Abstract
Lipomas may be located in all parts of the body and may be confused clinically with other soft tissue masses. They infrequently occur in the head and neck. A large neck mass (greater than 10 cm) with a rapid growth rate should raise concerns about a possible malignancy. Failure to distinguish a liposarcoma from a lipoma may represent a medicolegal pitfall. Surgical excision of a lipoma is often used as the definitive treatment modality, and alternative treatments described for lipomas range from liposuction to steroid injections. In the present study, a 60-year-old man who presented with a rapidly enlarging submental mass is described. A 15 cm × 12 cm mass was successfully removed. The surgery produced excellent cosmetic results and no functional impairment. An integrated review of the literature regarding etiology, epidemiology, diagnostic and treatment modalities of submental lipomas follows.
Keywords: Lipoma, Liposarcoma, Mass, Neck
Abstract
Les lipomes peuvent se situer n’importe où sur le corps et, d’un point de vue clinique, on peut les confondre avec d’autres masses des tissus mous. Dans de rares cas, ils se manifestent sur la tête et le cou. Une grosse masse sur le cou (de plus de 10 cm) au taux de croissance rapide doit soulever la possibilité d’une malignité. Le fait de ne pas distinguer un liposarcome d’un lipome peut représenter un écueil médicolégal. L’excision chirurgicale d’un lipome constitue souvent une modalité de traitement définitive, et les autres traitements décrits varient de la liposuccion aux injections de stéroïdes. Dans la présente étude, on décrit le cas d’un homme de 60 ans qui a consulté en raison d’une masse sous-mentale à la croissance rapide. On lui a excisé une masse de 15 cm × 12 cm. L’opération a donné d’ex-cellents résultats esthétiques, sans atteinte fonctionnelle. Suit une analyse bibliographique intégrée au sujet de l’étiologie, de l’épidémiologie, du diagnostic et des modalités de traitement des lipomes sous-mentaux.
Lipomas infrequently occur in the head and neck. A large neck mass (greater than 10 cm) with a rapid growth rate should raise concerns about a possible malignancy. In the present study, we describe a 60-year-old man who presented with a rapidly enlarging submental mass. A 15 cm × 12 cm mass was successfully removed. The surgery produced excellent cosmetic results and no functional impairment. An integrated review of the literature regarding etiology, epidemiology, diagnostic and treatment modalities of submental lipomas follows.
It is broadly accepted that lipomas are one of the most common mesenchymal tumours (1–4). Failure to distinguish a benign lipoma from a liposarcoma (the most common soft tissue malignancy in adults) may represent a potential medical and legal pitfall (5). Distinguishing a lipoma from a well-differentiated liposarcoma, however, can represent a unique challenge, but it is highly important due to differences in treatment, prognosis and follow-up (5,6).
Gathering information from the medical history and physical examination may narrow the differential diagnosis. Information about rate of growth, size, location, consistency and attachment to adjacent tissues is essential for differentiating benign from malignant masses. Diagnostic imaging, including computed tomography (CT) or magnetic resonance imaging (MRI), can provide adjunctive information in the diagnosis of the mass (7,8). Lipomas may be located in all parts of the body and may be classified as superficial or deep based on the site of origin (9). Liposarcomas generally arise as painless masses in the lower extremities or the retroperitoneum, and can be exceptionally large (2,9). Lipomas are pathologically distinctive both grossly and microscopically, being composed of a collection of solitary vacuole fat cells (9). Lipomas, although rarely, may exhibit a malignant transformation to a liposarcoma. Liposarcomas are histologically described as being similar to lipomas, but with scattered atypical fibroblasts or sometimes signet ring cells present.
Historically, the most common treatment for lipomas is surgical excision. Other modalities have been reported, ranging from liposuction (10–14) to steroid injections (15). Liposuction is sometimes preferred to excision because it causes less scarring (13,14). The recurrence rate may be higher compared with excision if residual tumour, including the capsule, remains after the procedure. Steroid injections are often used for the treatment of smaller lipomas, but may require several injections and may depigment the overlying skin. Surgical excision remains the treatment of choice for lipomas. Some of the most common complications from surgical excision include hematoma, ecchymosis, infection, deformity, damage to adjacent structures, excessive scarring and fat embolus. Recurrence after excision occurs in less than 5% of cases depending upon location and extent of the resection (2,6). We report a case of a giant lipoma of the submental area and a review of the literature.
CASE PRESENTATION
The institution from which the present report originates does not require institutional review board approval for publication of retrospective reports.
A 60-year-old African-American male presented to the plastic surgery clinic, complaining of recent enlargement of a submental mass. It had been present for over 15 years, but had enlarged rapidly over the past two months. The patient denied any recent weight loss or pain associated with the mass. He also denied any fevers or blunt trauma to the area. The patient was otherwise in good health except for mild hypertension for which he took no medication. Vital signs demonstrated that the patient was afebrile and hemodynamically stable. The patient’s height was 1.75 m, and his weight on admission was 119 kg.
Physical examination revealed an approximately 14 cm, mobile soft mass located in the subcutaneous tissue of the submental area (Figure 1). He had no noticeable lymphadenopathy or other palpable masses, and his oral pharynx was normal. There was no apparent facial nerve deficit. Pertinent laboratory data included a white blood cell count of 7.1×109/L, hemoglobin 134 g/L, platelet count of 225×109/L and a creatinine of 83.9 μmol/L. His coagulation profile consisted of a pro-thrombin time of 12.0 s, international normalized ratio of 1.0 and a partial thromboplastin time of 28.7 s.
Figure 1).
An intraoperative preincision photograph of the patient’s submental mass
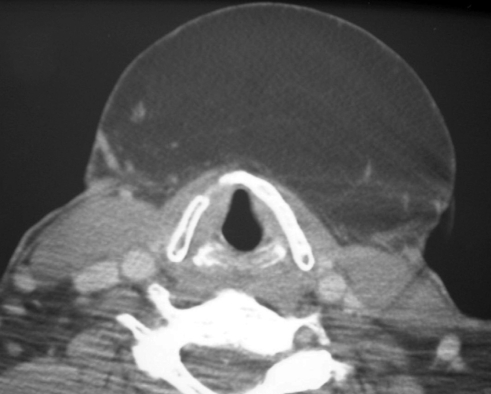
The mass appeared benign in origin because it was a soft, mobile, subcutaneous mass present for 15 years. Its location in the neck and recent increased rate of growth raised concern for a malignant etiology. A CT of the soft tissue of the patient’s neck was recommended. The CT revealed a 14 cm × 12 cm mass in transverse and longitudinal dimensions, respectively (Figure 2). The mass was well-circumscribed and located in the submental area without evidence of invasion of adjacent structures. The signal intensity of the mass in the CT was homogeneous without internal septations or nodularity. The density of the mass on the CT suggested that the majority of the tumour was composed of fat. Risks and benefits of surgical excision and liposuction were discussed with the patient at length. Due to the large size of the tumour, it was thought that liposuction would produce a higher risk of recurrence. Surgical excision of the tumour was recommended to the patient, because the possibility of a malignancy was present in the differential diagnosis.
Figure 2).
Computed tomography of the patient’s submental mass at the level of the hyoid
After general anesthesia was induced, the anterior neck was exposed and accessed via an elliptical incision because excess skin was anticipated (Figure 3). The platysma muscle was divided, and superior and inferior flaps were created. A large mass approximately 15 cm in diameter was excised in its entirety. Hemostasis was achieved with electrocautery, and the inferior flap was brought over the superior flap to measure skin redundancy. The mass and the redundant skin were both excised, and the tissue closed in two layers after a 10 Fr drain was placed. The patient was discharged from the hospital the same day of the surgery.
Figure 3).
Intraoperative photograph of the patient’s neck after excision of the mass in its entirety
Pathological examination revealed a 15 cm × 12 cm encapsulated tumour. It contained mature adipocytes with no cellular atypia. Numerous fibrous bands through the specimen were evident. The final pathological diagnosis was lipoma. The patient was seen at one and three weeks postoperatively with excellent cosmetic results and no functional impairment. At 12 months postoperatively he had no evidence of recurrence.
DISCUSSION
Lipomas are the most common mesenchymal tumours of adulthood. Malignant degeneration to liposarcomas has been rarely reported in the literature (5). A peak incidence of lipoma formation is noted in the fifth and sixth decades of life, and lipomas are more common in obese individuals (14). An annual incidence of one per 1000 persons is estimated. This is most likely an underestimation because these lesions are generally brought to the attention of a physician after they become cosmetically unpleasing, cause pain or impair function (15,16). Lipomas make up approximately 5% of all benign tumours of the body, and they may occur anywhere on the surface of the body (17). Most lipomas are less than 5 cm but there are reports of giant lipomas of more than 20 cm (9). Solitary lesions are most common (80%), especially in women. Multiple lipomas (lipomatosis) are more common in men (5). Common locations for lipomas are the back, arm, shoulder, anterior chest wall, breast, thigh, abdominal wall, legs, forehead and face, in decreasing order of frequency (18). Lipomas rarely occur in the head and neck (1). Of those lipomas that occur in the head and neck region, the most common location is the posterior neck. Intraoperatively, lipomas may be seen as soft, yellow, shiny, smooth, mobile, encapsulated and occasionally lobulated subcutaneous masses. Microscopically, the lesions show lobular growth of mature adipocytes with demarcated borders, a fibrous capsule and a central vacuole (6). Lipomas are classified into conventional lipomas, angiolipomas, fibrolipomas, spindle cell lipomas, pleomorphic lipomas, hibernomas, myelolipomas and atypical lipomas depending on their microscopic appearance (19). In some instances, lipomas infiltrate into adjacent muscle and are termed infiltrating lipomas (15). A new variant of lipoma, termed adenolipoma, is characterized by the presence of eccrine sweat glands throughout the tumour and is usually found on the proximal extremities (20).
Lipomas are composed of physiologically distinct mature adipocytes; its lipids are not available for metabolic utilization. This, along with their autonomous growth, allows their classification as a benign neoplasm. Differentiating a lipoma from a well-differentiated liposarcoma may represent a challenge for the pathologist. The absence of vacuoles in the irregularly shaped nuclei and increased size of the cells are some of the characteristics that may guide the pathologist toward the diagnosis of a well-differentiated liposarcoma. Conventional lipomas have characteristic chromosomal abnormalities. For example, conventional lipomas often show chromosomal rearrangements of 12q14–15, 6p and 13q.9 (15,16). In most cases, however, there is usually no history of familial occurrence, and there is no evidence to support any type of genetic transmission (17,18). Lipomas appear to be associated with trauma, but it has not been determined whether the trauma causes the tumour or if the discovery of the tumour is incidental (19). Clinical features vary greatly depending upon the lesion’s size, location and rate of growth. In most cases, these benign tumours present as painless, mobile, palpable masses, which are well circumscribed and are often overlooked by patients until the mass increases appreciably in size. They are nonfluctuant, have a rubbery consistency and may be associated with syndromes including hereditary multiple lipomatosis (lipomas over the extremities and trunk) (16), Gardner’s syndrome (associated with intestinal polyposis, cysts and osteomas), Madelung’s disease (lipomatosis of the head, neck, shoulders and proximal upper extremities) (21) and Dercum’s disease (multiple painful subcutaneous lipomas) (22). The differential diagnosis between lipomas and liposarcomas is broad and includes such indicators as epidermal cysts, subcutaneous tumours, nodular fascitis, liposarcomas, metastatic disease, erythema nodosum, nodular subcutaneous fat necrosis, vasculitic nodules, rheumatic nodules, sarcoidosis, infections and hematomas.
Most lipomas pose no diagnostic dilemmas. However, when presented with large (more than 10 cm) or rapidly growing masses, especially of the head and neck region, one should be concerned about a malignancy. The main diagnostic dilemma is to distinguish a lipoma from a liposarcoma. Liposarcomas are usually located in the retroperitoneum, buttock, leg muscles or mediastinum (deeper soft tissue rather than in the subcutaneous areas). The appearance of tumour margins, the signal intensity homogeneity, the size, peritumoral signal intensity on diagnostic imaging, the apparent neurovascular bundle encasement or displacement and bone invasion are not consistent features that differentiate liposarcomas, especially well-differentiated liposarcomas, from lipomas.
CT or MRI before excision may provide important information in distinguishing a fatty benign lesion from a liposarcoma before a surgical approach is made. Treatment modalities for lipomas can be divided into nonexcisional and excisional techniques. Nonexcisional techniques involve steroid injections, which results in fat atrophy, and liposuction, which destroys the adipose tissue but not the fibrous capsule. Steroid injections are used for patients who have small lipomas or do not wish excision. The volume of steroid injected depends upon the size of the lipoma. Regardless, steroid injections will not eliminate the lipoma. Disadvantages include the need for multiple injections and possible depigmentation of the overlying skin. Liposuction may be used for small or large lipomas; however, removal of the entire tumour is difficult (12,13). This may be done in the office setting depending on the location and size of the tumour and the experience of the surgeon (10). Simple excision is the most common modality of treatment for lipomas. Numerous techniques have been described ranging from simple excision to squeeze delivery of subcutaneous lipomas (23–28). We chose surgical excision because the clinical features of the mass placed the patient at a higher risk of having a tumour with a malignant etiology. In this case, the tumour was easily excised in its entirety through an elliptical incision. Complications after excision of a lipoma most commonly include hematoma, followed by seroma, ecchymosis, infection, deformity, injury to adjacent structures, excessive scarring and fat embolus. Ordinary lipomas recur locally in less than 5% of cases (28,29). Those that do recur are usually located in difficult anatomical locations or have microscopically infiltrated into adjacent muscle and were not resected completely during the initial operation. The present study reported a case of a patient with a rapid enlargement of a giant submental lipoma treated successfully with surgical excision through an elliptical incision. A CT of the soft tissues of the neck was recommended because of the clinical features of the mass. Improved diagnostic imaging technology (such as CT or MRI) has been accompanied by increasing reports of the utility of these imaging techniques in the diagnosis of complex or unusual neck masses.
As the biological behaviour of tumours such as lipomas and liposarcomas is discovered, patients with suspicious neck masses can be further evaluated with CT or MRI. In the patient having a mass without malignant features (size, location, rate of growth, etc), medical history and physical examination still represent a secure evaluation method before surgical treatment of the tumour.
REFERENCES
- 1.Barnes L, Ferlito A. Soft tissue neoplasms. In: Ferlito A, editor. Neoplasms of the Larynx. 1st edn. London: Churchill-Livingstone; 1993. pp. 265–304. [Google Scholar]
- 2.Truhan AP, Garden JM, Caro WA, Roenigk HH., Jr Facial and scalp lipomas: Case reports and study of prevalence. J Dermatol Surg Oncol. 1985;11:981–4. doi: 10.1111/j.1524-4725.1985.tb01381.x. [DOI] [PubMed] [Google Scholar]
- 3.Som PM, Scherl MP, Rao VM, Biller HF. Rare presentations of ordinary lipomas of the head and neck: A review. AJNR Am J Neuroradiol. 1986;7:657–64. [PMC free article] [PubMed] [Google Scholar]
- 4.Ramakantan R, Shah P. Anterior neck lipoma masquerading as an external laryngocoele. J Laryngol Otol. 1989;103:1087–8. doi: 10.1017/s0022215100111077. [DOI] [PubMed] [Google Scholar]
- 5.Rydholm A, Berg NO. Size, site and clinical incidence of lipoma. Factors in the differential diagnosis of lipoma and sarcoma. Acta Orthop Scand. 1983;54:929–34. doi: 10.3109/17453678308992936. [DOI] [PubMed] [Google Scholar]
- 6.Weiss SW. Lipomatous tumors. Monogr Pathol. 1996;38:207–39. [PubMed] [Google Scholar]
- 7.Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): Results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182:733–9. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 8.Tateishi U, Gladish GW, Kusumoto M, et al. Chest wall tumors: Radiologic findings and pathologic correlation: Part 2. Malignant tumors. Radiographics. 2003;23:1491–508. doi: 10.1148/rg.236015527. [DOI] [PubMed] [Google Scholar]
- 9.Cotran RS, Kumar V, Collins T. Robbins Pathologic Basis of Disease. 6th edn. Philadelphia: WB Saunders Co; 1999. pp. 1260–1. [Google Scholar]
- 10.Wilhelmi BJ, Blackwell SJ, Mancoll JS, Phillips LG. Another indication for liposuction: Small facial lipomas. Plast Reconstr Surg. 1999;103:1864–7. doi: 10.1097/00006534-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Sharma PK, Janninger CK, Schwartz RA, Rauscher GE, Lambert WC. The treatment of atypical lipoma with liposuction. J Dermatol Surg Oncol. 1991;17:332–4. doi: 10.1111/j.1524-4725.1991.tb01706.x. [DOI] [PubMed] [Google Scholar]
- 12.Field LM. Lipo-suction surgery: A review. J Dermatol Surg Oncol. 1984;10:530–8. doi: 10.1111/j.1524-4725.1984.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 13.Rubenstein R, Roenigk HH, Garden JM, Goldberg NS, Pinski JB. Liposuction for lipomas. J Dermatol Surg Oncol. 1985;11:1070–4. doi: 10.1111/j.1524-4725.1985.tb01395.x. [DOI] [PubMed] [Google Scholar]
- 14.Calhoun KH, Bradfield JJ, Thompson C. Liposuction-assisted excision of cervicofacial lipomas. Otolaryngol Head Neck Surg. 1995;113:401–3. doi: 10.1016/S0194-59989570075-7. [DOI] [PubMed] [Google Scholar]
- 15.Koh HK, Bhawan J. Tumors of the skin. In: Moschella SL, Hurley HJ, editors. Dermatology. 3rd edn. Philadelphia: Saunders; 1992. pp. 1721–808. [Google Scholar]
- 16.Zuber TJ. Soft Tissue Surgery for the Family Physician (illustrated manuals, videotapes, and CD-ROMs of soft tissue surgery techniques) Kansas City: American Academy of Family Physicians; 1998. Skin biopsy, excision and repair techniques; pp. 100–6. [Google Scholar]
- 17.Enzinger FM, Weiss SW. Benign lipomatous tumors. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumors. 2nd edn. St Louis: Mosby; 1988. pp. 301–45. [Google Scholar]
- 18.Rapidis AD. Lipoma of the oral cavity. Int J Oral Surg. 1982;11:30–5. doi: 10.1016/s0300-9785(82)80045-8. [DOI] [PubMed] [Google Scholar]
- 19.Ashley DJB. Evans’ Histological Appearances of Tumours. 3rd edn. Edinburgh: Churchill Livingston; 1978. p. 54. [Google Scholar]
- 20.Del Agua C, Felipo F. Adenolipoma of the skin. Dermatol Online J. 2004;10:9. [PubMed] [Google Scholar]
- 21.Austin RM, Mack GR, Townsend CM, Lack EE. Infiltrating (intramuscular) lipomas and angiolipomas. A clinicopathologic study of six cases. Arch Surg. 1980;115:281–4. doi: 10.1001/archsurg.1980.01380030031007. [DOI] [PubMed] [Google Scholar]
- 22.Anders KH, Ackerman AB. Neoplasms of the subcutaneous fat. In: Freeberg IM, Eisen AZ, Wolff K, et al., editors. Fitzpatrick’s Dermatology in General Medicine. 5th edn. New York: McGraw-Hill; 1999. pp. 1292–300. [Google Scholar]
- 23.Bataineh AB, Mansour MJ, Abalkhail A. Oral infiltrating lipomas. Br J Oral Maxillofac Surg. 1996;34:520–3. doi: 10.1016/s0266-4356(96)90249-1. [DOI] [PubMed] [Google Scholar]
- 24.Luba MC, Bangs SA, Mohler AM, Stulberg DL. Common benign skin tumors. Am Fam Physician. 2003;67:729–38. [PubMed] [Google Scholar]
- 25.Signorini M, Campiglio GL. Posttraumatic lipomas: Where do they really come from? Plast Reconstr Surg. 1998;101:699–705. doi: 10.1097/00006534-199803000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Uhlin SR. Benign symmetric lipomatosis. Arch Dermatol. 1979;115:94–5. [PubMed] [Google Scholar]
- 27.Amine B, Leguilchard F, Benhamou CL. Dercum’s disease (adiposis dolorosa): A new case report. Joint Bone Spine. 2004;71:147–9. doi: 10.1016/S1297-319X(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 28.Kenawi MM. ‘Squeeze delivery’ excision of subcutaneous lipoma related to anatomic site. Br J Surg. 1995;82:1649–50. doi: 10.1002/bjs.1800821221. [DOI] [PubMed] [Google Scholar]
- 29.Batsakis JG. Tumors of the Head and Neck: Clinical and Pathologic Considerations. 2nd edn. Baltimore: Williams & Wilkins; 1979. pp. 360–4. [Google Scholar]