Abstract
We present an overview of the literature on the patterns of mental health service use and the unmet need for care in individuals with schizophrenia with a focus on studies in the United States. We also present new data on the longitudinal course of treatments from a study of first-admission patients with schizophrenia. In epidemiological surveys, approximately 40% of the respondents with schizophrenia report that they have not received any mental health treatments in the preceding 6–12 months. Clinical epidemiological studies also find that many patients virtually drop out of treatment after their index contact with services and receive little mental health care in subsequent years. Clinical studies of patients in routine treatment settings indicate that the treatment patterns of these patients often fall short of the benchmarks set by evidence-based practice guidelines, while at least half of these patients continue to experience significant symptoms. The divergence from the guidelines is more pronounced with regard to psychosocial than medication treatments and in outpatient than in inpatient settings. The expansion of managed care has led to further reduction in the use of psychosocial treatments and, in some settings, continuity of care. In conclusion, we found a substantial level of unmet need for care among individuals with schizophrenia both at community level and in treatment settings. More than half of the individuals with this often chronic and disabling condition receive either no treatment or suboptimal treatment. Recovery in this patient population cannot be fully achieved without enhancing access to services and improving the quality of available services. The recent expansion of managed care has made this goal more difficult to achieve.
Keywords: unmet need for care, treatment patterns, mental health services
Introduction
This article presents an overview of the literature on patterns of mental health service use and, by extension, the unmet need for care in individuals with schizophrenia. In addition, new data on the longitudinal course of treatments in a first-admission sample of patients with schizophrenia are presented. Randomized clinical trials have repeatedly shown the efficacy of pharmacological and psychosocial interventions in the management of schizophrenia.1,2 Findings from these studies have been synthesized into practice guidelines with the aim of improving the treatment of schizophrenia across various settings.3–8 However, treatments offered in routine clinical practice often fall short of guideline recommendations, and many patients in the community receive no or little treatment.9–18 Thus, our knowledge of evidence-based treatment practices does not always translate into better care and outcomes for patients.
In comparison to hundreds of randomized clinical trials of various pharmacological and psychosocial treatments for schizophrenia, there are relatively few studies of the treatment patterns in routine care settings and the extent and the correlates of the unmet treatment needs in this patient population. Furthermore, much of the available data focus on patterns of pharmacotherapy, and less is known about the patterns of use of psychosocial treatments.
From a public health perspective, the issue of unmet need for care can be defined at different levels (eg, the community and the services) or from different perspectives (eg, the patients, their families, or their clinicians). Furthermore, there is currently a debate about the threshold at which care would be essential, and the lack of care would constitute an unmet need.19 For example, it is not clear whether treatment would be needed for the large number of people in community-based epidemiological studies who meet the full diagnostic criteria for a mood or anxiety disorder but who do not seek treatment.20–22 Some authors have argued that many of these individuals experience “appropriate homeostatic responses that are neither pathologic nor in need of treatment.”20(p114) These debates are likely less relevant to schizophrenia, in which the duration of illness, the severity of symptoms, and the social and occupational dysfunction that are the defining characteristics of the disorder23 justify treatment in almost all individuals with the diagnosis.
In both community and service settings, unmet needs are often evaluated by examining the patterns of service use and by comparing these patterns with the treatments recommended by evidence-based practice guidelines. An alternative approach would be to directly assess the perceptions of consumers, family members, or clinicians of the extent of met and unmet needs.
At the level of services, unmet needs commonly result from the discontinuities in treatment or provision of substandard treatments due to inadequate resources, prohibitive cost of treatments, inadequate health insurance, changes in insurance coverage, or the lack of satisfaction with the available treatments. These factors often coexist and may act synergistically in interfering with treatment.
In this article, we will present an overview of some of the studies that have evaluated the unmet need for treatment in schizophrenia. We will approach the question of unmet need for treatment according to 3 definitions as (a) the prevalence of cases of disorder that have not received any treatment in community settings or patients who have dropped out of treatment in representative clinical samples, (b) the prevalence of inadequate treatment or treatment of low quality in routine clinical settings, and (c) the prevalence of self-rated unmet need for treatment as perceived by the patients. For assessing the extent of unmet need for treatment based on the first 2 definitions, we will rely on studies of treatment patterns among individuals who meet the criteria for schizophrenia in general population epidemiological surveys or in clinical epidemiological studies that are based on representative clinical samples drawn from delimited geographical regions and clinical sample of patients drawn from routine treatment settings. We will also present data on the longitudinal course of mental health treatments in patients with schizophrenia from the Suffolk County Mental Health Project—a clinical epidemiological study of first-admission psychotic disorders in Long Island, New York. To assess the prevalence of unmet need for treatment as perceived by patients, we will briefly examine the growing literature on patient-perceived needs. Discussing these studies in concert highlights the various limitations and strengths of each approach as well as the complexities of assessing the unmet needs for care in schizophrenia. Our overview focuses on studies from the United States. However, where appropriate or in cases where there are few US studies, we will also discuss studies conducted in other countries.
Treatment Patterns
Treatment Patterns in Population Samples
Much of our current knowledge about treatment patterns in individuals with common mood and anxiety disorders comes from the epidemiological surveys of general populations.24,25 Fewer epidemiological studies of general populations have investigated the treatment patterns in representative samples of individuals with schizophrenia. In a 1980 review of the literature on the rates of mental health treatment in epidemiological studies, Link and Dohrenwend18 identified 7 studies from across the world conducted between 1938 and 1973 that specifically examined the lifetime treatment rates for schizophrenia. The median rate of lifetime treatment in these studies was 83.3% (range: 50%–100%) as compared with the general population studies of overall psychopathology (mostly mood, anxiety, and alcohol disorders) in which the median rate of treatment was only 26.7% (range: 7.8%–52.0%). Comparison across these studies, however, is hampered by the sociocultural variations in the samples, variations in case ascertainment methodology, and diagnostic criteria.
The introduction of explicit diagnostic criteria such as the Diagnostic and Statistical Manual of Mental Disorders (Third Edition) (DSM-III) and the incorporation of these diagnostic criteria into structured interview instruments paved the way for a second generation of epidemiological studies, which use standardized assessments and generally have large and representative population-based samples.26 In the United States, the Epidemiologic Catchment Area (ECA) study is the earliest and the best known of the second-generation studies that specifically focused on DSM-III disorders, including schizophrenia.27 The ECA was conducted in the early 1980s and sampled over 20 000 adults from 5 sampling sites across the United States. One advantage of the ECA over subsequent epidemiological studies was that in addition to the household samples, individuals in institutions were also sampled. The ECA found that about 1.3% of the population met lifetime DSM-III criteria for schizophrenia based on the lay-administered Diagnostic Interview Schedule.27 Another 0.2% met criteria for the schizophreniform disorder. The large majority of these cases were identified in the community as opposed to an institutional setting.27 The ECA found that among individuals with symptoms in the past 6 months (6-mo schizophrenia), only 57% had received some form of outpatient mental health care in this period: 40% from the specialty mental health sector (psychiatrists, psychologists, social worker, or other mental health professionals) and 17% from the general medical sector or the human services (such as the clergy or nonmental health social work).27 The ECA study did not report the lifetime history of treatment in this group of patients. However, the 57% rate of 6-month treatment seeking is much smaller than the 83% lifetime treatment from earlier epidemiological studies. It is not clear whether changes in the time and the diagnostic criteria or differences in the time frame (6 mo vs lifetime), in sociocultural characteristics of the samples, or in the ascertainment methods (structured interview vs clinician evaluation) accounted for this difference.
The second landmark US epidemiological survey, the National Comorbidity Survey (NCS), was conducted a decade later, between 1990 and 1992. The NCS included a nationally representative sample of individuals between the ages 15 and 54 years and administered the University of Michigan revised version of the Composite International Diagnostic Interview (CIDI). This study found a similar lifetime prevalence of the Diagnostic and Statistical Manual of Mental Disorders (Third Edition Revised) schizophrenia and schizophreniform disorder to that from the ECA (1.3%).28 However, the NCS also reported prevalence estimates based on the clinical reinterviews with the NCS respondents who had been assigned a diagnosis of schizophrenia or schizophreniform disorder by the lay-administered structured interview. The concordance between the structured interview and the interviews by the senior clinicians was quite low, with only 10% of the reinterviewed subjects being assigned a diagnosis of schizophrenia or schizophreniform disorder and 37% receiving a broader diagnosis of “nonaffective psychoses.” By the clinician diagnosis, the lifetime prevalence rates were 0.2% for schizophrenia or schizophreniform disorders and 0.3% for nonaffective psychoses—much lower than the estimates from the structured interviews. Among the clinician-identified cases of nonaffective psychoses symptomatic in the past 12 months, 57.9% had used some form of mental health services in that time frame: 47.5% had used specialty mental health services, 21.5% general medical services, 16.3% human services, and 22.0% self-help resources.29
A further wave of the NCS, the US National Comorbidity Survey-Replication (NCS-R), was conducted a decade later, between 2001 and 2003. The NCS-R sampled adults aged 18 years and older and administered a revised version of the CIDI. It also used a significantly modified ascertainment scheme to minimize false-positive responses30 as well as the statistical method of multiple imputation,31 commonly used to estimate missing data, to estimate the predicted prevalence of the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) clinician-diagnosed nonaffective psychoses based on the responses to the structured interviews. The lifetime prevalence of the probable nonaffective psychoses (including schizophrenia, schizophreniform disorder, as well as the other nonaffective psychoses) was 1.5% based on the structured interviews and 0.5% based on the predicted clinician diagnoses.30 We note that the 0.5% prevalence rate is consistent with the estimates from the other epidemiological studies.32
Among the NCS-R cases with a predicted clinician diagnosis of nonaffective psychosis who had active symptoms in the past 12 months, 57.8% reported mental health treatment contacts in the same 12-month period: 49.8% were treated in the mental health specialty sector, 5.0% in the general medical sector, 11.9% in the human services sector, and 13.4% in the complementary-alternative medicine sector.30
The differences in the sampling frame, the age ranges, the diagnostic criteria, the interview instruments, and the ascertainment methods make comparisons across these 3 US surveys very difficult.20 The difficulty is compounded by the inaccuracies inherent in estimating the prevalence of rare conditions in population samples33 that are likely responsible for the discrepancy in prevalence rates based on the lay-administered interviews and the clinician interviews.
The probability of correctly identifying cases of a disorder based on a screen-positive result (positive predictive validity) and of the cases free of the disorder based on a screen-negative result (negative predictive validity) is significantly affected by the true prevalence of the disorder, as well as by the sensitivity and specificity of the screening test. Eaton et al33 estimated that, eg, in a population survey of 1000 persons with a true prevalence of schizophrenia of 1%, a measure having 90% sensitivity and specificity (far higher than the sensitivity of currently available structured interview instruments) would identify 9 true cases and 99 false-positive cases, generating a prevalence estimate of more than 10% or 10 times higher than the true prevalence of the disorder.
Thus, the majority of the cases of schizophrenia identified using a lay-administered interview would be false-positive cases. Unless true cases of a disorder in a population can be identified with some accuracy, the patterns of treatment for that disorder cannot be accurately determined. Furthermore, the prevalence estimates of rare disorders are particularly sensitive to the selective nonresponse,25 and there is some evidence that individuals with schizophrenia in the community are less likely than other individuals to respond to surveys or appear in population-based samples if they are living in nursing homes and other quasi-institutional community settings.34
Despite these limitations, the similarity in treatment patterns of individuals with schizophrenia across the 3 population surveys is remarkable. About 57%–58% of individuals with active symptoms of schizophrenia in the 6–12 months prior to interview reported receiving some form of mental health treatment in that time frame. In the NCS and the NCS-R, between 47.5% and 49.8% received treatment in the specialty mental health sector. Thus, based on these data, at least 40% of individuals with actively symptomatic schizophrenia-spectrum disorders living in community settings in the United States have no consistent contact with needed services, and more than half have no contact with the specialty mental health treatment sector. These numbers reflect a large degree of potential unmet need for treatment among individuals with schizophrenia living in the various US communities.
Treatment Patterns in Clinical Epidemiological Samples
Whereas general population epidemiological surveys have typically been the gold standard for estimating the burden of the unmet need for treatment in the population,24 the limitations in ascertaining cases of rare disorders, noted earlier, constrain their usefulness for assessing the degree of unmet need for treatment in schizophrenia. Furthermore, many seriously ill individuals are likely underrepresented in these surveys because they live in the institutional settings or because they are homeless or incarcerated. Finally, epidemiological surveys generally collect limited information about the specific content and course of the treatments, such as history of recent hospitalizations and outpatient visits and the current use of medications. A thorough assessment of the psychiatric treatment history would require more detailed information on the content and course of treatments.
Epidemiological studies of clinical populations have an advantage over general population epidemiological surveys in that they typically collect more detailed information on the content and course of treatments in patients recruited from clinical settings in a well-defined geographical region.11,35–39 The ascertainment of cases in some of these studies is quite exhaustive, approximating that of general population surveys.36 When compared with clinical studies, epidemiological studies of clinical samples also provide a less biased picture of the use of clinical services and the extent of unmet need for care. This is especially true of the longitudinal studies involving first-contact or first-admission patients36,37 in which the frequent and infrequent users of services are equally likely to be included. In contrast, in studies of current patients in routine clinical settings, the probability of being sampled is proportional to the volume of service use, leading to what Cohen and Cohen labeled the “clinician's illusion.”40 Thus, longitudinal studies of first-contact or first-admission patients offer a more balanced view of the patterns of service use and the unmet needs for care than is possible when drawing from cross-sectional clinical samples.
For example, the report of Jablensky et al36 based on the follow-up data from the World Health Organization (WHO) 10-country study identified subgroups of patients with psychotic disorders who had considerable gaps in their care. Furthermore, the treatment patterns varied significantly across the settings. Only 15.9% of the patients in the developing countries (Colombia, India, and Nigeria) were on antipsychotic medications for more than 75% of the follow-up period, compared with 60.8% in the industrialized countries (Czech Republic, Denmark, Ireland, Japan, Russia, United Kingdom, and United States). Similarly, 55.5% of the patients in the developing countries were never hospitalized during the follow-up period compared with 8.1% in the industrialized countries.32 These numbers reflect considerable variation across the industrialized and the developing countries in the patterns of service use and the unmet need for care that would not be identified in studies involving clinical samples as the patients with less use of services in clinical samples would not be equally represented as the frequent users.
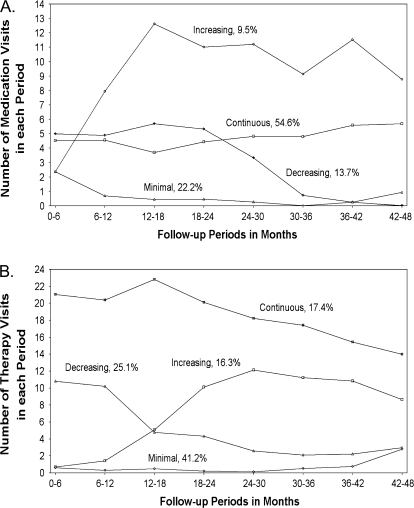
As another example, in a clinical epidemiological study of first-admission psychotic disorders from the private and public inpatient facilities in the Suffolk County, NY,14,37,41 we were able to use the latent growth class methodology42–44 to identify subgroups of schizophrenia patients according to their use of services in the 4-year period after their first admission.42,44 Groups were defined based on their longitudinal patterns (or trajectories) of medication and psychotherapy (individual, group, and family therapy combined) visits assessed at 6-month intervals (figure 1A and 1B).
Fig. 1.
Trajectories of Medication Visits (A) and Therapy Visits (B) in Patients With a Diagnosis of Schizophrenia in the Suffolk County Mental Health Project.
In this study, which took place in a semiurban area of Long Island, only 54.6% of the 172 first-admission patients with a consensus diagnosis of schizophrenia based on 2 years of observation had continuous medication visits in the 4 years following first admission (ie, 3–6 visits per 6 mo throughout the 4-y follow-up) and only 17.4% had continuous psychotherapy visits (ie, 12–24 visits per 6 mo). In contrast, 22.2% had minimal medication visits in the follow-up (ie, consistently less than 3 visits per 6 mo), and 41.2% had minimal therapy visits (ie, consistently less than 6 visits per 6 mo) (figure 1A and 1B). Overall, 12.8% of the sample fell in both the minimum medication and therapy visits and 16.3% in both the continuous medication and therapy visit classes.
Medication visits were strongly associated with being on psychiatric medications at each time point. For example, at the 6-month follow-up, 85.7% of the participants with continuous medication visits were taking any psychiatric medications compared with 44.4% of those with minimal medication visits (χdf = 12 = 21.94, P < .001). Similarly, 90.0% of those with continuous medication visits and 39.4% with minimal medication visits were taking any psychiatric medications at the 24-month follow-up (χdf = 12 = 34.32, P < .001).
The majority of the patients in the minimal medication visits and minimal psychotherapy visits remained in need of treatment through most of the first 4-year period after the index admission. Almost half of these patients were rated as continuously ill on the WHO Course of Illness Scale36 at the 4-year follow-up and as many were rated as having marked deterioration on the Schedule for Affective Disorders and Schizophrenia45 (tables 1 and 2). Furthermore, large percentages of patients in minimal medication or psychotherapy visit groups suffered from multiple episodes of illness with incomplete remission between episodes (45.7% in the minimal medications group and 50.0% in the minimal psychotherapy group). Very few of the patients with minimal contact with services remained in full remission after the first episode of illness (tables 1 and 2).
Table 1.
Outcomes at 4 and 10 y According to Medication Visit Trajectories in First-Admission Patients With a Research Diagnosis of Schizophrenia in the Suffolk County Mental Health Project
| Medication Visit Trajectories |
||||||||||
| Continuous (N = 94) |
Increasing (N = 16) |
Decreasing (N = 24) |
Minimal (N = 38) |
Comparisons, Testdf, P |
||||||
| Variable | N | % | N | % | N | % | N | % | All Groups | Continuous Vs Minimal |
| Outcomes, 4 y | ||||||||||
| SADS rating of functioning45,a | ||||||||||
| Return to highest premorbid level | 13 | 15.3 | 0 | 0.0 | 3 | 13.6 | 3 | 9.7 | χ62 = 9.01, .173 | χ22 = 0.81, .668 |
| Any residual impairment | 37 | 43.5 | 3 | 20.0 | 7 | 31.8 | 13 | 41.9 | ||
| Marked deterioration | 35 | 41.2 | 12 | 80.0 | 12 | 54.6 | 15 | 48.4 | ||
| WHO rating of course of illness36,b | ||||||||||
| Single psychotic episode + full remission | 1 | 1.1 | 0 | 0.0 | 0 | 0.0 | 1 | 2.9 | χ62 = 6.90, .330 | χ22 = 3.55, .169 |
| Multiple episodes or incomplete remission | 58 | 65.2 | 7 | 46.7 | 11 | 47.8 | 16 | 45.7 | ||
| Continuous illness | 30 | 33.7 | 8 | 53.3 | 12 | 52.2 | 17 | 48.6 | ||
| Number of rehospitalizationsc | ||||||||||
| 0 | 33 | 35.1 | 5 | 31.3 | 13 | 54.2 | 17 | 44.7 | χ62 = 11.7, .070 | χ22 = 6.18, .045* |
| 1 | 41 | 43.6 | 9 | 56.3 | 8 | 33.3 | 8 | 21.1 | ||
| 2+ | 20 | 21.3 | 2 | 12.5 | 3 | 12.5 | 13 | 34.2 | ||
| Outcomes, 10 y | ||||||||||
| SADS rating of functioning45,d | ||||||||||
| Return to highest premorbid level | 2 | 2.6 | 1 | 7.1 | 0 | 0.0 | 3 | 10.0 | χ62 = 6.00, .424 | χ22 = 3.15, .207 |
| Any residual impairment | 28 | 35.9 | 3 | 21.4 | 8 | 44.4 | 8 | 26.7 | ||
| Marked deterioration | 48 | 61.5 | 10 | 71.4 | 10 | 55.6 | 19 | 63.3 | ||
| WHO rating of course of illness36,e | ||||||||||
| Single psychotic episode + full remission | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | χ32 = 1.31, .726 | χ22 = 1.19, .275 |
| Multiple episodes or incomplete remission | 27 | 34.2 | 5 | 35.7 | 6 | 33.3 | 7 | 23.3 | ||
| Continuous illness | 52 | 65.8 | 9 | 64.3 | 12 | 66.7 | 23 | 76.7 | ||
| Number of rehospitalizationsf | ||||||||||
| 0 | 41 | 54.0 | 8 | 57.1 | 8 | 47.1 | 14 | 51.9 | χ62 = 1.70, .945 | χ22 = 0.36, .834 |
| 1 | 8 | 10.5 | 2 | 14.3 | 3 | 17.7 | 2 | 7.4 | ||
| 2+ | 27 | 35.5 | 4 | 28.6 | 6 | 35.3 | 11 | 40.7 | ||
| Percent of time in treatment between 4- and 10-y follow-upsg | ||||||||||
| 0 | 0 | 0.0 | 0 | 0.0 | 1 | 5.9 | 3 | 12.5 | χ92 = 15.87, .070 | χ32 = 11.71, .008** |
| 1 to <50 | 3 | 4.4 | 1 | 8.3 | 1 | 5.9 | 3 | 12.5 | ||
| 50 to <100 | 16 | 23.2 | 1 | 8.3 | 6 | 35.3 | 3 | 12.5 | ||
| 100 | 50 | 74.5 | 10 | 83.3 | 9 | 52.9 | 15 | 62.5 | ||
| Medication use at 10-y follow-uph | ||||||||||
| Any | 68 | 91.9 | 14 | 100 | 16 | 88.9 | 19 | 76.0 | χ32 = 6.84, .077 | χ12 = 4.43, .035* |
| None | 6 | 8.1 | 0 | 0.0 | 2 | 11.1 | 6 | 24.0 | ||
Note: SADS, Schedule for Affective Disorders and Schizophrenia; WHO, World Health Organization.
N = 153.
N = 162.
N = 172.
N = 140.
N = 141.
N = 134.
N = 122.
N = 131.
*P < .05, **P < .01.
Table 2.
Outcomes at 4 and 10 y According to Therapy Visit Trajectories in First-Admission Patients With a Research Diagnosis of Schizophrenia in the Suffolk County Mental Health Project
| Therapy Visit Trajectories |
||||||||||
| Continuous (N = 94) |
Increasing (N = 16) |
Decreasing (N = 24) |
Minimal (N = 38) |
Comparisons, Testdf, P |
||||||
| Variable | N | % | N | % | N | % | N | % | All Groups | Continuous Vs Minimal |
| Outcomes, 4 y | ||||||||||
| SADS rating of functioning45,a | ||||||||||
| Return to highest premorbid level | 5 | 18.5 | 3 | 12.0 | 4 | 10.3 | 7 | 11.3 | χ62 = 2.81, .832 | χ22 = 2.14, .342 |
| Any residual impairment | 12 | 44.4 | 9 | 36.0 | 17 | 43.6 | 22 | 35.5 | ||
| Marked deterioration | 10 | 37.0 | 13 | 52.0 | 18 | 46.2 | 33 | 53.2 | ||
| WHO rating of course of illness36,b | ||||||||||
| Single psychotic episode + full remission | 0 | 0.0 | 0 | 0.0 | 1 | 2.6 | 1 | 1.5 | χ62 = 6.65, .354 | χ22 = 5.36, .069 |
| Multiple episodes or incomplete remission | 22 | 75.9 | 16 | 57.1 | 21 | 53.9 | 33 | 50.0 | ||
| Continuous illness | 7 | 24.1 | 12 | 42.9 | 17 | 43.6 | 31 | 47.0 | ||
| Number of rehospitalizationsc | ||||||||||
| 0 | 14 | 46.7 | 9 | 32.1 | 19 | 44.2 | 26 | 36.6 | χ62 = 8.14, .228 | χ22 = 1.95, .377 |
| 1 | 11 | 36.7 | 16 | 57.1 | 15 | 34.9 | 24 | 33.8 | ||
| 2+ | 5 | 16.7 | 3 | 10.7 | 9 | 20.9 | 21 | 29.6 | ||
| Outcomes, 10 y | ||||||||||
| SADS rating of functioning45,d | ||||||||||
| Return to highest premorbid level | 3 | 10.7 | 0 | 0.0 | 1 | 2.9 | 2 | 3.5 | χ62 = 8.09, .232 | χ22 = 4.62, .099 |
| Any residual impairment | 13 | 46.4 | 5 | 25.0 | 11 | 32.4 | 18 | 31.0 | ||
| Marked deterioration | 12 | 42.9 | 15 | 75.0 | 22 | 64.7 | 38 | 65.5 | ||
| WHO rating of course of illness36,e | ||||||||||
| Single psychotic episode + full remission | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | χ32 = 4.61, .203 | χ22 = 3.66, .056 |
| Multiple episodes or incomplete remission | 14 | 48.3 | 5 | 25.0 | 10 | 29.4 | 16 | 27.6 | ||
| Continuous illness | 15 | 51.7 | 15 | 75.0 | 24 | 70.6 | 42 | 72.4 | ||
| Number of rehospitalizationsf | ||||||||||
| 0 | 17 | 58.6 | 12 | 60.0 | 17 | 53.1 | 25 | 47.2 | χ62 = 3.79, .705 | χ22 = 1.07, .587 |
| 1 | 4 | 13.8 | 1 | 5.0 | 2 | 6.3 | 8 | 15.1 | ||
| 2+ | 8 | 27.6 | 7 | 35.0 | 13 | 40.6 | 20 | 37.7 | ||
| Percent of time in treatment between 4- and 10-y follow-upsg | ||||||||||
| 0 | 0 | 0.0 | 0 | 0.0 | 1 | 3.3 | 3 | 6.3 | χ92 = 9.41, .400 | χ32 = 3.98, .264 |
| 1 to <50 | 0 | 0.0 | 1 | 5.6 | 4 | 13.3 | 3 | 6.3 | ||
| 50 to <100 | 6 | 23.1 | 5 | 27.8 | 8 | 26.7 | 7 | 14.6 | ||
| 100 | 20 | 76.9 | 12 | 66.7 | 17 | 56.7 | 35 | 72.9 | ||
| Psychotherapy visits in the last 6 mo of the 10-y follow-uph | ||||||||||
| Any visits | 22 | 75.9 | 12 | 63.2 | 18 | 56.3 | 25 | 47.2 | χ32 = 6.59, .086 | χ12 = 6.31, .012* |
| None | 7 | 24.1 | 7 | 36.8 | 14 | 43.8 | 28 | 52.8 | ||
Note: SADS, Schedule for Affective Disorders and Schizophrenia; WHO, World Health Organization.
N = 153.
N = 162.
N = 172.
N = 140.
N = 141.
N = 134.
N = 122.
N = 133.
*P < .05.
Patients with minimal medication visits were more likely than those with continuous medication visits to have multiple hospitalizations during the first 4 years (34.2% vs 21.3%, P = .045). However, they were less likely to remain consistently in treatment between the 4- and 10-year follow-ups or to be on any psychiatric medications at the 10-year follow-up (table 1).
Compared with patients with continuous psychotherapy visits in the first 4 years, those with minimal psychotherapy visits were more likely to be continuously ill during the first 4 years and between the 4- and 10-year follow-ups (47.0% vs 24.1% in the first 4 y and 72.4% vs 51.7% between the 4 and 10 y). However, these differences were only at a statistical trend level and did not reach a statistically significant level. Patients with continuous psychotherapy visits in the first 4 years were significantly more likely to be receiving any psychotherapy at the 10-year follow-up (table 2).
Another example that shows the utility of clinical epidemiological studies is the Australian Study of Low Prevalence Disorders.11 In that study, Jablensky et al used a 2-phase survey of all the individuals with psychotic disorders who made a contact with the public mental health services in 4 urban or predominantly urban areas in Australia in the late 1990s.11 In the second phase of the study, relatively detailed interviews were conducted with a stratified random sample of the individuals screened in the first phase of the survey. In addition, the authors surveyed individuals with psychotic disorders who received care from general medical professionals or psychiatrists in private practice; homeless individuals identified at night shelters, hostels, or other “safety net” services in the community; and individuals with a history of contact with services in the past 3 years but no current contact who were identified from the service registries.46 Among the patients thus identified, only 59.6% had used any outpatient services in the past 12 months and 43.6% had used inpatient services.47 A total of 21.9% reported that they had used no psychiatric services in this period.
The nonusers of services generally had lower levels of symptomatology and were twice as likely as the current users to have a course of illness characterized by a single episode of psychotic illness followed by recovery and 3 times less likely to have a course of illness characterized by severe deterioration.11 The nonusers were also less likely to have a comorbid substance use disorder and to have a history of self-harm behavior, arrests, and/or victimization.11 These variations echo earlier research in other settings48 indicating that in heterogeneous samples of patients with various psychotic disorders service use and the needs for care vary considerably among different subgroups of patients. However, these results are at variance with those from the homogeneous prospectively followed sample of patients with a diagnosis of schizophrenia from the Suffolk County Mental Health Project, discussed earlier, in which the course of illness in the minimal treatment group was characterized by continuous illness or significant residual symptoms.
In summary, clinical epidemiological studies address some of the deficiencies of the general population epidemiological surveys by using patient samples, thus reducing the false-positive rate, and by incorporating more detailed information on the nature and the volume of service use. Furthermore, studies of first-contact or first-admission patients, such as the Suffolk County Mental Health Project41 or the WHO 10-country study,36 and studies using patient registries to identify the previous users of services, such as in the Australian Study of Low Prevalence Disorders,11 can identify subgroups of patients who use fewer services or drop out of treatment—patients who are not well represented in cross-sectional clinical samples (see below).
Nevertheless, clinical epidemiological studies tend to be labor intensive and expensive. As a result, relatively few recent clinical epidemiological studies of psychotic disorders are available, and much of our knowledge about the patterns and the quality of treatments in schizophrenia patients comes from nonepidemiological, cross-sectional studies of chronically ill, clinical samples.
Treatment Patterns in Clinical Samples
Over the years, a number of studies have examined patterns of treatment in clinical samples of patients with schizophrenia.9,10,12,15–17,49–64 Differences in the time period, chronicity of the patient populations, treatment settings, and assessment methods make comparison across these studies difficult. Nevertheless, a common theme that emerges from many of these studies is the inadequate quality of treatments provided in routine treatment settings.
A number of studies have compared the treatment patterns in routine treatment settings against the evidence-based practice guideline benchmarks.9,12,17,49,53,55,64 However, again the diversity of practice guidelines and the differences in operationalization of the benchmarks limit comparison across these studies.58,65 Nevertheless, some of these studies used the Schizophrenia Patient Outcome Research Team (PORT) benchmarks.9,12,49,66 The results of 4 such studies are summarized in table 3. The PORT benchmarks set evidence-based quality indicators for pharmacological as well as psychosocial treatments of schizophrenia in inpatient and outpatient settings. The PORT guidelines were first published in 19988 and were subsequently revised in 2004.67 All studies in table 3 used the 1998 PORT guidelines.
Table 3.
Percent of Participants With Schizophrenia in Clinical Studies Who Are Receiving Treatments That Are Conformant With the PORT Treatment Recommendations
| Lehman et al12 |
West et al49 |
Dickey et al9 |
Busch et al66 |
||||
| PORT Recommendations | Inpatient (%) | Outpatient (%) | Mixed Inpatient and Outpatient (%) | Inpatient (%) | Outpatient (%) | Outpatient Managed Care (%) | Outpatient Fee for Servicea (%) |
| Inpatient antipsychotic treatment | 89.2 | —b | —c | 86.2–86.7 | —b | —b | —b |
| Appropriate dose of inpatient antipsychotics | 62.4 | —b | —c | 59.3–69.2 | —b | —b | —b |
| Maintenance antipsychotic treatment | —b | 92.3 | 99c | —b | 92.9–95.1 | 88.3 | 86.2–87.6 |
| Appropriate dose of maintenance antipsychotics | —b | 29.1 | 83c | —b | 34.1–45.0e | —d | —d |
| Anti-Parkinson treatment | 53.9 | 46.1 | 51 | —d | —d | 4.8 | 4.9–5.6 |
| Depot medication | 50.0 | 35.0 | 30 | —d | —d | —d | —d |
| Adjunctive depression medications | 32.2 | 45.7 | 38–100f | —d | —d | —d | —d |
| Adjunctive anxiety medications | 33.3 | 41.3 | 45 | —d | —d | —d | —d |
| Adjunctive psychosis medications | 22.9 | 14.4 | —d | —d | —d | —d | —d |
| Any psychotherapy | 96.5 | 45.0 | 69 | 90.0–98.9g | 79.2–81.2g | 20.3h | 36.9–71.6h |
| Family therapy | 31.6 | 9.6 | —d | 30.0–53.2i | —d | 0.05 | 0.2–0.6 |
| Vocational rehabilitation | 30.4 | 22.5 | 0 | —d | 20.4–23.2 | —d | —d |
| Case management | 8.6j | 10.1j | 38 | 31.9–38.3 | 43.4–64.0k | —d | —d |
Note: PORT, Patient Outcome Research Team.
Includes patients in carve-out region before transition to the carve-out plan and patients in comparison regions before and after transition.
Not relevant.
The study did not report separate values for inpatients and outpatients.
Not reported.
Mean standardized monthly dose within PORT-recommended range.
All the patients with a diagnosis of major depression received antidepressants, but only 38% of those with “moderate to severe” depressive symptoms did so.
Any psychosocial treatment.
Individual therapy and/or group therapy.
Any family contact.
Assertive community treatment and assertive case management were included.
Case management was reported only in high-risk patients (ie, patients with a history of hospitalization in the past 6 mo).
The PORT group's study is perhaps the best-known research assessing the conformance of the treatment patterns in routine care settings with the evidence-based recommendations.12 The study examined treatment patterns in a random sample of over 700 individuals with a clinical diagnosis of schizophrenia recruited from routine care settings in a southern and a midwestern state between 1994 and 1997. The patients were sampled from inpatient units and outpatient clinics in private and public institutions, including the Veteran's Administration facilities. The sampling sites included rural as well as urban sites.12 The data collected by surveying the patients and abstracting the inpatient and outpatient medical records showed a modest level of conformance with nearly all evidence-based recommendations, except for any prescription of antipsychotic medications, for which there was a high conformance (table 3). For most recommendations, fewer than half of the patients received guideline-conformant treatment. Furthermore, conformance was generally poorer for the outpatient treatments than for the inpatient treatments and for psychosocial treatments than for medications.12
Similar findings were reported in the 1999 American Psychiatric Association Practice Research Network (PRN) study, which used a nationally representative group of psychiatrists to obtain information about a sample of their patients and the treatments they received.49 Of the 151 patients with a clinical diagnosis of schizophrenia identified in this study, 99% received antipsychotic medications. However, 37% of these patients had difficulty adhering to medications, and 64% suffered from moderate to severe psychotic symptoms, likely partly due to poor adherence. Only 42% of the patients received any psychotherapy and 69% any form of psychosocial intervention, including case management.49 The rates of conformance with the practice guideline recommendations for the psychosocial treatments ranged from 0% to 43% and were especially lower among the patients with public insurance.
The variation across the studies in table 3 can be attributable to a number of factors including differences in the composition of samples, method of assessing conformance, and differences in the definitions used. For example, the study by Lehman et al12 examined conformance with PORT guidelines in patients in public mental health facilities in 2 states using chart reviews, whereas the study by West et al49 used a sample of patients from practices of psychiatrists who volunteered to participate in the American Psychiatric Association PRN study, and the data provided by these psychiatrists were not independently verified. As another example, Dickey et al9 categorized any family contact as family therapy, whereas in Busch et al66 study family therapy was more stringently defined based on coded claims data. These differences make direct comparison of estimates in table 3 difficult. Furthermore, the definitions of psychotherapy and vocational rehabilitation in these and other studies of quality of treatments in routine clinical settings are often very broad and overinclusive. Thus, these studies likely overestimate the rates of conformance with evidence-based guidelines with regard to these treatments. Nevertheless, it is noteworthy that even with the broad and overinclusive definitions the rates of conformance in these studies are consistently low (table 3).
A few studies have investigated the impact of contextual and service-level characteristics on treatment patterns.9,17,51 For example, Young et al17 examined the treatment patterns of 224 outpatients with schizophrenia recruited from 2 publicly funded clinics: an outpatient Veterans Administration (VA) clinic and a Community Mental Health Center (CMHC) clinic. The authors found significant differences in the treatment patterns between the 2 settings. More patients in the VA clinic compared with the CMHC clinic received poor quality medication management of their symptoms and side effects (44% vs 31%). Even after excluding patients who had characteristics that contributed to poor treatment quality (such as poor adherence or substance use disorders), the difference between the settings persisted. However, the schizophrenia patients with severe disability in the CMHC clinic were somewhat more likely to receive poor quality case management than those in the VA clinic.17
A reanalysis of the PORT study data by Rosenheck et al51 mainly confirmed the results of the Young et al17 study by finding greater conformance with the PORT guidelines in the non-VA settings compared with the VA settings of the PORT study. Patients in the non-VA outpatient settings were more likely than their VA counterparts to be taking at least one antipsychotic medication, to be on a depot medication if they had trouble with compliance, or to be receiving work therapy or job training and were less likely to be receiving a dose greater than 600 mg equivalent of chlorpromazine. Patients in the non-VA inpatient settings were also more likely to be offered individual or group therapy or assertive community treatment. However, these patients were more likely than their VA counterparts to be on a dose smaller than 300 mg chlorpromazine equivalent.51
In summary, studies comparing treatment patterns in routine treatment settings have mostly found that conformance is poorer for psychosocial treatments than for medications treatments, for outpatient settings than for inpatient settings, and in the VA than in the non-VA facilities. When contrasted with the relatively high-conformance rates with medication treatment benchmarks, the modest conformance rates for vocational rehabilitation and family therapy suggest that the main focus of treatments in many services is on management of symptoms rather than on rehabilitation and improvement of social and occupational functioning.
Correlates of Treatment Patterns
A large number of clinical studies have specifically examined the impact of clinical and sociodemographic characteristics on treatment patterns in general and on adherence with medication treatments in particular.68,69 Lack of insight, cognitive problems, comorbid substance use disorders, minority racial status, and younger age have all been associated with poorer adherence with treatment.16,68–71 Whereas the use of depot medications68 and various psychosocial interventions2,72 have been shown to improve adherence with medication treatments, the use of both remains limited (table 1). Lack of efficacy and bothersome side effects remain the major reasons for medication nonadherence in most cases.1
The Impact of Managed Care
The majority of studies reviewed above were based on data from the 1990s. However, since then, there have been significant changes in the structure and the content of services for patients with severe mental disorders in the United States, most importantly due to expansion of managed care plans. Findings with regard to patterns of treatment under managed care payment arrangements have been mixed.37,65,66,73,74 One study of 420 Medicaid beneficiaries in Massachusetts found no differences between patients enrolled in a capitated managed care plan and those in a fee-for-service program with regard to patterns of medication use or the use of psychosocial treatments.9
In another study of Medicaid enrollees, the introduction of a carve-out arrangement led to a reduction in the proportion of patients with schizophrenia who received any form of psychosocial treatment, including individual or group psychotherapy or psychosocial rehabilitation. No changes were observed in the area of medication management (eg, likelihood of receiving any antipsychotic medication, receiving second-generation antipsychotics, management of side effects). The authors attributed these changes in the receipt of psychosocial treatments to the fact that managed care carve outs were at financial risk for providing these treatments but not for providing medications.66
Similar findings were reported in other settings. For example, results from a Medicaid program in 2 counties in Florida between 1994 and 2000 revealed no meaningful changes in the percentage of patients with schizophrenia who had used antipsychotic medications: 86.2% in 1994–1995 vs 89.8% in 1999–2000.73 In contrast, in the same time span, the use of individual and/or group therapy decreased from 52.4% to 30.4%, and the rate of psychosocial rehabilitation decreased from 47.6% to 39.7. Less than 1% of the patients received family therapy across the years.73 A later study based on a sample of patients in the Florida Medicaid program found that the care of patients in a prepaid mental health program and a Health Maintenance Organization was much less likely to conform to the American Psychiatric Association's practice guidelines, mainly due to the low conformance with psychotherapy guidelines.75
Another study found a significant increase in the discontinuity of antipsychotic medications after transition to the mental health carve-out arrangement in the Tennessee Medicaid program.74 The study used administrative data on over 8000 patients in 2 cohorts enrolled in the Medicaid program, one cohort preceded the introduction of the carve-out plan and the other immediately followed it. Among patients for whom continuity of treatment was deemed “essential” based on their history, 29% in the posttransition cohort compared with 20% in the pretransition cohort experienced discontinuity of over 60 days in medication treatment.74 This study did not examine changes in the use of psychosocial treatments.
Finally, a study examining the prior authorization regulation for the use of atypical antipsychotic medications implemented in the Maine Medicaid program in 2003 also found increased psychiatric medication discontinuity and switching of medications.76 The Maine program was discontinued in 2004, but as the authors note, many other Medicaid managed care programs across the United States require preauthorization for the costlier antipsychotic medications.76
The introduction of the new Medicare Part D insurance may have created new complexities in the care of patients with schizophrenia as this insurance plan includes a cap on spending. There is some evidence that patients with severe mental disorders are at increased risk of discontinuities in medication treatment when faced with gaps in medication insurance coverage such as those imposed by spending caps.77 The effects of the Part D insurance in this patient population have yet to be fully appreciated.
In summary, managed care arrangements have had variable effects across different settings but are typically associated with reduced use of psychosocial treatments.71,73,75,78 Furthermore, in some, but not all settings, managed care arrangements appear to be associated with increased discontinuity in treatment.37,74,78,79
Unmet Need for Other Services
Patients with schizophrenia often face unmet needs for many other services beyond the traditional mental health services. There has been a renewed interest in the medical care of these patients, including receipt of the needed preventive and treatment services for chronic medical conditions and dental care.80,81 There is also a growing body of literature pointing to the lower quality of the medical services in patients with schizophrenia and other severe mental disorders,82–84 as well as a widening mortality gap between these patients and the general population.85
The widespread use of the atypical or second-generation antipsychotic medications has further contributed to the medical problems of patients with schizophrenia as some of these medications are associated with significant weight gain and an increased risk of hyperglycemia and hyperlipidemia.1 Nevertheless, the need for proper monitoring of these metabolic parameters and interventions to reduce the risk of future comorbidities often remains unmet. In one study of Medicaid patients who were started on an atypical antipsychotic medication, only 19% received baseline glucose testing and 6% received baseline lipid testing.86 The rates increased modestly between 1998 and 2003.86 In another study of patients in 3 VA clinics between 2002 and 2004, 46.2% had a weight problem.87 In almost none was the weight problem appropriately managed. As another example, a recent study of smokers with type 2 diabetes found that individuals with schizophrenia in this sample were significantly less likely than their counterparts without a serious mental illness to receive preventive treatments such as regular blood pressure examinations, lipid profiles, or treatment with angiotensin converting enzyme inhibitors or statins.88
The high prevalence of medical problems in patients with schizophrenia also calls for integration or better coordination of mental health and general medical services.89 However, coordination between various services for this patient group and other patients with severe mental disorders is often inadequate.90 For example, in a study of the Massachusetts Medicaid beneficiaries, contact between the mental health and the outpatient primary care providers was noted in only 43%–50% of the inpatients and 22.1%–24.2% of the outpatients with schizophrenia.9
Another mostly unmet service need in this patient population that also calls for integration of services or coordination across services is the need for substance abuse treatment.90 Drug and alcohol disorders are commonly comorbid with schizophrenia. For example, in the National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness, about 60% of schizophrenia patients were found to use substances and 37% met criteria for a current substance use disorder.91 Furthermore, these disorders have significant implications for the management and the social and clinical outcomes of schizophrenia.91–94 Nevertheless, in many of these patients, substance disorders go untreated. In one study, only about half of the schizophrenia patients with a need for substance abuse treatment received such care.9 The traditional separation between mental health and substance abuse services further contributes to the problem of unmet need for substance abuse treatment in this patient population. The recognition that substance comorbidity in this population is the norm rather than an exception and that addressing one problem without the other is inefficient has led to a number of recent attempts at implementation of integrated programs.95,96 Dual diagnosis programs are also now available in many substance disorder treatment facilities, although the range of services needed by dual diagnosis patients is not available in all these programs.97
Many schizophrenia patients smoke.98–100 A meta-analysis of over 40 studies from across the world found both a greater risk of current smoking (odds ratio [OR] = 5.3, 95% confidence interval [CI] = 4.9–5.7) and a lower likelihood of smoking cessation (OR = 0.46, 95% CI = 0.23–0.69) in patients with schizophrenia.98 The estimated prevalence of smoking in schizophrenia patients in this meta-analysis was 62%,98 attesting to the unmet need for management of smoking in this patient population.
Meeting the patients’ multiple needs for medical care and substance abuse treatment is especially difficult for practitioners working in solo practices or in small, single specialty group practices. For these practitioners, the solution to this problem calls for establishing more meaningful links and better coordination with other providers or agencies. The growing use of information technology can potentially facilitate such coordination.101,102 However, psychiatry has been slow in adopting information technology.103
Better integration of individuals with schizophrenia in the community would ultimately depend on their ability to attain meaningful social roles, including useful employment that can provide a sense of mastery and self-worth. Due to the disabling nature of the illness, many individuals with schizophrenia would need extra support and guidance beyond traditional vocational counseling to find and maintain useful employment. There is a growing body of literature indicating that supported employment produces better results than conventional vocational training or other interventions in this patient population.104–107 Dissemination of these practices in the VA system has produced modest but promising results.108–110
Finally, many patients with schizophrenia are at increased risk of homelessness and associated adverse social and health outcomes, such as victimization and sexually transmitted diseases.91,111–116 These patients often need the help of a case manager to negotiate the elaborate maze of social service organizations and to obtain housing and other needed social services.117 However, as data reviewed earlier suggest (table 3), only a minority of patients in need of case management receive such service.
Patients’ Perceived Unmet Need for Care
The studies reviewed above underscore the deficiencies in the treatment of schizophrenia by examining the patterns of service use in routine treatment settings and, in some cases, by comparing these patterns with the evidence-based practice guideline recommendations for the treatment of schizophrenia. Another perspective on the problem of unmet need for care in this patient population is the patients’ perceptions of the nature and extent of their met and unmet needs.118–124 This direct approach to assessing needs is in keeping with current trends toward shared decision making in the care of patients with severe mental disorders and reflects the diversity of the needs in this patient population.125–127
Over the years, a number of instruments have been developed to assess the patients’ perceptions of their needs.122–124 Perhaps, the most widely used of these measures is the Camberwell Assessment of Needs (CAN) instrument that asks questions regarding the perceived met and unmet needs of the patients in areas ranging from the management of psychotic symptoms to the need for food, child-care, and transportation. Studies comparing patient and staff reports of met and unmet needs in these areas have identified some consistencies.119,123 However, the studies have also identified differences between the patient and staff views, especially with regard to unmet needs. For example, in a Nordic study of schizophrenia patients, the most prevalent patient-identified unmet needs were in the domains of company, intimate relationships, and psychological distress; whereas, psychotic symptoms and daytime activities were among the top-rated areas of unmet need by the staff.119 Furthermore, the small number of patient-reported unmet needs in these studies is surprising given the wide gaps in the quality of treatment in routine treatment settings. For example, out of the 22 possible unmet needs on the CAN instrument, the patients and caregivers in the Nordic study identified on average about 2 unmet needs.119 The differences in the patient and staff views, as well as between the unmet needs identified in the epidemiological and the clinical studies on the one hand and the patients’ perceptions of unmet needs on the other hand, highlight the complexities inherent in defining needs and, by extension, in defining the unmet needs in this patient population.122
A number of factors likely contribute to the differences in results of need assessment using these different approaches and perspectives. Many patients with schizophrenia may not fully appreciate the extent of their mental health problems and their mental health-care needs.128,129 Furthermore, individuals vary in their needs and responses to treatments, whereas evidence-based standards provide universal benchmarks based on the needs and treatment responses of a typical patient. Finally, perceptions of need naturally differ between different stakeholders, and no one perspective can be said to be necessarily more accurate or true than another. Rather, these differences in the patient and provider perspectives may present opportunities to involve patients and families as well as other stakeholders in the treatment planning process.130,131
Conclusion
The preceding overview of the literature on patterns of treatment in schizophrenia and the extent of the unmet need for care reveals considerable gaps in our current knowledge. First, there is a paucity of reliable data from population-based epidemiological studies in the United States on which to base the population estimates of treatment and the potential unmet need for treatment. As noted earlier, difficulties inherent in the assessment of rare disorders severely limit our ability to accurately identify individuals with schizophrenia in ongoing epidemiological surveys of general populations using lay-administered interview instruments.33 Without accurate identification of the cases, establishing treatment patterns and the extent of the unmet need for care in these surveys is not feasible. Multistage survey methods132 or clinician-augmented surveys30 improve upon such classification, but they typically incur considerable additional costs and are not always implemented. Furthermore, these methods cannot resolve the problem of selective nonresponse and undersampling of individuals who are homeless, incarcerated, or living in quasi-institutional community settings.30
Nevertheless, the available data from the major US population surveys suggest that approximately 40% of individuals in the community with schizophrenia remain out of care either consistently or at least for long periods of time while experiencing significant symptoms. Clinical epidemiological studies address some of the limitations of general population surveys by reducing the false-positive rate and by using more detailed assessments.11,36,41 These studies also indicate that a significant percentage of patients remain consistently out of treatment after their initial contact with services. In the Suffolk County Mental Health Project, eg, 20% of patients with a diagnosis of schizophrenia remained consistently out of medication treatment and about 40% remained consistently out of therapy.
As the large majority of these individuals continue to experience significant symptoms and disability, making services available to them remains a priority. The stigma associated with mental illness and its treatment is a major barrier to treatment seeking among these individuals. Much attention has focused on reducing this stigma using media and educational campaigns. The World Psychiatric Association's program to fight stigma and discrimination against schizophrenia, implemented in over 20 countries, has been one of the most extensive of such efforts.133 With regard to more common disorders, such public campaigns have resulted in modest improvements in attitudes and treatment seeking.134,135 There is also evidence from Australia and Germany that public attitudes toward mental health treatment seeking for schizophrenia became more favorable between the early 1990s and the early 2000s.136,137 However, due to the relative rarity of schizophrenia, the impact of changes in public attitudes on treatment seeking for this disorder may be more difficult to assess than the impact on treatment seeking for the more common mood and anxiety disorders.
Another significant problem affecting the continuity of treatment of schizophrenia in routine care settings is the problem of nonadherence with treatments.14–16,72 Up to half of schizophrenia patients, experience extended gaps in their treatment in a 1-year period leading to increased hospitalizations and other adverse outcomes.14,138,139 There have been a number of focused attempts to reduce the frequency of these gaps and to improve the patients’ adherence using psychosocial interventions based on motivational interviewing methods, other cognitive-behavioral approaches, psychoeducation, medication self-management, and, more recently, environmental support.72,140,141 However, the evidence with regard to the efficacy of some of these interventions has been mixed.142–144 Furthermore, the mental health services have been slow in adopting these interventions.
The problem of unmet need for care in individuals who never initiate treatment or in patients who disengage from treatment is compounded by the unmet needs of a large proportion of patients who are in treatment but who continue to experience significant symptoms and disability. At least half of all patients with schizophrenia treated in routine care settings continue to have significant psychotic or other psychiatric symptoms that are potentially amenable to pharmacological treatments.49,87 Comparisons of the treatment patterns in routine treatment settings with evidence-based standards show that the overwhelming majority of individuals in treatment receive antipsychotic medications. Furthermore, at least in inpatient settings, the dose of prescribed antipsychotic medications is usually in the therapeutic range. However, there are gaps between current practices and evidence-based recommendations with regard to the appropriate pharmacological management of nonpsychotic symptoms and side effects, use of psychosocial treatments, and use of medical, dental, and substance disorder services and social services and with regard to coordination among the different services.
There is growing evidence that guideline-conformant treatments could potentially improve patient outcomes and reduce the avertable social and health burden of psychiatric illness75,145 at minimal additional costs.75,146 However, services have been slow in adopting care practices that are consistent with the evidence-based guidelines. The individual practice styles and institutional barriers such as lack of resources all likely contribute to the slow adoption of the guideline-consistent practices.147,148
Setting performance measures appears to be a straightforward approach to improving conformance with practice guidelines. In the VA health-care system, creating system-wide evidence-based performance measures has had some degree of success in improving conformance with the guidelines.149–151 For example, one performance measure requiring that all veterans have a primary care provider has led to significant improvement in medical care and receipt of preventive services in patients with severe mental disorders. However, changing clinician's practice styles is not easy.152 Although introducing incentives, eg, in the form of pay-for-performance arrangements, appears to be an attractive approach to changing clinician's behaviors, when applied in general medical settings, these initiatives have had mixed results, sometimes with unintended adverse consequences.153–157
The expansion of managed care in more recent years may have further widened the gap between usual practice and evidence-based standards, at least with regard to the use of psychosocial treatments66,73,75 and, perhaps, continuity of treatments.37,74 As Mechanic65 notes, the trend toward restricting the intensity of services under managed care plans may have led to more homogeneous service patterns and less variation among the different patient populations with different levels of need.
The consistent finding of a reduced use of psychosocial treatments under managed care is disconcerting as psychosocial treatments are often complementary to medications and can potentially address problem areas that are less responsive to medication treatments, such as poor social skills and negative symptoms.2,158,159 Furthermore, psychosocial treatments are likely more beneficial in the later stages of illness when the acute symptoms have subsided.2 The long-term impact of managed care on the clinical and social outcomes of the patients with schizophrenia remains to be fully appreciated.65,75
References
- 1.Lieberman JA. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia: efficacy, safety and cost outcomes of CATIE and other trials. J Clin Psychiatry. 2007;68:e04. doi: 10.4088/jcp.0207e04. [DOI] [PubMed] [Google Scholar]
- 2.Mojtabai R, Nicholson RA, Carpenter BN. Role of psychosocial treatments in management of schizophrenia: a meta-analytic review of controlled outcome studies. Schizophr Bull. 1998;24:569–587. doi: 10.1093/oxfordjournals.schbul.a033350. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Psychiatric Association. Clinical practice guidelines. Treatment of schizophrenia. Can J Psychiatry. 2005;50:7S–57S. [PubMed] [Google Scholar]
- 4.Royal Australian and New Zealand College of Psychiatrists Clinical Practice Guidelines Team for the Treatment of Schizophrenia and Related Disorders. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of schizophrenia and related disorders. Aust N Z J Psychiatry. 2005;39:1–30. doi: 10.1080/j.1440-1614.2005.01516.x. [DOI] [PubMed] [Google Scholar]
- 5.Miller AL, Crismon ML, Rush AJ, et al. The Texas Medication Algorithm Project: clinical results for schizophrenia. Schizophr Bull. 2004;30:627–647. doi: 10.1093/oxfordjournals.schbul.a007111. [DOI] [PubMed] [Google Scholar]
- 6.Moore TA, Buchanan RW, Buckley PF, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry. 2007;68:1751–1762. doi: 10.4088/jcp.v68n1115. [DOI] [PubMed] [Google Scholar]
- 7.Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161:1–56. [PubMed] [Google Scholar]
- 8.Lehman AF, Steinwachs DM. Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophr Bull. 1998;24:1–10. doi: 10.1093/oxfordjournals.schbul.a033302. [DOI] [PubMed] [Google Scholar]
- 9.Dickey B, Normand SL, Hermann RC, et al. Guideline recommendations for treatment of schizophrenia: the impact of managed care. Arch Gen Psychiatry. 2003;60:340–348. doi: 10.1001/archpsyc.60.4.340. [DOI] [PubMed] [Google Scholar]
- 10.Fischer EP, McCarthy JF, Ignacio RV, et al. Longitudinal patterns of health system retention among veterans with schizophrenia or bipolar disorder. Community Ment Health J. 2008;44:321–330. doi: 10.1007/s10597-008-9133-z. [DOI] [PubMed] [Google Scholar]
- 11.Jablensky A, McGrath J, Herrman H, et al. Psychotic disorders in urban areas: an overview of the Study on Low Prevalence Disorders. Aust N Z J Psychiatry. 2000;34:221–236. doi: 10.1080/j.1440-1614.2000.00728.x. [DOI] [PubMed] [Google Scholar]
- 12.Lehman AF, Steinwachs DM. Patterns of usual care for schizophrenia: initial results from the Schizophrenia Patient Outcomes Research Team (PORT) client survey. Schizophr Bull. 1998;24:11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy JF, Blow FC, Valenstein M, et al. Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: evaluating accessibility and availability barriers. Health Serv Res. 2007;42:1042–1060. doi: 10.1111/j.1475-6773.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mojtabai R, Lavelle J, Gibson PJ, et al. Gaps in use of antipsychotics after discharge by first-admission patients with schizophrenia, 1989 to 1996. Psychiatr Serv. 2002;53:337–339. doi: 10.1176/appi.ps.53.3.337. [DOI] [PubMed] [Google Scholar]
- 15.Valenstein M, Blow FC, Copeland LA, et al. Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophr Bull. 2004;30:255–264. doi: 10.1093/oxfordjournals.schbul.a007076. [DOI] [PubMed] [Google Scholar]
- 16.Valenstein M, Ganoczy D, McCarthy JF, Myra Kim H, Lee TA, Blow FC. Antipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective review. J Clin Psychiatry. 2006;67:1542–1550. doi: 10.4088/jcp.v67n1008. [DOI] [PubMed] [Google Scholar]
- 17.Young AS, Sullivan G, Burnam MA, Brook RH. Measuring the quality of outpatient treatment for schizophrenia. Arch Gen Psychiatry. 1998;55:611–617. doi: 10.1001/archpsyc.55.7.611. [DOI] [PubMed] [Google Scholar]
- 18.Link BG, Dohrenwend BP. Formulation of hypotheses about the ratio of untreated to treated cases in the true prevalence studies of functional psychiatric disorders in adults in the United States. In: Dohrenwend BP, editor. Mental Illness in the United States: Epidemiological Estimates. 1980: 133–149. [Google Scholar]
- 19.Andrews G, Henderson S. Unmet Need in Psychiatry: Problems, Resources, Responses. Cambridge: Cambridge University Press; 2000. [Google Scholar]
- 20.Regier DA, Kaelber CT, Rae DS, et al. Limitations of diagnostic criteria and assessment instruments for mental disorders. Implications for research and policy. Arch Gen Psychiatry. 1998;55:109–115. doi: 10.1001/archpsyc.55.2.109. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL. Diagnosis and need for treatment are not the same. Arch Gen Psychiatry. 1998;55:120. doi: 10.1001/archpsyc.55.2.120. [DOI] [PubMed] [Google Scholar]
- 22.Wakefield JC, Schmitz MF, First MB, Horwitz AV. Extending the bereavement exclusion for major depression to other losses: evidence from the National Comorbidity Survey. Arch Gen Psychiatry. 2007;64:433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Task Force on DSM-IV. Diagnostic and Statistical Manual of Mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 24.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klerman GL. Paradigm shifts in USA psychiatric epidemiology since World War II. Soc Psychiatry Psychiatr Epidemiol. 1990;25:27–32. doi: 10.1007/BF00789067. [DOI] [PubMed] [Google Scholar]
- 27.Robins LN, Regier DA. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: Free Press; 1991. [Google Scholar]
- 28.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–1031. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 29.Kessler RC, Zhao S, Katz SJ, et al. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Birnbaum H, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R) Biol Psychiatry. 2005;58:668–676. doi: 10.1016/j.biopsych.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harel O, Zhou XH. Multiple imputation: review of theory, implementation and software. Stat Med. 2007;26:3057–3077. doi: 10.1002/sim.2787. [DOI] [PubMed] [Google Scholar]
- 32.Jablensky A. Epidemiology of schizophrenia: the global burden of disease and disability. Eur Arch Psychiatry Clin Neurosci. 2000;250:274–285. doi: 10.1007/s004060070002. [DOI] [PubMed] [Google Scholar]
- 33.Eaton WW, Hall AL, Macdonald R, McKibben J. Case identification in psychiatric epidemiology: a review. Int Rev Psychiatry. 2007;19:497–507. doi: 10.1080/09540260701564906. [DOI] [PubMed] [Google Scholar]
- 34.Allgulander C. Psychoactive drug use in a general population sample, Sweden: correlates with perceived health, psychiatric diagnoses, and mortality in an automated record-linkage study. Am J Public Health. 1989;79:1006–1010. doi: 10.2105/ajph.79.8.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bromet EJ, Finch SJ, Carlson GA, et al. Time to remission and relapse after the first hospital admission in severe bipolar disorder. Soc Psychiatry Psychiatr Epidemiol. 2005;40:106–113. doi: 10.1007/s00127-005-0864-7. [DOI] [PubMed] [Google Scholar]
- 36.Jablensky A, Sartorius N, Ernberg G, et al. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl. 1992;20:1–97. doi: 10.1017/s0264180100000904. [DOI] [PubMed] [Google Scholar]
- 37.Mojtabai R, Herman D, Susser ES, et al. Service use and outcomes of first-admission patients with psychotic disorders in the Suffolk County Mental Health Project. Am J Psychiatry. 2005;162:1291–1298. doi: 10.1176/appi.ajp.162.7.1291. [DOI] [PubMed] [Google Scholar]
- 38.Becker T, Knapp M, Knudsen HC, et al. The EPSILON Study—a study of care for people with schizophrenia in five European centres. World Psychiatry. 2002;1:45–47. [PMC free article] [PubMed] [Google Scholar]
- 39.Knapp M, Chisholm D, Leese M, et al. Comparing patterns and costs of schizophrenia care in five European countries: the EPSILON study. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Acta Psychiatr Scand. 2002;105:42–54. doi: 10.1034/j.1600-0447.2002._10310.x. [DOI] [PubMed] [Google Scholar]
- 40.Cohen P, Cohen J. The clinician's illusion. Arch Gen Psychiatry. 1984;41:1178–1182. doi: 10.1001/archpsyc.1984.01790230064010. [DOI] [PubMed] [Google Scholar]
- 41.Bromet EJ, Schwartz JE, Fennig S, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18:243–255. doi: 10.1093/schbul/18.2.243. [DOI] [PubMed] [Google Scholar]
- 42.Lennon MC, McAllister W, Kuang L, Herman DB. Capturing intervention effects over time: reanalysis of a critical time intervention for homeless mentally ill men. Am J Public Health. 2005;95:1760–1766. doi: 10.2105/AJPH.2005.064402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muthen LK, Muthen BO. Mplus User's Guide. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- 44.Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychol Methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 45.Endicott J, Spitzer RL. Use of the Research Diagnostic Criteria and the Schedule for Affective Disorders and Schizophrenia to study affective disorders. Am J Psychiatry. 1979;136:52–56. doi: 10.1176/ajp.136.1.52. [DOI] [PubMed] [Google Scholar]
- 46.Jablensky A, McGrath J, Herrman H, et al. People Living With Psychotic Illness: An Australian Study 1997–98. Canberra, Australia: Commonwealth of Australia; 1999. [Google Scholar]
- 47.Carr VJ, Johnston PJ, Lewin TJ, Rajkumar S, Carter GL, Issakidis C. Patterns of service use among persons with schizophrenia and other psychotic disorders. Psychiatr Serv. 2003;54:226–235. doi: 10.1176/appi.ps.54.2.226. [DOI] [PubMed] [Google Scholar]
- 48.Warner R. Recovery From Schizophrenia: Psychiatry and Political Economy. 3rd ed. New York, NY: Brunner-Routledge; 2004. [Google Scholar]
- 49.West JC, Wilk JE, Olfson M, et al. Patterns and quality of treatment for patients with schizophrenia in routine psychiatric practice. Psychiatr Serv. 2005;56:283–291. doi: 10.1176/appi.ps.56.3.283. [DOI] [PubMed] [Google Scholar]
- 50.dosReis S, Johnson E, Steinwachs D, et al. Antipsychotic treatment patterns and hospitalizations among adults with schizophrenia. Schizophr Res. 2008;101:304–311. doi: 10.1016/j.schres.2007.12.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rosenheck RA, Desai R, Steinwachs D, Lehman A. Benchmarking treatment of schizophrenia: a comparison of service delivery by the national government and by state and local providers. J Nerv Ment Dis. 2000;188:209–216. doi: 10.1097/00005053-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Fischer EP, Owen RR. Quality of public sector care for schizophrenia in Arkansas. Ment Health Serv Res. 1999;1:213–221. doi: 10.1023/a:1022321407522. [DOI] [PubMed] [Google Scholar]
- 53.Walkup JT, McAlpine DD, Olfson M, Labay LE, Boyer C, Hansell S. Patients with schizophrenia at risk for excessive antipsychotic dosing. J Clin Psychiatry. 2000;61:344–348. doi: 10.4088/jcp.v61n0504. [DOI] [PubMed] [Google Scholar]
- 54.Yanos PT, Crystal S, Kumar R, Walkup JT. Characteristics and service use patterns of nonelderly Medicare beneficiaries with schizophrenia. Psychiatr Serv. 2001;52:1644–1650. doi: 10.1176/appi.ps.52.12.1644. [DOI] [PubMed] [Google Scholar]
- 55.Leslie DL, Rosenheck RA. Use of pharmacy data to assess quality of pharmacotherapy for schizophrenia in a national health care system: individual and facility predictors. Med Care. 2001;39:923–933. doi: 10.1097/00005650-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 56.Baldessarini RJ, Katz B, Cotton P. Dissimilar dosing with high-potency and low-potency neuroleptics. Am J Psychiatry. 1984;141:748–752. doi: 10.1176/ajp.141.6.748. [DOI] [PubMed] [Google Scholar]
- 57.Johnson DA, Wright NF. Drug prescribing for schizophrenic out-patients on depot injections. Repeat surveys over 18 years. Br J Psychiatry. 1990;156:827–834. doi: 10.1192/bjp.156.6.827. [DOI] [PubMed] [Google Scholar]
- 58.Owen RR, Feng W, Thrush CR, Hudson TJ, Austen MA. Variations in prescribing practices for novel antipsychotic medications among Veterans Affairs hospitals. Psychiatr Serv. 2001;52:1523–1525. doi: 10.1176/appi.ps.52.11.1523. [DOI] [PubMed] [Google Scholar]
- 59.Segal SP, Cohen D, Marder SR. Neuroleptic medication and prescription practices with sheltered-care residents: a 12-year perspective. Am J Public Health. 1992;82:846–852. doi: 10.2105/ajph.82.6.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sernyak MJ, Dausey D, Desai R, Rosenheck R. Prescribers’ nonadherence to treatment guidelines for schizophrenia when prescribing neuroleptics. Psychiatr Serv. 2003;54:246–248. doi: 10.1176/appi.ps.54.2.246. [DOI] [PubMed] [Google Scholar]
- 61.Strous RD, Bar F, Keret N, et al. Analysis of clinical characteristics and antipsychotic medication prescribing practices of first-episode schizophrenia in Israel: a naturalistic prospective study. Isr J Psychiatry Relat Sci. 2006;43:2–9. [PubMed] [Google Scholar]
- 62.Wheeler A, Humberstone V, Robinson G. Trends in antipsychotic prescribing in schizophrenia in Auckland. Australas Psychiatry. 2006;14:169–174. doi: 10.1080/j.1440-1665.2006.02273.x. [DOI] [PubMed] [Google Scholar]
- 63.Leslie DL, Rosenheck RA. Benchmarking the quality of schizophrenia pharmacotherapy: a comparison of the Department of Veterans Affairs and the private sector. J Ment Health Policy Econ. 2003;6:113–121. [PubMed] [Google Scholar]
- 64.Goldman M, Healy DJ, Florence T, Simpson L, Milner KK. Assessing conformance to medication treatment guidelines for schizophrenia in a community mental health center (CMHC) Community Ment Health J. 2003;39:549–555. doi: 10.1023/b:comh.0000003015.68850.f2. [DOI] [PubMed] [Google Scholar]
- 65.Mechanic D. Managing behavioral health in Medicaid. N Engl J Med. 2003;348:1914–1916. doi: 10.1056/NEJMe030040. [DOI] [PubMed] [Google Scholar]
- 66.Busch AB, Frank RG, Lehman AF. The effect of a managed behavioral health carve-out on quality of care for Medicaid patients diagnosed as having schizophrenia. Arch Gen Psychiatry. 2004;61:442–448. doi: 10.1001/archpsyc.61.5.442. [DOI] [PubMed] [Google Scholar]
- 67.Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull. 2004;30:193–217. doi: 10.1093/oxfordjournals.schbul.a007071. [DOI] [PubMed] [Google Scholar]
- 68.Bhanji NH, Chouinard G, Margolese HC. A review of compliance, depot intramuscular antipsychotics and the new long-acting injectable atypical antipsychotic risperidone in schizophrenia. Eur Neuropsychopharmacol. 2004;14:87–92. doi: 10.1016/S0924-977X(03)00109-3. [DOI] [PubMed] [Google Scholar]
- 69.Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63:892–909. doi: 10.4088/jcp.v63n1007. [DOI] [PubMed] [Google Scholar]
- 70.Mark TL, Palmer LA, Russo PA, Vasey J. Examination of treatment pattern differences by race. Ment Health Serv Res. 2003;5:241–250. doi: 10.1023/a:1026281118990. [DOI] [PubMed] [Google Scholar]
- 71.Busch AB, Frank RG, Lehman AF, Greenfield SF. Schizophrenia, co-occurring substance use disorders and quality of care: the differential effect of a managed behavioral health care carve-out. Adm Policy Ment Health. 2006;33:388–397. doi: 10.1007/s10488-006-0045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zygmunt A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159:1653–1664. doi: 10.1176/appi.ajp.159.10.1653. [DOI] [PubMed] [Google Scholar]
- 73.Frank RG, Berndt ER, Busch AB, Lehman AF. Quality-constant “prices” for the ongoing treatment of schizophrenia: an exploratory study*. Q Rev Econ Finance. 2004;44:390–409. doi: 10.1016/j.qref.2004.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ray WA, Daugherty JR, Meador KG. Effect of a mental health “carve-out” program on the continuity of antipsychotic therapy. N Engl J Med. 2003;348:1885–1894. doi: 10.1056/NEJMsa020584. [DOI] [PubMed] [Google Scholar]
- 75.Stiles PG, Boothroyd RA, Dhont K, Beiler PF, Green AE. Adherence to practice guidelines, clinical outcomes, and costs among Medicaid enrollees with severe mental illnesses. Eval Health Prof. 2009;32:69–89. doi: 10.1177/0163278708328744. [DOI] [PubMed] [Google Scholar]
- 76.Soumerai SB, Zhang F, Ross-Degnan D, et al. Use of atypical antipsychotic drugs for schizophrenia in Maine Medicaid following a policy change. Health Aff (Millwood) 2008;27:w185–w195. doi: 10.1377/hlthaff.27.3.w185. [DOI] [PubMed] [Google Scholar]
- 77.Simoni-Wastila L, Zuckerman IH, Shaffer T, Blanchette CM, Stuart B. Drug use patterns in severely mentally ill medicare beneficiaries: impact of discontinuities in drug coverage. Health Serv Res. 2008;43:496–514. doi: 10.1111/j.1475-6773.2007.00779.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wallace NT, Bloom JR, Hu TW, Libby AM. Medication treatment patterns for adults with schizophrenia in Medicaid managed care in Colorado. Psychiatr Serv. 2005;56:1402–1408. doi: 10.1176/appi.ps.56.11.1402. [DOI] [PubMed] [Google Scholar]
- 79.Chou AF, Wallace N, Bloom JR, Hu TW. Variation in outpatient mental health service utilization under capitation. J Ment Health Policy Econ. 2005;8:3–14. [PubMed] [Google Scholar]
- 80.Bromet EJ, Hamdy A. Paper presented at: Mental Health America. The Suffolk County Mental Health Project: physical health. June 2008; Washington, DC. [Google Scholar]
- 81.Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand. 2007;116:317–333. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 82.Druss BG, Bradford WD, Rosenheck RA, Radford MJ, Krumholz HM. Quality of medical care and excess mortality in older patients with mental disorders. Arch Gen Psychiatry. 2001;58:565–572. doi: 10.1001/archpsyc.58.6.565. [DOI] [PubMed] [Google Scholar]
- 83.Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506–511. doi: 10.1001/jama.283.4.506. [DOI] [PubMed] [Google Scholar]
- 84.Mitchell AJ, Malone D. Physical health and schizophrenia. Curr Opin Psychiatry. 2006;19:432–437. doi: 10.1097/01.yco.0000228767.71473.9e. [DOI] [PubMed] [Google Scholar]
- 85.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 86.Morrato EH, Newcomer JW, Allen RR, Valuck RJ. Prevalence of baseline serum glucose and lipid testing in users of second-generation antipsychotic drugs: a retrospective, population-based study of Medicaid claims data. J Clin Psychiatry. 2008;69:316–322. doi: 10.4088/jcp.v69n0219. [DOI] [PubMed] [Google Scholar]
- 87.Young AS, Niv N, Cohen AN, Kessler C, McNagny K. The appropriateness of routine medication treatment for schizophrenia. Schizophr Bull. doi: 10.1093/schbul/sbn138. November 07, 2008; doi:10.1093/schbul/sbn138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Himelhoch S, Leith J, Goldberg R, Kreyenbuhl J, Medoff D, Dixon L. Care and management of cardiovascular risk factors among individuals with schizophrenia and type 2 diabetes who smoke. Gen Hosp Psychiatry. 2009;31:30–32. doi: 10.1016/j.genhosppsych.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Meyer JM. Strategies for the long-term treatment of schizophrenia: real-world lessons from the CATIE trial. J Clin Psychiatry. 2007;68(suppl 1):28–33. [PubMed] [Google Scholar]
- 90.Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series. Washington, DC: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 91.Swartz MS, Wagner HR, Swanson JW, et al. Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study. J Nerv Ment Dis. 2006;194:164–172. doi: 10.1097/01.nmd.0000202575.79453.6e. [DOI] [PubMed] [Google Scholar]
- 92.Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophr Res. 1999;35(suppl):S93–S100. doi: 10.1016/s0920-9964(98)00161-3. [DOI] [PubMed] [Google Scholar]
- 93.Blanchard JJ, Brown SA, Horan WP, Sherwood AR. Substance use disorders in schizophrenia: review, integration, and a proposed model. Clin Psychol Rev. 2000;20:207–234. doi: 10.1016/s0272-7358(99)00033-1. [DOI] [PubMed] [Google Scholar]
- 94.Drake RE, Green AI. Current research on co-occurring substance-use disorder in schizophrenia. Schizophr Bull. 2006;32:616–617. doi: 10.1093/schbul/sbl020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Drake RE, Mueser KT, Brunette MF. Management of persons with co-occurring severe mental illness and substance use disorder: program implications. World Psychiatry. 2007;6:131–136. [PMC free article] [PubMed] [Google Scholar]
- 96.Drake RE, Mueser KT, Brunette MF, McHugo GJ. A review of treatments for people with severe mental illnesses and co-occurring substance use disorders. Psychiatr Rehabil J. 2004;27:360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- 97.Mojtabai R. Which substance abuse treatment facilities offer dual diagnosis programs? Am J Drug Alcohol Abuse. 2004;30:525–536. doi: 10.1081/ada-200032281. [DOI] [PubMed] [Google Scholar]
- 98.de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005;76:135–157. doi: 10.1016/j.schres.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 99.Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry. 1986;143:993–997. doi: 10.1176/ajp.143.8.993. [DOI] [PubMed] [Google Scholar]
- 100.Kotov R, Guey LT, Bromet EJ, Schwartz JE. Smoking in schizophrenia: diagnostic specificity, symptom correlates, and illness severity. Schizophr Bull. doi: 10.1093/schbul/sbn066. June 17, 2008; doi:10.1093/schbul/sbn1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Marchibroda JM. The impact of health information technology on collaborative chronic care management. J Manag Care Pharm. 2008;14:S3–S11. [PubMed] [Google Scholar]
- 102.Cavacuiti C, Svoboda T. The use of electronic medical records for homeless outreach. J Health Care Poor Underserved. 2008;19:1270–1281. doi: 10.1353/hpu.0.0090. [DOI] [PubMed] [Google Scholar]
- 103.Mojtabai R. Datapoints: use of information technology by psychiatrists and other medical providers. Psychiatr Serv. 2007;58:1261. doi: 10.1176/ps.2007.58.10.1261. [DOI] [PubMed] [Google Scholar]
- 104.Drake RE, McHugo GJ, Bebout RR, et al. A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Arch Gen Psychiatry. 1999;56:627–633. doi: 10.1001/archpsyc.56.7.627. [DOI] [PubMed] [Google Scholar]
- 105.Crowther RE, Marshall M, Bond GR, Huxley P. Helping people with severe mental illness to obtain work: systematic review. BMJ. 2001;322:204–208. doi: 10.1136/bmj.322.7280.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Latimer EA, Lecomte T, Becker DR, et al. Generalisability of the individual placement and support model of supported employment: results of a Canadian randomised controlled trial. Br J Psychiatry. 2006;189:65–73. doi: 10.1192/bjp.bp.105.012641. [DOI] [PubMed] [Google Scholar]
- 107.Twamley EW, Jeste DV, Lehman AF. Vocational rehabilitation in schizophrenia and other psychotic disorders: a literature review and meta-analysis of randomized controlled trials. J Nerv Ment Dis. 2003;191:515–523. doi: 10.1097/01.nmd.0000082213.42509.69. [DOI] [PubMed] [Google Scholar]
- 108.Drake RE, Bond GR. The future of supported employment for people with severe mental illness. Psychiatr Rehabil J. 2008;31:367–376. doi: 10.2975/31.4.2008.367.376. [DOI] [PubMed] [Google Scholar]
- 109.Resnick SG, Rosenheck R. Dissemination of supported employment in Department of Veterans Affairs. J Rehabil Res Dev. 2007;44:867–878. doi: 10.1682/jrrd.2007.02.0043. [DOI] [PubMed] [Google Scholar]
- 110.Rosenheck RA, Mares AS. Implementation of supported employment for homeless veterans with psychiatric or addiction disorders: two-year outcomes. Psychiatr Serv. 2007;58:325–333. doi: 10.1176/ps.2007.58.3.325. [DOI] [PubMed] [Google Scholar]
- 111.Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162:370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- 112.Hiday VA, Swartz MS, Swanson JW, Borum R, Wagner HR. Criminal victimization of persons with severe mental illness. Psychiatr Serv. 1999;50:62–68. doi: 10.1176/ps.50.1.62. [DOI] [PubMed] [Google Scholar]
- 113.Cournos F, McKinnon K, Sullivan G. Schizophrenia and comorbid human immunodeficiency virus or hepatitis C virus. J Clin Psychiatry. 2005;66(suppl 6):27–33. [PubMed] [Google Scholar]
- 114.Blank MB, Mandell DS, Aiken L, Hadley TR. Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatr Serv. 2002;53:868–873. doi: 10.1176/appi.ps.53.7.868. [DOI] [PubMed] [Google Scholar]
- 115.Carey MP, Carey KB, Maisto SA, Schroder KE, Vanable PA, Gordon CM. HIV risk behavior among psychiatric outpatients: association with psychiatric disorder, substance use disorder, and gender. J Nerv Ment Dis. 2004;192:289–296. doi: 10.1097/01.nmd.0000120888.45094.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Brekke JS, Prindle C, Bae SW, Long JD. Risks for individuals with schizophrenia who are living in the community. Psychiatr Serv. 2001;52:1358–1366. doi: 10.1176/appi.ps.52.10.1358. [DOI] [PubMed] [Google Scholar]
- 117.Susser E, Valencia E, Conover S, Felix A, Tsai WY, Wyatt RJ. Preventing recurrent homelessness among mentally ill men: a “critical time” intervention after discharge from a shelter. Am J Public Health. 1997;87:256–262. doi: 10.2105/ajph.87.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cleary M, Hunt GE, Walter G, Freeman A. The patient's view of need and caregiving consequences: a cross-sectional study of inpatients with severe mental illness. J Psychiatr Ment Health Nurs. 2006;13:506–514. doi: 10.1111/j.1365-2850.2006.00972.x. [DOI] [PubMed] [Google Scholar]
- 119.Hansson L, Vinding HR, Mackeprang T, et al. Comparison of key worker and patient assessment of needs in schizophrenic patients living in the community: a Nordic multicentre study. Acta Psychiatr Scand. 2001;103:45–51. doi: 10.1034/j.1600-0447.2001.00083.x. [DOI] [PubMed] [Google Scholar]
- 120.Wennstrom E, Sorbom D, Wiesel FA. Factor structure in the Camberwell Assessment of Need. Br J Psychiatry. 2004;185:505–510. doi: 10.1192/bjp.185.6.505. [DOI] [PubMed] [Google Scholar]
- 121.Wiersma D, van den Brink R, Wolters K, et al. Individual unmet needs for care: are they sensitive as outcome criterion for the effectiveness of mental health services interventions? Soc Psychiatry Psychiatr Epidemiol. 2009;44:317–324. doi: 10.1007/s00127-008-0432-z. [DOI] [PubMed] [Google Scholar]
- 122.Thornicroft G, Johnson S, Leese M, Slade M. The unmet needs of people suffering from schizophrenia. In: Andrews G, Henderson S, editors. Unmet Need in Psychiatry. Cambridge: Cambridge University Press; 2000. pp. 197–216. [Google Scholar]
- 123.Slade M, Phelan M, Thornicroft G. A comparison of needs assessed by staff and by an epidemiologically representative sample of patients with psychosis. Psychol Med. 1998;28:543–550. doi: 10.1017/s0033291798006564. [DOI] [PubMed] [Google Scholar]
- 124.Brewin C. Measuring individual needs for care and services. In: Thornicroft G, Brewin CR, Wing J, editors. Measuring Mental Health Needs. London, UK: Gaskell/Royal College of Psychiatrists; 1992. pp. 220–236. [Google Scholar]
- 125.Adams JR, Drake RE. Shared decision-making and evidence-based practice. Community Ment Health J. 2006;42:87–105. doi: 10.1007/s10597-005-9005-8. [DOI] [PubMed] [Google Scholar]
- 126.Adams JR, Drake RE, Wolford GL. Shared decision-making preferences of people with severe mental illness. Psychiatr Serv. 2007;58:1219–1221. doi: 10.1176/ps.2007.58.9.1219. [DOI] [PubMed] [Google Scholar]
- 127.O'Neal EL, Adams JR, McHugo GJ, Van Citters AD, Drake RE, Bartels SJ. Preferences of older and younger adults with serious mental illness for involvement in decision-making in medical and psychiatric settings. Am J Geriatr Psychiatry. 2008;16:826–833. doi: 10.1097/JGP.0b013e318181f992. [DOI] [PubMed] [Google Scholar]
- 128.Amador XF, Flaum M, Andreasen NC, et al. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994;51:826–836. doi: 10.1001/archpsyc.1994.03950100074007. [DOI] [PubMed] [Google Scholar]
- 129.Amador XF, David AS. Insight and Psychosis. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 130.Seale C, Chaplin R, Lelliott P, Quirk A. Sharing decisions in consultations involving anti-psychotic medication: a qualitative study of psychiatrists’ experiences. Soc Sci Med. 2006;62:2861–2873. doi: 10.1016/j.socscimed.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 131.Hamann J, Cohen R, Leucht S, Busch R, Kissling W. Shared decision making and long-term outcome in schizophrenia treatment. J Clin Psychiatry. 2007;68:992–997. doi: 10.4088/jcp.v68n0703. [DOI] [PubMed] [Google Scholar]
- 132.Levav I, Kohn R, Dohrenwend BP, et al. An epidemiological study of mental disorders in a 10-year cohort of young adults in Israel. Psychol Med. 1993;23:691–707. doi: 10.1017/s0033291700025472. [DOI] [PubMed] [Google Scholar]
- 133.Sartorius N, Schulze H. Global Programme of the World Psychiatric Association. Reducing the Stigma of Mental Illness: A Report From a Global Programme of the World Psychiatric Association. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 134.Jorm AF, Christensen H, Griffiths KM. The impact of beyondblue: the national depression initiative on the Australian public's recognition of depression and beliefs about treatments. Aust N Z J Psychiatry. 2005;39:248–254. doi: 10.1080/j.1440-1614.2005.01561.x. [DOI] [PubMed] [Google Scholar]
- 135.Paykel ES, Hart D, Priest RG. Changes in public attitudes to depression during the Defeat Depression Campaign. Br J Psychiatry. 1998;173:519–522. doi: 10.1192/bjp.173.6.519. [DOI] [PubMed] [Google Scholar]
- 136.Angermeyer MC, Matschinger H. Have there been any changes in the public's attitudes towards psychiatric treatment? Results from representative population surveys in Germany in the years 1990 and 2001. Acta Psychiatr Scand. 2005;111:68–73. doi: 10.1111/j.1600-0447.2004.00441.x. [DOI] [PubMed] [Google Scholar]
- 137.Jorm AF, Christensen H, Griffiths KM. The public's ability to recognize mental disorders and their beliefs about treatment: changes in Australia over 8 years. Aust N Z J Psychiatry. 2006;40:36–41. doi: 10.1080/j.1440-1614.2006.01738.x. [DOI] [PubMed] [Google Scholar]
- 138.Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J, Weiden PJ. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2000;51:216–222. doi: 10.1176/appi.ps.51.2.216. [DOI] [PubMed] [Google Scholar]
- 139.Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull. 1995;21:419–429. doi: 10.1093/schbul/21.3.419. [DOI] [PubMed] [Google Scholar]
- 140.Nose M, Barbui C, Gray R, Tansella M. Clinical interventions for treatment non-adherence in psychosis: meta-analysis. Br J Psychiatry. 2003;183:197–206. doi: 10.1192/bjp.183.3.197. [DOI] [PubMed] [Google Scholar]
- 141.Velligan DI, Mueller J, Wang M, et al. Use of environmental supports among patients with schizophrenia. Psychiatr Serv. 2006;57:219–224. doi: 10.1176/appi.ps.57.2.219. [DOI] [PubMed] [Google Scholar]
- 142.Byerly MJ, Fisher R, Carmody T, Rush AJ. A trial of compliance therapy in outpatients with schizophrenia or schizoaffective disorder. J Clin Psychiatry. 2005;66:997–1001. doi: 10.4088/jcp.v66n0806. [DOI] [PubMed] [Google Scholar]
- 143.Kemp R, Hayward P, Applewhaite G, Everitt B, David A. Compliance therapy in psychotic patients: randomised controlled trial. BMJ. 1996;312:345–349. doi: 10.1136/bmj.312.7027.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.O'Donnell C, Donohoe G, Sharkey L, et al. Compliance therapy: a randomised controlled trial in schizophrenia. BMJ. 2003;327:834. doi: 10.1136/bmj.327.7419.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Falloon IR, Montero I, Sungur M, et al. Implementation of evidence-based treatment for schizophrenic disorders: two-year outcome of an international field trial of optimal treatment. World Psychiatry. 2004;3:104–109. [PMC free article] [PubMed] [Google Scholar]
- 146.Andrews G, Sanderson K, Corry J, Issakidis C, Lapsley H. Cost-effectiveness of current and optimal treatment for schizophrenia. Br J Psychiatry. 2003;183:427–435. doi: 10.1192/bjp.183.5.427. [DOI] [PubMed] [Google Scholar]
- 147.Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997;157:408–416. [PMC free article] [PubMed] [Google Scholar]
- 148.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 149.Walter LC, Davidowitz NP, Heineken PA, Covinsky KE. Pitfalls of converting practice guidelines into quality measures: lessons learned from a VA performance measure. JAMA. 2004;291:2466–2470. doi: 10.1001/jama.291.20.2466. [DOI] [PubMed] [Google Scholar]
- 150.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:2218–2227. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 151.Rosenheck R, Cicchetti D. A mental health program report card: a multidimensional approach to performance monitoring in public sector programs. Community Ment Health J. 1998;34:85–106. doi: 10.1023/a:1018720414126. [DOI] [PubMed] [Google Scholar]
- 152.Owen RR, Hudson T, Thrush C, Thapa P, Armitage T, Landes RD. The effectiveness of guideline implementation strategies on improving antipsychotic medication management for schizophrenia. Med Care. 2008;46:686–691. doi: 10.1097/MLR.0b013e3181653d43. [DOI] [PubMed] [Google Scholar]
- 153.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA. 2005;294:1788–1793. doi: 10.1001/jama.294.14.1788. [DOI] [PubMed] [Google Scholar]
- 154.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355:375–384. doi: 10.1056/NEJMsa055505. [DOI] [PubMed] [Google Scholar]
- 155.Doran T, Fullwood C, Reeves D, Gravelle H, Roland M. Exclusion of patients from pay-for-performance targets by English physicians. N Engl J Med. 2008;359:274–284. doi: 10.1056/NEJMsa0800310. [DOI] [PubMed] [Google Scholar]
- 156.Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006;145:265–272. doi: 10.7326/0003-4819-145-4-200608150-00006. [DOI] [PubMed] [Google Scholar]
- 157.Glickman SW, Ou FS, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007;297:2373–2380. doi: 10.1001/jama.297.21.2373. [DOI] [PubMed] [Google Scholar]
- 158.Kurtz MM, Mueser KT. A meta-analysis of controlled research on social skills training for schizophrenia. J Consult Clin Psychol. 2008;76:491–504. doi: 10.1037/0022-006X.76.3.491. [DOI] [PubMed] [Google Scholar]
- 159.Mueser KT, Penn DL. Meta-analysis examining the effects of social skills training on schizophrenia. Psychol Med. 2004;34:1365–1367. doi: 10.1017/s0033291704213848. [DOI] [PubMed] [Google Scholar]