Abstract
Objective
Develop a cerebrospinal fluid biomarker signature for mild Alzheimer’s disease (AD) in Alzheimer’s Disease Neuroimaging Initiative (ADNI) subjects.
Methods
Amyloid-β 1 to 42 peptide (Aβ1-42), total tau (t-tau), and tau phosphorylated at the threonine 181 were measured in (1) cerebrospinal fluid (CSF) samples obtained during baseline evaluation of 100 mild AD, 196 mild cognitive impairment, and 114 elderly cognitively normal (NC) subjects in ADNI; and (2) independent 56 autopsy-confirmed AD cases and 52 age-matched elderly NCs using a multiplex immunoassay. Detection of an AD CSF profile for t-tau and Aβ1-42 in ADNI subjects was achieved using receiver operating characteristic cut points and logistic regression models derived from the autopsy-confirmed CSF data.
Results
CSF Aβ1-42 was the most sensitive biomarker for AD in the autopsy cohort of CSF samples: receiver operating characteristic area under the curve of 0.913 and sensitivity for AD detection of 96.4%. In the ADNI cohort, a logistic regression model for Aβ1-42, t-tau, and APOε4 allele count provided the best assessment delineation of mild AD. An AD-like baseline CSF profile for t-tau/Aβ1-42 was detected in 33 of 37 ADNI mild cognitive impairment subjects who converted to probable AD during the first year of the study.
Interpretation
The CSF biomarker signature of AD defined by Aβ1-42 and t-tau in the autopsy-confirmed AD cohort and confirmed in the cohort followed in ADNI for 12 months detects mild AD in a large, multisite, prospective clinical investigation, and this signature appears to predict conversion from mild cognitive impairment to AD.
If the clinical diagnosis of probable AD is imprecise with accuracy rates of approximately 90% or lower using established consensus criteria for probable AD, but definite AD requires autopsy confirmation, it is not surprising that diagnostic accuracy is lower at early and presymptomatic stages of AD.1–4 It is believed that the development of full-blown AD takes place over an approximately 20-year prodromal period, but this is difficult to determine in the absence of biomarkers that reliably signal the onset of nascent disease before the emergence of measurable cognitive impairments. Because intervention with disease-modifying therapies for AD is likely to be most efficacious before significant neurodegeneration has occurred, there is an urgent need for biomarker-based tests that enable a more accurate and early diagnosis of AD.5–7 Moreover, such tests could also improve monitoring AD progression, evaluation of new AD therapies, and enrichment of AD cohorts with specific subsets of AD subjects in clinical trials.
The defining lesions of AD are neurofibrillary tangles and senile plaques formed, respectively, by neuronal accumulations of abnormal hyperphosphorylated tau filaments and extracellular deposits of amyloid β (Aβ) fibrils, mostly the 1 to 42 peptide (Aβ1-42), the least soluble of the known Aβ peptides produced from Aβ precursor protein by the action of various peptidases.1–3 Hence, for these and other reasons summarized in consensus reports on AD biomarkers, cerebrospinal fluid (CSF), total tau (t-tau), and Aβ were identified as being among the most promising and informative AD biomarkers.5,6 Increased levels of tau in CSF are thought to occur after its release from damaged and dying neurons that harbor dystrophic tau neurites and tangles, whereas reduced CSF levels of Aβ1-42 are believed to result from large-scale accumulation of this least soluble of Aβ peptides into insoluble plaques in the AD brain. The combination of increased CSF concentrations of t-tau and phosphotau (p-tau) species and decreased concentrations of Aβ1-42 are considered to be a pathological CSF biomarker signature that is diagnostic for AD.5,6,8,9 Notably, recent studies have provided compelling preliminary data to suggest that this combination of CSF tau and Aβ biomarker changes may predict the conversion to AD in mild cognitive impairment (MCI) subjects.10 Thus, an increase in levels of CSF tau associated with a decline in levels of CSF Aβ1-42 may herald the onset of AD before it becomes clinically manifest.
However, before the utility of CSF Aβ1-42 and tau concentrations for diagnosis of AD can be established, it is critical to standardize the methodology for their measurement.5–8,10 For example, among the published studies of CSF tau and Aβ, there is considerable variability in the observed levels of these analytes, as well as their diagnostic sensitivity and specificity. This is attributable to variability in analytical methodology standardization and other factors that differ between studies of the same CSF analytes in similar but not identical cohorts.5–7
The Alzheimer’s Disease Neuroimaging Initiative (ADNI) was launched in 2004 to address these and other limitations in AD biomarkers (see reviews in Shaw and colleagues7 and Mueller and coauthors,11 and the ADNI Web site [http://www.adni-info.org/index] where the ADNI grant and all ADNI data are posted for public access). To this end, the Biomarker Core of ADNI conducts studies on ADNI-derived CSF samples to measure CSF Aβ1-42, t-tau, and p-tau (tau phosphorylated at threonine181 [p-tau181p]) in standardized assays. Evaluation of CSF obtained at baseline evaluation of 416 of the 819 ADNI subjects is now complete, and we report here our findings on the performance of these tests using a standardized multiplex immunoassay system that measures the biomarkers simultaneously in the same sample aliquot in ADNI subjects and in an independent cohort of autopsy-confirmed AD cases.
Subjects and Methods
The ADNI is a large, multicenter, longitudinal neuroimaging study, launched in 2004 by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, the Food and Drug Administration, private pharmaceutical companies, and nonprofit organizations. ADNI includes 819 adult subjects, 55 to 90 years old, who meet entry criteria for a clinical diagnosis of amnestic MCI (n = 397), probable AD (n = 193), or normal cognition (n = 229). Participants receive baseline and periodic physical and neurological examinations and standardized neuropsychological assessments, and provide biological samples (blood, urine, and in a subset, CSF) throughout the study. Imaging (magnetic resonance imaging and for a subset, F-fluorodeoxyglucose positron emission tomography and Pittsburgh compound B positron emission tomography) is performed at baseline and at regular intervals thereafter (for reviews and more details, see Shaw and colleagues,7 Mueller and coauthors,11 and http://www.adni-info.org/). All AD subjects met National Institute of Neurological and Communication Disorders/Alzheimer’s Disease and Related Disorders Association criteria for probable AD with a Mini-Mental State Examination score between 20 and 26, a global Clinical Dementia Rating of 0.5 or 1, a sum-of-boxes Clinical Dementia Rating of 1.0 to 9.0, and, therefore, are only mildly impaired. Entry criteria for amnestic MCI subjects include a Mini-Mental State Examination score of 24 to 30 and a Memory Box score of at least 0.5, whereas other details on the ADNI cohort can be found online at: http://www.nia.nih.gov/Alzheimers/ResearchInformation/ClinicalTrials/ADNI.htm. In brief, exclusion criteria included any serious neurological disease other than possible AD, any history of brain lesions or head trauma, or psychoactive medication use (including antidepressants, neuroleptics, chronic anxiolytics, or sedative hypnotics).
Baseline CSF samples were obtained in the morning after an overnight fast from 416 ADNI subjects (AD = 102, MCI = 200, NC = 114 with average [± standard deviation] ages of 75 ± 8, 75 ± 7, and 76 ± 5 years, respectively; Table 1) from individuals enrolled at 56 participating centers at the time the subjects entered ADNI (ie, baseline). Their demographic, clinical, and APOε genotyping results are comparable with that in the full ADNI patient population (http://www.adni-info.org/index). Lumbar puncture was performed with a 20- or 24-gauge spinal needle as described in the ADNI procedures manual (http://www.adni-info.org/). In brief, CSF was collected into collection tubes provided to each site, then transferred into polypropylene transfer tubes followed by freezing on dry ice within 1 hour after collection, and shipped overnight to the ADNI Biomarker Core laboratory at the University of Pennsylvania Medical Center on dry ice. Aliquots (0.5ml) were prepared from these samples after thawing (1 hour) at room temperature and gentle mixing. The aliquots were stored in bar code–labeled polypropylene vials at −80°C. Written informed consent was obtained for participation in these studies, as approved by the institutional review board at each participating center.
Table 1.
Demographic Characteristics of Alzheimer’s Disease Neuroimaging Initiative Study Subjects Who Provided a Cerebrospinal Fluid Sample at the Baseline Visit
| Characteristics | AD | MCI | NC |
|---|---|---|---|
| n | 100 | 196 | 114 |
| Sex, M/F | 58/42 (58%) | 131/65 (67%) | 58/56 (51%) |
| Age, yr | |||
| Median | 76 | 75 | 76 |
| Mean ± SD | 75 ± 8 | 75 ± 7 | 76 ± 5 |
| 95% CI | 73–77 | 74–76 | 75–77 |
| MMSE score | |||
| Median | 24 | 27 | 29 |
| Mean ± SD | 23.5 ± 1.9 | 26.9 ± 1.8 | 29.1 ± 1.0 |
| 95% CI | 23.2–23.9 | 26.7–27.2 | 28.9–29.3 |
| ADAS Cog 11 | |||
| Median | 17.2 | 11.3 | 6.3 |
| Mean ± SD | 18.2 ± 6.2 | 11.6 ± 4.5 | 6.4 ± 2.9 |
| 95% CI | 16.9–19.4 | 11–12.3 | 5.9–6.9 |
| ApoE ε4+/ε4− | 69/31 (69%) | 106/90 (54%) | 27/87 (24%) |
AD = Alzheimer’s disease; MCI = mild cognitive impairment; NC = cognitively normal; SD = standard deviation; CI = confidence interval; MMSE = Mini-Mental State Examination; ApoE = apolipoprotein; ADAS Cog 11 = Alzheimers Disease Assessment Scale-cognitive subscale 11.
An independent set of premortem CSF samples from 56 autopsy-confirmed AD cases and 52 cognitively normal elderly subjects followed by the University of Pennsylvania Alzheimer’s Disease Clinical Core provided an independent analysis sample set that was matched with the ADNI samples with respect to age (mean ± standard deviation [95% confidence interval]: 71 ± 10 [69–74] and 70 ± 11 [67–73] years, respectively) at the time of their lumbar puncture. The cases and control subjects were evaluated and followed as described previously,12–14 and all of these CSF samples were collected at University of Pennsylvania Alzheimer’s Disease Clinical Core using standardized methodology including storage of aliquots in polypropylene vials maintained in the repository at −80°C.12–14 Written informed consent was obtained for participation in these studies, which was approved by the University of Pennsylvania Institutional Review Board.
Aβ1-42, t-tau, and p-tau181p were measured in each of the 416 CSF ADNI baseline aliquots using the multiplex xMAP Luminex platform (Luminex Corp, Austin, TX) with Innogenetics (INNO-BIA AlzBio3; Ghent, Belgium; for research use–only reagents) immunoassay kit–based reagents. Full details of this combination of immunoassay reagents and analytical platform are provided elsewhere.15,16 In brief, Innogenetics kit reagents included well-characterized capture monoclonal antibodies specific for Aβ1-42(4D7A3), t-tau(AT120), and p-tau181p (AT270), each chemically bonded to unique sets of color-coded beads, and analyte-specific detector antibodies (HT7, 3D6). Calibration curves were produced for each biomarker using aqueous buffered solutions that contained the combination of three biomarkers at concentrations ranging from 56 to 1,948pg/ml for recombinant tau, 27 to 1,574pg/ml for synthetic Aβ1-42 peptide, and 8 to 230pg/ml for a tau synthetic peptide phosphorylated at the threonine 181 position (ie, the p-tau181p standard). Before performing these analyses of the ADNI and the independent autopsy-based CSF samples in the ADNI University of Pennsylvania ADNI Biomarker Core laboratory, an interlaboratory study was conducted to qualify the performance conditions, including all major variables that can affect the test results, for the immunoassay reagents and analytical platform. These studies were conducted using strategies and procedures to standardize the assay similar to those that Vanderstichele and colleagues16 described. This investigation (Shaw and colleagues, manuscript in preparation, but see summary of these data online at: http://www.adni-info.org/) provided the basis for achieving day-to-day reproducibility for the three biomarkers of less than 10% variation for CSF pool samples and less than 7% for aqueous quality controls. The ADNI baseline CSF samples were analyzed over a 14-day period and included test–retest analyses of 29 of the samples that further substantiated the analytical performance (r2 values for comparison of initial test result with retest result of 0.98, 0.90, and 0.85 for t-tau, Aβ1-42, and p-tau181p, respectively for 29 randomly selected samples). Only subjects with a valid test result for all 3 biomarkers are included in this study, that is, 114 NC, 196 MCI, and 100 AD subjects.
APOε genotyping was done for all ADNI study candidates using EDTA blood samples collected at the screening visit (see Table 1). TaqMan quantitative polymerase chain reaction assays were used for genotyping APOε nucleotides 334 T/C and 472 CT with an ABI 7900 real-time thermo-cycler (Applied Biosystems, Foster City, CA) using DNA freshly prepared from EDTA whole blood. A total of 96 samples randomly selected from the total of 1,131 subjects screened before inclusion (or exclusion) into the ADNI study were retested by sequencing using an ABI 3130 sequencer (Applied Biosystems). Except for the 5 samples that failed to sequence, the remaining 91 were concordant with the Taq-Man genotyping results.
Receiver operating characteristic curve (ROC) and logistic regression (LR) analyses were done using SAS v 9.1.3 (SAS Institute, Cary, NC) and R v 2.7.1. Between-group differences for each biomarker were assessed by the Mann–Whitney U test using GraphPad Prism, v 5.
Results
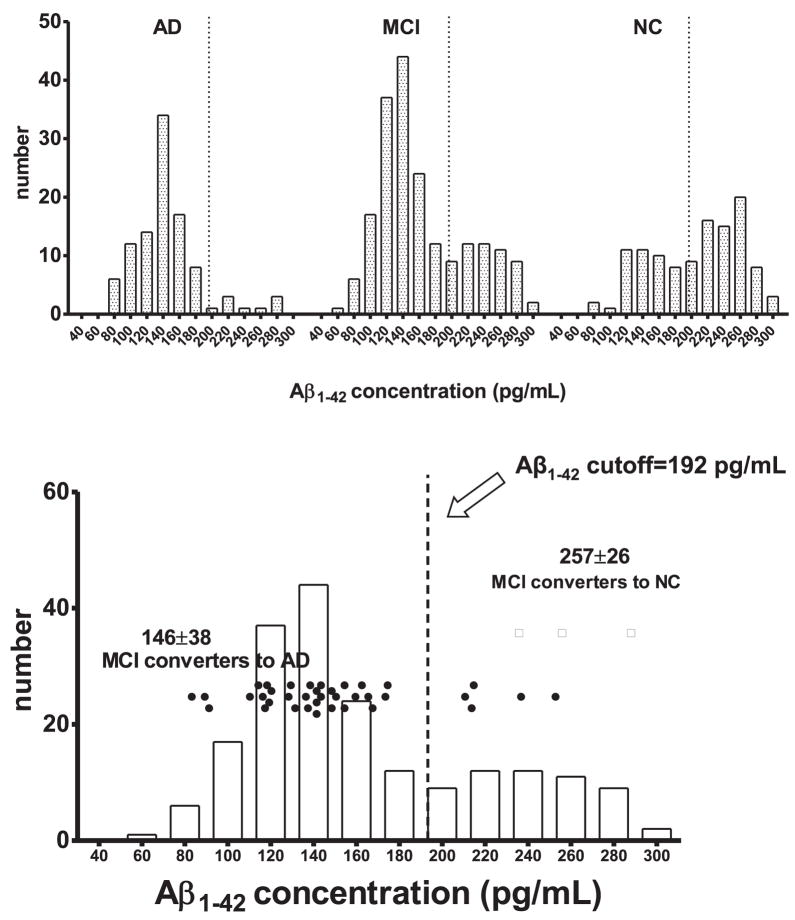
Mean ± standard deviation values for CSF t-tau, Aβ1-42, p-tau181p, t-tau/Aβ1-42 and p-tau181p/Aβ1-42, for the ADNI AD, MCI, and NC study groups are summarized in Table 2. These data confirm the findings of the majority of single and smaller multicenter studies for these biomarkers in AD subjects wherein most investigators report increases in t-tau, p-tau181p concentrations, t-tau/Aβ1-42, and p-tau181p/Aβ1-42 ratio values when comparing NC with MCI, and then further increases in these values when comparing MCI with AD.7–10,12–16 Aβ1-42 average concentrations, on the other hand, decrease when comparing NC with MCI, then decrease further in comparing MCI with AD.7–10,12–16 Closer examination of the distribution of each biomarker and ratios demonstrated that the distributions are not normal, and for Aβ1-42, the distributions appear to be bimodal (Fig 1). Typical published single enzyme-linked immunosorbent assay test values for tau and Aβ1-42 are generally up to two to four times greater than with the multiplex xMAP Lumnex platform using the INNO-BIA AlzBio3 immunoassay reagents, although the two methods correlate well with each other and provide equivalent diagnostic performance when CSF samples are analyzed by both methods within the same study.15–17 In the ADNI Biomarker Core, we observed single-test enzyme-linked immunosorbent assay t-tau concentrations approximately 4-fold greater, Aβ1-42 approximately 2-fold greater, and p-tau181p approximately 25% greater than xMAP (data not shown). The differences in the absolute values between the two assay formats could be related to differences in the monoclonal antibodies used, assay test conditions (time, temperature, multiplexing), and/or the fact that the calibrators are not produced in the same matrix (CSF).
Table 2.
Cerebrospinal Fluid Biomarker Concentrations and Ratios in Alzheimer’s Disease Neuroimaging Initiative Study Subjects at Baseline
| Characteristics | tau (pg/ml) | Aβ1–42 (pg/ml) | p-tau181p (pg/ml) | tau/Aβ1–42 Ratio | p-tau181p/Aβ1–42 Ratio |
|---|---|---|---|---|---|
| AD (n = 100) | |||||
| Median | 110 | 138 | 36 | 0.86 | 0.29 |
| Mean ± SD | 122 ± 58 | 144 ± 41 | 42 ± 20 | 0.92 ± 0.48 | 0.32 ± 0.19 |
| 95% CI | 110–133 | 135–152 | 38–46 | 0.82–1.0 | 0.28–0.36 |
| MCI (n = 196) | |||||
| Median | 86 | 146 | 32 | 0.62 | 0.23 |
| Mean ± SD | 103 ± 61 | 164 ± 55 | 36 ± 18 | 0.75 ± 0.62 | 0.26 ± 0.18 |
| 95% CI | 95–112 | 156–171 | 33–38 | 0.66–0.84 | 0.24–0.29 |
| NC (n = 114) | |||||
| Median | 61 | 217 | 20 | 0.31 | 0.10 |
| Mean ± SD | 70 ± 30 | 206 ± 55 | 25 ± 15 | 0.39 ± 0.27 | 0.14 ± 0.13 |
| 95% CI | 64–75 | 195–216 | 22–28 | 0.34–0.43 | 0.12–0.17 |
| MCI→AD (n = 37)a | |||||
| Median | 93 | 139 | 40 | 0.71 | 0.28 |
| Mean ± SD | 107 ± 54 | 146 ± 38 | 42 ± 18 | 0.81 ± 0.47 | 0.32 ± 0.17 |
| 95% CI | 89–125 | 133–159 | 36–48 | 0.64–0.95 | 0.26–0.37 |
| MCI→normal (n = 3)b | |||||
| Median | 73 | 253 | 21 | 0.29 | 0.08 |
| Mean ± SD | 75 ± 7 | 257 ± 26 | 22 ± 3 | 0.29 ± 0.02 | 0.09 ± 0.02 |
| 95% CI | 57–93 | 192–322 | 15–29 | 0.24–0.34 | 0.03–0.14 |
Mann–Whitney test: p < 0.0001, for each of the five biomarker tests for Alzheimer’s disease (AD) vs cognitively normal (NC) and for mild cognitive impairment (MCI) vs NC. For AD vs MCI: p < 0.005, tau; p < 0.05, amyloid–β 1 to 42 peptide (Aβ1–42); p < 0.01, tau phosphorylated at the threonine 181 position (p-tau181p); p < 0.0005, tau/Aβ1–42; p < 0.005, p-tau181p/Aβ1–42. p < 0.0001 for MCI converters to AD vs NC for each of the biomarkers and ratios.
Alzheimer’s Disease Neuroimaging Initiative (ADNI) MCI subjects who converted to a clinical diagnosis of probable AD at 1 year.
ADNI MCI subjects who converted to cognitively normal at 1 year. SD = standard deviation; CI = confidence interval.
Fig 1.
(A) Frequency distribution of cerebrospinal fluid (CSF) amyloid-β 1 to 42 peptide (Aβ1-42) concentration in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Alzheimer’s disease (AD), mild cognitive impairment (MCI), and cognitively normal (NC) groups at their baseline visit. Dotted vertical lines within each diagnosis is the Aβ1-42 cutoff concentration of 192pg/ml determined from the ADNI-independent autopsy-based AD CSF samples. (B) Aβ1-42 concentrations in CSF, collected at the baseline visit, of 37 ADNI MCI subjects who at their 1-year visit converted to a diagnosis of probable AD. Data points for the MCI→AD converters are presented as a horizontal dot plot with the x-axis scale identical to that of the Aβ1-42 frequency plot for the entire ADNI MCI group.
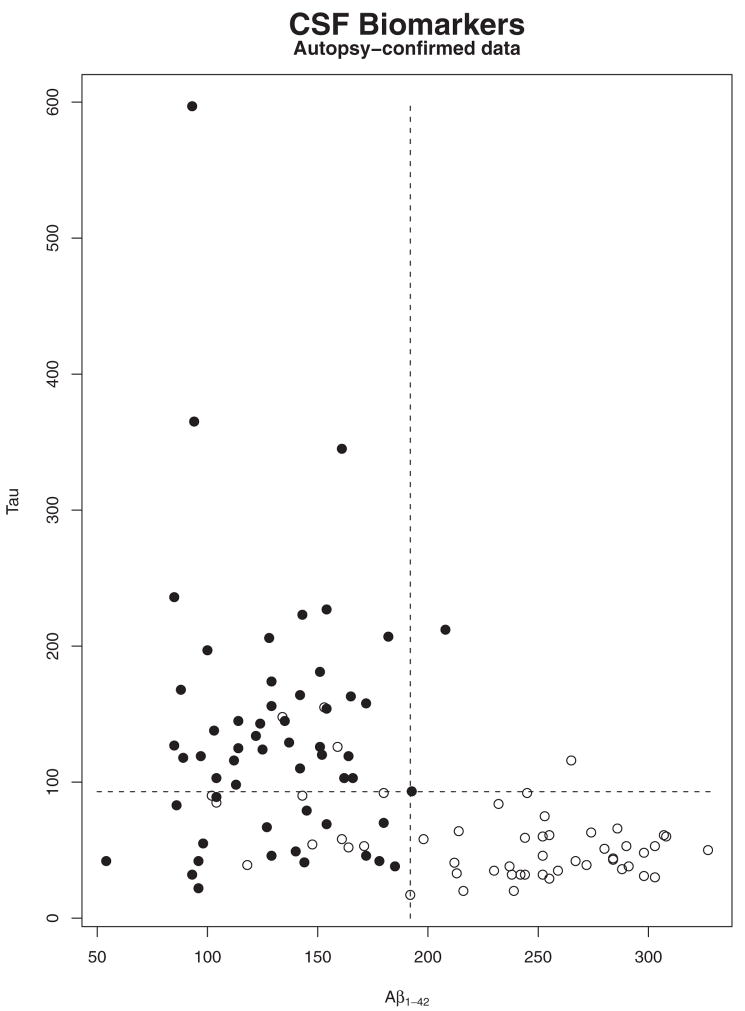
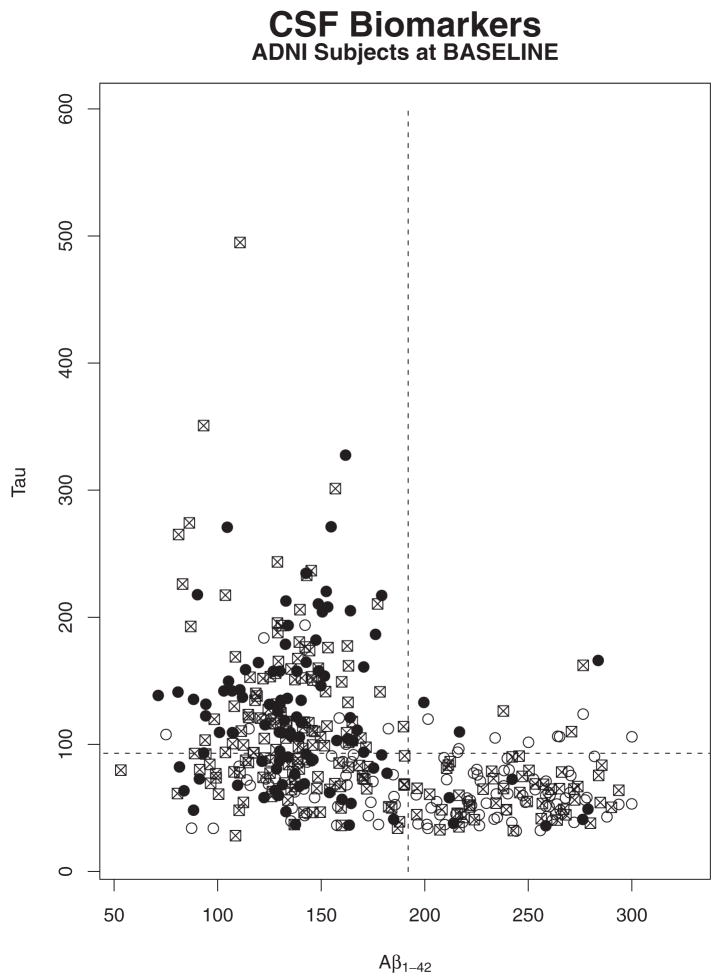
Premortem CSF was obtained from separate, ADNI-independent groups of autopsy-confirmed AD cases and additional NC subjects who were matched for age to provide a pathological basis for these biomarker measurements. The CSF t-tau, p-tau181p, and Aβ1-42 concentrations of these individuals were measured using the same reagents and assay system described earlier for the baseline CSF samples from ADNI subjects. These data are summarized in Table 3. The same trends for each of the mean concentrations or ratio values for the t-tau and Aβ biomarker parameters were observed for these ADNI-independent subjects and autopsy-confirmed AD cases, as well as in the age-matched ADNI-independent NC group as observed for the ADNI AD and NC cohorts (see Table 3 and compare Figs 2 and 3).
Table 3.
Cerebrospinal Fluid Biomarker Concentrations and Ratios in Non–Alzheimer’s Disease Neuroimaging Initiative Samples Collected before Autopsy for Alzheimer’s Disease and an Age-Matched Elderly Cognitively Normal Control Group
| Characteristics | tau (pg/ml) | Aβ1–42 (pg/ml) | p-tau181p(pg/ml) | tau/Aβ1–42 Ratio | p-tau181P/Aβ1–42 Ratio |
|---|---|---|---|---|---|
| AD (n = 56) | |||||
| Median | 122 | 129 | 29 | 1.0 | 0.2 |
| Mean ± SD | 135 ± 95 | 132 ± 34 | 39 ±29 | 1.1 ± 1.0 | 0.3 ± 0.2 |
| 95% CI | 110–161 | 123–141 | 31–47 | 0.9–1.4 | 0.2–0.4 |
| NC (n = 52) | |||||
| Median | 52 | 245 | 13 | 0.2 | 0.06 |
| Mean ± SD | 57 ± 30 | 233 ± 58 | 18 ±16 | 0.3 ± 2 | 0.1 ± 0.1 |
| 95% CI | 49–65 | 217–250 | 14–23 | 0.2–0.4 | 0.06–0.1 |
Mann–Whitney test: p < 0.0001 for each biomarker or ratio for Alzheimer’s disease (AD) vs cognitively normal (NC). Aβ1–42 =amyloid-β 1 to 42 peptide; p-tau181p = tau phosphorylated at the threonine 181 position; SD = standard deviation; CI = confidence interval.
Fig 2.
Plot of cerebrospinal fluid (CSF) tau concentration versus CSF amyloid-β 1 to 42 peptide (Aβ1-42) concentration for the autopsy-confirmed Alzheimer’s disease (AD) cases (solid circles) and elderly cognitively normal (NC) subjects (open circles).
Fig 3.
Plot of cerebrospinal fluid (CSF) tau concentration versus CSF amyloid-β 1 to 42 peptide (Aβ1-42) concentration for the Alzheimer’s Disease Neuroimaging Initiative (ADNI) probable Alzheimer’s disease (AD; solid circles), mild cognitive impairment (MCI; squares), and elderly cognitively normal (NC; open circles) subjects.
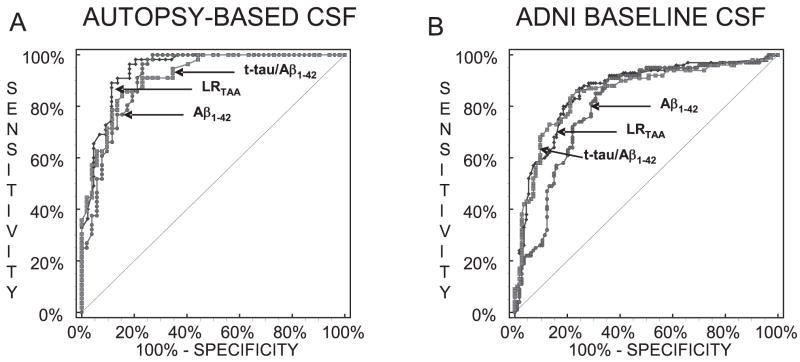
ROC analyses of the autopsy-confirmed AD cases versus the NC group provided cutpoint concentrations achieved at the greatest diagnostic test accuracy and assessments of the diagnostic sensitivity and specificity, and the positive and negative predictive values for the biomarker measurements as summarized in Table 4. The greatest ROC area under the curve (AUC) value for a single parameter was obtained for Aβ1-42 (0.913). This biomarker had the greatest sensitivity value (96.4%) and negative predictive value of 95.2% (ie, the probability that AD is not present when the test is negative, ie, when CSF Aβ1-42 concentration is greater than the cutoff value of 192pg/ml and comparing AD with NC subjects), and diagnostic test accuracy (87.0%) (ie, the percentages of all results for the AD vs NC groups that are classified correctly) of the three single biomarkers or the two biomarker ratios (see Table 4). The diagnostic specificity for Aβ1-42 was 76.9%. The diagnostic specificity for t-tau, on the other hand, was 92.3%, and the greater for all five test parameters was the positive predictive value of 90.7% (ie, the probability that the disease is present when the t-tau CSF concentration value is greater than the cutoff concentration value of 93pg/ml). The test accuracy and sensitivity were 80.6 and 69.6%, respectively, for t-tau. For the t-tau/Aβ1-42 ratio, the AUC value is 0.917, the sensitivity and specificity values are 85.7 and 84.6%, the test accuracy is 85.2%, positive predictive value is 85.7%, and negative predictive value is 84.6%.
Table 4.
Receiver Operating Characteristic Curve Parameters for Non–Alzheimer’s Disease Neuroimaging Initiative Autopsy-Based Alzheimer’s Disease Cases versus Cognitively Normal Subjects
| Parameters | tau | Aβ1–42 | p-tau181p | tau/Aβ1–42 | p-tau181p/Aβ1–42 | LRTAA Model |
|---|---|---|---|---|---|---|
| ROC AUC | 0.831 | 0.913 | 0.753 | 0.917 | 0.856 | 0.942 |
| Threshold value | 93pg/ml | 192pg/ml | 23pg/ml | 0.39 | 0.10 | 0.34 |
| Sensitivity (%) | 69.6 | 96.4 | 67.9 | 85.7 | 91.1 | 98.2 |
| Specificity (%) | 92.3 | 76.9 | 73.1 | 84.6 | 71.2 | 79.5 |
| Test accuracy (%) | 80.6 | 87.0 | 70.4 | 85.2 | 81.5 | 89.9 |
| Positive predictive value (%) | 90.7 | 81.8 | 73.1 | 85.7 | 77.3 | 85.7 |
| Negative predictive value (%) | 73.8 | 95.2 | 67.9 | 84.6 | 88.1 | 97.2 |
Aβ1–42= amyloid-β 1 to 42 peptide; p-tau181p = tau phosphorylated at the threonine 181 position; LR = logistic regression; ROC = receiver operating characteristic; AUC = area under the curve.
LR analyses were performed using the variables sex, years of education, age at the time of lumbar puncture, APOε4 allele expression (0, 1, or 2 APOε4 alleles), and each of the three biomarkers, with backward elimination and insertion into the model that had only Aβ1-42 and t-tau as variables to determine which variables contributed most to the discrimination between AD and NC. Aβ1-42, t-tau, and APOε4 allele number were significant contributors to the LR model, whereas p-tau181p and the other variables were not. The LR model for Aβ1-42 + t-tau + APOε4(1) + APOε4(2) (LRTAA) is: Pi = 1/1 + exp(−3.907 −0.0182*Tau + 0.0338*Aβ1-42 + {0 if no APOε4 allele is present; −0.671 if 1 APOε4 allele is present; −17.673 if 2 APOε4 alleles are present}). Using the LRTAA model as the independent variable and performing ROC analysis for the CSF biomarkers from the autopsy-confirmed AD cases in the cohort of ADNI-independent, age-matched AD and NC group, we found that the AUC, sensitivity, test accuracy, and negative predictive values improved modestly to 0.942, 98.2%, 89.9% and 97.2%, respectively (see Table 4). Plots of CSF tau versus CSF Aβ1-42 concentrations are summarized in Figures 2 and 3, respectively.
Because the APOε4 allele is the most robust genetic risk factor for sporadic AD, we performed comparisons of average values for each of the biomarkers and ratios thereof as summarized in Table 5 for the ADNI subjects who were carriers of zero, one, or two APOε4 alleles. Notably, as seen in Table 5, Aβ1-42 concentration is lowest in AD, MCI, and NC subjects with two alleles of APOε4, and concentrations increase as the number of alleles decreases. MCI subjects who had one or two APOε4 alleles had greater average t-tau and p-tau181p concentrations, as well as greater t-tau/Aβ1-42 and p-tau181p/Aβ1-42 ratio values than subjects lacking any APOε4 allele (APOε4−), although there was no difference between carriers of one versus two alleles. CSF t-tau concentrations in AD and NC subjects did not increase as a function of number of APOε4 alleles, and there was not a consistent dose–response effect for p-tau181p in either the AD or NC groups. Because there were only two of the elderly NC group who expressed two APOε4 alleles, it is not possible in this ADNI NC cohort to fully test for a relation between APOε4 allele number and CSF biomarker concentrations or ratios. Thus, because it is known that there is greater AD pathology in AD patients who are APOε4+ (reviewed in Roses and Saunders’s article18), one might expect that ADNI NC and MCI subjects who are APOε4+ would show more limited difference in their CSF t-tau and Aβ1-42 profile compared with the CSF profile of these AD biomarkers in their ADNI counterparts with early AD.
Table 5.
Mean Values for Biomarkers in Alzheimer’s Disease Neuroimaging Initiative Patients, Stratified by Number of APOEε4 Alleles
| Characteristics | Tau, Mean ± SD, (pg/ml) | Aβ1–42, Mean ± SD, (pg/ml) | p-tau181P, Mean ± SD, (pg/ml) | tau/Aβ1–42 Ratio, Mean ± SD | p-tau181P/Aβ1–42 Ratio, Mean ± SD |
|---|---|---|---|---|---|
| AD | |||||
| 0 ApoEε4 alleles (n = 31) | 124.9 ± 68.7 | 170.5 ± 52.3 | 41.5 ± 22.2 | 0.82 ± 0.50 | 0.28 ± 0.17 |
| 1 ApoEε4 allele (n = 46) | 116.7 ± 52.4 | 139.7 ± 26.0 | 38.5 ± 17.1 | 0.86 ± 0.39 | 0.29 ± 0.14 |
| 2 ApoEε4 alleles (n = 23) | 126.9 ± 52.8 | 114.7 ± 23.0 | 48.2 ± 21.5 | 1.16 ± 0.57 | 0.44 ± 0.24 |
| p: ApoEε4 = 0 vs ApoEε4 = 1 | 0.8233 | 0.001 | 0.7551 | 0.6616 | 0.7553 |
| p: ApoEε4 = 0 vs ApoEε4 = 2 | 0.733 | < 0.0001 | 0.1346 | 0.0433 | 0.008 |
| p: ApoEε4 = 1 vs ApoEε4 = 2 | 0.4007 | 0.0002 | 0.0397 | 0.0417 | 0.0016 |
| MCI | |||||
| 0 ApoEε4 alleles (n = 90) | 86.2 ± 47.2 | 186.8 ± 59.6 | 29.9 ± 16.4 | 0.55 ± 0.40 | 0.20 ± 0.15 |
| 1 ApoEε4 allele (n = 85) | 119.5 ± 71.8 | 149.7 ± 43.0 | 40.4 ± 19.0 | 0.92 ± 0.75 | 0.31 ± 0.19 |
| 2 ApoEε4 alleles (n = 21) | 110.6 ± 45.9 | 119.8 ± 23.5 | 40.2 ± 15.3 | 0.96 ± 0.49 | 0.35 ± 0.16 |
| p: ApoEε4 = 0 vs ApoEε4 = 1 | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 |
| p: ApoEε4 = 0 vs ApoEε4 = 2 | 0.0038 | < 0.0001 | 0.0042 | < 0.0001 | < 0.0001 |
| p: ApoEε4 = 1 vs ApoEε4 = 2 | 0.8494 | 0.0021 | 0.7938 | 0.2019 | 0.1677 |
| NC | |||||
| 0 ApoEε4 alleles (n = 87) | 66.3 ± 26 | 220.7 ± 47.9 | 22.6 ± 11.1 | 0.33 ± 0.19 | 0.11 ± 0.09 |
| 1 ApoEε4 allele (n = 25) | 81.2 ± 41.8 | 159.3 ± 49.6 | 33.4 ± 21.3 | 0.57 ± 0.38 | 0.25 ± 0.20 |
| 2 ApoEε4 alleles (n = 2) | 71.0 ± 2.8 | 126 ± 2.8 | 18.0 ± 4.2 | 0.56 ± 0.01 | 0.15 ± 0.04 |
| p: ApoEε4 = 0 vs ApoEε4 = 1 | 0.1394 | < 0.0001 | 0.016 | 0.0001 | < 0.0001 |
SD = standard deviation; Aβ1–42= amyloid-β 1 to 42 peptide; p-tau181p =tau phosphorylated at the threonine 181 position; AD = Alzheimer’s disease; Apo = apolipoprotein; MCI = mild cognitive impairment; NC = cognitively normal; CI = confidence interval.
As expected, there were ADNI MCI subjects who converted to a clinical diagnosis of probable AD during the first year of follow-up. As of August 15, 2008, there were a total of 37 MCI subjects who had provided CSF samples at baseline when they entered ADNI and who 12 months thereafter were documented to be converters to AD at the time of their year 1 visit (see CSF ADNI baseline biomarker data summarized in Table 2). The average biomarker concentrations and ratio values for these MCI to AD converters were different (p < 0.0001) from the corresponding results for the ADNI NC group, and as noted later, they had an AD-like CSF profile incidence comparable with that seen in the ADNI AD group (see Table 2 and Fig 1B). On the other hand, the three MCI subjects who back-converted to NC status showed an NC-like CSF tau and Aβ profile at baseline. The CSF t-tau values for these MCI subjects were 69, 73, and 83pg/ml, all less than the cutoff value of 93pg/ml; the values for Aβ1-42 were 253, 233, and 285pg/ml, all greater than the cutoff value of 192pg/ml; and the values for p-tau181p were 21, 25, and 20pg/ml, two less than the cutoff value of 23pg/ml and one slightly more than it. The change in clinical diagnosis for these three MCI individuals was based on an improvement on several cognitive measures including the ADAS-Cog, Mini-Mental State Examination, and memory measures. These subjects also improved on the Clinical Dementia Rating according to informants. It should be noted that results for all three of these subjects were mild at the time of their initial diagnosis and consequently were just on the border of normal and MCI. Because of the small numbers of subjects, it is important to be cautious about drawing any definitive conclusions from these subjects, and it will be important to confirm this finding with greater numbers of MCI subjects at later stages in the study. Finally, application of the cut points for the three best pathologically based parameters, Aβ1-42, t-tau/Aβ1-42, and the LRTAA model, for the presence of an AD-like CSF profile in the ADNI AD, MCI, and NC groups, as well as in the MCI subjects who converted to AD, showed the following incidence of an AD-like CSF profile: 91, 88, and 89%, respectively, for AD; 74, 69, and 70%, respectively, for MCI; 38, 34, and 31%, respectively, for NC; and 86.5, 89, and 86.5%, respectively, for MCI converters to AD.
Discussion
ADNI is a multisite, prospective clinical study funded by the National Institute on Aging, industry, and foundations (see Acknowledgements for details on sources for ADNI funding) with the following mission: (1) to develop standardized neuroimaging and biomarker methods for AD clinical trials; (2) to determine optimum methods for acquiring and processing brain images; (3) to validate AD neuroimaging and biomarker findings by correlating them with ADNI behavioral test data; and (4) to provide a database available to the public for all ADNI findings for further analysis.7,11 This is the first report on studies of baseline CSF samples from ADNI subjects, and we measured tau and Aβ1-42 values in the approximately 50% of ADNI subjects who consented to lumbar puncture, including representatives of the AD, MCI, and NC groups. Our objective in this study was to establish a CSF profile for these biomarkers that might serve as CSF signatures for the presence of AD pathology, and thus aid in the identification of patients among elderly individuals with late-life cognitive impairment. To do this, we measured Aβ1-42, t-tau, and p-tau181p in each of the 416 CSF ADNI baseline aliquots (102 = AD; 200 = MCI; 114 = NC) using the well-characterized and standardized multiplex xMAP Luminex platform with Innogenetics (INNO-BIA AlzBio3) immunoassay kit–based reagents.15,16 We also performed these CSF measurements using the same methods on CSF samples from an ADNI-independent set of 56 autopsy-confirmed cases with AD and 52 age-matched NC subjects for comparison with the ADNI data set and to inform our interpretations of these ADNI data. Hence, this also is the first study to compare CSF data from ADNI subjects with those from a comparable ADNI-independent cohort of autopsy-confirmed AD cases. This enabled us to define an AD CSF profile for tau and Aβ levels in the ADNI AD subjects and in the ADNI-independent autopsy-confirmed AD cases using ROC analyses and LR modeling (Fig 4). In brief, among the CSF biomarker studies here, CSF Aβ1-42 concentration was the most sensitive analyte for the detection of AD, thereby indicating that CSF Aβ1-42 is the most informative single AD biomarker both for the ADNI cohort and the ADNI-independent autopsy-confirmed cohort of AD cases. Specifically, for these CSF samples, we observed the following for CSF Aβ1-42: ROC AUC = 0.913; sensitivity for detection of AD = 96.4%; negative predictive value = 95.2%; specificity for discriminating AD from elderly NC = 76.9%; and positive predictive value = 81.8% with an overall test accuracy of 87%.
Fig 4.
(A) Receiver operating characteristic curve (ROC) curves for the non–Alzheimer’s Disease Neuroimaging Initiative (ADNI) autopsy-based Alzheimer’s disease (AD) cases versus non-ADNI cognitively normal (NC) subjects. The LRTAA model, amyloid-β 1 to 42 peptide (Aβ1-42), and tau/Aβ1-42 ratio are the independent variables whose ROC curves are shown. (B) ROC curves for ADNI probable AD versus NC subjects. CSF = cerebrospinal fluid.
Because these metrics are critical for the assessment of AD biomarkers,7 it is important to note that a sensitivity of 100% indicates that a diagnostic test identifies 100% of subjects with AD, whereas a test with 100% specificity distinguishes AD from non-AD subjects. Consensus reports recommend that informative biomarkers of AD should have a sensitivity and specificity of more than 85%.5,6 On the other hand, prior probability is the frequency of a disease in specific populations, and the positive predictive value of an AD biomarker is the percentage of people who are positive for the biomarker and who also are confirmed to have definite AD at autopsy. Clinically useful biomarker tests should have a positive predictive value of more than 80%.7 The negative predictive value of a test also is informative because this indicates the percentage of people with a negative test who, at autopsy, prove not to have the disease. Thus, a negative predictive value of 100% indicates that the test completely rules out the possibility that an individual has the disease pathology when the test is performed. Clearly, a reliable AD biomarker with a high negative predictive value would be extremely useful. Given the values of these metrics for CSF Aβ1-42 reported here, our study identifies CSF Aβ1-42 as the most informative AD biomarker of those we examined in the context of the ADNI study. It is important to emphasize here that the diagnostic test outcomes described are applicable to the ADNI study subjects but not necessarily to individuals in other settings. For example, the prevalence of AD would be lower and the presence of other neurodegenerative disorders higher in memory disorder clinics or other clinical settings in which a patient is evaluated for a memory complaint. The performance of these tests in such patients would require further independent studies to derive the diagnostic utility of these biomarker tests.
However, it is likely that a panel of biomarkers rather than a single analyte will have the most utility for the diagnosis of AD, predicting which NC individuals and which subjects with MCI will progress to AD, as well as for monitoring the response of patients to disease-modifying therapies. Further studies are needed to confirm the potential utilities of the biomarkers examined here, but several studies indicate that CSF tau and Aβ assays look increasingly promising for the early diagnosis of AD and recognizing those MCI subjects with the greatest likelihood to progress to AD.10,13,14,19,20 The presence of possible AD pathology in approximately 40% of the ADNI NC group is consistent with Li and colleagues’21 and Fagan and coauthors’22 findings that in the aging cognitively normal population there is a significant decrease in Aβ1-42 concentration and increased tau concentration in individuals older than 60 years, as compared with those younger than 60 years, and Gustafson and investigators’23 and Stomrud and researchers’24 reports that CSF Aβ1-42 concentration decreases are the most sensitive predictor of cognitive decline in elderly healthy subjects. Long-term follow-up of the ADNI cognitively normal individuals will be required to confirm that the CSF signature for AD accurately predicts AD pathology.
Indeed, our LRTAA model showed that the combination of Aβ1-42, t-tau, and the number of APOε4 alleles provided the best delineation of mild AD from MCI and cognitively normal subjects in ADNI. An AD-like pathological CSF profile for Aβ1-42 and t-tau, the t-tau/Aβ1-42 ratio, was detected in 33 of the 37 ADNI MCI subjects who converted to a diagnosis of probable AD 1 year after their baseline CSF collection, whereas the addition of APOε4 as a covariate in the LR model did not improve on the prediction of conversion from MCI to probable AD. Further work is needed to develop additional panels of biomarkers, as well as to identify more genetic risk factors that will help distinguish AD from other neurodegenerative diseases associated with cognitive impairments.25–28
Based on the data reported here from the first ADNI CSF biomarker study, we have confirmed and extended reports from other laboratories suggesting that CSF tau and Aβ are the most informative AD biomarkers,7–10,12–16,19,20 and that there is a dose–response relation between CSF biomarkers and the number of APOε4 alleles,29 but the significance of our findings goes beyond this because our data are based on the use of validated CSF methods to measure tau and Aβ1-42 using CSF samples collected over a period of a year from 56 different ADNI performance sites. Thus, the results of these studies offer the promise that the methods used here can be exported to many different clinical laboratory settings to enable wider access to these AD biomarker tests by clinicians and researchers.
Acknowledgments
We thank our ADNI colleagues for their contributions to the work summarized here. We thank Hugo Vanderstichele and Innogenetics NV Gent, Belguim for the generous donation of the INNO-BIA AlzBio 3 Research-use Immunoassay Kits used in this study. We also thank M. Figurski for help with the statistical analyses. We are grateful to Christopher M. Clark, A. Fagan, H. Arai, and H. Soares for providing aliquots of non-ADNI CSF samples to prepare the CSF quality-control pools used in the immunoassay system employed in this investigation. We thank D. Baldwin and the Molecular Diagnosis Genotyping Facility at the University of Pennsylvania Medical Center for provision of the ApoEε genotyping data.
ADNI is supported by (AG024904), from the NIH (National Institute on Aging; National Institute of Biomedical Imaging and Bioengineering), Foundation for the National Institutes of Health, Pfizer, Wyeth Research, Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Merck & Company, AstraZeneca AB, Novartis Pharmaceuticals Corporation, Alzheimer’s Association, Eisai Global Clinical Development, Elan Corporation plc, Forest Laboratories, and Institute for the Study of Aging, U.S. Food and Drug Administration. V.H.-Y.L. is supported by (AG10124) from the NIH (National Institute on Aging), Marian S. Ware Alzheimer Program, the John H. Ware 3rd Professorship for Alzheimer’s Disease Research, and JQT is supported by the William Maul Measy-Truman G. Schnabel Jr MD Professorship of Geriatric Medicine and Gerontology (JQT).
Appendix
Data used in preparing this article were produced by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Biomarker Core at the University of Pennsylvania or obtained from the ADNI database (www.loni.ucla.edu/ADNI). Many ADNI investigators contributed to the design and implementation of ADNI or provided data but did not participate in the analysis of the data presented here or in the writing of this report. ADNI investigators include (complete listing available at www.loni.ucla.edu\ADNI\Collaboration\ADNI_Manuscript_Citations.pdf).
Footnotes
Potential conflict of interest: Nothing to report.
References
- 1.Forman MS, Trojanowski JQ, Lee VM-Y. Neurodegenerative diseases: a decade of discoveries paves the way for therapeutic breakthroughs. Nat Med. 2004;10:1055–1063. doi: 10.1038/nm1113. [DOI] [PubMed] [Google Scholar]
- 2.Selkoe DJ. Cell biology of protein misfolding: the examples of Alzheimer’s and Parkinson’s diseases. Nat Cell Biol. 2004;6:1054–1061. doi: 10.1038/ncb1104-1054. [DOI] [PubMed] [Google Scholar]
- 3.Skovronsky DM, Lee VMY, Trojanowski JQ. Neurodegenerative diseases: new concepts of pathogenesis and their therapeutic implications. Annu Rev Pathol Mech Dis. 2006;1:151–170. doi: 10.1146/annurev.pathol.1.110304.100113. [DOI] [PubMed] [Google Scholar]
- 4.Forman MS, Farmer J, Johnson JK, et al. Ann Neurol. 2006;59:952–962. doi: 10.1002/ana.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Consensus report of the Working Group on: Biological Markers of Alzheimer’s Disease. The Ronald and Nancy Reagan Research Institute of the Alzheimer’s Association and the National Institute on Aging Working Group. Neurobiol Aging. 1998;19:109–116. [PubMed] [Google Scholar]
- 6.Frank RA, Galasko D, Hampel H, et al. Biological markers for therapeutic trials in Alzheimer’s disease—proceedings of the Biological Measures Working Group: NIA Initiative on Neuroimaging in Alzheimer’s Disease. Neurobiol Aging. 2003;24:521–536. doi: 10.1016/s0197-4580(03)00002-2. [DOI] [PubMed] [Google Scholar]
- 7.Shaw LM, Korecka M, Clark CM, et al. Biomarkers of neurodegeneration for diagnosis and monitoring therapeutics. Nat Rev Drug Dis. 2007;6:295–303. doi: 10.1038/nrd2176. [DOI] [PubMed] [Google Scholar]
- 8.Sunderland T, Linker G, Mirza N, et al. Decreased β-amyloid1–42 and increased Tau levels in cerebrospinal fluid of patients with Alzheimer disease. JAMA. 2003;289:2094–2103. doi: 10.1001/jama.289.16.2094. [DOI] [PubMed] [Google Scholar]
- 9.Blennow K, Hampel H. CSF markers for incipient Alzheimer’s disease. Lancet Neurology. 2003;2:605–613. doi: 10.1016/s1474-4422(03)00530-1. [DOI] [PubMed] [Google Scholar]
- 10.Hansson O, Zetterberg H, Buchhave P, et al. Association between CSF biomarkers and incipient Alzheimer’s disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol. 2006;5:228–234. doi: 10.1016/S1474-4422(06)70355-6. [DOI] [PubMed] [Google Scholar]
- 11.Mueller SG, Weiner MW, Thal LJ, et al. Ways toward an early diagnosis in Alzheimer’s disease: the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Alzheimers Dement. 2005;1:55–66. doi: 10.1016/j.jalz.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark CM, Xie S, Chittams J, et al. Cerebrospinal fluid tau and β-Amyloid: how well do these biomarkers reflect autopsy-confirmed dementia diagnoses. Arch Neurol. 2003;60:1696–1702. doi: 10.1001/archneur.60.12.1696. [DOI] [PubMed] [Google Scholar]
- 13.Clark CM, Davatzikos C, Borthakur A, et al. Biomarkers for early detection of Alzheimer pathology. NeuroSignals. 2008;16:11–18. doi: 10.1159/000109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark CM, Pratico D, Shaw L, et al. Biochemical biomarkers of late-life dementia. Alzheimers Dement. 2006;2:287–293. doi: 10.1016/j.jalz.2006.05.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olsson A, Vanderstichele H, Andreasen N, et al. Simultaneous measurement of β-amyloid(1-42), total tau and phosphorylated tau (thr181) in cerebrospinal fluid by the xMAP technology. Clin Chem. 2005;51:336–345. doi: 10.1373/clinchem.2004.039347. [DOI] [PubMed] [Google Scholar]
- 16.Vanderstichele H, De Meyer G, Engelborghs B, et al. Alzheimer’s disease biomarkers: from concept to clinical utility. In: Galimberti D, Scarpini E, editors. BioMarkers for early diagnosis of Alzheimer’s disease. Nova Science Publishers; Haupauge, NY: 2008. pp. 81–122. [Google Scholar]
- 17.Reijn TSM, Rikkert MO, van Geel WJA, et al. Diagnostic accuracy of ELISA and xMAP technology for analysis of amyloid β42 and tau proteins. Clin Chem. 2007;53:859–865. doi: 10.1373/clinchem.2006.081679. [DOI] [PubMed] [Google Scholar]
- 18.Roses AD, Saunders AM. ApoE, Alzheimer’s disease, and recovery from brain stress. Ann N Y Acad Sci. 1997;826:200–212. doi: 10.1111/j.1749-6632.1997.tb48471.x. [DOI] [PubMed] [Google Scholar]
- 19.de Leon MJ, De Santi S, Zinkowski R, et al. Longitudinal CSF and MRI biomarkers improve the diagnosis of mild cognitive impairment. Neurobiol Aging. 2006;27:394–401. doi: 10.1016/j.neurobiolaging.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Thal LJ, Kantarci K, Reiman EM, et al. The role of biomarkers in clinical trials for Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20:6–15. doi: 10.1097/01.wad.0000191420.61260.a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li G, Sokal I, Quinn JF, et al. CSF tau/Aβ42 ratio for increased risk of mild cognitive impairment: a followup study. Neurology. 2007;69:631–639. doi: 10.1212/01.wnl.0000267428.62582.aa. [DOI] [PubMed] [Google Scholar]
- 22.Fagan AM, Roe CM, Xiong C, et al. Cerebrospinal fluid tau/β-amyloid42 ratio as a prediction of cognitive decline in non-demented older adults. Arch Neurol. 2007;64:343–349. doi: 10.1001/archneur.64.3.noc60123. [DOI] [PubMed] [Google Scholar]
- 23.Gustafson DR, Skoog I, Rosengren L, et al. Cerebrospinal fluid β-amyloid1–42 concentration may predict cognitive decline in older women. J Neurol Neurosurg Psychiatry. 2007;78:461–464. doi: 10.1136/jnnp.2006.100529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stomrud E, Hansson O, Blennow K, et al. Cerebrospinal fluid biomarkers predict decline in subjective cognitive function over 3 years in healthy controls. Dement Geriatr Cogn Disor. 2007;24:118–124. doi: 10.1159/000105017. [DOI] [PubMed] [Google Scholar]
- 25.Bian H, Van Swieten JC, Leight S, et al. CSF biomarkers in frontotemporal lobar degeneration with known pathology. Neurology. 2008;70:1827–1835. doi: 10.1212/01.wnl.0000311445.21321.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grossman M, Farmer J, Leight S, et al. Cerebrospinal fluid profile in frontotemporal dementia and Alzheimer’s disease. Ann Neurol. 2005;57:721–729. doi: 10.1002/ana.20477. [DOI] [PubMed] [Google Scholar]
- 27.Kauwe JS, Cruchaga C, Mayo K, et al. Variation in MAPT is associated with cerebrospinal fluid tau levels in the presence of amyloid-beta deposition. Proc Natl Acad Sci U S A. 2008;105:8050–8054. doi: 10.1073/pnas.0801227105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang J, Sokal I, Peskind ER, et al. CSF multianalyte profile distinguishes Alzheimer and Parkinson diseases. Am J Clin Pathol. 2008;129:526–529. doi: 10.1309/W01Y0B808EMEH12L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galasko D, Chang L, Motter R, et al. High cerebrospinal fluid tau and low Aβ42 levels in the clinical diagnosis of Alzheimer disease in relation to apolipoprotein E genotype. Arch Neurol. 1998;55:937–945. doi: 10.1001/archneur.55.7.937. [DOI] [PubMed] [Google Scholar]