Abstract
Objective:
We examined the long-term effects of childhood familial and neighborhood risk on adolescent substance use and psychiatric symptomatology.
Method:
This study used data from an ongoing 2-decade long study that recruited alcoholic and neighborhood control families through fathers' drunk-driving records and door-to-door canvassing in a four county area. The sample included 220 male, initially 3- to 5-year-old children of the participant families, who received in-home assessments at baseline and thereafter at 3-year intervals. Parental lifetime psychopathology and offspring symptomatology at ages 18-20 were assessed by semistructured diagnostic interviews. Census tract variables were used to indicate neighborhood characteristics.
Results:
The isomorphic parental symptomatology predicted offspring psychopathology. For marijuana-use disorder, major depressive disorder, and nicotine dependence, the other parental comorbidities were also significant predictors. Neighborhood residential instability in childhood contributed to the development of late adolescent alcohol-use disorder, marijuana-use disorder, major depressive disorder, antisocial personality disorder, and nicotine-dependence symptomatology. Although lower family socioeconomic status in childhood contributed to more adolescent marijuana-use disorder, major depressive disorder, and nicotine-dependence symptoms, neighborhood socioeconomic status did not predict adolescent psychopathology. Longitudinal changes in neighborhood environments from early childhood to adolescence had significant effects on alcohol-use disorder, marijuana-use disorder, and major depressive disorder symptoms in late adolescence. A higher frequency of family mobility from early childhood to adolescence predicted more nicotine-dependence symptoms in late adolescence.
Conclusions:
Findings indicate that parental psychopathology, family socioeconomic status, and neighborhood residential instability are all important risk factors for the development of substance-use disorder and other comorbid psychopathology. Intervention programming might effectively use these early parental psychopathology indicators to identify risk and might target community activity to stabilize the social environment and provide youth services to counteract the effects of family transience.
Characterization of neighborhood effects on children's behavioral or mental health problems can provide important information for prevention programming as well as policy making. Existing studies addressing this issue are mostly cross-sectional (e.g., Winstanley et al., 2008) and have been reviewed comprehensively by Leventhal and Brooks-Gunn (2000). These cross-sectional studies are insufficient to establish a causal relationship between neighborhood characteristics and behavioral/mental health problems because they account for neither exposure time nor individual differences in choice of a residence place (Buu et al., 2007). Furthermore, without characterization of familial influence, models of more distal neighborhood effects are at best incomplete and at worst provide inaccurate conclusions. Well-characterized prospective family studies are essential to sort out proximal and distal relationships and to establish an order of precedence of these effects.
Review of existing longitudinal studies
There are two types of longitudinal studies in the literature: quasi-experimental and observational studies. Each approach has its own strengths and weaknesses. Residential mobility studies such as Moving to Opportunity (Katz et al., 2001; Kling et al., 2007; Leventhal and Brooks-Gunn, 2003) and the Yonkers project (Fauth et al., 2005) randomly assigned low-income families residing in high-poverty neighborhoods to relocate to low-poverty neighborhoods. Two to 5 years later (durations vary across studies), the children of movers reported fewer behavior problems than did the children of stayers. Gender differences were also found in the Moving to Opportunity study, with female youth benefiting most from the relocation (Kling et al., 2007). Although experimental studies (through random assignments) are theoretically better designs to control for confounding variables than observational studies, in reality, participants in these residential mobility studies can choose not to use the vouchers offered to them. For example, the compliance rate was only 47% across all five sites of the Moving to Opportunity program (Leventhal and Brooks-Gunn, 2003). Although the compliance rate for the movers in the Yonkers project was 95%, the stayer group was not recruited through randomization, and pre-move differences between movers and stayers could not be tested because baseline data were unavailable (Fauth et al., 2005). Another practical issue with the quasi-experimental studies is that the mover sometimes experiences social alienation or hostility from new neighbors (Fauth et al., 2004; Rubinowitz and Rosenbaum, 2000). Such negative interaction or lack of interaction with new neighbors may confound the program effects. In particular, older youth tended to experience more discrimination distress (Fauth et al., 2005) and also were able to travel back to their old high-poverty neighborhoods, thus vitiating the change-of-residence effects (Leventhal and Brooks-Gunn, 2003). To deal with these potential confounding effects, these studies usually control for family background variables such as ethnicity, age, and education during data analyses.
Conducted in natural settings, a small group of longitudinal observational studies provide an alternative way to examine neighborhood effects without problems from artificially manipulating participants' residences. However, neighborhood effects in these studies are evident only when a number of relevant confounding variables, including family socioeconomic status, parental psychopathology, and family mobility, are controlled. Luthar and Cushing (1999) studied the effects of neighborhood socioeconomic status (indicated by census data) on internalizing/externalizing behaviors and substance use among the offspring (ages 7-17) of patients who met Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R; American Psychiatric Association, 1987), criteria for cocaine or opioid dependence. Neighborhood effects were shown only for drug use in their 2-year-long study. Hoffmann (2002) used data of 10th and 12th graders from the National Educational Longitudinal Study to examine the impact of neighborhood environment (measured by zip code–level census data) on youth drug use. Although no “neighborhood” effects were found, family mobility in the 2-year time frame contributed to drug use. Although the study involved a national sample, the effect tested was not at the neighborhood level because zip code areas vary dramatically in size and may include residents with considerable heterogeneity of socioeconomic status (Thomas et al., 2006). Using self-report data, Lambert et al. (2004) found that perceptions of neighborhood disorganization in Grade 7 predicted increased tobacco, alcohol, and marijuana use in Grade 9 among urban black youths. A recent study on children of alcoholics and controls (Trim and Chassin, 2008) found that, among children of nonalcoholics, higher neighborhood socioeconomic status predicted increased rates of alcohol use and consequences, whereas among children of alcoholics, the opposite association was true. A significant effect for family mobility on adolescent alcohol use in the 3-year interval was also found. Although the four studies reviewed above had primary interests in the direct impact of neighborhood on youth mental health, other longitudinal studies have examined if neighborhood contexts moderate other risk factors' effects. Roche et al. (2007) found that the stakes of uninvolved and permissive parenting for problematic adolescent outcomes were greater in higher risk neighborhoods based on two-wave data (over 16 months) from minority youth in low-income urban areas. Analyzing three-wave data (over 6 years) of the Project on Human Development in Chicago Neighborhoods, Fauth et al. (2007) showed that participation in community-based clubs was positively associated with youth anxiety/depression in violent neighborhoods only, whereas church groups were protective against substance use in nonviolent neighborhoods.
Unique features of the present study
The present study analyzed data from the second-generation participants in the Michigan Longitudinal Study (Zucker et al., 2000) to examine both familial and neighborhood effects over the course of childhood on the development of substance-use disorder and other psychopathologies at ages 18-20. There are several unique features to the study. First, it extends the developmental period over which effects may occur to ages 3 through 20, whereas prior longitudinal studies covered shorter developmental intervals (1-6 years). Second, we examine not only neighborhood socioeconomic status effects, as in prior longitudinal studies, but also the effect of neighborhood residential instability—another factor identified as an important dimension of neighborhood influence in cross-sectional studies (Leventhal and Brooks-Gunn, 2000). Third, the study uses DSM, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), symptom counts on substance-use disorders and comorbid psychiatric disorders, including alcohol-use disorder, marijuana-use disorder, major depressive disorder, antisocial personality disorder, and nicotine dependence as outcome measures. Most earlier work used nonstandard parent or self-report assessments of mental health outcomes or substance use. Fourth, as psychopathology is transmissible from parents to children (Dierker et al., 1999), neighborhood effects are clearly evident only after the effects of parental psychopathology and proximal family influences are taken into account, as done here. Relatedly, a significant short-term effect of family mobility on substance use (2-3 years) was found in two of the previous studies (Hoffmann, 2002; Trim and Chassin, 2008) but was not examined in other longitudinal work. This study examines the effects of both the frequency of family mobility and patterns of change in neighborhoods over the course of 12 years on the development of these psychopathologies.
Theoretical framework and hypotheses
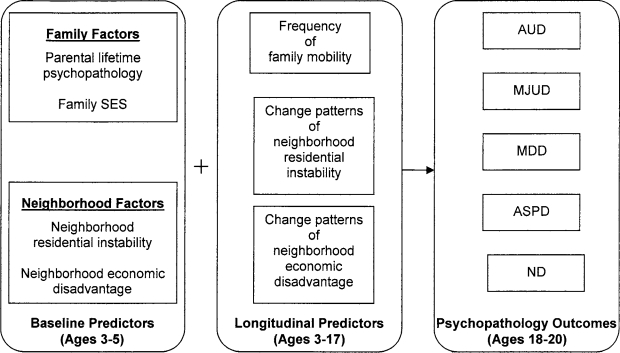
Figure 1 provides the theoretical framework that guided the statistical analysis. It begins with the most proximal familial influences (genetic and socialization effects as indexed by parental psychopathology), the proximal opportunity structure (as measured by family socioeconomic status), and then moves to the more distal neighborhood contextual influences. In the family-level model, we tested familial transmission of psychopathology based on the sequences listed in Table 1. The conceptual framework guiding order of entry always began with the parental psychopathology that paralleled the child psychopathology being predicted. Thereafter, the order of parental comorbidity was selected based on the strength of the comorbid relationship between the primary and comorbid disorder, or the existing literature, which suggested a common genetic factor existed (e.g., alcohol-use disorder and antisocial personality disorder [Kendler et al., 2003], alcohol-use disorder and nicotine dependence [Jackson et al., 2000], major depressive disorder and nicotine dependence [Paperwalla et al., 2004]). Conditional on familial factors at baseline, we examined the impact of neighborhood factors at baseline. We hypothesized that neighborhood residential instability and neighborhood economic disadvantage during childhood would both have negative influences on youth symptomatology in late adolescence. Given the baseline predictors, the effects of longitudinal changes in neighborhood environments on adolescent symptomatology were tested. We hypothesized that family mobility and worsening neighborhood environments both contributed to more symptomatology during late adolescence.
Figure 1.
Theoretical framework for the impact of familial risk factors and developmental changes in neighborhood environment on substance-use disorders and other psychopathology outcomes in late adolescence. SES = socioeconomic status; AUD = alcohol-use disorder; MJUD = marijuana-use disorder; MDD = major depressive disorder; ASPD = antisocial personality disorder; ND = nicotine dependence.
Table 1.
Theoretical sequences of the influences of parental psychopathology on the mental health outcomes of offspring
| Step | Offspring AUD | Offspring MJUD | Offspring MDD | Offspring ASPD | Offspring ND |
| Step 1 | Parental AUD | Parental MJUD | Parental MDD | Parental ASPD | Parental ND |
| Step 2 | Parental ND | Parental ND | Parental AUD | Parental AUD | Parental MDD |
| Step 3 | Parental ASPD | Parental AUD | Parental ND | Parental MJUD, MDD, & ND | Parental AUD |
| Step 4 | Parental MDD | Parental ASPD | Parental MJUD & ASPD | Parental MJUD | |
| Step 5 | Parental MDD | Parental ASPD |
Notes: AUD = alcohol-use disorder; MJUD = marijuana-use disorder; MDD = major depressive disorder; ASPD = antisocial personality disorder; ND = nicotine dependence.
Method
Design and sample
Alcoholic families were ascertained through men with drunk-driving convictions in a four-county area involving a blood alcohol concentration of at least .15% (if first conviction) or at least .12% (if a previous drinking-related legal problem had occurred). They also needed to meet diagnosis for probable/definite alcoholism and, because of offspring studies also conducted with this sample, were required to have at least one 3- to 5-year-old biological son. Only male children were initially recruited into the study, because sons of male alcoholics are at highest risk for subsequent alcoholism (Zucker et al., 1995). Although subsequent funding allowed later assessments to include a female sibling, these girls joined the project at ages 6-11 and thus were not included in the analysis because of insufficient multiwave data. Recruitment criteria also required the men to be living with the child and his biological mother at the time of family consent. Alcoholic status of the mothers was free to vary. A contrast/control group of nonalcoholic families (neither parent with a history of substance use) was recruited through door-to-door canvassing in the same neighborhoods as the alcoholic families. This procedure also recruited an intermediate-risk group: families of parallel composition who had alcoholic fathers without a history of alcohol-related legal or drunk-driving problems occurring during the life of their child. Original recruitment of fathers used Feighner criteria (Feighner et al., 1972). As the study progressed, new diagnostic systems were introduced, and participants were rediagnosed using DSM-IV alcohol-use disorder criteria. A more detailed description of the study method is provided in an earlier report (Zucker et al., 2000).
Michigan Longitudinal Study families received extensive in-home assessments at baseline (Time 1: ages 3-5) and, thereafter, at 3-year intervals (e.g., Time 2: ages 6-8; Time 5: ages 15-17). In this study, we included only the 220 male target children of the participant families (all white) who had completed Time 6 (ages 18-20; i.e., who had outcome data available through late adolescence and the start of adulthood). The sample consists of 101 children (46%) recruited from court alcoholic families, 46 (21%) from community alcoholic families, and 73 (33%) from nonalcoholic families. Ninety-seven census tracts are represented. The average number of participants per census tract was 2, with a range of 1-10. All participants completed both Time 1 and Time 6 assessments, although the completion rates from Time 2 to Time 5 were 76%, 84%, 92%, and 95%, respectively. Missing assessments did not affect sample size because the analysis required only information on frequency of family mobility and change in neighborhood environment from Time 1 to Time 5.
Measures
Diagnostic Interview Schedule.
The Diagnostic Interview Schedule is a well-validated and widely used diagnostic instrument that gathers extensive information about psychiatric, physical, alcohol-related, and drug-related symptoms. The Diagnostic Interview Schedule-III (Robins et al., 1980) was administered at earlier waves, whereas the Diagnostic Interview Schedule-IV (Robins et al., 1996) was used for assessment in later waves. The total numbers of symptoms corresponding to the DSM-IV criteria for some disorders are different between the two versions. To make them comparable across waves, symptom counts from Diagnostic Interview Schedule-III data were prorated based on the Diagnostic Interview Schedule-IV counts. The numbers of possible symptoms were 11 for alcohol-use disorder, 10 for marijuana-use disorder, 9 for major depressive disorder, 7 for antisocial personality disorder, and 7 for nicotine dependence. Youth symptom counts on alcohol-use disorder, marijuana-use disorder, major depressive disorder, antisocial personality disorder, and nicotine dependence at Time 6 (ages 18-20) were used as mental health outcomes in late adolescence. Parental lifetime symptom counts on these disorders at baseline (when offspring were ages 3-5) were employed as the variables for parental psychopathology. Symptom counts, rather than diagnoses, were used because of their better statistical properties.
Family socioeconomic status.
At baseline, both biological parents filled out a demographic questionnaire that asked about his or her occupation. These data were coded for socioeconomic status based on the Duncan Socioeconomic Index, which was one of the best measures when our study began (Mueller and Parcels, 1981). The index is a continuous scale ranging from 0 (unemployed) to 9.04 (law professor). Family socioeconomic status was calculated by averaging the socioeconomic status coding of both parents.
Residential neighborhood characteristics.
Residential addresses of the 220 youth at Time 1 and Time 5 were matched with census tract coding at the census years (April 1 of 1980, 1990, or 2000) that were closest to the assessment dates. In this interval of approximately 12 years, the assessment dates of 87% of the participants correspond to 1990 and 2000 censuses, 10% correspond to 1980 and 2000 censuses, and 3% correspond to 1980 and 1990 censuses. During this period, 134 (61%) of the youth moved to different census tracts, making it likely that their neighborhood characteristics changed. For the participants who remained in the same census tract, census statistics for those neighborhoods also underwent change from Time 1 to Time 5 because of changes in local socioeconomic environment and resident composition. The following six neighborhood variables that may relate to individual substance use were computed to characterize neighborhood environments: (1) percentage of people living in different residence 5 years ago, (2) percentage of vacant households, (3) percentage of rented housing units, (4) adult unemployment rate, (5) poverty rate, and (6) percentage of people with education lower than high school diploma. Principal component analysis on baseline data was conducted to investigate the possibility of reducing the dimensions. Results showed that there were two major components: (1) the neighborhood residential instability component, with high loadings on the first three neighborhood variables (explaining 49% of the variance), and (2) the neighborhood economic disadvantage component, with high loadings on the rest of the three neighborhood variables (explaining 27% of the variance). To make the composite scores comparable from Time 1 to Time 5 because the loadings in each wave may vary, we constructed each of the two composite scores by averaging the three corresponding standardized census variables. We used these two composite scores at baseline (ages 3-5) as measures for their neighborhood risk factors in early childhood. The longitudinal change in neighborhood environments from Time 1 to Time 5 (ages 3-17) on each of the composite scores was measured with the change score between these two time points and categorized into three groups: (1) worse, (2) same, and (3) better, using the 25th and 75th percentiles of the difference scores as cutoff points.
Family mobility.
Family mobility frequency from Time 1 to Time 5 was calculated by comparing each child's addresses over the interval. This captured family moves every 3 years prospectively, instead of relying on self-report retrospective data. The resulting variable ranged from 0 to 4.
Analytic approach
Because psychopathology outcomes are discrete count variables, linear regression models based on the normality assumption are not applicable. We therefore employed the Poisson regression model, the most common method for discrete count variables (Agresti, 2002; Long, 1997), to examine the effects of familial and neighborhood risk factors in childhood and longitudinal changes in neighborhood environment on psychopathology outcomes during late adolescence. Following the theoretical framework presented in Figure 1, a Poisson regression model for each outcome was built through multiple stages. First, we tested the effects of parental lifetime psychopathology using the theoretical sequence for each disorder listed in Table 1. A particular parental lifetime symptom count stayed in the model if it had a significant effect (p < .05) above and beyond the effect of the parental psychopathology predictor(s) selected from previous step(s). After the submodel of parental psychopathology was built, it was tested to see if family socioeconomic status had an additional contribution (p < .05). If it did, it stayed in the final model; otherwise, it was excluded.
Given the influence of baseline familial factors, the impact of baseline neighborhood factors, including neighborhood residential instability and neighborhood economic disadvantage, was tested. These two variables stayed in the final model, regardless of their significance, because the impact of longitudinal changes in neighborhood environment is evident only when the initial neighborhood environment is considered. Finally, controlling for the baseline risk factors, the impact of longitudinal changes in neighborhood environment was tested. This block contains three sets of variables: (1) frequency of family mobility, (2) longitudinal changes on neighborhood residential instability, and (3) longitudinal changes on neighborhood economic disadvantage. Both the second and third sets contain two binary variables to contrast (i) the group whose neighborhood became worse with the group whose neighborhood remained the same (i.e., the control group) and (ii) the group whose neighborhood became better with the control group.
Results
Descriptive statistics
Table 2 lists descriptive statistics for childhood and longitudinal predictors and late adolescent outcomes. Because most of the variables are neither continuous nor distributed symmetrically, the median was a better statistic for central tendency. Minimum and maximum values are listed to describe the overall spread of the distribution. Fifty percent of the parents had at least one lifetime DSM-IV symptom on all the comorbid substance use or psychiatric disorders except marijuana-use disorder (median = 0.5). Among them, nicotine dependence had the highest median (2.5). The variances among the symptomatology of all these disorders were large. Median family socioeconomic status (2.90) was lower than the median of the scale (4.52). Examples of the occupations corresponding to the median socioeconomic status are receptionist (2.90) and optician (2.92).
Table 2.
Descriptive statistics of the baseline/longitudinal predictors and the psychopathology outcomes in late adolescence (N = 220)
| Variable | Median (SD) | Min. | Max. |
| Baseline familial factors (ages 3–5) | |||
| Parental lifetime AUD symptom count | 1.50 (1.87) | 0.00 | 7.50 |
| Parental lifetime MJUD symptom count | 0.50 (1.07) | 0.00 | 4.50 |
| Parental lifetime MDD symptom count | 1.00 (1.65) | 0.00 | 7.50 |
| Parental lifetime ASPD symptom count | 1.00 (1.09) | 0.00 | 4.00 |
| Parental lifetime ND symptom count | 2.50 (2.24) | 0.00 | 7.00 |
| Family SES | 2.90 (1.30) | 0.80 | 7.26 |
| Baseline neighborhood factors (ages 3–5) | |||
| Neighborhood residential instabilitya | −0.07 (0.85) | −1.58 | 3.46 |
| Neighborhood economic disadvantageb | −0.28 (0.88) | −1.20 | 2.90 |
| Longitudinal changes in neighborhood environments (ages 3–17) | |||
| Frequency of family mobility | 1.00 (0.90) | 0.00 | 4.00 |
| Change in neighborhood residential instabilityc | 0.13 (0.89) | −3.18 | 2.81 |
| Change in neighborhood economic disadvantagec | 0.02 (0.97) | −3.51 | 3.50 |
| Psychopathology outcomes in late adolescence (ages 18–20) | |||
| AUD symptom count | 1.00 (2.08) | 0.00 | 10.00 |
| MJUD symptom count | 0.00 (1.63) | 0.00 | 7.00 |
| MDD symptom count | 0.00 (2.60) | 0.00 | 9.00 |
| ASPD symptom count | 1.00 (1.77) | 0.00 | 7.00 |
| ND symptom count | 0.00 (1.21) | 0.00 | 5.00 |
Notes: Min. = minimum; max. = maximum; AUD = alcohol-use disorder; MJUD = marijuana-use disorder; MDD = major depressive disorder; ASPD = antisocial personality disorder; ND = nicotine dependence; SES = socio-economic status.
Composite score of three census variables: (1) percentage of people living in different residence 5 years ago, (2) percentage of vacant household, and (3) percentage of rented housing units;
composite score of three census variables: (1) adult unemployment rate, (2) poverty rate, and (3) percentage of people with education lower than high school diploma;
these variables are recoded into binary variables (using the 25th and 75th percentiles as cutoff points) to test the differences between the male children whose neighborhoods stayed the same and those children whose neighborhoods became worse/better.
Neighborhood variables are average scores from standardized census variables; therefore, their magnitudes do not make intuitive sense. To describe the baseline neighborhood characteristics, the means (SD) of the six census variables used to calculate the composite scores are (1) 46% (10%) lived in a different residence 5 years ago, (2) 4% (2%) of households were vacant, (3) 30% (16%) of housing units were rented, (4) 7% (4%) of adults were unemployed, (5) 11% (9%) were in poverty, and (6) 19% (8%) had no high school diploma.
At least 50% of the children in the study had moved during the 12-year interval (Time 1-Time 5). The longitudinal changes in neighborhood residential instability and neighborhood economic disadvantage from Time 1 to Time 5 are both approximately normal distributions with means around 0. We thus used the top and bottom 25% to define the groups of children whose neighborhood environment changed significantly positively or negatively. Fifty percent of the children already had at least one DSM-IV symptom on alcohol-use disorder and antisocial personality disorder by ages 18-20. As with their parents, there were large variances in the symptomatology of these youth.
Poisson regression models
Table 3 shows the final Poisson regression models with regression coefficients, standard errors, and statistical testing results. Controlling for parental lifetime alcohol-use disorder symptomatology, neither the other parental comorbid disorders nor family socioeconomic status had significant effects on youth alcohol-use disorder symptoms. In addition to parental marijuana-use disorder symptomatology, both parental nicotine dependence and family socioeconomic status contributed to youth marijuana-use disorder symptoms. For youth major depressive disorder symptoms, both parental antisocial personality disorder and family socioeconomic status had significant effects after controlling for parallel parental psychopathology. As with youth alcohol-use disorder symptoms, the isomorphic parental psychopathology was the only significant familial risk factor for youth antisocial personality disorder symptoms. Controlling for the influence of parental nicotine dependence, parental major depressive disorder and family socioeconomic status both had significant impact on youth nicotine-dependence symptoms.
Table 3.
Poisson regression of male target children's psychopathology outcomes in late adolescence (ages 18-20) on baseline familial/neighborhood factors and longitudinal changes in neighborhood environment (N = 220)
| Variable | AUD symptoms | MJUD symptoms | MDD symptoms | ASPD symptoms | ND symptoms |
| Intercept | 0.34* | −0.35* | 0.06 | 0.17 | −0.83* |
| (0.08) | (0.10) | (0.09) | (0.10) | (0.15) | |
| Baseline familial factors (ages 3-5) | |||||
| Parental AUD | 0.06* | – | – | – | – |
| (0.03) | |||||
| Parental MJUD | – | 0.22* | −0.11 | – | |
| (0.06) | (0.06) | ||||
| Parental MDD | – | – | 0.12* | – | 0.07* |
| (0.03) | (0.03) | ||||
| Parental ASPD | – | – | 0.16* | 0.19* | – |
| (0.04) | (0.05) | ||||
| Parental ND | – | 0.06* | – | – | 0.16* |
| (0.02) | (0.04) | ||||
| Family SES | – | −0.07* | −0.04* | – | −0.05* |
| (0.02) | (0.02) | (0.03) | |||
| Baseline neighborhood factors (ages 3-5) | |||||
| Neighborhood residential instability | 0.17* | 0.41* | 0.30* | 0.21* | 0.24* |
| (0.06) | (0.07) | (0.06) | (0.06) | (0.09) | |
| Neighborhood economic disadvantage | −0.10 | −0.13 | 0.05 | 0.03 | −0.01 |
| (0.07) | (0.08) | (0.06) | (0.06) | (0.09) | |
| Longitudinal changes in neighborhood environments (ages 3-17) | |||||
| Frequency of family mobility | 0.11 | 0.12 | −0.03 | 0.09 | 0.19* |
| (0.06) | (0.07) | (0.07) | (0.06) | (0.08) | |
| Becoming more stable | −0.30* | 0.05 | 0.04 | −0.07 | −0.01 |
| (0.14) | (0.16) | (0.14) | (0.13) | (0.18) | |
| Becoming less stable | −0.04 | −0.01 | 0.30* | 0.05 | −0.01 |
| (0.12) | (0.17) | (0.13) | (0.12) | (0.18) | |
| Becoming more affluent | 0.15 | −0.43* | −0.06 | −0.08 | −0.25 |
| (0.13) | (0.20) | (0.15) | (0.14) | (0.20) | |
| Becoming less affluent | −0.04 | 0.07 | −0.40* | −0.03 | −0.05 |
| (0.12) | (0.15) | (0.15) | (0.12) | (0.17) | |
Notes: The numbers in each cell are Poisson regression coefficients (standard error). AUD = alcohol-use disorder; MJUD = marijuana-use disorder; MDD = major depressive disorder; ASPD = antisocial personality disorder; ND = nicotine dependence; SES = socioeconomic status.
p < .05.
Baseline neighborhood residential instability had significant effects on all outcomes; this was above and beyond the contribution of the familial risk factors. On the other hand, baseline neighborhood economic disadvantage did not contribute additionally to any of the adolescent symptoms. Controlling for the effects of baseline risk factors and the patterns of longitudinal change in the neighborhood, the frequency of family mobility had no effect on any of the adolescent symptoms except for nicotine dependence. Children whose neighborhoods became more stable during the 12-year interval tended to have fewer alcohol-use disorder symptoms than those whose corresponding neighborhood environment stayed the same (i.e., the control), whereas children whose neighborhoods became less stable tended to have more major depressive disorder symptoms than the control. Moreover, children whose neighborhoods became more affluent tended to develop fewer marijuana-use disorder symptoms than the control. The only unexpected result was that children whose neighborhoods became less affluent developed fewer major depressive disorder symptoms than the control.
Discussion
Parental psychopathology effects
As expected for all substance-use disorder and psychopathology outcomes, the isomorphic parental symptomatology predicted the level of offspring psychopathology. However, other parental comorbidities differed in their degree of influence. For nicotine dependence, our findings are consistent with a genetic link between depression and smoking (Paperwalla et al., 2004; Quattrocki, 2000); after controlling for the effect of parent lifetime nicotine-dependence symptoms, parent lifetime major depressive disorder symptoms still predicted adolescent nicotine-dependence symptoms. Furthermore, parental lifetime nicotine-dependence symptoms predicted offspring development of not only isomorphic drug dependence but also the development of symptomatology on the other drug with a smoking route of delivery (marijuana). In addition, parent lifetime antisocial personality disorder predicted offspring antisocial personality disorder as well as major depressive disorder symptoms. Disorder-specific transmission existed only for alcohol-use disorder and antisocial personality disorder; for the other three disorders, parental comorbid psychopathology had significant effects.
There are two long-term risk identification implications for these findings. First, to prevent adolescent marijuana-use disorder, major depressive disorder, and nicotine dependence, targeting only those children whose parents have parallel symptom histories will omit other significant risk conveyed by parental comorbid psychiatric disorders. Second, because environmental risk factors from both the family and the neighborhood, above and beyond parental psychopathology, play a role in shaping these late-adolescent outcomes, an ecological approach to risk reduction that focuses on familial and neighborhood/community factors as well as individual risk is warranted.
Neighborhood residential instability
Our study shows that living in an unstable neighborhood where residents move in/out frequently during childhood is a significant contributor to the development of all five adolescent psychopathology outcomes. According to Sampson et al. (1997), neighborhood residential instability hinders the formation of social cohesion among neighbors and weakens their willingness to intervene on behalf of the common good. The association between neighborhood residential instability and youth psychopathology may be largely mediated by such low “collective efficacy.” Community efforts to improve neighborhood environments for youth development, such as providing support networks for families and building community-level institutions to supervise and monitor the behavior of residents, particularly using age-appropriate youth activities, may usefully reduce the risk for youth mental disorders. The findings that children whose neighborhoods become more stable from early childhood to adolescence tend to develop fewer alcohol-use disorder symptoms and children whose neighborhoods become less stable have more major depressive disorder symptoms shed some light on the potential of neighborhood intervention as a tool in the prevention armamentarium.
Neighborhood socioeconomic status versus family socioeconomic status
Findings also show that, although lower family socioeconomic status during childhood contributed to more marijuana-use disorder, major depressive disorder, and nicotine-dependence symptoms in late adolescence, neighborhood socioeconomic status (disadvantage) during childhood was not a predictor for adolescent psychopathology. This is not a surprising result in light of other studies that found family-level variables tended to be more strongly associated with individual outcomes than neighborhood-level variables. The relative contributions of these two levels of influence on children's mental health were quantified in a nationwide study of 2-year-old twins (Caspi et al., 2000): Environmental factors shared by members of a family accounted for 20% of the population variation in children's behavior problems, whereas neighborhood deprivation accounted for only 5% of this family-wide environmental effect.
Although neighborhood socioeconomic status during early childhood did not contribute to adolescent outcomes, controlling for familial risk factors, longitudinal changes in neighborhood economic environment over the course of childhood did. That is, a changing neighborhood environment during the 12-year interval of childhood and adolescence predicted the emergence of marijuana-use disorder as well as major depressive disorder symptomatology in late adolescence. However, the nature of this relationship was opposite across the two disorders, with an increase in neighborhood affluence predicting a lower level of marijuana symptoms and a decrease in neighborhood affluence predicting a lower level of major depressive disorder symptoms. The marijuana effect is the more straightforward one, involving more difficult access to illegal drugs with increasing neighborhood affluence (Storr et al., 2004). The major depressive disorder effect is not intuitively obvious, although an increasing literature has observed this association (Luthar, 2003; Schwartz, 2004).
Family mobility
Previous studies have observed a short-term effect of family mobility on adolescent substance use (Hoffmann, 2002; Trim and Chassin, 2008). We examined the long-term effect of family mobility after controlling for the patterns of longitudinal changes in neighborhood environment and other developmental risk factors and found that a higher frequency of family mobility predicted only a higher level of nicotine-dependence symptoms. Theoretical rationales for such an effect include heightened feelings of stress and anxiety, lessened parental supervision, and so on (DeWit, 1998). The nonsignificant effects of family mobility on the symptom levels of the other four disorders imply that it is where you move to, instead of how many times you move, that is going to make a difference.
Limitations and advantages
One obvious limitation in our work is the absence of any measures of peer influence. Our final models did not include peer factors because we chose to focus primarily on familial and neighborhood effects. Moreover, additional analysis did not find that participants' reports on both peers' substance use and delinquent behavior at Time 5 (ages 15-17) predicted their own psychopathology outcomes at Time 6 (ages 18-20) above and beyond the familial and neighborhood risk factors already included in the model. Future studies might probe these complex interactions among familial, neighborhood, and peer influences in an ecological framework, but this was beyond the scope of the present work.
Second, the study is observational rather than experimental; from that perspective, it is not the ideal design to establish causal inference. At the same time, it is virtually impossible to manipulate both the familial and neighborhood risk factors. Nevertheless, we carefully controlled for important confounding factors in the regression model. Moreover, we used risk factors measured over the course of childhood to predict psychiatric symptomatology in late adolescence. Thus, one may argue for the direction of causal relationship based on the time series of events.
Third, because of the family study design, a man recruited into the study had to reside with his son (ages 3-5) and the son's biological mother at the time of initial recruitment. This recruitment criterion reduces external validity to some degree, because results can be generalized only to children who were born in an initially coupled relationship and also only to families at a relatively early stage in the family life cycle.
Fourth, our analyses focus on only the developmental psy-chopathology of male children; therefore, the results cannot be generalized to girls. Because of the original recruitment protocol of the Michigan Longitudinal Study, only male target children had complete childhood data. Future studies need to test similar models involving female children from early childhood to study the impact of familial and neighborhood risk factors on their symptom development. A final limitation is that the study relies on relatively macrolevel census data to characterize neighborhood context; therefore, we cannot evaluate hypotheses about the microprocesses through which neighborhoods may influence children. The social organizational characteristics of neighborhoods—established by aggregating responses of individuals to community surveys in the same neighborhood—would allow for a more microlevel mechanistic examination of the neighborhood influencing process (cf. Sampson et al., 1997).
This study also has two distinct advantages that differentiate it from most other studies in this area. One is the young developmental stage of the families at the time of recruitment; another is the extended interval of a 15-year time span. This meant we were able to evaluate these familial and neighborhood effects across virtually the entire span of childhood and adolescence rather than just a portion of that time. The narrow recruitment age range of the children also meant that these effects would not be diluted or confounded by the developmental heterogeneity of the sample at the time the contextual influences were operating.
Acknowledgments
The authors thank Susan Refior and Wei Wang for their invaluable assistance with the initial data collection (SR) and in the preparation of this manuscript (WW).
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R37 AA-07065 to Robert A. Zucker and Hiram E. Fitzgerald.
References
- Agresti A. Categorical Data Analysis. 2nd Edition. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcsm Clin. Exp. Res. 2007;31:1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Taylor A, Moffitt TE, Plomin R. Neighborhood deprivation affects children's mental health: Environmental risks identified in a genetic design. Psychol. Sci. 2000;11:338–342. doi: 10.1111/1467-9280.00267. [DOI] [PubMed] [Google Scholar]
- DeWit DJ. Frequent childhood geographic relocation: Its impact on drug use initiation and the development of alcohol and other drug-related problems among adolescents and young adults. Addict. Behav. 1998;23:623–634. doi: 10.1016/s0306-4603(98)00023-9. [DOI] [PubMed] [Google Scholar]
- Dierker LC, Merikangas KR, Szatmari P. Influence of parental concordance for psychiatric disorders on psychopathology in offspring. J. Amer. Acad. Child Adolesc. Psychiat. 1999;38:280–288. doi: 10.1097/00004583-199903000-00015. [DOI] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults' outcomes. Social Sci. Med. 2004;59:2271–2284. doi: 10.1016/j.socscimed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Early impacts of moving from poor to middle-class neighborhoods on low-income youth. J. Appl. Devel. Psychol. 2005;26:415–439. [Google Scholar]
- Fauth RC, Roth JL, Brooks-Gunn J. Does the neighborhood context alter the link between youth's after-school time activities and developmental outcomes? A multilevel analysis. Devel. Psychol. 2007;43:760–777. doi: 10.1037/0012-1649.43.3.760. [DOI] [PubMed] [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA, Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch. Gen. Psychiat. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Hoffmann JP. The community context of family structure and adolescent drug use. J. Marr. Fam. 2002;64:314–330. [Google Scholar]
- Jackson KM, Sher KJ, Wood PK. Prospective analysis of comor-bidity: Tobacco and alcohol use disorders. J. Abnorm. Psychol. 2000;109:679–694. doi: 10.1037//0021-843x.109.4.679. [DOI] [PubMed] [Google Scholar]
- Katz LF, Kling JR, Liebman JB. Moving to opportunity in Boston: Early results of a randomized mobility experiment. Q. J. Econ. 2001;116:607–654. [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch. Gen. Psychiat. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75:83–119. [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. Amer. J. Commun. Psychol. 2004;34:205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychol. Bull. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving to opportunity: An experimental study of neighborhood effects on mental health. Amer. J. Publ. Hlth. 2003;93:1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JS. Regression Models for Categorical and Limited Dependent Variables. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- Luthar SS. The culture of affluence: Psychological costs of material wealth. Child Devel. 2003;74:1581–1593. doi: 10.1046/j.1467-8624.2003.00625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cushing G. Neighborhood influences and child development: A prospective study of substance abusers' offspring. Devel. Psychopathol. 1999;11:763–784. doi: 10.1017/s095457949900231x. [DOI] [PubMed] [Google Scholar]
- Mueller CW, Parcel TL. Measures of socioeconomic status: Alternatives and recommendations. Child Devel. 1981;52:13–30. [Google Scholar]
- Paperwalla KN, Levin TT, Weiner J, Saravay SM. Smoking and depression. Med. Clin. No. Amer. 2004;88:1483–1494. doi: 10.1016/j.mcna.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Quattrocki E, Baird A, Yurgelun-Todd D. Biological aspects of the link between smoking and depression. Harvard Rev. Psychiat. 2000;8:99–110. [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. The National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics and validity. Arch. Gen. Psychiat. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Robins L, Marcus L, Reich W, Cunningham R, Gallagher T. NIMH Diagnostic Interview Schedule, Version IV (DIS-IV) St. Louis, MO: Washington University School of Medicine; 1996. [Google Scholar]
- Roche KM, Ensminger ME, Cherlin AJ. Variations in parenting and adolescent outcomes among African American and Latino families living in low-income, urban areas. J. Fam. Issues. 2007;28:882–909. [Google Scholar]
- Rubinowitz LS, Rosenbaum JE. Crossing the Class and Color Lines: From Public Housing to White Suburbia. Chicago, IL: Univ. of Chicago Press; 2000. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime:A multi level study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schwartz B. The Paradox of Choice: Why More is Less. New York: Harper Collins; 2004. [Google Scholar]
- Storr CL, Chen C-Y, Anthony JC. “Unequal opportunity”: Neighborhood disadvantage and the chance to buy illegal drugs. J. Epidemiol. Commun. Hlth. 2004;58:231–237. doi: 10.1136/jech.2003.007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas AJ, Eberly LE, Smith GD, Neaton JD for the Multiple Risk Factor Intervention Trial (MRFIT) Research Group. Zip-code-based versus tract-based income measures as long-term risk-adjusted mortality predictors. Amer. J. Epidemiol. 2006;164:586–590. doi: 10.1093/aje/kwj234. [DOI] [PubMed] [Google Scholar]
- Trim RS, Chassin L. Neighborhood socioeconomic status effects on adolescent alcohol outcomes using growth models: Exploring the role of parental alcoholism. J. Stud. Alcohol Drugs. 2008;69:639–648. doi: 10.15288/jsad.2008.69.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend. 2008;92:173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Fitzgerald HE, Moses HD. Emergence of alcohol problems and the several alcoholisms: A developmental perspective on etiologic theory and life course trajectory. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology, Vol. 2: Risk, Disorder, and Adaptation. Hoboken, NJ: John Wiley & Sons; 1995. pp. 677–711. [Google Scholar]
- Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implications for a differentiated social policy. In: Fitzgerald HE, Lester BM, Zuckerman BS, editors. Children of Addiction: Research, Health, and Public Policy Issues. New York: Routledge Falmer; 2000. pp. 109–141. [Google Scholar]