Importance of evaluating all vascular phases on contrast-enhanced sonography in the differentiation of benign from malignant focal liver lesions. AJR Am J Roentgenol. 2006;186:158–167. doi: 10.2214/AJR.04.1009. [DOI] [PubMed] [Google Scholar]
- 65.Kim SH, Lee JM, Lee JY, Han JK, An SK, Han CJ, Lee KH, Hwang SS, Choi BI. Value of contrast-enhanced sonography for the characterization of focal hepatic lesions in patients with diffuse liver disease: receiver operating characteristic analysis. AJR Am J Roentgenol. 2005;184:1077–1084. doi: 10.2214/ajr.184.4.01841077. [DOI] [PubMed] [Google Scholar]
- 66.Kim SR, Maekawa Y, Ninomiya T, Imoto S, Matsuoka T, Ando K, Mita K, Ku K, Koterazawa T, Nakajima T, et al. Multiple hypervascular liver nodules in a heavy drinker of alcohol. J Gastroenterol Hepatol. 2005;20:795–799. doi: 10.1111/j.1440-1746.2005.03244.x. [DOI] [PubMed] [Google Scholar]
- 67.Maruyama H, Matsutani S, Kondo F, Yoshizumi H, Kobayashi S, Okugawa H, Ebara M, Saisho H. Ring-shaped appearance in liver-specific image with Levovist: a characteristic enhancement pattern for hypervascular benign nodule in the liver of heavy drinkers. Liver Int. 2006;26:688–694. doi: 10.1111/j.1478-3231.2006.01286.x. [DOI] [PubMed] [Google Scholar]
- 68.Amano S, Ebara M, Yajima T, Fukuda H, Yoshikawa M, Sugiura N, Kato K, Kondo F, Matsumoto T, Saisho H. Assessment of cancer cell differentiation in small hepatocellular carcinoma by computed tomography and magnetic resonance imaging. J Gastroenterol Hepatol. 2003;18:273–279. doi: 10.1046/j.1440-1746.2003.02957.x. [DOI] [PubMed] [Google Scholar]
- 69.Sakabe K, Yamamoto T, Kubo S, Hirohashi K, Hamuro M, Nakamura K, Inoue Y, Kaneda K, Suehiro S. Correlation between dynamic computed tomographic and histopathological findings in the diagnosis of small hepatocellular carcinoma. Dig Surg. 2004;21:413–420. doi: 10.1159/000082318. [DOI] [PubMed] [Google Scholar]
- 70.Takayasu K, Muramatsu Y, Mizuguchi Y, Moriyama N, Ojima H. Imaging of early hepatocellular carcinoma and adenomatous hyperplasia (dysplastic nodules) with dynamic ct and a combination of CT and angiography: experience with resected liver specimens. Intervirology. 2004;47:199–208. doi: 10.1159/000078473. [DOI] [PubMed] [Google Scholar]
- 71.Libbrecht L, Desmet V, Roskams T. Preneoplastic lesions in human hepatocarcinogenesis. Liver Int. 2005;25:16–27. doi: 10.1111/j.1478-3231.2005.01016.x. [DOI] [PubMed] [Google Scholar]
- 72.Terminology for hepatic allograft rejection. International Working Party. Hepatology. 1995;22:648–654. [PubMed] [Google Scholar]
- 73.Borzio M, Fargion S, Borzio F, Fracanzani AL, Croce AM, Stroffolini T, Oldani S, Cotichini R, Roncalli M. Impact of large regenerative, low grade and high grade dysplastic nodules in hepatocellular carcinoma development. J Hepatol. 2003;39:208–214. doi: 10.1016/s0168-8278(03)00190-9. [DOI] [PubMed] [Google Scholar]
- 74.Tanaka M, Nakashima O, Wada Y, Kage M, Kojiro M. Pathomorphological study of Kupffer cells in hepatocellular carcinoma and hyperplastic nodular lesions in the liver. Hepatology. 1996;24:807–812. doi: 10.1053/jhep.1996.v24.pm0008855180. [DOI] [PubMed] [Google Scholar]
- 75.Imai Y, Murakami T, Yoshida S, Nishikawa M, Ohsawa M, Tokunaga K, Murata M, Shibata K, Zushi S, Kurokawa M, et al. Superparamagnetic iron oxide-enhanced magnetic resonance images of hepatocellular carcinoma: correlation with histological grading. Hepatology. 2000;32:205–212. doi: 10.1053/jhep.2000.9113. [DOI] [PubMed] [Google Scholar]
- 76.Quaglia A, Bhattacharjya S, Dhillon AP. Limitations of the histopathological diagnosis and prognostic assessment of hepatocellular carcinoma. Histopathology. 2001;38:167–174. doi: 10.1046/j.1365-2559.2001.01000.x. [DOI] [PubMed] [Google Scholar]
- 77.Roncalli M. Hepatocellular nodules in cirrhosis: focus on diagnostic criteria on liver biopsy. A Western experience. Liver Transpl. 2004;10:S9–S15. doi: 10.1002/lt.20047. [DOI] [PubMed] [Google Scholar]
- 78.Bolondi L, Gaiani S, Celli N, Golfieri R, Grigioni WF, Leoni S, Venturi AM, Piscaglia F. Characterization of small nodules in cirrhosis by assessment of vascularity: the problem of hypovascular hepatocellular carcinoma. Hepatology. 2005;42:27–34. doi: 10.1002/hep.20728. [DOI] [PubMed] [Google Scholar]
- 79.Takayasu K, Muramatsu Y, Mizuguchi Y, Okusaka T, Shimada K, Takayama T, Sakamoto M. CT Evaluation of the progression of hypoattenuating nodular lesions in virus-related chronic liver disease. AJR Am J Roentgenol. 2006;187:454–463. doi: 10.2214/AJR.05.0705. [DOI] [PubMed] [Google Scholar]
- 80.Ohto M, Karasawa E, Tsuchiya Y, Kimura K, Saisho H, Ono T, Okuda K. Ultrasonically guided percutaneous contrast medium injection and aspiration biopsy using a renal-time puncture transducer. Radiology. 1980;136:171–176. doi: 10.1148/radiology.136.1.7384495. [DOI] [PubMed] [Google Scholar]
- 81.Caturelli E, Solmi L, Anti M, Fusilli S, Roselli P, Andriulli A, Fornari F, Del Vecchio Blanco C, de Sio I. Ultrasound guided fine needle biopsy of early hepatocellular carcinoma complicating liver cirrhosis: a multicentre study. Gut. 2004;53:1356–1362. doi: 10.1136/gut.2003.032359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Durand F, Regimbeau JM, Belghiti J, Sauvanet A, Vilgrain V, Terris B, Moutardier V, Farges O, Valla D. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol. 2001;35:254–258. doi: 10.1016/s0168-8278(01)00108-8. [DOI] [PubMed] [Google Scholar]
- 83.Nakashima T, Kojiro M. Hepatocellular carcinoma. Tokyo: Springer-Verlag; 1987. pp. 105–115. [Google Scholar]
- 84.Ebara M, Ohto M, Sugiura N, Kita K, Yoshikawa M, Okuda K, Kondo F, Kondo Y. Percutaneous ethanol injection for the treatment of small hepatocellular carcinoma. Study of 95 patients. J Gastroenterol Hepatol. 1990;5:616–626. doi: 10.1111/j.1440-1746.1990.tb01115.x. [DOI] [PubMed] [Google Scholar]
- 85.Livraghi T, Bolondi L, Lazzaroni S, Marin G, Morabito A, Rapaccini GL, Salmi A, Torzilli G. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma in cirrhosis. A study on 207 patients. Cancer. 1992;69:925–929. doi: 10.1002/1097-0142(19920215)69:4<925::aid-cncr2820690415>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 86.Redvanly RD, Chezmar JL, Strauss RM, Galloway JR, Boyer TD, Bernardino ME. Malignant hepatic tumors: safety of high-dose percutaneous ethanol ablation therapy. Radiology. 1993;188:283–285. doi: 10.1148/radiology.188.1.8390070. [DOI] [PubMed] [Google Scholar]
- 87.Goldberg SN, Gazelle GS, Solbiati L, Rittman WJ, Mueller PR. Radiofrequency tissue ablation: increased lesion diameter with a perfusion electrode. Acad Radiol. 1996;3:636–644. doi: 10.1016/s1076-6332(96)80188-7. [DOI] [PubMed] [Google Scholar]
- 88.Solbiati L, Goldberg SN, Ierace T, Livraghi T, Meloni F, Dellanoce M, Sironi S, Gazelle GS. Hepatic metastases: percutaneous radio-frequency ablation with cooled-tip electrodes. Radiology. 1997;205:367–373. doi: 10.1148/radiology.205.2.9356616. [DOI] [PubMed] [Google Scholar]
- 89.Ryu M, Shimamura Y, Kinoshita T, Konishi M, Kawano N, Iwasaki M, Furuse J, Yoshino M, Moriyama N, Sugita M. Therapeutic results of resection, transcatheter arterial embolization and percutaneous transhepatic ethanol injection in 3225 patients with hepatocellular carcinoma: a retrospective multicenter study. Jpn J Clin Oncol. 1997;27:251–257. doi: 10.1093/jjco/27.4.251. [DOI] [PubMed] [Google Scholar]
- 90.Lencioni R, Bartolozzi C, Caramella D, Paolicchi A, Carrai M, Maltinti G, Capria A, Tafi A, Conte PF, Bevilacqua G. Treatment of small hepatocellular carcinoma with percutaneous ethanol injection. Analysis of prognostic factors in 105 Western patients. Cancer. 1995;76:1737–1746. doi: 10.1002/1097-0142(19951115)76:10<1737::aid-cncr2820761010>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 91.Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999;210:655–661. doi: 10.1148/radiology.210.3.r99fe40655. [DOI] [PubMed] [Google Scholar]
- 92.Lencioni RA, Allgaier HP, Cioni D, Olschewski M, Deibert P, Crocetti L, Frings H, Laubenberger J, Zuber I, Blum HE, et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology. 2003;228:235–240. doi: 10.1148/radiol.2281020718. [DOI] [PubMed] [Google Scholar]
- 93.Giorgio A, Tarantino L, de Stefano G, Scala V, Liorre G, Scarano F, Perrotta A, Farella N, Aloisio V, Mariniello N, et al. Percutaneous sonographically guided saline-enhanced radiofrequency ablation of hepatocellular carcinoma. AJR Am J Roentgenol. 2003;181:479–484. doi: 10.2214/ajr.181.2.1810479. [DOI] [PubMed] [Google Scholar]
- 94.Ebara M, Okabe S, Kita K, Sugiura N, Fukuda H, Yoshikawa M, Kondo F, Saisho H. Percutaneous ethanol injection for small hepatocellular carcinoma: therapeutic efficacy based on 20-year observation. J Hepatol. 2005;43:458–464. doi: 10.1016/j.jhep.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 95.Takayasu K, Muramatsu Y, Asai S, Muramatsu Y, Kobayashi T. CT fluoroscopy-assisted needle puncture and ethanol injection for hepatocellular carcinoma: a preliminary study. AJR Am J Roentgenol. 1999;173:1219–1224. doi: 10.2214/ajr.173.5.10541092. [DOI] [PubMed] [Google Scholar]
- 96.Sato M, Watanabe Y, Tokui K, Kawachi K, Sugata S, Ikezoe J. CT-guided treatment of ultrasonically invisible hepatocellular carcinoma. Am J Gastroenterol. 2000;95:2102–2106. doi: 10.1111/j.1572-0241.2000.02275.x. [DOI] [PubMed] [Google Scholar]
- 97.Schweiger GD, Brown BP, Pelsang RE, Dhadha RS, Barloon TJ, Wang G. CT fluoroscopy: technique and utility in guiding biopsies of transiently enhancing hepatic masses. Abdom Imaging. 2000;25:81–85. doi: 10.1007/s002619910016. [DOI] [PubMed] [Google Scholar]
- 98.Shibata T, Iimuro Y, Yamamoto Y, Ikai I, Itoh K, Maetani Y, Ametani F, Kubo T, Konishi J. CT-guided transthoracic percutaneous ethanol injection for hepatocellular carcinoma not detectable with US. Radiology. 2002;223:115–120. doi: 10.1148/radiol.2231010862. [DOI] [PubMed] [Google Scholar]
- 99.Kickuth R, Laufer U, Hartung G, Gruening C, Stueckle C, Kirchner J. 3D CT versus axial helical CT versus conventional tomography in the classification of acetabular fractures: a ROC analysis. Clin Radiol. 2002;57:140–145. doi: 10.1053/crad.2001.0860. [DOI] [PubMed] [Google Scholar]
- 100.Solomon SB, Bohlman ME, Choti MA. Percutaneous gadolinium injection under MR guidance to mark target for CT-guided radiofrequency ablation. J Vasc Interv Radiol. 2002;13:419–421. doi: 10.1016/s1051-0443(07)61747-3. [DOI] [PubMed] [Google Scholar]
- 101.Maruyama H, Kobayashi S, Yoshizumi H, Okugawa H, Akiike T, Yukisawa S, Fukuda H, Matsutani S, Ebara M, Saisho H. Application of percutaneous ultrasound-guided treatment for ultrasonically invisible hypervascular hepatocellular carcinoma using microbubble contrast agent. Clin Radiol. 2007;62:668–675. doi: 10.1016/j.crad.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 102.Bartolozzi C, Lencioni R, Ricci P, Paolicchi A, Rossi P, Passariello R. Hepatocellular carcinoma treatment with percutaneous ethanol injection: evaluation with contrast-enhanced color Doppler US. Radiology. 1998;209:387–393. doi: 10.1148/radiology.209.2.9807563. [DOI] [PubMed] [Google Scholar]
- 103.Wen YL, Kudo M, Zheng RQ, Minami Y, Chung H, Suetomi Y, Onda H, Kitano M, Kawasaki T, Maekawa K. Radiofrequency ablation of hepatocellular carcinoma: therapeutic response using contrast-enhanced coded phase-inversion harmonic sonography. AJR Am J Roentgenol. 2003;181:57–63. doi: 10.2214/ajr.181.1.1810057. [DOI] [PubMed] [Google Scholar]
- 104.Meloni MF, Goldberg SN, Livraghi T, Calliada F, Ricci P, Rossi M, Pallavicini D, Campani R. Hepatocellular carcinoma treated with radiofrequency ablation: comparison of pulse inversion contrast-enhanced harmonic sonography, contrast-enhanced power Doppler sonography, and helical CT. AJR Am J Roentgenol. 2001;177:375–380. doi: 10.2214/ajr.177.2.1770375. [DOI] [PubMed] [Google Scholar]
- 105.Choi D, Lim HK, Kim SH, Lee WJ, Jang HJ, Lee JY, Paik SW, Koh KC, Lee JH. Hepatocellular carcinoma treated with percutaneous radio-frequency ablation: usefulness of power Doppler US with a microbubble contrast agent in evaluating therapeutic response-preliminary results. Radiology. 2000;217:558–563. doi: 10.1148/radiology.217.2.r00oc07558. [DOI] [PubMed] [Google Scholar]
- 106.Kim CK, Choi D, Lim HK, Kim SH, Lee WJ, Kim MJ, Lee JY, Jeon YH, Lee J, Lee SJ, et al. Therapeutic response assessment of percutaneous radiofrequency ablation for hepatocellular carcinoma: utility of contrast-enhanced agent detection imaging. Eur J Radiol. 2005;56:66–73. doi: 10.1016/j.ejrad.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 107.Solbiati L, Goldberg SN, Ierace T, Dellanoce M, Livraghi T, Gazelle GS. Radio-frequency ablation of hepatic metastases: postprocedural assessment with a US microbubble contrast agent--early experience. Radiology. 1999;211:643–649. doi: 10.1148/radiology.211.3.r99jn06643. [DOI] [PubMed] [Google Scholar]
- 108.Cioni D, Lencioni R, Bartolozzi C. Therapeutic effect of transcatheter arterial chemoembolization on hepatocellular carcinoma: evaluation with contrast-enhanced harmonic power Doppler ultrasound. Eur Radiol. 2000;10:1570–1575. doi: 10.1007/s003300000496. [DOI] [PubMed] [Google Scholar]
- 109.Morimoto M, Shirato K, Sugimori K, Kokawa A, Tomita N, Saito T, Imada T, Tanaka N, Nozawa A, Numata K, et al. Contrast-enhanced harmonic gray-scale sonographic-histologic correlation of the therapeutic effects of transcatheter arterial chemoembolization in patients with hepatocellular carcinoma. AJR Am J Roentgenol. 2003;181:65–69. doi: 10.2214/ajr.181.1.1810065. [DOI] [PubMed] [Google Scholar]
- 110.Pompili M, Riccardi L, Covino M, Barbaro B, Di Stasi C, Orefice R, Gasbarrini G, Rapaccini GL. Contrast-enhanced gray-scale harmonic ultrasound in the efficacy assessment of ablation treatments for hepatocellular carcinoma. Liver Int. 2005;25:954–961. doi: 10.1111/j.1478-3231.2005.01135.x. [DOI] [PubMed] [Google Scholar]
- 111.Minami Y, Kudo M, Kawasaki T, Kitano M, Chung H, Maekawa K, Shiozaki H. Transcatheter arterial chemoembolization of hepatocellular carcinoma: usefulness of coded phase-inversion harmonic sonography. AJR Am J Roentgenol. 2003;180:703–708. doi: 10.2214/ajr.180.3.1800703. [DOI] [PubMed] [Google Scholar]
- 112.Lim HS, Jeong YY, Kang HK, Kim JK, Park JG. Imaging features of hepatocellular carcinoma after transcatheter arterial chemoembolization and radiofrequency ablation. AJR Am J Roentgenol. 2006;187:W341–W349. doi: 10.2214/AJR.04.1932. [DOI] [PubMed] [Google Scholar]
- 113.Rankin RN, Fenster A, Downey DB, Munk PL, Levin MF, Vellet AD. Three-dimensional sonographic reconstruction: techniques and diagnostic applications. AJR Am J Roentgenol. 1993;161:695–702. doi: 10.2214/ajr.161.4.8372741. [DOI] [PubMed] [Google Scholar]
- 114.Picot PA, Rickey DW, Mitchell R, Rankin RN, Fenster A. Three-dimensional colour Doppler imaging. Ultrasound Med Biol. 1993;19:95–104. doi: 10.1016/0301-5629(93)90001-5. [DOI] [PubMed] [Google Scholar]
- 115.Downey DB, Fenster A. Vascular imaging with a three-dimensional power Doppler system. AJR Am J Roentgenol. 1995;165:665–668. doi: 10.2214/ajr.165.3.7645492. [DOI] [PubMed] [Google Scholar]
- 116.Ritchie CJ, Edwards WS, Mack LA, Cyr DR, Kim Y. Three-dimensional ultrasonic angiography using power-mode Doppler. Ultrasound Med Biol. 1996;22:277–286. doi: 10.1016/0301-5629(95)02052-7. [DOI] [PubMed] [Google Scholar]
- 117.Acar P, Dulac Y, Taktak A, Abadir S. Real-time three-dimensional fetal echocardiography using matrix probe. Prenat Diagn. 2005;25:370–375. doi: 10.1002/pd.1159. [DOI] [PubMed] [Google Scholar]
- 118.Monaghan MJ. Role of real time 3D echocardiography in evaluating the left ventricle. Heart. 2006;92:131–136. doi: 10.1136/hrt.2004.058388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ohto M, Kato H, Tsujii H, Maruyama H, Matsutani S, Yamagata H. Vascular flow patterns of hepatic tumors in contrast-enhanced 3-dimensional fusion ultrasonography using plane shift and opacity control modes. J Ultrasound Med. 2005;24:49–57. doi: 10.7863/jum.2005.24.1.49. [DOI] [PubMed] [Google Scholar]
- 120.Kennedy JE, Wu F, ter Haar GR, Gleeson FV, Phillips RR, Middleton MR, Cranston D. High-intensity focused ultrasound for the treatment of liver tumours. Ultrasonics. 2004;42:931–935. doi: 10.1016/j.ultras.2004.01.089. [DOI] [PubMed] [Google Scholar]
- 121.Li CX, Xu GL, Jiang ZY, Li JJ, Luo GY, Shan HB, Zhang R, Li Y. Analysis of clinical effect of high-intensity focused ultrasound on liver cancer. World J Gastroenterol. 2004;10:2201–2204. doi: 10.3748/wjg.v10.i15.2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wu F, Wang ZB, Chen WZ, Zou JZ, Bai J, Zhu H, Li KQ, Jin CB, Xie FL, Su HB. Advanced hepatocellular carcinoma: treatment with high-intensity focused ultrasound ablation combined with transcatheter arterial embolization. Radiology. 2005;235:659–667. doi: 10.1148/radiol.2352030916. [DOI] [PubMed] [Google Scholar]