Abstract
Background
Evidence suggests gender differences in abuse of prescription opioids. This study aimed to describe characteristics of women who abuse prescription opioids in a treatment-seeking sample and to contrast gender differences among prescription opioid abusers.
Methods
Data collected November 2005 to April 2008 derived from the Addiction Severity Index Multimedia Version Connect (ASI-MV® Connect) database. Bivariate and multivariable logistic regression examined correlates of prescription opioid abuse stratified by gender.
Results
29,906 assessments from 220 treatment centers were included, of which 12.8% (N=3,821) reported past month prescription opioid abuse. Women were more likely than men to report use of any prescription opioid (29.8% females vs. 21.1% males, p< 0.001) and abuse of any prescription opioid (15.4% females vs. 11.1% males, p < 0.001) in the past month. Route of administration and source of prescription opioids displayed gender-specific tendencies. Women-specific correlates of recent prescription opioid abuse were problem drinking, age <54, inhalant use, residence outside of West US Census region, and history of drug overdose. Men-specific correlates were age <34, currently living with their children, residence in the South and Midwest, hallucinogen use, and recent depression. Women prescription opioid abusers were less likely to report a pain problem although they were more likely to report medical problems than women who abused other drugs.
Conclusions
Gender-specific factors should be taken into account in efforts to screen and identify those at highest risk of prescription opioid abuse. Prevention and intervention efforts with a gender-specific approach are warranted.
Keywords: Gender, opioids, prescription opioids, substance-related disorders, surveillance, overdose
1. Introduction
Over the past few decades, the number and available potency of pharmaceutical prescription opioids has expanded dramatically (Volkow, 2008), equipping clinicians with a much needed, wider array of analgesics in the treatment of pain. However, because these same key drugs are potentially abuseable, these advances have been subjected to careful scrutiny prior to their approval for therapeutic use and, even after their approval, as the objects of potential diversion and abuse. Estimates from the U.S. National Survey on Drug Use among Households (NSDUH) from 1990 to 2006, reflect trends of increasing self-reported recent abuse of prescription opioids (Cicero et al., 2005; Dasgupta et al., 2006; Galaif et al., 2001; Gilson et al., 2004; SAMHSA, 2006; Zacny et al., 2003). During the same period, the number of prescription opioid-involved deaths increased (Paulozzi et al., 2006), with some areas of the country now reporting more than 90% of unintentional poisoning deaths attributable to prescription opioids (Hall et al., 2008). Many explanations for this upsurge in prescription opioid abuse exist including increases in prescribing practices (Wisniewski et al., 2008), expansion of medical use of opioids in primary care (Reid et al., 2002), the introduction of multiple potent and modified-release formulations (Goodman and Glassman, 2005), the increase in prescribing of methadone for outpatient pain management (Nicholson, 2007), and limited opioid substitution treatment options (Brands et al., 2004; Hall et al., 2008).
Women represent a large and growing population of prescription opioid abusers (Cicero et al., 2008; SAMHSA, 2006; Tetrault et al., 2008). Unlike for heroin, an equal or greater proportion of women appear to abuse prescription opioids (Kelly et al., 2008; Simoni-Wastila et al., 2004). It is well-established that various gender differences exist, including those rooted in biology (Lynch et al., 2002), which may influence the abuse of alcohol and illicit drugs. For example, women drug abusers are more likely than men to report psychiatric problems (Lin et al., 2004; Milani et al., 2004) and histories of physical, emotional, and/or sexual abuse (Galaif et al., 2001; Gentilello et al., 2000) which put them at greater risk of abuse of drugs. Studies conducted outside of the United States suggest worrying increases in abuse of prescription opioids among women who obtained these drugs through their own prescriptions (2005; Lloyd, 2008). Women tend to use and to be prescribed abuseable medications more often than men (Isacson and Bingefors, 2002; Simoni-Wastila, 1998) and are more likely to report prescription opioids as their primary drug of abuse (Office of Applied Statistics, 2001, 2005). Despite these trends, there have been few efforts to explore the nature of prescription opioid abuse among women or to understand the special considerations for diagnosis, prevention, drug-related risks and treatment of women who abuse prescription opioids in the United States.
This study examined data from patients entering substance abuse treatment to explore the role of gender in abuse of prescription opioids. Specifically, there were two aims: first, to describe the characteristics of women as compared to men who abuse prescription opioids in a treatment-seeking sample and second, to contrast gender differences among prescription opioid abusers in order to identify gender-specific correlates of abuse.
2. Methods
2.1 Data source
Participants for this study comprised of clients 18 years and older attending substance abuse treatment centers across the United States who completed the Addiction Severity Index-Multimedia Version® (ASI-MV®) Connect (Butler et al., 2008) (see description below) as part of their treatment experience. The ASI-MV® Connect is a commercial product, purchased by treatment facilities for efficient and cost-effective patient evaluation and treatment planning purposes and is used as part of the standard clinical intake. Treatment centers in the ASI-MV® Connect network include primarily inpatient/residential units, outpatient non-methadone sites, and methadone maintenance programs, but respondents also may have completed the ASI-MV® Connect as part of their experience in drug court, probation/parole, TANF (Temporary Assistance for Needy Families) programs, or DWI/DUI (Driving While Intoxicated/Driving Under the Influence) programs. Thus, the data presented here are collected as part of ongoing clinical care and not as part of a study. Patient level data are made HIPAA (Health Insurance Portability and Accountability Act) compliant, de-identified, and uploaded to a server at Inflexxion, Inc. The research reported here is exempt from IRB policy since it uses de-identified patient data collected under a Business Associate Agreement and Limited Data Set Use Agreement with participating treatment facilities around the country under conditions specified under the Code of Federal Regulations.
The ASI-MV® Connect is a component of the National Addictions Vigilance Intervention and Prevention Program (NAVIPPRO™) (Butler et al., 2008). NAVIPPRO™ is a comprehensive risk management system for prescription opioids and other Schedule II and III therapeutic agents. The Food and Drug Administration (FDA) developed guidelines (DHHS, 2008) for pharmaceutical companies that make or submit new drug applications (NDAs) for substances with potential for abuse or addiction. These guidelines call for the creation of Risk Evaluation and Mitigation Strategy plans (called REMS), previously known as risk minimization action plans, or RiskMAPs, that include post-marketing surveillance to monitor indicators that might suggest the occurrence of adverse events, such as an emerging trend of abuse. NAVIPPRO™ was developed to provide post-marketing surveillance, signal detection, signal verification, and targeted prevention and intervention strategies. ASI-MV® Connect data are used as part of NAVIPPRO™ to monitor prescription abuse reported by individuals entering substance abuse treatment (see (Butler et al., 2008)), alongside other data sources including publicly available datasets, such as the National Survey on Drug Use & Health (NSDUH), the Treatment Episode Data Set (TEDS), the FDA Adverse Event Reporting System (FDA-AERS), the Drug Abuse Warning Network (DAWN Live!), and the American Association of Poison Control Centers’ (AAPCC) New Core System database (NCSBeta) and a proprietary database of Internet posts called Web Informed Services (WIS). These data are also examined, as the ASI-MV® Connect data are here, to increase our understanding of abuse patterns and trends in the United States.
2.2. Measures: ASI-MV® Connect
The ASI-MV® Connect is a continuous, real-time data stream that collects data on substances used and abused by adult clients (18 years or older) entering a substance abuse treatment. The ASI-MV® is a modified version of the Addiction Severity Index (ASI); a standard intake assessment designed for use upon treatment admission with demonstrated reliability and validity (Hendricks et al., 1989). The ASI assesses severity of addiction and the need for treatment (McLellan et al., 1992; McLellan et al., 1980) by measuring patients’ medical, employment, drug, legal, family and social relationships, and psychiatric problems. The ASI-MV® is a computer-administered version of the traditional ASI interview that is conducted by on-screen interviewers who present the questionnaire items according to a tree-logic that asks follow up questions only when appropriate, simulating a live interviewer. ASI questions are presented in both text and audio to address literacy limitations. An upgraded version of the ASI-MV®, called the ASI-MV® Connect, collects product-specific, geographically sensitive information about prescription opioids in addition to questions about the client’s route(s) of administration (oral, smoking, snorting, injecting), source of drug, presence of pain and pain treatment. The ASI-MV® Connect is web-enabled so that de-identified client information is uploaded to a central server and is, therefore, available immediately for review and analysis.
Prescription opioid use was operationalized as self-reported past 30-day use of any prescription opioid while prescription opioid abuse was operationalized as self-reported past 30-day use of any prescription opioid “in a way not prescribed by your doctor, that is, taking it for the way it makes you feel and not for pain relief”. The focus of this analysis is on abuse of prescription opioids, however, we present limited data on self-reported use of prescription opioids to reflect the high prevalence of any use (e.g., for medical purposes, for psycho-physiologic effects, etc.) in the population. The ASI-MV® Connect currently tracks 64 branded and generic prescription opioids. In addition to prescription drug variables, the ASI-MV obtains self-report of a number of medical, psychosocial and psychiatric variables (McLellan et al., 1992; McLellan et al., 1980). Relevant variables, considered for this analysis, included socio-demographics (age, race/ethnicity, gender, employment and educational status defined as < and ≥ 12 yrs education, currently living with their children, currently living with anyone who uses non-prescription drugs, family conflicts, incarceration history, patient’s 3-digit residential ZIP code, Census region of respondent’s residence), current illicit drug use by substance, duration of any illicit drug use, history of overdose, concurrent medical and psychiatric problems/symptoms, presence of chronic pain, treatment for pain, current receipt of psychiatric medications, and product-specific source and route of administration of prescription opioids tracked by the ASI-MV® Connect. Drugs of abuse that are monitored, in addition to prescription opioids, include alcohol, heroin, methadone maintenance, barbiturates, sedatives/hypnotics/tranquilizers (grouped together), cocaine, amphetamines, cannabis, hallucinogens, and inhalants (all inhalants grouped together). Medical and psychiatric problems were self-reported symptoms and problems and not diagnosed conditions. The medical problems variable was dichotomized as yes/no if the respondent reported experiencing physical or medical problems (e.g., illness, pains, discomfort, disability, or a severe cold or flu but not including drug or alcohol symptoms or withdrawal) for more than one day in the past thirty. The psychiatric problems inquired about in the ASI-MV® Connect and analyzed for this study included past 30-day experience of depression, anxiety, hallucinations, violence (i.e., “trouble controlling violent behavior including episodes of rage, or violence”), suicidal thoughts, and suicide attempts. To clarify, questions asking about self-reported pain problems, medical problems, and being prescribed pain medications were asked of all respondents and receipt of these questions did not depend on responses to earlier questions. Thus, it was possible to report being prescribed pain medications but to not currently be experiencing a medical or pain problem.
2.3 Study Sample
The study sample consisted of 29,906 assessments from people entering substance abuse treatment from November 2005 through March 2008, of whom 3,821 (12.8%) self-reported abuse of prescription opioids in the past month. Assessments were conducted in 220 treatment centers representing 175 unique site 5-digit zip codes and 362 unique client 3-digit zip codes. The mean age of the sample was 34.9 years (SD = 11.6, range 13 to 87); males represented 61% of the sample. Approximately half (47%) of the sample was non-white, with 8% African-American, 31% Hispanic/Latino, 1% Asian, 6% Native American, and 1% other ethnicity.
2.4 Data analysis
The first goal of the study aimed to describe the characteristics of women, as compared to men, who abused prescription opioids. Descriptive and bivariate analyses (i.e., χ2 tests, t-tests, or other appropriate non-parametric tests) were conducted among prescription opioid abusers only (i.e., patients endorsing non-medical use of any prescription opioid in the past 30 days; N=3,821). To accomplish the second aim of identifying correlates of prescription opioid abuse, we performed multivariable logistic regression analyses using the full dataset (N=29,906), stratified by gender. Since evidence suggests that gender may be an important moderator of prescription opioid abuse (Tetrault et al., 2008) and women drug abusers differ from men who abuse drugs, we performed stratification rather than including a series of model interaction terms. Using bivariate analysis and a cutoff of p<0.15, the modeling approach consisted of first screening for possible correlates, selected for testing based on the literature (Becker et al., 2008; Cicero et al., 2008; Grau et al., 2007; Tetrault et al., 2008). This screening was done separately for men and women. We then incorporated candidate variables into gender-specific multivariable models in a non-automated backward stepwise fashion, testing for changes in statistical significance, improved model fit, and evidence of confounding. The final and most parsimonious models incorporated variables that reached statistical significance at the p<0.05 level, improved model fit, or were important demographic variables regardless of statistical significance (e.g., educational status). The logistic models also included dummy variables for the year of data collection to control for possible period effects, and U.S. Census region (Northeast, South, West, Midwest) to control for geographic differences. We report adjusted odds ratios (AOR) and 95% confidence intervals (CI). SPSS version 16.0 (Chicago, IL) was used to conduct all analyses.
3. Results
Of the 29,906 assessments, approximately one third (34.5%) of respondents reported any use of prescription opioids in the past 30 days while 12.8% (N=3,821) self-reported abuse of prescription opioids in the past 30 days. Overall, 44.3% of respondents reported experiencing a medical problem in the past month. Notably, 33.9% of the full sample reported having a pain problem.
Gender differences were detected at the most fundamental levels of prescription opioid use and abuse. Women were more likely than men to report use of any prescription opioid in the past 30 days (29.8% females vs. 21.1% males, χ2=291.92, p<0.001) as well as abuse of prescription opioids in the past 30 days (15.4% females vs. 11.1% males, χ2=117.32, p<0.001).
3.1 Gender differences among recent prescription opioid abusers
Differences between men and women who reported prescription opioid abuse in the past 30 days (N = 3,821) are reported in Table 1. Although there were important between-gender differences, there were also some marked similarities. Women reported use of methadone, cocaine, inhalants, barbiturates, and to have injected a prescription opioid in the past month at rates similar to men (all p>0.05). They were also equally as likely to report having a pain problem and to have comparable histories of overdose (all p>0.05). However, compared to their male counterparts, women who reported recent prescription opioid abuse tended to be younger (aged 21 to 34), less ethnically diverse, divorced, separated or widowed, to live with their children, report more recent family conflicts, were less likely to have histories of incarceration and of drug injection, and were less likely employed in skilled manual labor. Women who reported abuse of prescription opioids reported less hazardous drinking, less concurrent heroin and marijuana use but more concurrent benzodiazepine and amphetamine use than the men. They were more likely to report experiencing medical problems than their male counterparts. Different from the men, women prescription opioid abusers were more likely to have been prescribed and taking medication for pain problems and reported higher rates of lifetime emotional, physical and sexual abuse; being troubled by psychological problems; and higher endorsement of most recent psychiatric problems, except for hallucinations and suicidal thoughts. Women reporting recent prescription opioid abuse also reported a higher rate of being prescribed psychiatric medication. Markers of help-seeking behavior (medical or psychiatric help, receipt of prescribed medications, or emergency room attendance) distinguished the females from the males who reported abuse of prescription opioids.
Table 1.
Gender differences among recent prescription opioid abusers: Socio-demographic and health status characteristics (N=3821)
| Variable | Men | Women | χ2 | p-value |
|---|---|---|---|---|
| Age category | ||||
| <21 | 7.5 | 6.9 | 13.05 | 0.005 |
| 21–34 | 53.2 | 56.1 | ||
| 35–54 | 34.9 | 34.7 | ||
| 55+ | 4.4 | 2.4 | ||
| Non-white minority | 30.2 | 26.2 | 7.16 | 0.007 |
| Marital status | ||||
| Married | 21.8 | 22.7 | 47.29 | <.0001 |
| Divorced/separated/widowed | 21.6 | 30.5 | ||
| Never married | 56.6 | 46.8 | ||
| Lives with children | 28.3 | 42.3 | 81.45 | <.0001 |
| Serious family conflicts, past 30 days | 35.6 | 46.7 | 49.13 | <.0001 |
| ≥ 12 yrs education | 71 | 71.9 | 0.36 | NS |
| Usual/last occupation | ||||
| Professional/management | 11.6 | 18.9 | 849.80 | <.0001 |
| Clerical/sales | 6.4 | 18.6 | ||
| Skilled manual | 39.7 | 5.2 | ||
| Semi-skilled | 10.1 | 10.5 | ||
| Homemaker | 0.9 | 13.3 | ||
| Student | 5.1 | 6.2 | ||
| Disabled | 2.4 | 2.8 | ||
| None/unskilled/did not work | 16 | 14.9 | ||
| Did not work for pay in past 3 years | 7.9 | 9.6 | ||
|
| ||||
| Past 30 days: | ||||
| Alcohol to intoxication >3 times/wk | 20.2 | 14.4 | 22.48 | <.0001 |
| Drugs also used | ||||
| Heroin | 22.2 | 14.2 | 40.21 | <.0001 |
| Methadone | 23.4 | 21.7 | 1.62 | NS |
| Benzodiazepine | 41.8 | 51.4 | 35.23 | <.0001 |
| Cocaine | 36.9 | 38.1 | 0.623 | NS |
| Amphetamine | 12.6 | 17.5 | 18.55 | <.0001 |
| Marijuana | 51.9 | 47.3 | 8.16 | 0.004 |
| Barbiturate | 7.8 | 9.1 | 1.98 | NS |
| Inhalant | 2.0 | 1.8 | 0.28 | NS |
| Hallucinogen | 4.2 | 2.5 | 8.12 | 0.004 |
| Used >1 substance | 69.8 | 65.8 | 6.90 | 0.009 |
| Injected a prescription opioid | 20.6 | 18.4 | 2.99 | NS |
|
| ||||
| Lifetime history of: | ||||
| Drug injection | 44.4 | 39 | 11.45 | 0.001 |
| Overdose | 37.5 | 38.8 | 0.71 | NS |
| Incarceration | 60.7 | 36 | 231.90 | <.0001 |
| Emotional abuse | 55.5 | 81.4 | 280.20 | <.0001 |
| Physical abuse | 36.8 | 69.3 | 392.30 | <.0001 |
| Sexual abuse | 15.5 | 52.8 | 581.30 | <.0001 |
|
| ||||
| Self-reported medical conditions & problems, past 30 days: | ||||
| Medical problems (any, not including drug or alcohol symptoms or withdrawal) | 61.2 | 69.6 | 29.47 | <.0001 |
| Receiving help from medical professional for medical problem | 43.5 | 49.6 | 9.10 | 0.003 |
| Has a pain problem | 55.2 | 54.5 | 0.20 | NS |
| Taken prescribed medication for pain | 36 | 41.5 | 12.28 | <.0001 |
| Emergency room visits | ||||
| 0 | 64.1 | 60.1 | 6.60 | 0.037 |
| 1 to 5 | 34.3 | 38.0 | ||
| >5 | 1.5 | 1.8 | ||
| Currently pregnant | -- | 5.9 | ||
|
| ||||
| Self-reported psychiatric problems, past 30 days: | ||||
| Depression | 56.6 | 69.4 | 63.72 | <.0001 |
| Anxiety | 63.9 | 78.7 | 98.31 | <.0001 |
| Hallucinations | 12.2 | 13.5 | 1.43 | NS |
| Trouble understanding | 56 | 68.8 | 63.73 | <.0001 |
| Violent* | 30.5 | 34.6 | 7.09 | 0.008 |
| Suicidal thoughts | 12 | 14.1 | 3.73 | NS |
| Suicide attempts | 4.6 | 6.2 | 4.68 | 0.03 |
| Troubled by any of psychiatric problems above (considerably-extremely) | 37.3 | 53.9 | 105.80 | <.0001 |
| Prescribed psychiatric medications | 27.6 | 42.1 | 87.78 | <.0001 |
Participant reported experiencing “trouble controlling violent behavior including episodes of rage, or violence” in the past 30 days
3.2 Prescription opioid abuse product-specific differences by gender
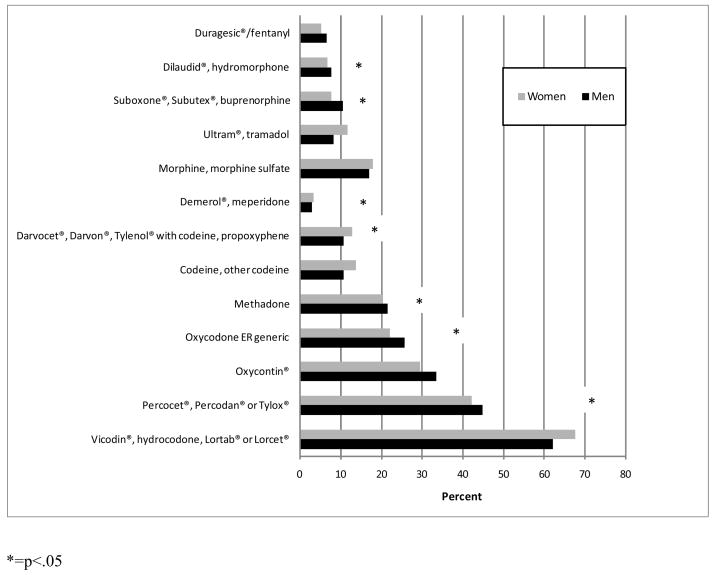
Among this treatment population, women were more likely than men to report abuse of Ultram®/tramadol (11.8% women vs. 8.4% men, p<0.001), propoxyphene formulations (12.9% women vs. 10.8% men, p=0.049), codeine (13.8% women vs. 10.8% men, p=0.005), and Vicodin®/hydrocodone formulations (67.6% women vs. 62.1% men, p<0.001) (Figure 1). Men in this treatment population were more likely than women to report abuse of buprenorphine formulations (10.7% men vs. 7.8% women, p=0.002), OxyContin® (33.6% men vs. 29.6% women, p=0.008), and generic oxycodone ER (25.7% men vs. 22.2% women, p=0.01). There were no gender differences for any of the other drug classes or products.
Figure 1.
Abuse of prescription opioids in the past 30 days by gender
3.3 Route of administration of prescription opioids
Men and women reported similar means of taking the prescription opioids they abused, administering them primarily orally, by inhalation, or by injection, and rarely by smoking (all product-specific comparisons, p>0.05). More men than women who reported prescription opioid abuse had a history of injecting any drug (44.4 % vs. 39%, respectively, p=0.001) but both men and women reported similar past month injection of a prescription opioid (20.6% vs. 18.4%, p>0.05). Of the branded prescription opioids, only OxyContin® was more likely to be injected by men than women (37.3% vs. 31.3%, respectively, p=0.02).
3.4 Source of prescription opioids abused by respondents
A variety of sources were indicated as means to acquire prescription opioids, with gender differences observed. Prescription opioid brand differences were detected; therefore, results in Table 2 depict data at this level of specificity. For women, prescription opioids were more likely obtained from family, friends or acquaintances or from their own prescriptions, whereas men were more likely to report obtaining prescription opioids from dealers (Table 2); in each instance, women were as or more likely than men to report their own prescription(s) as source of diverted pharmaceutical. Relative rankings of prescription opioid sources also reveal abuse patterns by gender. For example, women reported obtaining Vicodin® primarily from friends, family, or acquaintances (44.6%), followed by a dealer (37.5%), then their own prescriptions (28.8%) but men obtained Vicodin® primarily from a dealer (45.2%), followed by friends, family, or acquaintances (40.6%), and finally their own prescriptions (25.4%). A high percentage of both men and women reported obtaining prescription opioids from a dealer, suggesting strong street market forces for these drugs. By contrast, other prescription opioids, such as Vicodin® and Lortab®, suggest social networks as a key source for women but not for men. Other sources of prescription opioids (e.g., multiple doctors, stealing, Internet) represented less than 15% of responses rendering low power to test for gender differences.
Table 2.
Significant gender differences in source of prescription opioid abused in the past 30 days
| Family, friends, acquaintance | Dealer | Own prescriptions | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Men % | Women % | pvalue | Men % | Women % | pvalue | Men % | Women % | pvalue | |
| Lortab® (n=1512) | 35.4 | 45.3‡ | <0.0001 | 50.6† | 40.4 | <0.0001 | 24.3 | 31.9‡ | 0.001 |
| Vicodin® (n=1334) | 40.6 | 44.6 | NS | 45.2† | 37.5 | 0.004 | 25.4 | 28.8 | NS |
| Lorcet® (n=389) | 33.3 | 44.5‡ | 0.024 | 73.2† | 51.8 | 0.0001 | 13.1 | 20.9‡ | 0.04 |
| Other hydrocodone (n=981) | 36.3 | 43‡ | 0.033 | 53.7† | 44.4 | 0.004 | 23.5 | 27.1 | NS |
| Percocet® (n=1410) | 33.2 | 43.7‡ | 0.001 | 52.3† | 40.2 | 0.0001 | 20.4 | 26.6‡ | 0.006 |
| Oxycontin® (n=1305) | 29.4 | 40.6‡ | <0.0001 | 70.1† | 61.7 | 0.001 | 10.4 | 10.4 | NS |
| Methadone* (n=565) | 30.7 | 39.8‡ | 0.025 | 62.8 | 55 | NS | 15.9 | 19.3 | NS |
| Darvocet® (n=369) | 45 | 36.5 | NS | 26.6† | 14.5 | 0.004 | 27.8 | 40‡ | 0.014 |
| Tylenol® with codeine (n=150) | 38 | 45.1 | NS | 35.4† | 16.9 | 0.01 | 21.5 | 35.2 | NS |
| Morphine (n=132) | 28.8 | 49.3‡ | 0.017 | 59.3 | 53.4 | NS | 5.1 | 11 | NS |
| Ultram® (n=322) | 25.5 | 37.3‡ | 0.026 | 13.1 | 11.4 | NS | 54.7 | 49.7 | NS |
| Fentanyl (n=209) | 34.7 | 32.9 | NS | 61.3† | 47.1 | 0.042 | 4 | 15.3‡ | 0.004 |
Men significantly greater than women
Women significantly greater than men
Mallinckrodt tablet formulation
NS=not statistically significant
3.5 Correlates of prescription opioid abuse: Stratified multivariable regressions
Table 3 presents results of the multivariable logistic regression analyses of risk factors for prescription opioid abuse, stratified by gender. For both genders, factors associated with past month prescription opioid abuse included demographics (ethnicity, age, geographic location), social circumstances (serious recent family conflicts, living with someone who uses non-prescription drugs, lacking a history of incarceration), emotional and psychiatric considerations (not having a history of emotional abuse, recent psychiatric problems, not taking psychiatric medications), medical condition (having taken prescribed medications for pain, recent visits to the emergency room), and drug use factors (history of drug injection, concurrent use of other drugs, longer durations of illegal drug use). While these factors reflected similarities in magnitude and direction of association, other differences persist.
Table 3.
Multivariable logistic regression results: Correlates of prescription opioid abuse by gender
| Men (n=16,189) | Women (n=10,429) | |||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | |||
| Non-white minority | 0.84 | 0.72 | 0.98 | 0.71 | 0.60 | 0.85 |
| History of injection | 1.88 | 1.59 | 2.21 | 1.60 | 1.34 | 1.91 |
| Age (ref=<21) | ||||||
| 21–34 | 1.11 | 0.86 | 1.44 | 1.31 | 0.97 | 1.77 |
| 35–54 | 0.65 | 0.49 | 0.86 | 0.78 | 0.56 | 1.08 |
| 55+ | 0.58 | 0.39 | 0.87 | 0.48 | 0.29 | 0.80 |
| Serious family conflicts* | 1.39 | 1.19 | 1.62 | 1.32 | 1.13 | 1.54 |
| Currently lives with their children | 1.30 | 1.10 | 1.53 | - | ||
| Lives with anyone who used non- prescription drugs | 1.49 | 1.19 | 1.86 | 1.29 | 1.02 | 1.62 |
| US Census region (ref=West) | ||||||
| Northeast | 1.19 | 0.89 | 1.58 | 1.42 | 0.99 | 2.03 |
| South | 2.03 | 1.72 | 2.39 | 2.09 | 1.75 | 2.50 |
| Midwest | 1.25 | 1.00 | 1.57 | 1.75 | 1.37 | 2.24 |
| History of incarceration | 0.78 | 0.68 | 0.91 | 0.69 | 0.59 | 0.81 |
|
| ||||||
| Alcohol to intoxication >3 times/wk* | - | 1.41 | 1.12 | 1.79 | ||
| Heroin* | 2.23 | 1.79 | 2.78 | 1.50 | 1.15 | 1.97 |
| Methadone* | 2.97 | 2.42 | 3.65 | 2.74 | 2.18 | 3.45 |
| Benzodiazepine* | 2.44 | 2.09 | 2.86 | 2.23 | 1.90 | 2.61 |
| Cocaine* | 1.32 | 1.12 | 1.55 | 1.59 | 1.34 | 1.89 |
| Amphetamine* | 1.66 | 1.31 | 2.09 | 1.44 | 1.15 | 1.81 |
| Marijuana* | 1.48 | 1.28 | 1.72 | 1.29 | 1.09 | 1.51 |
| Barbiturate* | 5.65 | 3.68 | 8.67 | 2.16 | 1.46 | 3.20 |
| Inhalant* | - | 3.52 | 1.48 | 8.37 | ||
| Hallucinogen* | 2.17 | 1.38 | 3.42 | - | ||
| Used >1 substance* | 2.80 | 2.40 | 3.26 | 2.60 | 2.20 | 3.08 |
| Duration of illegal drug use (ref=0 yrs) | ||||||
| <1 to 3 years | 2.44 | 1.77 | 3.35 | 3.28 | 2.36 | 4.56 |
| >3 to 10 years | 3.75 | 2.73 | 5.14 | 3.94 | 2.81 | 5.53 |
| >10 years | 2.55 | 1.82 | 3.57 | 4.27 | 2.98 | 6.12 |
| History of overdose | 1.13 | 0.97 | 1.32 | 1.20 | 1.02 | 1.41 |
|
| ||||||
| Emotional abuse history | 0.86 | 0.74 | 0.99 | 0.71 | 0.58 | 0.86 |
| Sexual abuse history | - | 1.03 | 0.88 | 1.20 | ||
| Has a pain problem* | 1.00 | 0.82 | 1.22 | 0.63 | 0.50 | 0.78 |
| Taken prescribed medication for pain* | 5.93 | 4.90 | 7.19 | 6.16 | 5.00 | 7.60 |
| Medical problems* | 1.18 | 0.98 | 1.41 | 1.26 | 1.05 | 1.51 |
| Anxiety* | 0.98 | 0.83 | 1.16 | 1.21 | 1.00 | 1.47 |
| Depression* | 1.29 | 1.09 | 1.53 | 1.15 | 0.96 | 1.38 |
| Psychiatric medications* | 0.74 | 0.62 | 0.87 | 0.76 | 0.65 | 0.89 |
| Emergency room visits (ref=0)* | ||||||
| 1 to 5 | 1.46 | 1.25 | 1.70 | 1.25 | 1.07 | 1.46 |
| >5 | 1.06 | 0.56 | 2.03 | 1.75 | 0.97 | 3.14 |
= in past 30 days, self-reported
Other variables adjusted for in both models include number of dependents, usual/last occupation, educational status, duration of alcohol use (women), and past month hallucinations, violent behavior, suicidal thoughts, and suicide attempts.
A dash (-) indicates that the variable was not included in the model. It did not reach statistical significance and did not improve model fit.
3.6 Women
Adjusting for other important covariates and in addition to the shared risk factors noted above, for women, recent prescription opioid abuse versus abuse of some drug other than a prescription opioid was associated with younger age (<54 years); residence in US Census regions outside of the West; frequent problem drinking; any inhalant use; and a history of drug overdose. We found evidence of increasing odds of recent prescription opioid abuse with increasing duration of illegal drug use, even after controlling for age. Exploratory analysis of the age-duration relationship revealed a preponderance of young female initiators (i.e., under 21 or 21–34 with duration of use 3–10 years) and middle aged female long-term users (i.e., 35–54 with duration of use >10 years) who reported recent prescription opioid abuse (data not shown). Despite the marginally significant association between prescription opioid abuse and reported anxiety in the past 30 days, women who abused prescription opioids were less likely to take psychiatric medication compared to women who abused other drugs. The strongest risk factor for abuse of prescription opioids was taking prescribed medication for pain; however, women who abused prescription opioids were less likely to report having a pain problem than women who abused other drugs, but they were more likely to report having a medical problem.
Among women, reporting having a pain problem was associated with being prescribed pain medication although this was independent of individuals reporting a medical problem (Cochran-Mantel-Haenzel AOR 145.79, p<0.001, Breslow-Day χ2 = .60, p=0.44). Among men, stratifying by presence of a medical problem deflated the relationship between a self-reported pain problem and being prescribed pain medication (Breslow-Day χ2 = 4.15, p=0.04, AOR 83.12 no medical problem vs. 159.78 medical problem, both p<0.001). This discrepancy might suggest that men with a pain problem are more likely to be prescribed pain medications if they have a medical problem but women with a pain problem are more likely to be prescribed pain medications regardless of whether or not they have a medical problem.
Last, while not part of the regression analyses, we also found that pregnancy was not associated with recent prescription opioid abuse (5.9% prescription opioid abuse vs. 5.6% no prescription opioid abuse, χ2=0.20, NS).
3.7 Men
For men, recent prescription opioid abuse versus abuse of other drugs was associated with age < 34 years, currently living with their children, residence in the South and Midwest, more heroin, barbiturate and hallucinogen use, and recent depression (Table 3). The relationship between duration of illicit drug use and recent prescription opioid abuse peaked among men with more than 3 to 10 years of drug use experience. Given that men <34 years were the predominant abusers of prescription opioids, there appears to be a young onset of abuse in this population. Unlike the women, men who abused prescription opioids did not report experiencing proportionally more pain or medical problems compared to those who abused other drugs; however, as observed among the women, having taken prescribed pain medications in the past 30 days remained the strongest predictor of prescription opioid abuse.
4. Discussion
This exploratory study was intended to help clarify characteristics of women and men who abuse prescription opioids in a treatment-seeking sample and to identify gender-specific correlates of abuse. Our findings support the general observation of gender differences in patterns and correlates of prescription opioid abuse at new and more specific levels of inquiry. We found that women were 1.59 times more likely than men to report use of any prescription opioid in the past month and 1.50 times more likely to report recent abuse of prescription opioids. Product-specific differences suggest more prevalent abuse of immediate release opioid analgesic formulations among women while men were more likely to abuse extended release formulations.
This is the first study of which we are aware that attempted to incorporate geographic trends into the characterization of gender differences in prescription opioid abuse. Areas of Appalachia have long been associated with prescription opioid abuse (Kelly et al., 2008); we found higher prevalence of prescription opioid abuse among men in the South U.S. Census region. However, for women, an association of prescription opioid abuse extended beyond states located in the South Central region of the U.S. to include higher rates in the Midwest and a trend toward higher rates in the Northeast, compared to the West. Lack of a significant regional concentration suggests that the problem of prescription opioid abuse among women may be widespread. One starting point for helping to understand and explore gender differences in the spatial variation of prescription opioid abuse may be found in the methods and research evolving from the field of feminist geography (Dias and Blecha, 2007; Oberhauser and Pope, 2004; Pope, 2001), which looks at geographic differences in gender relations and gender equality. This approach challenges the biomedical and public health model to think about who abuses prescription opioids where, rather than just who abuses prescription opioids.
We found that lifetime history of overdose was associated with abuse of prescription opioids among women but not men. The association was a relatively modest one (AOR 1.20, 95% CI 1.02, 1.41). However, considered alongside the stronger associations also detected between prescription opioid abuse and concomitant use of alcohol, sedatives, and barbiturates- all known risk factors for opioid overdose (Shah et al., 2007; Warner-Smith et al., 2001)- it appears that preventive interventions for opioid overdose may be warranted. While fatal unintentional heroin overdose is more common among men, recent trends reported by Shah et al. indicate high rates of unintentional fatal overdose involving prescription opioids among women are worrisome (Shah et al., 2007). In light of the observation that, compared to men, women in our study were more likely to be prescribed medication for their pain and to report abusing some of their own prescriptions, proactive measures to protect against opioid overdose, including naloxone prescription and physician education, should be considered as risk management interventions and as good public health policy (Dasgupta et al., 2007).
In this study, women who abused prescription opioids were less likely to report experiencing a pain problem, whereas men exhibited no such association. Interestingly, abuse of prescription opioids was strongly associated for both genders with having recently taken prescribed opioids for pain. While it is not entirely clear what accounts for this apparently anomalous finding, it is possible that the women who abused prescription opioids in our sample were more likely to seek care for their pain problems, and to receive medication, as has been reported elsewhere (Simoni-Wastila, 1998). Men may not seek care for their pain, may be less likely to obtain medication or may be under-medicated for their pain, leading them to abuse prescription opioids as a means of self-medication. The more prominent role of medical problems for women than men may also be due to the constellation of poorly-defined painful medical conditions from which women suffer disproportionately (e.g., fibromyalgia, restless leg syndrome, irritable bowel syndrome, pre-menstrual syndrome) and for which women with histories of trauma or psychiatric problems, such as those in our sample, may experience more severely (Crofford, 2007). Another possible contributing factor to the gender discrepancy in prescription opioid abuse and current pain problem could be gender differences in psychiatric problems. Psychiatric problems, which have persistently stigmatized connotations, may be being medicated by prescription opioids rather than by psychiatric medications, opening another opportunity for abuse. It is well established that pain interpretation is influenced by psychological factors as well as by physical ones (Chapman and Gavrin, 1999) and that women and men experience pain differently. Women and men may also require different care. For example, individuals in this population with known substance problems may not be getting high enough doses of prescribed opioids or sufficiently nuanced psychiatric care due to concerns about their abuse or dependence problems. Further exploration of how pain problems versus other types of medical problems are perceived and experienced by men and women in this population as well as how these individuals seek and obtain medical treatment may disentangle these relationships.
Both similarities and differences were observed between the current study and the few other studies exploring gender differences in abuse of prescription opioids in a national sample (Cicero et al., 2008; Simoni-Wastila et al., 2004; Tetrault et al., 2008). Similar to others, we found that abuse of prescription opioids among men and women was associated with being under 35 (Cicero et al., 2008; Simoni-Wastila et al., 2004; Tetrault et al., 2008), visiting the emergency room 1 to 5 times in the past month (Tetrault et al., 2008), and use of marijuana, cocaine, stimulants, and/or sedatives (Cicero et al., 2008; Tetrault et al., 2008), with stark gender differences in source of drug and in health status (Cicero et al., 2008). In contrast, we found that inhalant use was associated with prescription opioid abuse among women in the current study, while Tetrault and colleagues reported a similar association but among men (Tetrault et al., 2008). They also found an association with severe mental illness for women only while our findings suggest that the connection between psychopathology and prescription opioid abuse may be a universal one, with gender differences exhibited by type of recent mental problem experienced (anxiety among women, depression among men). Cicero and colleagues (Cicero et al., 2008) also found that women who abuse prescription opioids had more self-reported psychopathology than men, in particular anxiety, and poorer mental health scores, although their sample was restricted to people diagnosed with prescription opioid abuse/dependence recruited from private, for-pay treatment centers only. The few discrepancies between our findings and those reported in the literature may be due to any number of factors, including the time frame used for obtaining covariates (lifetime, past month) or outcome (past year vs. past month), specificity of covariates, differences in the underlying sampling frame, or other variables. Taken together, there is growing evidence of differential and gendered pathways leading to prescription opioid abuse which should be explored in prospective epidemiological studies.
We are aware of no other large, treatment sample-based study contrasting gender and abuse of prescription opioids with source and route of administration of the drug, co-morbid chronic pain conditions, and use of one’s own prescribed pain medications at the brand- and class-specific levels. Pharmaceutical- and class-specific gender differences in abuse of prescription opioids may be explained by, among other reasons, the indications for their use which makes them more readily available, marketing of the drug, users’ expectations, drug accessibility, and extent and routes of diversion. Differences in rates of abuse of particular brands and classes of prescription opioids and in sources that make these drugs available suggest a need for gender-specific approaches to screening, prevention and treatment of prescription opioid abuse and dependence.
Limitations to our study should be noted. Our assessment tool did not assess important risk factors and potential confounders such as smoking status. In this way, residual confounding of the detected associations may have occurred. The design is cross-sectional and association and correlation not causation can be concluded from our findings. While we found association between chronic pain and prescription opioid abuse, for example, a prospective cohort design would best address questions of temporality. A limitation to this study is the inability to provide medical and psychiatric clinical diagnoses. While the ASI and ASI-MV® questions have been validated (Butler et al., 2001; McLellan et al., 1992) the purpose of the measure is to assess problem severity level, not to derive clinical diagnoses. Because the ASI-MV® Connect is used as a clinical intake measure and a surveillance mechanism, inclusion of additional diagnostic instruments was not feasible. Future studies should more explicitly inquire about the medical problems and chronic pain conditions experienced by this population. It is possible that this study sample over-represents prescription opioid abusers, as the initial aim of NAVIPPRO™ was to create a surveillance system of prescription drug abuse. Caution in interpreting the prevalence rates of prescription opioid abuse should be taken. The treatment centers contributing data to the ASI-MV® Connect represent a complete census in some instances (e.g., state of New Mexico) and a non-random sample in other places. The 3-digit ZIP codes of patients seeking treatment at the centers reflect reasonable geographic coverage (Butler et al., 2008) beyond the treatment site but do not necessarily provide evidence of a representative sample on par with a systematic national survey. Nonetheless, analysis of the relative patterns of prescription opioid abuse and the regression analyses conducted on the sample are well-powered and appropriate for exploring underlying gender differences. At the same time, it is acknowledged that a large number of associations were examined, inflating the possibility of a Type I error. Furthermore, the large number of cases resulted in some differences between men and women being statistically significant; however, the extent to which these differences are clinically significant remains an empirical question. Results of the present research should be considered as hypothesis-generating and in some cases supportive of previous findings, rather than conclusive.
Other limitations include this study’s reliance on treatment admissions data. These data are a convenient and widely-available source of information on drug abuse trends, nevertheless, such data may not be generalizable to the overall population. Entry into treatment may be influenced by a host of factors, including mandates from criminal justice proceedings, variations in insurance and reimbursement, and availability of effective treatment paradigms, perceptions of risk of continued drug use and the perceived benefits of treatment. Therefore, treatment program attendees may be a selected subset of the drug abusing population. The extent to which fluctuations in specific drugs abused by those admitted to treatment programs may relate to population-based data is unknown. Regardless, people entering treatment reflect those suffering from the greatest adverse consequences of drug use; thus, studies on this population are a key aspect of drug abuse epidemiology pertaining to prescription opioid abuse. Finally, these data reflect information on people who have survived long enough to continue to use and abuse prescription opioids; death from accidental prescription opioid overdose is of increasing concern, and its epidemiology deserves further study.
In conclusion, women and men appear to differ in factors associated with recent prescription opioid abuse, both among prescription opioid abusers and when compared to abusers of other drugs of the same gender. Our findings imply that a ‘one-size fits all’ model of preventing and treating prescription opioid abuse may fail to address key issues specific to the sizeable population of women abusing prescription opioids. Instead, a gender-specific approach to improve surveillance, identification, prevention, and treatment of prescription opioid abuse in the United States is warranted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 2005. National report (2004 data) to the EMCDDA Reitox National Focal Point
- Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA. Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical and substance use correlates. Drug Alcohol Depend. 2008;94:38–47. doi: 10.1016/j.drugalcdep.2007.09.018. [DOI] [PubMed] [Google Scholar]
- Brands B, Blake J, Sproule B, Gourlay D, Busto U. Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug Alcohol Depend. 2004;73:199–207. doi: 10.1016/j.drugalcdep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Goldman RJ, Newman FL, Beckley KE, Trottier D, Cacciola JS. Initial validation of a computer-administered Addiction Severity Index: the ASI-MV. Psychol Addict Behav. 2001;15:4–12. doi: 10.1037/0893-164x.15.1.4. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Licari A, Cassidy TA, Lioy K, Dickinson J, Brownstein JS, Benneyan JC, Green TC, Katz N. National Addictions Vigilance Intervention and Prevention Program (NAVIPPRO™): A real-time, product-specific, public health surveillance system for monitoring prescription drug abuse. Pharmacoepidemiology and Drug Safety. 2008;17:1142–1154. doi: 10.1002/pds.1659. [DOI] [PubMed] [Google Scholar]
- Chapman CR, Gavrin J. Suffering: the contributions of persistent pain. Lancet. 1999;353:2233–2237. doi: 10.1016/S0140-6736(99)01308-2. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Inciardi JA, Munoz A. Trends in abuse of Oxycontin and other opioid analgesics in the United States: 2002–2004. J Pain. 2005;6:662–672. doi: 10.1016/j.jpain.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Lynskey M, Todorov A, Inciardi JA, Surratt HL. Co-morbid pain and psychopathology in males and females admitted to treatment for opioid analgesic abuse. Pain. 2008;139:127–135. doi: 10.1016/j.pain.2008.03.021. [DOI] [PubMed] [Google Scholar]
- Crofford LJ. Violence, Stress, and Somatic Syndromes. Trauma, Violence, & Abuse. 2007;8:299–313. doi: 10.1177/1524838007303196. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Brason FWSA., II Project Lazarus: Overdose Prevention and Responsible Pain Management. Policy brief to North Carolina StateMedical Board 2007 [Google Scholar]
- Dasgupta N, Kramer ED, Zalman MA, Carino S, Jr, Smith MY, Haddox JD, Wright Ct. Association between non-medical and prescriptive usage of opioids. Drug Alcohol Depend. 2006;82:135–142. doi: 10.1016/j.drugalcdep.2005.08.019. [DOI] [PubMed] [Google Scholar]
- DHHS. [Accessed on March 25, 2009];Identification of Drug and Biological Products Deemed to Have Risk Evaluation and Mitigation Strategies for Purposes of the Food and Drug Administration Amendments Act of 2007. 2008 http://www.fda.gov/CBER/genadmin/rems.htm.
- Dias K, Blecha J. Feminism and Social Theory in Geography: An Introduction. The Professional Geographer. 2007;59:1–9. [Google Scholar]
- Galaif ER, Stein JA, Newcomb MD, Bernstein DP. Gender differences in the prediction of problem alcohol use in adulthood: exploring the influence of family factors and childhood maltreatment. J Stud Alcohol. 2001;62:486–493. doi: 10.15288/jsa.2001.62.486. [DOI] [PubMed] [Google Scholar]
- Gentilello LM, Rivara FP, Donovan DM, Villaveces A, Daranciang E, Dunn CW, Ries RR. Alcohol problems in women admitted to a level I trauma center: a gender-based comparison. Journal of Trauma. 2000;48:108–114. doi: 10.1097/00005373-200001000-00018. [DOI] [PubMed] [Google Scholar]
- Gilson AM, Ryan KM, Joranson DE, Dahl JL. A Reassessment of Trends in the Medical Use and Abuse of Opioid Analgesics and Implications for Diversion Control: 1997–2002. J Pain Symptom Manage. 2004;28:176–188. doi: 10.1016/j.jpainsymman.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Goodman FD, Glassman P. Evaluating potentially aberrant outpatient prescriptions for extended-release oxycodone. Am J Health Syst Pharm. 2005;62:2604–2608. doi: 10.2146/ajhp040618. [DOI] [PubMed] [Google Scholar]
- Grau LE, Dasgupta N, Harvey AP, Irwin K, Givens A, Kinzly ML, Heimer R. Illicit use of opioids: is OxyContin a “gateway drug”? Am J Addict. 2007;16:166–173. doi: 10.1080/10550490701375293. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. Journal of the American Medical Association. 2008;200:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Hendricks VM, Kaplan CD, VanLimbeek J, Geerlings P. The Addiction Severity Index: Reliability and validity in a Dutch addict population. Journal of Substance Abuse Treatment. 1989;6:133–141. doi: 10.1016/0740-5472(89)90041-x. [DOI] [PubMed] [Google Scholar]
- Isacson D, Bingefors K. Epidemiology of analgesic use: a gender perspective. Eur J Anaesthesiol Suppl. 2002;26:5–15. doi: 10.1097/00003643-200219261-00003. [DOI] [PubMed] [Google Scholar]
- Kelly JP, Cook SF, Kaufman DW, Anderson T, Rosenberg L, Mitchell AA. Prevalence and characteristics of opioid use in the US adult population. Pain. 2008;138:507–513. doi: 10.1016/j.pain.2008.01.027. [DOI] [PubMed] [Google Scholar]
- Lin SK, Ball D, Hsiao CC, Chiang YL, Ree SC, Chen CK. Psychiatric comorbidity and gender differences of persons incarcerated for methamphetamine abuse in Taiwan. Psychiatry Clin Neurosci. 2004;58:206–212. doi: 10.1111/j.1440-1819.2003.01218.x. [DOI] [PubMed] [Google Scholar]
- Lloyd B. Gender and prescription drug use: How does gender influence use and risk?. Proceedings of the 19th Annual International Harm Reduction Association.2008. [Google Scholar]
- Lynch WJ, Roth ME, Carroll ME. Biological basis of sex differences in drug abuse: preclinical and clinical studies. Psychopharmacology (Berl) 2002;164:121–137. doi: 10.1007/s00213-002-1183-2. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Milani RM, Parrott AC, Turner JJ, Fox HC. Gender differences in self-reported anxiety, depression, and somatization among ecstasy/MDMA polydrug users, alcohol/tobacco users, and nondrug users. Addict Behav. 2004;29:965–971. doi: 10.1016/j.addbeh.2004.02.044. [DOI] [PubMed] [Google Scholar]
- Nicholson AB. Methadone for cancer pain. Cochrane Database Syst Rev. 2007:CD003971. doi: 10.1002/14651858.CD003971.pub3. [DOI] [PubMed] [Google Scholar]
- Oberhauser A, Pope C. Crossing Borders and Building Bridges: Feminist Geography in the 1990s. In: Gaile G, Willmott C, editors. Geography in America at the Dawn of the 21st Center. AAG; Washington, D.C: 2004. pp. 736–758. [Google Scholar]
- Office of Applied Statistics, S.A.M.H.S.A. [accessed on September 10 2008];The DASIS Report. How Men and Women Enter Substance Abuse Treatment. 2001 http://www.oas.samhsa.gov/2k1/enterTX/enterTX.htm.
- Office of Applied Statistics, S.A.M.H.S.A. [ accessed on September 10 2008>];The DASIS Report. A Comparison of Female and Male Treatment Admissions: 2002. 2005 http://www.oas.samhsa.gov/2k5/genderTX/genderTX.htm.
- Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Pope C. Babies and Borderlands: Factors Influencing Sonoran Women’s Decision to Seek Prenatal Care in Southern Arizona. In: McLafferty SL, ID, Lewis N, editors. Geographis of Women’s Health. Routledge; London: 2001. pp. 143–158. [Google Scholar]
- Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. J Gen Intern Med. 2002;17:173–179. doi: 10.1046/j.1525-1497.2002.10435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. National Prevalence Data with Correlates of Substance Abuse: SAMHSA’s National Survery on Drug Use & Health. Office of Applied Studies (OAS); Department of Health and Human Services (DHHS); 2006. [Google Scholar]
- Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2007;103:126–136. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L. Gender and psychotropic drug use. Med Care. 1998;36:88–94. doi: 10.1097/00005650-199801000-00010. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, Ritter G, Strickler G. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Subst Use Misuse. 2004;39:1–23. doi: 10.1081/ja-120027764. [DOI] [PubMed] [Google Scholar]
- Tetrault JM, Desai RA, Becker WC, Fiellin DA, Concato J, Sullivan LE. Gender and non-medical use of prescription opioids: results from a national US survey. Addiction. 2008;103:258–268. doi: 10.1111/j.1360-0443.2007.02056.x. [DOI] [PubMed] [Google Scholar]
- Volkow ND. Subcommittee on Crime and Drugs. US Senate; 2008. Scientific Research on Prescription Drug Abuse Judiciary Committee. [Google Scholar]
- Warner-Smith M, Darke S, Lynskey M, Hall W. Heroin overdose: causes and consequences. Addiction. 2001;96:1113–1125. doi: 10.1046/j.1360-0443.2001.96811135.x. [DOI] [PubMed] [Google Scholar]
- Wisniewski AM, Purdy CH, Blondell RD. The epidemiologic association between opioid prescribing, non-medical use, and emergency department visits. J Addict Dis. 2008;27:1–11. doi: 10.1300/J069v27n01_01. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug Alcohol Depend. 2003;69:215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]