Abstract
Social cognition has been suggested to be an important mediating variable in the relationship between neurocognition and functional outcome. The present study tested this model in relation to work rehabilitation outcome and added self-reported social discomfort as a possible mediator. One hundred fifty-one participants with schizophrenia or schizoaffective disorder participated in a 26-week work therapy program. Neurocognition was constructed as a latent construct comprised of selected variables from our intake test battery representing executive functioning, verbal memory, attention and working memory, processing speed, and thought disorder. Social cognition at intake was the other latent construct comprised of variables representing affect recognition, theory of mind, self-reported egocentricity, and ratings of rapport. The 2 latent constructs received support from confirmatory factor analysis. Social discomfort on the job was based on their self-report on a weekly questionnaire. In addition, we constructed a composite rehabilitation outcome that was based on how many hours they worked, how well they worked, and how complex was the job that they were doing. Path analysis showed direct effects of neurocognition on rehabilitation outcome and indirect effects mediated by social cognition and social discomfort. This model proved to be a good fit to the data and far superior to another model where only social cognition was the mediating variable between neurocognition and rehabilitation outcome. Findings suggest that neurocognition affects social cognition and that poorer social cognition leads to social discomfort on the job, which in turn leads to poorer rehabilitation outcomes. Implications for rehabilitation interventions are discussed.
Keywords: neurocognition, social cognition and discomfort, schizophrenia, work rehabilitation, vocational rehabilitation
Introduction
In 1996, Michael Green's landmark article1 established the significant relationship between neurocognition and community functioning in schizophrenia. Evidence for this relationship has strengthened since then by examining specific domains of functioning, including social competence,2–4 and vocational functioning.5,6 The idea that social cognition can be posited as a construct related to but distinct from neurocognition is not new and can be dated back to studies in the 80s and 90s.7,8 The independent contribution of social cognitive processes to understanding function has received further evidence in more recent studies.9–12 A review in 2006 found support for distinct associations between social perception, emotion perception, and theory of mind (or attributional style) to various measures of social functioning and that these social cognitive abilities often mediated or made independent contributions from neurocognition in explaining variance in social functioning.2
Social cognition has been variously defined but is generally agreed to represent cognitive capacity for processing social information, such as affect recognition, theory of mind, and understanding the gist of social conversations, and social reasoning. There is to date no common agreement on the assessment of social cognition though all would agree that it is a multifaceted construct. Despite complexities in the measurement of social cognition, it has recently been shown that social cognition represents a separable cognitive domain in schizophrenia.13,14 Studies have shown that people with schizophrenia performed poorly on tests of social cognition compared with the normal population.15,16
Despite uncertainty about what constitutes social cognition, a commonly accepted definition is that social cognition is the mental operations underlying social interactions, which include processes involved in perceiving, interpreting, and generating responses to the intentions, dispositions, and behaviors of others.17 A few investigators have recently examined the role that social cognition might play in community functioning.17–19 Using structural equation modeling, recent studies have found support for the hypothesis that social cognition mediates the effects of neurocognition on function.2,20
A complex examination of the relationship between neurocognition, social cognition, and several functional domains was recently presented by Bowie and Harvey.21 Using path analysis, they showed that attention/working memory and processing speed predicted social competence. Their social competence measure was based on the UCSD Performance based Skills Assessment and the Social Skills Performance Assessment, which is not the same as social cognition but contains skills that require social cognition. They found in their path analysis that this social competency endogenous variable mediated the relationship between neurocognition and community activities and work skills. Their finding regarding work skills is of special interest to our research group because of our focus on vocational rehabilitation for people with severe mental illness. While the article of Bowie and Harvey21 used a person's capacity for work based on ratings of employable skills, level of supervision required to complete tasks, ability to stay on task, and punctuality, the authors make a special point that these ratings were not based upon behavior during employment and should be distinguished from actual work performance on the job.
Working involves many features that may be related to social cognition. Work performance inventories used in rehabilitation programs usually include social skills, cooperativeness, and personal presentation22,23 as essential elements. Moreover, sustaining employment involves continuously dealing with new demands in the work environment from changes in schedule to new personnel, and adapting to these changes often requires social understanding. Misattributions and misperceptions in regard to these changes can lead to abrupt job loss and briefer periods of employment. Finally, social cognition may affect an individual's likelihood of being given more complex assignments by the supervisor because complexity usually includes greater interpersonal demands such as helping a trainee, organizing other workers, or dealing with the public.
In the present study, we examine the relationship of neurocognitive and social cognitive functioning to actual work rehabilitation outcomes. The rehabilitation outcome variable that we have developed incorporates the 3 most critical features of work performance: how well they worked, how much they worked, and how complex was the job that they were doing (detailed in “Method” section). Participants were outpatients with schizophrenia or schizoaffective disorder engaged in a 6-month work therapy (WT) program that provided up to 20 hours per week of paid work activity. By observing them on the job every other week, we were able to see their work performance over time. Thus, we believe that the outcome variable in our model has verisimilitude and adds significance to the predictive value of our tested variables.
In addition to neurocognition and social cognition, we had observed clinically that social discomfort on the job appeared to influence outcomes, and we reasoned that such discomfort might be caused in part by difficulty in social information processing. Therefore, we asked participants each week to rate their level of social discomfort on the job on 3 questions using Likert scales: was being at your job stressful?, was talking to your coworkers difficult for you?, and was it difficult to understand your coworkers? Thus, a single individual could give as many as 26 ratings on each of these questions over the course of their 6-month WT program. By averaging their weekly scores on each question, adding them together, and generating a z distribution, we were able to derive a single variable to capture this potentially important feature of the person's work experience. The present study is the first to offer a measure of social discomfort on the job as a possible mediator of neurocognitive and social cognitive variable's effects on vocational performance.
The purpose of this report is to test the relationship between neurocognition, social cognition, and vocational performance and to determine whether social discomfort is an important mediating variable. We hypothesize that neurocognition will have direct effects upon vocational performance as has been demonstrated in previous studies and that it will have indirect effects on vocational performance that are mediated by social cognition. We further hypothesize that impairments in social cognition will be related to social discomfort on the job, which will mediate the effect of social cognition on vocational performance.
Method
Participants
One hundred fifty-one participants with schizophrenia (n = 105, 69.5%) or schizoaffective disorder (n = 46, 30.5%) as determined by PhD psychologists using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, procedures24 participated in intake procedures after being referred by their clinicians. All provided informed, written consent. Participants were in treatment at the VA Connecticut Healthcare System, West Haven, or at the Connecticut Mental Health Center. The study was approved by the local institutional review boards at both institutions. Data were collected from 1998 to 2003 as part of a study that randomized subjects into WT or WT plus neurocognitive enhancement therapy (NET + WT), an experimental program of cognitive remediation.25 Participants were not considered sufficiently stable to participate if there had been a change in psychiatric medications or housing in the last 30 days, if they had an episode of drug abuse within the past 30 days, or if they had a Global Assessment of Functioning score of 30 or below. Known neurological disease and developmental disability were also cause for exclusion. Participants were on average 42.8 (8.9) years of age, 58% male, 63.8% single and never married, and 61.2% Caucasian. Their average Wechsler Adult Intelligence Scale III (WAIS-III) full-scale IQ was 88.5 (13.1), and their education was 13.19 (2.0) years. Average age of first onset was 22.6 (7.4) years, and their average age of first hospitalization was 25.8 (7.3) years with an average total number of hospitalizations of 13.2 (2.0). Twenty-two percent were receiving a typical antipsychotic only, 68% an atypical antipsychotic only, 8% were receiving both, and 2% were taking other psychoactive medications but not antipsychotics. Average chlorpromazine equivalent dosage was 684.7 (493.5).
Measures
Neuropsychological Assessment.
Our own factor analyses26 and others27 have consistently found that neuropsychological test performance in schizophrenia typically yield the following factors: executive functioning, verbal memory, attention and working memory, processing speed, and thought disorder. To create a single exogenous variable to represent the latent construct of neurocognition, we selected variables from our neurocognitive test battery that represented each of these factors. We limited ourselves to one variable to represent each factor in order to keep the number of parameters within the acceptable range for a confirmatory factor analysis given our sample size. Executive function was represented by percent conceptual level on the Wisconsin Card Sorting Test (WCST),28,29 verbal memory by the Hopkins Verbal Learning Test Revised30 trial 1 total, attention and working memory by Digit Span scaled score from the WAIS-III,31 processing speed by Digit Symbol Substitution Test also from the WAIS-III, and thought disorder by Bizarreness score on the Gorham's Proverbs Test.32,33
Social Cognition.
Unlike neurocognition, there is little consensus about how social cognition should be measured in schizophrenia. Although there is conceptual coherence to the construct, it remains a matter of conjecture as to what constitutes social cognitive processes. Our view is that social cognition is comprised of both elemental and more complex reasoning processes. Affect recognition and theory of mind are 2 elemental social cognitive processes that have received scientific development in terms of measurement methodology and some evidence of relationship to social functioning. These 2 aspects of social cognition were represented in our model by the Bell Lysaker Emotion Recognition Test (BLERT)34 total score and by the Hinting Task35,36 total score. However, we also wanted to capture a broader understanding of social cognition that is reflected in the self-experience of relatedness and in the ability to establish rapport. To do so, we employed the Bell Object Relations Inventory (BORI)37 Egocentricity Scale. This self-report instrument has been used in a number of studies in schizophrenia (eg, Bell and Bruscato38, Bell et al39, and Bell and Zito40), and the Egocentricity Scale is associated with a more autistic understanding of others. The assessment of capacity for rapport came from the Rapport item on the Quality of Life Scale (QLS),41 which was rated by our trained interviewers and is defined as how well the participant was able to engage and sustain connection during the questioning. Thus, we constructed our latent construct of social cognition with the deliberate intent of gaining robustness from convergent methods of assessment: performance (BLERT and Hinting Task), self-report (BORI Egocentricity), and interview (QLS Rapport).
Social Discomfort on the Job.
Each participant attended a workers group once per week (described below). At the beginning of each group, they were asked to respond to the following questions regarding social discomfort by circling a number on a scale from 1 (not at all) to 7 (completely). Was it difficult to understand your coworkers this week? Was being at your job stressful this week? Was talking to your coworkers difficult for you this week? These questions were developed from our observations of common concerns expressed by previous participants that we thought had influenced their work functioning.
Rehabilitation Outcome: Work Performance, Complexity, and Total Hours Worked.
We wanted to create a composite score of overall rehabilitation outcome that would capture the most salient features of good workers: how well they worked, how much they worked, and how complex the job was. We used the total score from the Work Behavior Inventory (WBI) to measure work performance. It is an observational measure that we have found reliable42 and predictive of future work functioning.23 WBI evaluations are done on site and include observation of the worker and brief interviews with the supervisor. We used the last 3 WBIs (over a 6-week period) as a measure of the workers’ final work performance. We used 3 rather than the last one because we wanted to increase the stability of measurement. WBI total ratings had excellent reliability in this study (intraclass correlation [ICC] = .91).
Along with the WBI ratings, the complexity of the job was rated using a complexity scale from 1 to 5, with higher scores indicating that the job required multiple tasks, greater autonomy, and more interpersonal complexity. Changes in complexity score occurred when a worker was given new duties. For example, a worker in mail delivery would generally begin by going with someone else and helping on the route of deliveries (rated “1”). The worker would then progress to having his own route (rated “2”) and then might be asked to learn several routes and to do package deliveries and take phone calls in the mailroom (rated “3”). The worker might be entrusted with special handling deliveries (such as refrigerated specimens), taught to operate complicated machines that sorted and stamped mail, and asked to handle the reception desk for general inquiries (rated “4”). Finally, the worker might be expected to do all the above and also break in new workers and assign work to others (rated “5”). Changes in complexity ratings for an individual were relatively infrequent and were done by consensus of the research staff after a presentation of the circumstances. This is a similar procedure used by our university for determining when a staff member's duties have changed sufficiently to warrant a possible raise. A job audit is conducted, and a panel makes a determination comparing the new duties with established standards. Because consensus ratings were used, ICCs were not established for the complexity score.
To capture the consistency of working, we chose to use the total hours worked over the 6 months of the program rather than merely the final 6-week period of the WBI evaluations. We did so to increase the range and to fairly capture the difference between someone who worked well but quit after 13 weeks and someone who worked steadily the entire 26 weeks. To create a composite score, average WBI totals, average complexity score, and total hours were normalized by creating z distributions, and then the z values were averaged, creating a single score representative of overall rehabilitation outcome.
Procedure
Following informed consent, diagnostic and psychosocial data were collected and the intake neuropsychological testing was performed over 2 or 3 sessions. PhD or Master's-level psychologists trained specifically in study methods performed all procedures. For brevity and to preserve the focus of the current report on predictors of work performance, we minimize the presentation of procedures related to the randomized study and do not present results regarding condition assignments, which are available elsewhere.25,26,39,43 Following intake testing, participants were stratified based on degree of cognitive impairment and randomly assigned to 6 months of either NET + WT or WT only.
Work Therapy.
WT consisted of (1) payment for work activity at the rate of $3.40 per hour for up to 15 hours per week with increasing bonus pay ($3.90–$8.40) for 16–20 hours; (2) job placement at the medical center; (3) individual counseling when problems arose; (4) a group offering support, problem solving, goal setting, and detailed work performance feedback based on the WBI42; (5) a job coach for job-related difficulties and individual vocational counseling; (6) a certificate of participation in the program; and (7) referral to other vocational services upon completion of the 6-month active phase. The most common work sites were in dietetics, mailroom, grounds, maintenance, patient transport, and medical administration with duties similar to those of entry-level employees supervised by regular medical center personnel.
Neurocognitive Enhancement Therapy.
NET consisted of (1) feedback from the Vocational Cognitive Rating Sacle (VCRS),36 a rating of work-related cognition, in the support group; (2) cognitive exercises for up to 5 hours each week for 26 weeks; and (3) a weekly social information–processing group. In addition to the cognitive exercises, participants in the NET condition were also able to participate in up to 15 hours of WT (see above), for a maximum of 20 hours productive activity. Pay structure and maximum hours of productive activity were equivalent between the conditions.
VCRS feedback was given on a biweekly schedule (at the same time as the WBI feedback) and consisted of job ratings of attention, memory, and executive function. Patients were also encouraged to develop goals based on their WBI and VCRS feedback.
Cognitive exercises involved repeated practice on computer-based exercises for attention, memory, and executive function and a dichotic listening task. Participants attended up to five 1-hour sessions per week. Cognitive exercises utilized a modified form of Psychological Software Services CogReHab Software,44 a multimedia cognitive rehabilitation software designed for use with individuals with compromised brain function. Details of the tasks are described in Bell et al39 and Fiszdon et al.45
Data Analyses
The analyses were performed by SPSS version 14 and AMOS version 7.0 (SPSS, Inc., Chicago, IL). Descriptive statistics of all variables involved were first computed. A correlational matrix between the variables for neurocognition and social cognition was produced. We then performed a confirmatory factor analysis to assess if the variables we selected load well on the latent constructs “neurocognition” and “social cognition.” Factor loadings were used to specify the association between the indicator variable and the latent construct. By using principal axis factoring, factor analysis was used to generate factor scores for subsequent path analysis. Factors with eigenvalues over 1 were extracted along with varimax rotation.
With support from the confirmatory factor analysis, we created factor scores for neurocognition and social cognition that were summated z scores of the relevant component variables. In addition, we compiled a composite rehabilitation outcome score based on the number of hours worked, WBI scores, and the complexity score. Again, it was a factor score by summation of the converted z scores of the 3 parameters. All the above factor scores were used for the subsequent analyses.
A correlational matrix showing the relationship between variables of neurocognition and social cognition and variables of perceived social discomfort and rehabilitation outcome was computed. Path analysis was then used to test the relationship between neurocognition, social cognition, and perceived social discomfort at work in relation to the rehabilitation outcome. In the analysis, neurocognition was treated as the exogenous variable while social cognition and perceived social discomfort in the workplace were treated as the mediating variables. We hypothesized that neurocognitive function has both direct and indirect effects on rehabilitation outcomes. We tested 2 models based on the literature and our hypothesis. In model 1, only social cognition was treated as the mediating variable between neurocognition and rehabilitation outcome based on available literature.2,20 In model 2, we test our own model that perceived social discomfort was treated as an additional mediating variable between social cognition and rehabilitation outcome. Three different goodness-of-fit statistics were used which included the model relative chi square (χ2/df),46 the comparative fit index (CFI),47 and the root mean square error of approximation (RMSEA).48 The relative chi square has the advantage of being less dependent on sample size.46 The CFI compares the final model with an “independence” model, which is a null model that assumes all variables are uncorrelated with dependent variable. It provides good model fit even with a small sample size.49 RMSEA is also a commonly used fit statistic because it does not require a null model.46 A model that fits well with the data has a χ2/df ratio less than 3,50 a CFI of greater than 0.90, and an RMSEA less than 0.08.51–53 To compare the 2 models to be developed by our analysis, we used the following formula to compute the P value for comparison of model fit.54
Results
The means and SDs of the variables pertaining to neurocognition, social cognition, and perceived social discomfort are presented in table 1. The correlational matrices of the variables are shown in table 2.
Table 1.
Descriptive Statistics
| Variables | N | Mean | SD |
| Neurocognition | |||
| Proverbs total | 149 | 3.23 | 4.02 |
| HVLT 1 | 151 | 4.62 | 1.64 |
| WCST conceptual level | 151 | 81.21 | 19.43 |
| Digit Span | 151 | 9.32 | 2.47 |
| Digit Symbol | 151 | 6.32 | 2.07 |
| Social Cognition | |||
| Hinting Task total | 150 | 16.02 | 3.68 |
| BLERT total | 151 | 15.90 | 4.60 |
| Egocentricity | 150 | 0.40 | 0.86 |
| Rapport | 151 | 4.06 | 1.11 |
| Perceived Social Discomfort | |||
| Difficult understanding coworkers | 143 | 2.28 | 1.07 |
| Work stressful | 143 | 2.62 | 1.26 |
| Difficult talking to coworkers | 143 | 2.23 | 1.12 |
| Composite Rehabilitation Outcomes | |||
| Hours (total number) | 148 | 227.40 | 164.87 |
| Complexity (average last 3 weeks) | 145 | 2.74 | 0.69 |
| WBI (average last 3 weeks) | 145 | 117.41 | 24.52 |
Note: Proverbs total refers to Bizarreness score on the Gorham's Proverbs Test. HVLT 1 refers to trial 1 total of Hopkins Verbal Learning Test Revised. WCST conceptual level refers to percent conceptual level on the Wisconsin Card Sorting Test. Digit Span and Digit Symbol are scores from Wechsler Adult Intelligence Scale III. Egocentricity refers to the scale of the Bell Object Relations Inventory. Rapport is extracted from the item from Quality of Life Scale. WBI, Work Behavior Inventory; BLERT, Bell Lysaker Emotion Recognition Test.
Table 2.
Corelational Matrices of Study Variables
| Neurocognition |
Social Cognition |
||||||||
| Proverbs Total | HVLT 1 | WCST Conceptual Level | Digit Span | Digit Symbol | Hinting Task Total | BLERT Total | Egocentricity | Rapport | |
| Proverbs total | 1.00 | −0.137 | −0.275*** | −0.229*** | −0.092 | −0.455*** | −0.186* | 0.038 | −0.045 |
| HVLT 1 | 1.00 | 0.242*** | 0.198* | 0.272*** | 0.253*** | 0.141 | −0.319*** | 0.247*** | |
| WCST conceptual level | 1.00 | 0.208* | 0.253*** | 0.260*** | 0.184* | −0.169* | 0.115 | ||
| Digit Span | 1.00 | 0.231*** | 0.234*** | 0.045 | −0.273*** | −0.018 | |||
| Digit Symbol | 1.00 | 0.100 | 0.170* | −0.282*** | 0.002 | ||||
| Hinting Task total | 1.00 | 0.169* | −0.202* | 0.196* | |||||
| BLERT total | 1.00 | −0.270*** | 0.167* | ||||||
| Egocentricity | 1.00 | −0.080 | |||||||
| Rapport | 1.00 | ||||||||
| Perceived Social Discomfort |
Composite Rehabilitation Outcomes |
|||||
| Understanding Coworkers | Stressful at Work | Talking to Coworkers | Hours | Complexity | WBI | |
| Proverbs total | −0.014 | −0.073 | −0.127 | −0.123 | −0.220*** | −0.199* |
| HVLT 1 | −0.247*** | −0.218*** | −0.262*** | 0.106 | 0.296*** | 0.243*** |
| WCST conceptual level | −0.086 | −0.028 | 0.037 | 0.077 | 0.058 | 0.120 |
| Digit Span | −0.101 | −0.091 | −0.051 | 0.207* | 0.178* | 0.169* |
| Digit Symbol | −0.099 | −0.074 | −0.081 | 0.109 | 0.108 | 173* |
| Hinting Task total | −0.190* | −0.138 | −0.181* | 0.154 | 0.349*** | 0.355*** |
| BLERT total | −0.153 | −0.076 | −0.133 | 0.024 | 0.123 | 0.096 |
| Egocentricity | 0.115 | 0.062 | 0.086 | −0.013 | −0.145 | −0.149 |
| Rapport | 0.076 | 0.092 | 0.036 | −0.037 | 0.056 | 0.101 |
| Understanding_1ST | 1.00 | 0.637*** | 0.796*** | −0.037 | −0.187* | −0.150 |
| Stressful_1ST | 1.00 | 0.728*** | −0.180* | −0.201* | −0.175* | |
| Talking_1ST | 1.00 | −0.047 | −0.191* | −0.144 | ||
| Hours | 1.00 | 0.488 | 0.637*** | |||
| Complexity | 1.00 | 0.707*** | ||||
| WBI | 1.00 | |||||
Note: HVLT, Hopkins Verbal Learning Test trial 1; WCST, Wisconsin Card Sorting Test; BLERT, Bell Lysaker Emotion Recognition Test; WBI, Work Behavior Inventory.
* P<.05; ***P < .001.
Confirmatory Factor Analysis
Table 3 summarizes the hypothesized model that neurocognition was a 5-factor latent construct that consisted of thought disorder, verbal memory, attention and working memory, executive function, and processing speed. The model shows that the 5-factor structure fit well with the observed data that was confirmed by the goodness-of-fit statistics (χ2 = 5.353, df = 5, P value = .374; CFI = 1.00 (saturated model), 0.992 (default Model); and RMSEA = 0.022.
Table 3.
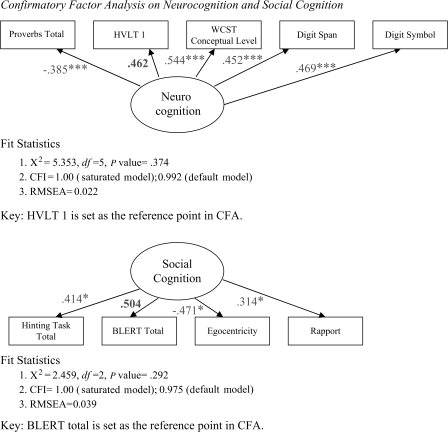 |
Similarly, confirmatory factor analysis shows that the 4-factor solution of social cognition variables—affect recognition, theory of mind, egocentricity, and rapport—fitted well with the observed data. This was confirmed by the goodness-of-fit statistics (χ2 = 2.459, df = 2, P value = .292; CFI = 1.00 (saturated model), 0.975 (default model); and RMSEA = 0.039).
Path Analysis
In our path analysis, we treated neurocognition as the exogenous variable and social cognition as the endogenous variable for our 2 models.
In model 1, we tested the model suggested by available literature that neurocognition had a direct effect on rehabilitation outcome and that it was also mediated by social cognition exerting its indirect effect on rehabilitation outcome. Table 4 shows the result of path analysis for this model.
Table 4.
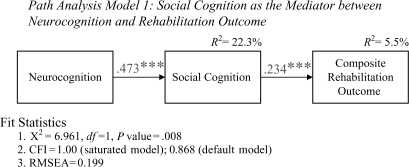 |
The model shows that social cognition was the mediator between neurocognition and rehabilitation outcome. Neurocognition explained 22.3% of variance of social cognition, which in turned explained 5.5% of variance of the rehabilitation outcome. However, the model on the whole did not fit well with the observed data. Statistics (χ2 = 6.961, df = 1, P value = .008; CFI = 1.00 (saturated model), 0.868 (default model); and RMSEA = 0.199) show that it is not a well-fitted model according to our criteria.
Table 5 shows the second model that was conceptualized as the multiple mediator model. First, social cognition was the mediator between neurocognition and rehabilitation outcome similar to model 1. Second, perceived social discomfort was conceptualized as another mediator between social cognition and rehabilitation outcome. This model shows that neurocognition had a significant direct effect on rehabilitation outcome. In addition, it exerted a significant indirect effect mediated by social cognition and perceived social discomfort. Neurocognition had a significant positive effect on social cognition explaining 22.5% of its variance. On the other hand, social cognition had a significant negative relationship with perceived social discomfort in the workplace with 6.7% of its variance explained. Perceived social discomfort similarly had a significant negative impact on rehabilitation outcome. The model explained altogether 18.4% of the total variance of the rehabilitation outcome. Goodness-of-fit statistics (χ2 = 2.128, df = 2, P value = .345; CFI = 1.00 (saturated model), 0.998 (default model); and RMSEA = 0.021) shows that the model is well fitted to the observed data.
Table 5.
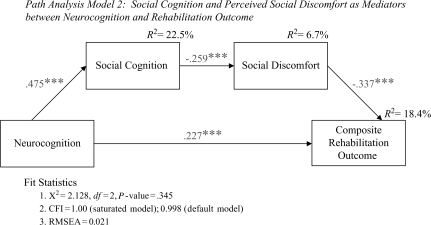 |
To compare the 2 models, we computed the P value based on the formula presented above. Table 6 shows that model 2 is better than model 1 in terms of their goodness of fit.
Table 6.
Comparison of Model 1 and Model 2
| CFI | RMSEA | χ2 | df | P | |
| Model 1: social cognition as mediator | 0.868 | 0.199 | 6.961 | 1 | .008 |
| Model 2: multiple mediating models | 0.988 | 0.021 | 2.128 | 2 | .345 |
| Comparisons of model fit | |||||
| Model 1 vs model 2 | .003 |
Note: Conclusion—Model 2 has a better fit than Model 1. RMSEA, root mean square error of approximation.
Discussion
Results of the current study reveal the contribution that social cognition and social discomfort make to vocational rehabilitation outcomes. The model that we tested was based on previous work showing that social cognition (measured in ways somewhat different than in this study) mediated the effects of neurocognition on community function.17–19 Our first model, which did not include social discomfort and did not have a direct path for neurocognition, proved to be a poor fit to the data. Our second model, which included the direct effects of neurocognition on rehabilitation outcome and the mediating role of both social cognition and social discomfort, proved to be a good fit to the data and far superior to the first model. These results may be interpreted to indicate that social cognition is dependent upon neurocognitive processes and that its functional impact may occur indirectly through its effects on social discomfort. People with poorer neurocognition are likely to have more problems with social cognition. Impaired social cognition makes it more difficult for people to be comfortable in the workplace, to understand their coworkers, and to communicate with them. These difficulties have direct effects upon how well they do their job, how much responsibility they are given, and how many hours of work they perform.
In order to test our model, we needed to make many choices in data reduction and in our selection of variables. In particular, our choice of variables to represent the latent construct of social cognition is somewhat original. We wanted to avoid shared method variance and enhance the robustness of the construct by selecting variables that came from performance testing (BLERT and Hinting Task), self-report (Egocentricity), and observation (Rapport). These variables had relatively low bivariate correlations with each other, but the confirmatory factor analysis showed that they all contributed significantly to the latent variable that we labeled social cognition. The resulting construct is contributed to by elemental features of social cognition such as theory of mind and affect recognition and more holistic aspects such as perceived relatedness and observed ability to establish rapport. As a latent construct, it proved to have an important role in explaining rehabilitation outcomes.
The final model suggests that social cognition and social discomfort on the job may both be relevant targets for intervention. There are a few interventions that have appeared recently in the literature including Social Cognition and Interaction Training,55 cognitive enhancement therapy,56 and social cognitive enhancement training57 that may be helpful in addressing both elemental functions such as affect recognition and more holistic functions such as “gistful learning.”11 Other interventions that directly concern social functioning in the workplace may be useful in addressing social discomfort. These include “Work Place Fundamentals,” a social skills training module58 and a work feedback and goal setting group described in Bell et al59 that includes issues of social skills and cooperativeness on the job. In addition, cognitive and behavioral techniques to help clients cope with stress60 and psychoeducation used to help people to handle work-related stress61 are promising approaches.
There are a number of limitations that come from the post hoc nature of this analysis and the choices that were necessary in selecting variables and building models. For example, tests selected for the social cognition construct did not include a specific assessment of attributional style, which may have been an important feature to capture. The data came from a randomized study of cognitive remediation, and the conditions of that trial are not included in the model because of limitations in power that constricted the number of parameters that could be included. However, the effects of condition should not have been relevant to neurcognition or social cognition that were evaluated before entry into condition. Furthermore, although cognitive training proved to have a favorable effect on vocational outcomes in the 6 months following the intervention,25 those effects were not found at the conclusion of the intervention, the time period when our rehabilitation outcome measure was recorded.
Results of this study may not be generalizable to other types of vocational rehabilitation such as supported employment or to a younger sample, such as those recovering from their first episode. However, results suggest the potential significance of social discomfort as a contributor to vocational outcomes, and future studies in supported employment or with first-episode patients may wish to consider examining its effects.
References
- 1.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 2.Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: A review. Schizophr Bull. 2006;32(suppl):S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mindt M, Moss M, Spaulding W. Cognitive measures: what can they tell us about social competence? Psychiatr Rehabil Skills. 1999;3:99–123. [Google Scholar]
- 4.Zanello A, Perrig L, Huguelet P. Cognitive functions related to interpersonal problem-solving skills in schizophrenic patients compared with healthy subjects. Psychiatry Res. 2006;142:67–78. doi: 10.1016/j.psychres.2003.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Abi-Saab D, Fiszdon J, Bryson G, Bell M. The implications of memory profiles in schizophrenia on vocational and neuropsychological functioning. Schizophr Res. 2006;75:73–182. doi: 10.1016/j.schres.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Evans JD, Bond GR, Meyer PS, et al. Cognitive and clinical predictors of success in vocational rehabilitation in schizophrenia. Schizophr Res. 2004;70:331–342. doi: 10.1016/j.schres.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Morrison RL, Bellack AS, Mueser KT. Deficits in facial-affect recognition and schizophrenia. Schizophr Bull. 1988;14:67–83. doi: 10.1093/schbul/14.1.67. [DOI] [PubMed] [Google Scholar]
- 8.Penn DL, Corrigan PW, Bentall RP, Racenstein JM, Newman L. Social cognition in schizophrenia. Psychol Bull. 1997;121:114–132. doi: 10.1037/0033-2909.121.1.114. [DOI] [PubMed] [Google Scholar]
- 9.Brekke JS, Hoe M, Long J, Green MF. How neurocognition and social cognition influence functional change during community-based psychosocial rehabilitation for individuals with schizophrenia. Schizophr Bull. 2007;33:1247–1256. doi: 10.1093/schbul/sbl072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickinson D, Bellack AS, Gold JM. Social/communication skills, cognition and vocational functioning in schizophrenia. Schizophr Bull. 2007;33:1213–1220. doi: 10.1093/schbul/sbl067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hogarty GE, Flesher S. Developmental theory for a cognitive enhancement therapy of schizophrenia. Schizophr Bull. 1999;25:677–692. doi: 10.1093/oxfordjournals.schbul.a033410. [DOI] [PubMed] [Google Scholar]
- 12.Silverstein SM. Information processing, social cognition, and psychiatric rehabilitation in schizophrenia. Psychiatry. 1997;60:327–340. doi: 10.1080/00332747.1997.11024810. [DOI] [PubMed] [Google Scholar]
- 13.Allen DN, Strauss GP, Donohue BC, van Kammen DP. Factor analytic support for social cognition as a separable cognitive domain in schizophrenia. Schizophr Res. 2007;93:325–333. doi: 10.1016/j.schres.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Sergi MJ, Rassovasky Y, Widmark C, et al. Social cognition in schizophrenia: relationships with neurocognition and negative symptoms. Schizophr Res. 2007;90:316–324. doi: 10.1016/j.schres.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 15.Bigelow NO, Paradiso S, Adolphs R, et al. Perception of socially relevant stimuli in schizophrenia. Schizophr Res. 2006;83:257–267. doi: 10.1016/j.schres.2005.12.856. [DOI] [PubMed] [Google Scholar]
- 16.Sergi MJ, Green MF. Social perception and early visual processing in schizophrenia. Schizophr Res. 2003;59:233–241. doi: 10.1016/s0920-9964(01)00405-4. [DOI] [PubMed] [Google Scholar]
- 17.Green MJ, Uhlhaas PJ, Coltheart M. Context processing and social cognition in schizophrenia. Curr Psychiatry Rev. 2005;1:11–22. [Google Scholar]
- 18.Toomey R, Wallace CJ, Corrigan PW, Schuldberg D, Green MF. Social processing correlates of nonverbal social perception in schizophrenia. Psychiatry. 1997;60:292–300. doi: 10.1080/00332747.1997.11024807. [DOI] [PubMed] [Google Scholar]
- 19.Wynn JK, Sergi MJ, Dawson ME, Schell AM, Green MF. Sensorimotor gating, orienting and social perception in schizophrenia. Schizophr Res. 2005;73:319–325. doi: 10.1016/j.schres.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Sergi MJ, Rasoovasky Y, Nuechterlein KH, Green MF. Social perception as a mediator of the influence of early visual processing on functional status in schizophrenia. Am J Psychiatry. 2006;163:448–454. doi: 10.1176/appi.ajp.163.3.448. [DOI] [PubMed] [Google Scholar]
- 21.Bowie CR, Harvey PD. Predicting real world outcomes from discrete functional and cognitive abilities. Schizophr Bull. 2007;33:554. [Google Scholar]
- 22.Bolton B, Roessler R. Manual for the Work Personality Profile. Fayetteville, Ark: Research and Training Center in Vocational Research; 1986. [Google Scholar]
- 23.Bryson G, Bell M, Kaplan E, Greig T. The Work Behavior Inventory: prediction of future work success of people with schizophrenia. Psychiatr Rehabil J. 1999;23:113–120. [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition (SCID-I/P, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 25.Bell MD, Bryson GJ, Greig TC, Fiszdon JM, Wexler BE. Neurocognitive enhancement therapy with work therapy: Productivity outcomes at 6-and 12-month follow-ups. J Rehabil Res Dev. 2005;42:829–838. doi: 10.1682/jrrd.2005.03.0061. [DOI] [PubMed] [Google Scholar]
- 26.Wexler BE, Bell MD. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr Bull. 2005;31:931–934. doi: 10.1093/schbul/sbi038. [DOI] [PubMed] [Google Scholar]
- 27.Harvey PD, Keefe RSE. Cognitive impairment in schizophrenia and implications of atypical neuroleptic treatment. CNS Spectr. 1997;2:1–11. [Google Scholar]
- 28.Heaton R. Wisconsin Card Sorting Test Manual. Odessa, Fla: Psychological Resources; 1981. [Google Scholar]
- 29.Bell MD, Greig TC, Kaplan E, Bryson G. Wisconsin Card Sorting Test dimensions in schizophrenia: Factorial, predictive, and divergent validity. J Clin Exp Neuropsychol. 1997;19:933–941. doi: 10.1080/01688639708403774. [DOI] [PubMed] [Google Scholar]
- 30.Brandt J, Benedict RHB. Professional manual. Lutz, Fla: Psychological Assessment Resources; 2001. Hopkins Verbal Learning Test-Revised. [Google Scholar]
- 31.Wechsler D. Wechsler Adult Intelligence Scale-3rd Edition (WAIS-3) New York, NY: Harcourt Assessment; 1997. [Google Scholar]
- 32.Gorham D. The use of the proverbs test for differentiating schizophrenia from normal. J Consult Psychol. 1950;20:435–440. doi: 10.1037/h0042949. [DOI] [PubMed] [Google Scholar]
- 33.Marengo J, Harrow M, Rogers C. A Manual for Scoring Abstract and Concrete Responses to Verbal Tests. New York, NY: Microfilm Publications; 1980. [Google Scholar]
- 34.Bell M, Bryson G, Lysaker P. Positive and negative affect recognition in schizophrenia: a comparison with substance abuse and normal control subjects. Psychiatr Res. 1997;73:73–82. doi: 10.1016/s0165-1781(97)00111-x. [DOI] [PubMed] [Google Scholar]
- 35.Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomatology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophr Res. 1995;17:5–13. doi: 10.1016/0920-9964(95)00024-g. [DOI] [PubMed] [Google Scholar]
- 36.Greig TC, Bryson GJ, Bell MD. Theory of Mind performance in schizophrenia: diagnosis, symptom and neuropsychological correlates. J Nerv Ment Dis. 2004;192:12–18. doi: 10.1097/01.nmd.0000105995.67947.fc. [DOI] [PubMed] [Google Scholar]
- 37.Bell MD. The Bell Object Relations Reality Testing Inventory (BORRTI) Los Angeles, Calif: Western Psychological Services; 1995. [Google Scholar]
- 38.Bell MD, Bruscato W. Object relations deficits in schizophrenia: a cross-cultural comparison between Brazil and USA. J Nerv Ment Dis. 2002;190:73–79. doi: 10.1097/00005053-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Bell M, Bryson G, Greig T, Corcoran C, Wexler BE. Neurocognitive enhancement therapy with work therapy: effects on neuropsychological test performance. Arch Gen Psychiatry. 2001;58:763–768. doi: 10.1001/archpsyc.58.8.763. [DOI] [PubMed] [Google Scholar]
- 40.Bell MD, Zito W. Integrated versus sealed-over recovery in schizophrenia: BORRTI and executive function. J Nerv Ment Dis. 2005;193:3–8. doi: 10.1097/01.nmd.0000149212.94261.1e. [DOI] [PubMed] [Google Scholar]
- 41.Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- 42.Bryson G, Bell M, Lysaker P. The Work Behavior Inventory: a scale for the assessment of work behavior for clients with severe mental illness. Psychiatr Rehabil J. 1997;20:47–55. [Google Scholar]
- 43.Bell MD, Fiszdon JM, Greig T, Wexler BW, Bryson G. Neurocognitive enhancement therapy with work therapy in schizophrenia: a six month follow-up of neuropsychological performance. J Rehabil Res Dev. 2007;44:761–770. doi: 10.1682/jrrd.2007.02.0032. [DOI] [PubMed] [Google Scholar]
- 44.Bracy O. CogReHab Software. Indianapolis, Ind: Psychological Software Services; 1995. [Google Scholar]
- 45.Fiszdon JM, Whelahan H, Bryson GJ, Wexler BE, Bell MD. Cognitive training of verbal memory using a dichotic listening paradigm: impact on symptoms and cognition. Acta Psychiatr Scand. 2005;112:187–93. doi: 10.1111/j.1600-0447.2005.00565.x. [DOI] [PubMed] [Google Scholar]
- 46.Ohaeri JU, Awadalla AW, El-Abas AHM, Jacob A. Confirmatory factor analytical study of the WHOQOL-Bref: experience with Sudanese general population and psychiatric samples. BMC Med Res Methodol. 2007;7:37. doi: 10.1186/1471-2288-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 48.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, Calif: Sage Publications; 1993. pp. 136–162. [Google Scholar]
- 49.Vauth R, Rusch N, Wirtz M, Corrigan PW. Does social cognition influence the relation between neurocognitive deficits and vocational functioning in schizophrenia? Psychiatr Res. 2004;128:155–165. doi: 10.1016/j.psychres.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 50.Carmines EG, McIver JP. Analysing Models With Unobserved Variables: Analysis of Covariance Structures. Beverly Hills, Calif: Sage; 1981. [Google Scholar]
- 51.Dunn G, Everitt B, Pickles A. Modeling Covariances and Latent Variables Using EQS. London, UK: Chapman & Hall; 1993. [Google Scholar]
- 52.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 53.Kelloway EK. Using Lisrel for Structural Equation Modeling: A researcher's Guide. Thousand Oaks, Calif: Sage; 1998. [Google Scholar]
- 54.Steiger JH, Shapiro A Browne MW. On the multivariate asymptotic distribution of sequential chi-square statistics. Psychometrika. 1985;50:253–264. [Google Scholar]
- 55.Combs DR, Adams SD, Penn DL, et al. Social cognition and interaction training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res. 2007;91:112–116. doi: 10.1016/j.schres.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 56.Eack SM, Hogarty GE, Greenwald DP, Hogarty SS, Keshavan MS. Cognitive enhancement therapy improves emotional intelligence in early course schizophrenia: preliminary effects. Schizophr Res. 2007;89:308–311. doi: 10.1016/j.schres.2006.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Choi KH, Kwon JH. Social cognitive enhancement training for schizophrenia: a preliminary randomized controlled trial. Community Ment Health J. 2006;42:177–187. doi: 10.1007/s10597-005-9023-6. [DOI] [PubMed] [Google Scholar]
- 58.Wallace CJ, Tauber R, Wilde J. Teaching fundamental workplace skills to persons with serious mental illness. Psychiatr Serv. 1999;50:1147–1153. doi: 10.1176/ps.50.9.1147. [DOI] [PubMed] [Google Scholar]
- 59.Bell MD, Lysaker P, Bryson G. A behavioral intervention to improve work performance in schizophrenia: Work Behavior Inventory Feedback. J Vocat Rehabil. 2003;18:43–50. [Google Scholar]
- 60.Norman RMG, Malla AK, McLean TS, et al. An evaluation of a stress management program for individuals with schizophrenia. Schizophr Res. 2002;58:293–303. doi: 10.1016/s0920-9964(01)00371-1. [DOI] [PubMed] [Google Scholar]
- 61.Lee H, Tan HK, Ma H, Tsai C, Liu Y. Effectiveness of a work-related stress management program in patients with chronic schizophrenia. Am J Occup Ther. 2006;60:435–441. doi: 10.5014/ajot.60.4.435. [DOI] [PubMed] [Google Scholar]


