Abstract
Background
3′-[F-18]Fluoro-3′-deoxythymidine (FLT) traces thymidine phosphorylation catalyzed by thymidine kinase during cell proliferation. Knowing the rate of cell proliferation during cancer treatment, such as radiation therapy, would be valuable in assessing whether tumor recurrence is likely and might indicate the need for additional treatments. However, the relationship between FLT kinetics and the effects of radiation is not well-understood. Nor has the method for optimal quantification of FLT uptake within the irradiated tumor microenvironment been extensively examined.
Materials and Methods
We performed dynamic FLT-positron emission tomography (PET) studies (60 min) on 22 mice implanted subcutaneously with syngeneic mammary MCaK tumors bilaterally in the shoulder area. A day before the FLT-PET imaging, the tumor on the right side was irradiated with a single dose (0, 2.5, 5, 10, or 20 Gy) or with fractionated exposures (4×2.5 Gy given in 12 h intervals). Standardized uptake value (SUVs) of FLT on tumors at 10 and 60 min post injection were calculated; model fitting was used to estimate the kinetic parameters. Significant radiation-induced changes were shown by comparing the irradiated tumor with the control tumor in the same animal and by comparing it to nonirradiated mice. The effect of radiation on MCaK cell cycle parameters and FLT uptake was also examined in vitro.
Results
In vivo FLT kinetics were sensitive to radiation doses of 5 Gy and higher (administered 1 day earlier), as judged by SUV semiquantitative measures and by modeling. Single irradiation with 10 Gy had greater impact on SUVs and kinetic parameters than fractionated exposures. Overall, the uptake constant Ki appeared to be the best marker for these radiation effects. FLT uptake by irradiated cells in vitro at various doses gave similar findings, and the in vitro FLT uptake correlated well with Ki. Radiation-induced G2/M arrest appeared to influence FLT uptake, and this was more pronounced after single than fractionated doses.
Conclusion
The kinetics of FLT uptake into murine mammary tumors was altered 1 day after radiation treatment. The dose-dependent response correlated well with in vitro FLT cellular uptake. Parameters (e.g., Ki) derived from FLT kinetics are expected to be useful for assessing the efficacy of irradiation treatment of tumors.
Keywords: 3′-Deoxy-3′-18F fluorothymidine (FLT), Positron emission tomography, MCaK tumor, Kinetic modeling, Quantitation, Radiation treatment, Cell proliferation
Introduction
Glucose metabolic imaging using 2-deoxy-2-[F-18] fluoro-d-glucose (FDG) is currently the mainstay of clinical positron emission tomography (PET) imaging for tumors, but other PET tracers are undergoing preclinical or clinical evaluation for their ability to image cellular proliferation, amino acid, protein and membrane biosynthesis, tissue hypoxia, angiogenesis, and tumor receptor expression. One of the most frequently used PET imaging agents for cellular proliferation is the thymidine analog, 3′-[F-18]fluoro-3′-deoxythymidine (FLT), which is accumulated after its phosphorylation by cellular thymidine kinase-1 (TK1). TK1 is a key enzyme of the pyrimidine salvage pathway of DNA synthesis whose activity is three to four times higher in malignant than in benign cells [1, 2]. Since this enzyme is functional only during the S-phase of the cell cycle, uptake of FLT is tied to cell proliferation [3]. This has been substantiated by the finding of correlations of FLT uptake with both TK enzyme activity and cell proliferation, as measured by Ki-67 (MIB-1) and proliferating cell nuclear antigen (PCNA) expression [4-9].
Results from in vivo cancer models have suggested that FLT may be superior to FDG in monitoring tumor response to treatment with chemotherapy, antiproliferative agents, or kinase inhibitors [2, 10-13]. However, only a limited number of reports have addressed the use of FLT-PET for monitoring tumor response to radiotherapy (RT). Sugiyama et al. suggested that FLT may be superior to FDG because RT causes minimal changes in tumor glycolysis while inducing inflammation, which increases overall glucose utilization [14, 15]. Recently, Molthoff et al. [16] studied RT effects on mouse tumors using FDG and FLT tracers. Their results suggested that FLT could be a good indicator for radiation-induced changes in proliferation. A similar conclusion was reached in other comparative studies on irradiated tumor cells in vitro and in vivo [17].
Multifractionation regimens, commonly used in conventional RT, produce better tumor control for a given level of normal tissue toxicity than a single large dose. A value of being able to measure tumor cell proliferation during or soon after RT could lie in early assessment of accelerated tumor repopulation which can occur during RT, especially if treatment is prolonged. Recognition of this occurrence would allow for treatment adjustment in an attempt to gain better local control.
The use of FLT-PET to monitor early therapy-induced changes in tumor behavior could be problematic if only simple semiquantitative measurements, like standardized uptake value (SUV) [18-21], tumor to background ratio, or injected dose per gram of tumor (%ID/g) [21] taken from a single delayed static image are used. Full characterization of the kinetics of tracer uptake into tissue will be more sensitive and this requires kinetic analysis to model the tissue uptake/clearance of tracer. Also, the imaging parameters will be less variable and provide a better correlate to patient outcome when kinetics is taken into account than those not utilizing the kinetic information [22].
The aim of the current study is to investigate changes in the rate of cell proliferation in a murine tumor model after RT using FLT and microPET and to evaluate the sensitivity of kinetic analysis over semiquantitative measures for monitoring radiation responses. The FLT kinetic findings were supported by radiation studies on in vitro FLT uptake by tumor cells and cell cycle analysis.
Materials and Methods
FLT PET image acquisition was performed 1 day after irradiation to single doses of 0, 2.5, 5, 10 to 20 Gy or 4×2.5 Gy. Semiquantitative and quantitative methods were applied to analyze the acquired PET images. Image-derived in vivo results were also compared to in vitro FLT uptake study under compatible irradiation regimens.
Radiopharmaceuticals
For the synthesis of FLT, fluoride ion was produced by 11-MeV proton bombardment of 95% 18O-enriched water via 18O(p,n) 18F nuclear reaction. The aqueous [18F]-fluoride ion (∼18.5 GBq) solution was released from the cyclotron target into a reaction vessel and treated with potassium carbonate and Kryptofix 2.2.2 (Merck). Water was evaporated by azeotropic distillation with acetonitrile. The dried K18F/Kryptofix residue was subsequently reacted with 5′-O-[4,4′-dimethoxytrityl]-2,3′-anhydrothymidine and then hydrolyzed with dilute HCl. The radiochemical yield and purity were 6-12% (after decay correction) and >99%, respectively [23].
Animals and Tumor Models
Six- to 8-week-old C3H/Sed//Kam mice (n=22) were maintained in a strict defined-flora, pathogen-free environment in the AALAC-accredited Animal Facilities of the Department of Radiation Oncology, UCLA. All local and national guidelines for the care of the animals were adhered to. The syngeneic murine mammary carcinoma cell line MCaK [24] was cultured in Dulbecco’s modification of Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum and 1% antibiotics-antimycotic solution. MCaK cells were injected subcutaneously as single-cell suspensions in phosphate buffer saline (PBS; 5×105 to 106 cells in 100 μl) bilaterally in the dorsal shoulder region of the mice. When the diameters of the tumors were approximately 5 mm, the tumor on the right side was irradiated, while the tumor on the left side acted as the control.
Irradiation Protocols
Mice were anesthetized with i.p. injection of ketamine/xylazine and positioned in a Lucite jig with lead shielding the body except for the right tumor area. Radiation was delivered at a dose rate of approximately 67 cGy/min (137Cs source; Atomic Energy of Canada, Ottawa, Canada). For dose response studies, the right tumors were irradiated with 2.5, 5, 10, and 20 Gy (three, five, four, and four studies, respectively). For examination of the effect of dose fractionation, two daily fractions of 2.5 Gy were applied with a 12-h interval for 2 days (n=4) to give a total dose of 10 Gy. In a baseline study, two mice were scanned without prior irradiation (n=2).
In Vitro FLT Uptake and Cell Cycle Distribution of Tumor Cells after Irradiation
For in vitro FLT uptake experiments, cells were incubated with 0.07 MBq/ml of FLT at 37°C for 1 h, washed three times with DMEM, and radioactivity taken up in the cells was measured with a calibrated well counter. To test the effect of irradiation, the same doses as in in vivo experiments (see above) were applied 1 day before FLT incubation. For the fractionated experiment, the incubation FLT concentration was at 0.028 MBq/ml. All experiments were done in triplicates (i.e., n=3).
For cell cycle analysis, 106 cells were trypsinized and collected by centrifugation at 2,000 rpm for 5 min. The cells were then fixed with ice-cold ethanol at -20°C overnight, washed three times with PBS, resuspended in isoton, treated with RNase A (0.5 mg/ml) for 15 min, and stained with propidium iodide (0.05 mg/ml) for 30 min at room temperature. Fluorescence was measured in a FACSCalibur flow cytometer (Becton Dickson, Mountain View, CA, USA) and cell cycle data were analyzed by ModFit version 3.1 (Verity Software House, Topsham, ME, USA).
MicroPET Imaging
MicroPET scans were performed 1 day after completion of the irradiation, using a microPET® Focus™ 220 tomograph (Siemens Preclinical Solutions, Knoxville, TN, USA). This scanner has a 7.6 cm axial field of view (FOV). Mice were maintained under anesthesia with 2% isoflurane and placed on a heating imaging chamber at 35°C during scanning. A 60-min dynamic scan was performed beginning at the time of tracer injection (8.14±0.74 MBq bolus via tail vein). For image reconstruction, list-mode data were first sorted into three-dimensional (3D) sinograms, followed by Fourier rebinning and two-dimensional (2D) filtered backprojection reconstruction using a ramp filter with a cutoff at the Nyquist frequency. The list-mode data were reframed according to the sequence: 8×15, 3×60, 5×300, 3×600 s. The spatial resolution of the reconstructed images is ∼1.75 mm at full-width at half-maximum.
Data Analysis
Kinetic Modeling
Images were analyzed with the AMIDE 0.8.8 software [25]. The 3D isocontour regions of interest (ROIs) were manually defined for bilateral tumors in each mouse on 60 min images with the same thresholds applied to both tumors. An elliptical ROI (2.0×1.5×1.5 mm) was drawn on the left ventricle (LV) region at the first time frame (1-15 s) and projected to all dynamic images to provide the LV time activity curve (TAC) which was used as the input function for modeling analysis. The tumor ROIs were also copied to the entire dynamic image sequence in order to obtain TACs that represented the kinetics of FLT in tumor tissues. A two-tissue compartment model (Fig. 1) was used to describe the kinetics of FLT in tumor tissue [11, 26]. The individual rate constants of the model represent the forward transport of FLT from plasma to tissue (K1), the reverse transport (k2), the phosphorylation (k3), and dephosphorylation (k4) steps. The values of the rate constants were estimated using the kinetic imaging system (KIS) [27], which is an Internet-based kinetics simulation and model fitting program. All the parameter values were derived from fitting the tissue TAC data using the LV TAC as the input function. The FLT model configuration is similar to the FDG model [27, 28], adapted from the DG model used originally by Sokoloff et al. [29]. It is also consistent with the model proposed by Mankoff et al. [30] for thymidine analogs. The ratio K1/k2 representing the concentration ratio of FLT in tissue relative to that in plasma when the phosphorylation rate is small is referred to as the distribution volume of the tracer in tissue. The value of the FLT uptake constant, Ki, was calculated as:
Fig. 1.
Compartmental model used to describe the kinetics of FLT in tumor tissue. Cp blood concentration of FLT, Ce exchangeable FLT concentration in tissue, Cm phosphorated FLTs (mainly FLT-monophosphate) in tissue. 18F-metabolites in blood are negligible and do not enter tumor cells. The rate constants, K1, k2, k3, and k4, represent the forward transport of FLT from blood to tissue, the reverse transport, the phosphorylation, and dephosphorylation steps, respectively.
Semiquantitative Analyses
For semiquantitative analyses, ROIs for both tumors were generated for each study as described above. To avoid contribution from the background region and to minimize sensitivity to how the ROI was defined, only voxels with image values above 70% of the highest voxel value within the ROI were included for the calculation of the average ROI value [31]. Several semiquantitative measures were calculated.
- SUVs at 60 and 10 min for both irradiated and control tumor were calculated as:
- SUVirrad_60 = (ROI of irradiated tumor at 60 min)/injected FLT dose/body weight)
- SUVirrad_10 = (ROI of irradiated tumor at 10 min)/injected FLT dose/body weight)
- SUVcontl_60 = (ROI of control tumor at 60 min)/injected FLT dose/body weight)
- SUVcontl_10 = (ROI of control tumor at 10 min)/injected FLT dose/body weight).
- Normalizing the irradiated tumor activity at 10 and 60 min to the corresponding value of the control tumor:
- SUVR60 = SUVirrad_60/SUVcontl_60
- SUVR10 = SUVirrad_10/SUVcontl_10.
- Ipsilateral normalization using the 60-min ROI value divided by the value at 10 min:
- SUVNirrad = SUVirrad_60/SUVirrad_10
- SUVNcontl = SUVcontl_60/SUVcontl_10.
Statistical Analysis
Data for each measure/parameter were grouped according to the irradiation dose level and all were stated as mean±SD. For each dose group, the values of individual kinetic parameters and of semiquantitative measures (except the standard uptake value ratios [SUVRs]) of the irradiated tumor (right side) were compared with those of the control tumor (left side) in the same mouse using a paired t test. p<0.05 was considered statistically significant. For SUVRs, the values of each dose group were tested to see if they are different from 1.0. Values of all the parameters/measures of each dose group were also compared with those of the 0-dose group, using unpaired t test. In this set of comparisons, since tumors on both sides of the animal of the 0-dose group could be considered as control, the values on tumors of both sides were pooled together as a single group for statistical tests. Statistical analyses were performed using the statistical tools in Microsoft Excel 2000.
Results
Dose Response Changes
A typical FLT PET image is shown in Fig. 2a. Results of the kinetic and semiquantitative analyses are summarized below.
Fig. 2.
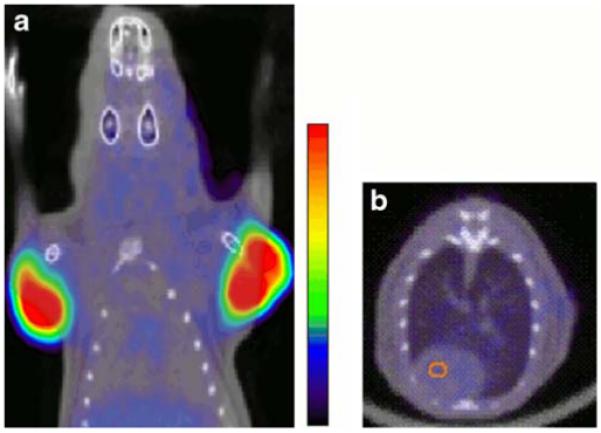
a Coronal section PET image of FLT in a mouse with implanted tumor at 60 min post tracer injection was fused with the CT image (in black and white) of the same section. The FLT PET image was displayed in color with the color scale shown on its right side. The animal had implanted tumors bilaterally in the shoulder region. The tumor on the right side (also the right side of the image) was irradiated (10 Gy) 24 h before PET imaging. b Transaxial section of FLT PET across the heart of a mouse at 60 min post FLT injection. The PET image is with the same color scale as in a and is fused with the CT image of the same section. The image shows the low uptake of FLT in the myocardium. The LV ROI that was defined based on early frame PET images and the fused CT image to obtain the LV TAC in this study is also shown on the image.
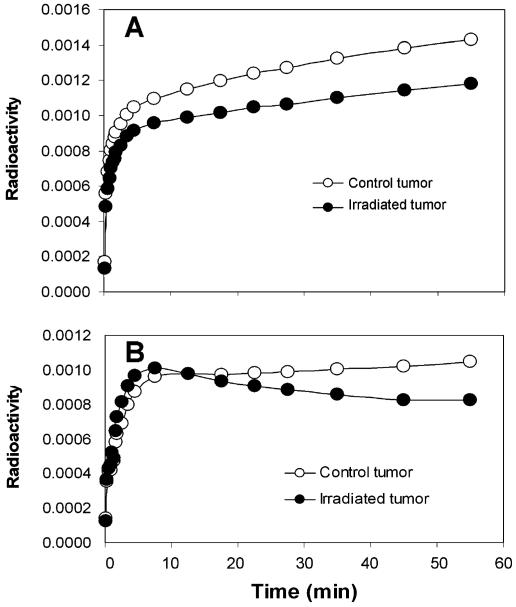
Kinetic Patterns of Tumor Time Activity Curves
Representative tumor FLT TACs 1 day after 2.5 and 20 Gy doses are shown in Fig. 3. After a bolus injection of FLT, tumor uptake in the control tumor or in tumors receiving 2.5 or 5 Gy radiation rose rapidly within the first 10 min and continued to rise, but more slowly thereafter (Fig. 3a). A distinctly different FLT kinetic pattern was observed for tumors irradiated with 10 Gy or higher. The pattern was characterized by a rapid, more marked increase within 10 min that was not sustained (Fig. 3b).
Fig. 3.
Representative tumor FLT TACs at 1 day after irradiation. a The two TACs are for a 2.5-Gy irradiated tumor and its corresponding control tumor from the same animal. The scaling difference between the two curves is due to the size difference between the irradiated and the control tumors. The similarity in shape of the two curves is representative of TACs with irradiation doses of less than or equal to 5 Gy. b The TAC of the irradiated tumor (20 Gy) was noticeably different from the one in the control tumor of the same animal. This is typical for cases with irradiation doses of 10 Gy or higher.
Semiquantitative Data Analysis
These distinct uptake patterns following irradiation are also seen in values of semiquantitative measures of FLT uptake that are summarized in Table 1. Most measures showed a gradual dose-dependent decrease after irradiation. However, not all reached statistical significance. SUVirrad_60, SUVirrad_10, and SUVNirrad had significantly lower values than those of the control side (paired t test, p<0.05) for 5 and 10 Gy doses. For the case of 20 Gy, none of the measures, except SUVR60, reached the significance level. The values of SUVR60 were significantly less than 1.0 for 5, 10, and 20 Gy doses. The value of SUVR10 was significantly less than 1.0 for 5 Gy dose.
Table 1.
Values of semiquantitative measures
| Irradiation dose in Gy | 0 (n=2) | 2.5 (n=3) | 5 (n=5) | 10 (n=4) | 20 (n=4) | 4×2.5 (n=4) | Correlation coefficient w/ in vitro FLT uptake (r) |
|---|---|---|---|---|---|---|---|
| SUVirrad_60 | 1.607±0.308 | 1.934±0.552 | 1.606±0.238* | 1.195±0.110*, ** | 0.900±0.263** | 1.852±0.495* | 0.76 |
| SUVirrad_10 | 1.362±0.129 | 1.563±0.041** | 1.472±0.127* | 1.440±0.092* | 1.012±0.339 | 1.371±0.268 | 0.65 |
| SUVcontl_60 | 1.692±0.428 | 2.689±1.391 | 2.444±0.199** | 1.987±0.391 | 1.185±0.380 | 2.721±0.893 | 0.51 |
| SUVcontl_10 | 1.351±0.112 | 1.662±0.221 | 1.676±0.132** | 1.646±0.144** | 1.001±0.346 | 1.574±0.034 | 0.53 |
| SUVR60 | 0.919±0.006 | 0.803±0.248 | 0.656±0.070*, ** | 0.621±0.140*, ** | 0.798±0.204* | 0.687±0.132*, ** | 0.16 |
| SUVR10 | 0.956±0.085 | 0.949±0.102 | 0.878±0.029*, ** | 0.882±0.119 | 1.032±0.155 | 0.888±0.104 | -0.03 |
| SUVNirrad | 1.170±0.121 | 1.232±0.323 | 1.098±0.187* | 0.832±0.082*, ** | 0.922±0.239 | 1.328±0.265 | 0.49 |
| SUVNcontl | 1.223±0.242 | 1.561±0.647 | 1.467±0.177 | 1.199±0.152 | 1.210±0.215 | 1.724±0.300 | 0.38 |
p<0.05, paired t test; values are significantly different between the irradiated and the control tumor or SUVRs were significantly different from 1.0
p<0.05, unpaired t test; values are significantly different from the corresponding ones at the 0-Gy dose
In the comparisons to the 0-dose radiation level, SUVR60 showed significant decrease at 10 and 20 Gy and SUVirrad_10 showed difference at 2.5 Gy. Somewhat surprisingly, SUVcontl_60 and SUVcontl_10 for 5 and/or 10 Gy doses were significantly increased from those of the 0-dose group. SUVNs of the irradiated tumor showed significant decreases only at the 10-Gy level. Excluding those for SUVcontl, all the significant differences in the comparison to the 0-dose group (except SUVirrad_60 at 20 Gy) were also revealed in the comparison between irradiated and control tumors within one animal. The differences judged significant by the paired comparison to the control tumor, but were missed by the comparison to the 0-Gy dose, were SUVirrad_60 and SUVNirrad at the 5-Gy dose level.
Quantitative Data Analysis
Values of the rate constants (K1, k2, k3, and k4) and Ki (FLT uptake constant) as estimated by model fitting to the tumor TACs in various dose groups are summarized in Table 2. Only values of k3, and Ki showed a clear gradual trend for dose-dependent changes, but not all values at all dose levels reached statistical significance. The rate constant k3, representing the rate limiting step of FLT phosphorylation, was lower in the irradiated than in the control tumor for 5 and 20 Gy doses. The equilibrium distribution volume of FLT (K1/k2) was not significantly different between the irradiated and the control sides, except at 20 Gy where it is higher on the irradiated side. Compared to the control side, significant decreases in Ki values for 5 and 20 Gy levels paralleled those of k3.
Table 2.
Values of rate constants obtained with kinetic analysis
| Irradiation dose in Gy | 0 (n=2) | 2.5 (n=3) | 5 (n=5) | 10 (n=4) | 20 (n=4) | 4×2.5 (n=4) | Correlation coefficient w/ in vitro FLT uptake (r) | |
|---|---|---|---|---|---|---|---|---|
| K1 | Irradiated | 0.083±0.005 | 0.247±0.054 | 0.296±0.147 | 0.217±0.055 | 0.067±0.014 | 0.244±0.068 | 0.41 |
| Control | 0.208±0.064 | 0.253±0.083 | 0.296±0.162 | 0.204±0.057 | 0.099±0.035 | 0.211±0.070 | 0.51 | |
| K2 | Irradiated | 0.130±0.010 | 0.342±0.126 | 0.468±0.275 | 0.296±0.101 | 0.085±0.02 | 0.426±0.236 | 0.40 |
| Control | 0.342±0.207 | 0.342±0.140 | 0.456±0.261 | 0.287±0.101 | 0.203±0.131 | 0.315±0.157 | 0.38 | |
| K3 | Irradiated | 0.136±0.017 | 0.042±0.011 | 0.047±0.012* | 0.019±0.009** | 0.009±0.005*, ** | 0.087±0.025 | 0.74 |
| Control | 0.054±0.001 | 0.059±0.018 | 0.067±0.015 | 0.035±0.017 | 0.055±0.037 | 0.109±0.070 | 0.18 | |
| K4 | Irradiated | 0.014±0.001 | 0.019±0.017 | 0.026±0.010 | 0.024±0.014 | 0.006±0.012 | 0.034±0.017 | 0.33 |
| Control | 0.054±0.073 | 0.019±0.016 | 0.021±0.014 | 0.016±0.008 | 0.024±0.013 | 0.030±0.024 | 0.17 | |
| Ki | Irradiated | 0.042±0.014 | 0.028±0.006 | 0.027±0.006* | 0.013±0.005** | 0.0065±0.003*, ** | 0.043±0.008 | 0.89 |
| Control | 0.030±0.008 | 0.038±0.007 | 0.037±0.008 | 0.022±0.008 | 0.021±0.008** | 0.052±0.026 | 0.61 | |
| K1/k2 | Irradiated | 0.641±0.05 | 0.77±0.16 | 0.65±0.08 | 0.76±0.11 | 0.846±0.09* | 0.632±0.170 | -0.53 |
| Control | 0.676±0.22 | 0.67±0.12 | 0.66±0.11 | 0.74±0.11 | 0.54±0.11 | 0.725±0.172 | 0.32 |
p<0.05, paired t test; values are significantly different between the irradiated and the control
p<0.05, unpaired t test; values are significantly different from the corresponding ones at the 0-Gy dose
In the unpaired comparison to control 0 Gy values, k3 and Ki of the irradiated tumor at both 10 and 20 Gy were significantly decreased. The Ki value of the control tumor at 20 Gy was also significantly decreased, suggesting some systemic effect.
Dose Fractionation
Kinetic TACs Patterns
The tumor TACs after exposure to fractionated doses did not have the characteristic pattern associated with TACs of a single dose of 10 Gy or higher, but was similar to those of lower single doses, indicating that the dose effect on the TAC pattern was not cumulative.
Semiquantitative Analysis
Semiquantitative analyses results are shown in Table 1. Among these measures, only SUVirrad_60 was found significantly different between the control tumor and the irradiated one (with fractionated regimen of 4×2.5 Gy). This was confirmed by the finding that the value of SUVR60 was significantly different from 1.0. However, this result is different from visual inspection of the kinetic TAC pattern (results of the “Kinetic TACs Patterns” section) and from the quantitative analysis below.
Quantitative Analysis
Results of the quantitative analyses are included in Table 2. Though the values of k3 and Ki tended to be lower in the irradiated tumor than in the control, none of the decreases was statistically significant. This is consistent with the findings of visual inspection of the kinetic TAC pattern that the 4×2.5 Gy doses in the fractionation regimen did not show a cumulative effect. The Ki value for tumors receiving dose fractionation was significantly higher than those in the 10-Gy single dose group (p<0.05), but was not significantly different from the single 2.5-Gy dose group, indicating that the fractionated dose gave irradiation effects equivalent to somewhere between 2.5 and 10 Gy single doses.
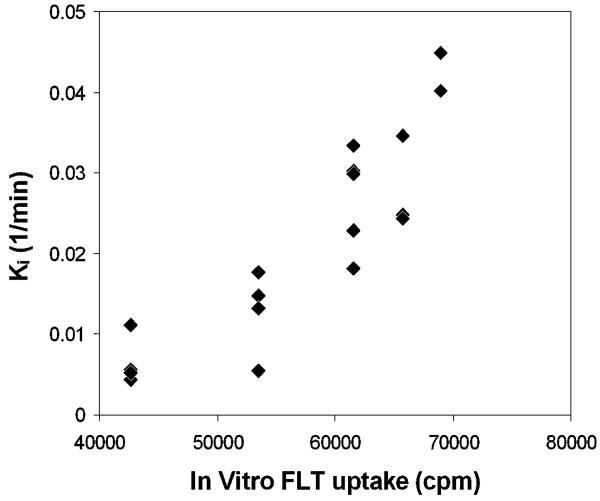
In Vitro FLT Uptake
In vitro studies were undertaken to determine if tracer uptake by tumor cells changes following irradiation that might explain in vivo imaging observations. The in vitro study results also served as a standard to evaluate the qualitative and quantitative measures derived from in vivo data.
Dose Response Changes
In vitro FLT uptake in MCaK cells after irradiation are shown in Table 3. Compared to the 0-Gy controls, FLT uptake was significantly decreased for cells 1 day after a single dose of 10 or 20 Gy. Correlations of in vitro FLT uptake with in vivo measures/parameters are shown in the last column of Tables 1 and 2 and in Fig. 4. The strongest correlation was with Ki values (r=0.86), followed by SUVirrad_60 (r=0.76), and k3 (r=0.74).
Table 3.
In vitro FLT uptake at various irradiation levels
| Irradiation dose (Gy) | 0 (n=3) | 2.5 (n=3) | 5 (n=3) | 10 (n=3) | 20 (n=3) |
|---|---|---|---|---|---|
| In vitro FLT_uptake | 68,945±3,385 | 65,737±1,516 | 61,556±3,794 | 53,493±1,669* | 42,674±2,686* |
p=0.05; value is significantly different from that of zero irradiation
Fig. 4.
Scatter diagram of the value of Ki (the uptake constant of FLT from in vivo PET imaging) versus in vitro FLT uptake (in cell line experiments) at various irradiation levels, showing a good correlation (r=0.89) between the in vivo kinetic parameter and the in vitro FLT uptake.
Dose Fractionation
The FLT uptake values in MCaK cells after 4×2.5 Gy fractionated doses of radiation delivered b.i. d. are in Table 4. Fractionated doses were again shown to be less effective in suppressing FLT uptake than a single comparable total dose. Compared to the nonirradiated (i.e., 0 Gy) control group, a single dose of 10 Gy decreased FLT uptake by 22% (p<0.05), which is consistent with the results shown in Table 3 (indicating good agreement between the two in vitro FLT uptake experiments performed at two different times and with different incubation FLT concentrations), while the 4×2.5 Gy regimen only decreased FLT uptake by 5% (the difference is insignificant, p>0.05). The lack of significant difference between the in vitro fractionated dose and zero dose is also consistent with the in vivo kinetic parameters results (Table 2) as well as with the kinetic TAC pattern of the in vivo experiments, but is somewhat different from the semiquantitative measures, SUVirrad_60 and SUVR60, in Table 1.
Table 4.
In vitro FLT uptake for fractionated irradiation
| Irradiation dose (Gy) | 0 (n=3) | 2.5 (n=3) | 10 (n=3) | 4×2.5 (n=3) |
|---|---|---|---|---|
| In vitro FLT_uptake | 27,428±2,257 | 26,295±606 | 21,558±2,208* | 26,244±1,549 |
p=0.05; value is significantly different from that of zero irradiation
Cell Cycle Phase Determination
Since the activity of thymidine kinase that is responsible for the phosphorylation of FLT is cell cycle-dependent during normal condition, the effects of irradiation on the cell cycle status of MCaK cells were studied using flow cytometry. The results of the fractions of cells in various cell cycle phases are shown in Table 5. A single dose of 10 Gy caused G2/M arrest (37.3% compared to 10.4% in controls). Dose fractionation (4×2.5 Gy) also increased the percentage of cells in G2/M, though to a lesser extent (28.1%). These increases were largely due to decreases in cells in the G1 phase with only a small drop in S-phase cells following single or fractionated doses of radiation (Table 5). The results indicated that the cell cycle was arrested in G2/M after irradiation more so with a single large dose than with fractionated doses (i.e., single 10 Gy is more than 4×2.5 Gy).
Table 5.
Percent cells in different cell cycles after irradiation
| Cell cycle phase | Control | Single dose (10 Gy) | Dose fractionation (4×2.5 Gy) |
|---|---|---|---|
| G2/M | 10.42 | 37.25 | 28.11 |
| G1 | 75.8 | 53.13 | 61.09 |
| S | 13.78 | 9.62 | 10.08 |
Discussion
PET, using FDG, is a routine functional imaging modality in oncology practice. In recent years, several additional tracers have been developed to image different aspects of tumor physiology, including cellular proliferation. After being transported across the cell membrane by a carrier-mediated mechanism [3], FLT undergoes monophosphorylation catalyzed by the cytosolic TK1 enzyme. It implies that TK1 activity ultimately governs FLT activity in tissue measured by PET and this presumption has been supported by in vitro experiments in A549 human lung carcinoma cells where FLT uptake by cells and TK1 activity were correlated [32]. Since TK1 activity is expressed in the S-phase and is thought to reflect the rate of cellular proliferation [33, 34], imaging this surrogate marker may provide a reasonable measure of tumor proliferation kinetics [8]. The fact that kinetic changes we measured in vivo following irradiation correlated well with FLT uptake in vitro demonstrates that parameters from PET measurement reflect biological activity in cells rather than simply tissue-related extracellular changes like perfusion. According to our cell cycle studies, G2/M arrest might be involved in decreasing FLT uptake after irradiation. This is consistent with previous findings on radiation-induced G2/M arrest [35]. Although the overall fraction of cells in the S-phase decreased less than as expected, one can still infer that the TK1 activity was suppressed when the cell cycle was arrested or with a prolonged cycling time post irradiation, thus leading to reduced uptake of FLT. We, therefore, believe that changes in the FLT kinetics in tumors provide insight into changes in cell cycle status.
Results of the present study show that tumor FLT kinetics is sensitive to radiation effects of 5 Gy or higher with some discrepancies between comparisons to different control groups, i.e., intramouse and intermouse. For each animal, the irradiated tumor and the control tumor were fed by the same plasma FLT concentration and over the same time course. Thus, variations in the plasma FLT TAC would not influence the intraanimal results. If the irradiated and the control tumors on an animal were of identical size, the partial volume effect (PVE) [36] due to small object size in imaging would also be minimized. However, in practice, it is difficult to have equal sizes for the irradiated and the control tumors, and the PVE could not be eliminated by the use of the control tumor. The pooling of both tumors of the animal in the 0-Gy group may have artificially increased the statistical power of the comparison to that group because the FLT uptakes in two tumors of an animal are not completely independent. However, using a single tumor of 0 Gy but adding the nonirradiated tumor of the animals with 2.5 Gy to form the control group (n=5) of 0 Gy did not change much the significance of the comparison to the control group. Only the values for SUVirrad_10 at 2.5 Gy, SUVcontl_60 at 5 Gy, and SUVcontl_10 at 5 and 10 Gy in Table 1 became insignificantly different from the nonirradiated group, and the values of K1 and k2 (in Table 2) of the irradiated tumor at 20 Gy became significantly different. However, the following discrepancies between the comparison to the control group (interanimal) and the intraanimal control tumor remain unchanged. Comparing against the control tumor in the same mouse, SUVirrad_60, k3, and Ki revealed irradiation effects at 5 Gy that were not indicated by comparison to the 0-Gy control mouse (different mouse). Use of the control tumor also revealed the increase in K1/k2 due to 20 Gy irradiation, while it failed to detect the effects of 20 Gy by SUVirrad_60 and Ki of the control as well as the effect at 10 Gy by the parameters k3 and Ki. One of the reasons for having missed these effects by intramouse comparison that were indicated by comparison to the 0-Gy control mouse may be systemic effects of irradiation, which can be experienced by tissue that are outside the radiation field, known as abscopal effects [37, 38]. It might also explain why the overall effectiveness of radiation was less obvious when compared to the control tumor on the contralateral side. Hence, the combined use of both types of comparison is more revealing than either one alone.
There are also differences between the use of the semiquantitative measures and the use of the modeling kinetic parameters which have been debated in the literature. Both have their advantages and limitations. We calculated the SUV values at 10 and 60 min because, based on the FLT tumor kinetics, the SUV values at those two time points well-characterized the magnitude and shape of the tissue kinetics. The value at 10 min is roughly related to the early uptake of FLT; the value at 60 min is related to the retained amount of FLT. SUVR is calculated to have a built-in comparison to a control tumor in the same animal and is useful only in the preclinical setting. By normalizing the value at 60 min by that at 10 min, SUVN is like an index of the slope of the kinetics between 10 and 60 min. It is less dependent on the magnitude and the PVE, but, like SUV, does not account for across-animal variations in the plasma FLT TAC.
Among the semiquantitative measures, SUVirrad_60 or SUVR60 were decreased above 5 Gy including in the fractionated regimen. In contrasts, the increases seen in SUVirrad_10 (or decrease in SUVR10) at 2.5-10 Gy (or 10 Gy) are harder to interpret. At the 5-Gy level, higher SUVirrad_10 values imply an irradiation-induced increase in early FLT uptake, yet the decrease in SUVR10 implies the opposite. Somewhat surprising is that SUVNirrad was less sensitive than SUVirrad_60 in showing irradiation effects at 20 Gy. This might be due to an increase in variability resulting from taking the ratio of two noisy measurements.
Compared to the semiquantitative measures, the kinetic parameters were more consistent. Based on the FLT model of Fig. 1, the decreases in k3 at the 5-, 10-, and 20-Gy levels reflect less FLT phosphorylation. Due to the small rate of dephosphorylation (k4), this decrease in k3 was propagated to the value of Ki. At 20 Gy, the decrease in the Ki value of the control tumor and the increase in K1/k2 of the irradiated tumor were consistent with abscopal effects. The high correlation of Ki with in vitro FLT uptake further indicated that the Ki value can be used to quantify radiation effects which has the added advantage that Ki can be estimated as the slope of the Patlak plot (a graphical method) [39] without going through the model fitting procedure. The results of this study showed that, for FLT studies between semiquantitative and kinetic modeling, Ki is probably the best measure in terms of ease and reliability to monitor tumor radiation responses in vivo. In this study, Ki demonstrated most accurately dose-dependent change in irradiated tumors.
PVE [36, 40] due to tumor size was not corrected in the present study. However, the tumor size was difficult to estimate from microPET images. Also, the tracer uptake in tumor could be quite heterogeneous, especially for largesized tumors with necrotic cores. The PVE probably accounted for a large share of the variability of the different measures obtained in this study. The measures affected directly by PVE include K1Ki, K1/k2, SUVs, and SUVRs. For SUVNs, if the relative distributions at 10 and 60 min were the same, the measures would not be affected by PVE, but this condition rarely occurred. The spillover of background activity to the tumor kinetics could also affect the estimates of k2, k3, and k4. However, due to the small background level of FLT uptake in normal tissue, the PVE on these parameters are relatively small.
There are other limitations in the current study, including the use of the TAC obtained directly from an ROI defined on the LV chamber region of the early image as the input function. It is technically challenging to take serial blood samples in mouse studies to give the input function. Some technical breakthroughs in mouse blood sampling [41] have emerged recently, but were not widely available when the present study was performed. The use of ROI on the LV chamber on dynamic microPET images to derive the input function has also been demonstrated [42, 43] and is the approach adopted in this study. However, the method has some limitations. Even though the myocardial uptake of FLT is low (see Fig. 2b), the kinetics in the myocardium is different than in the blood. This would give different spillovers from the myocardium at early times versus at later times and could potentially cause the shape of the LV ROI curve to deviate from the true blood curve, thus the input function. In a set of six studies, serial blood samples were taken from the tail artery and compared to the corresponding LV ROI curves. The area under the curves (AUC) were not found to be different (p>0.05) between the two sets of curves (after a PV correction of the LV ROI curves with a RC of 0.8). The difference between the plasma and whole blood concentrations of FLT was also reported before to be insignificant [11]. In this study, we did not correct for any labeled metabolites in the blood [11, 26] because FLT is metabolically stable in vivo. In mice, Barthel et al. demonstrated that parent FLT comprised 96% and 90% of the total radioactivity in plasma and liver samples, respectively [11]. Therefore, although the LV ROI curve was used to approximate the input function in the present study and the estimates of the rate constants in the modeling approach might contain some systematic bias, the effects on the evaluation of radiation response is expected to be relatively small (since all contained similar biases). However, future studies on these issues are warranted.
Ultimately, the all important question will be whether FLT can be used to monitor the impact of dose response and dose fractionation in the clinic. In this study, FLT was shown to be sensitive to radiation effects shortly after irradiation and without the “flare” response of FDG [15]. We further show that coupling the FLT data with the data from the flow cytometry indicate that radiation-induced changes in the Ki value indeed correlate with cell cycle redistribution, thus a change in cell proliferation rate.
For the formulation of individual therapeutic plans, measures of cellular proliferation, in addition to size, location, and extent of the tumor, could further guide therapy and evaluate treatment response early during the course of treatment, but this measure needs to perform with high sensitivity and reliability. Several research groups have investigated different aspects of FLT uptake in tumors and reported promising results. The majority of them have focused on the correlation of FLT uptake and tumor response to chemotherapy or kinase inhibitor agents [11-13]. However, low contrast between tumor uptake and background is one of the major drawbacks in the interpretation of FLT-PET images. We show that kinetic analysis is a potential solution to illuminate the associated biological changes in tumors in response to treatment.
Conclusion
The ability to measure tumor response soon after initiation therapy may provide an early indicator of the treatment efficacy. In the current clinical setting, patients are most often treated with a fixed therapy protocol when the success or failure of treatment is indicated only by the appearance of anatomic changes which may only be detected weeks or months after treatment begins. The results of the present study showed that FLT is a promising imaging marker for the prediction of tumor responses early, namely, 24 h after irradiation. The value of Ki, best correlated with in vitro FLT uptake in tumor cells, is expected to be useful as an indicator for early assessment of radiation treatment efficacy that can guide the therapeutic protocol to tailor to individual patient/tumor regarding radiation frequency and radiation doses administered or the timing to add adjuvant therapies.
Acknowledgement
The authors would like to thank Dr. Arion Chatziioannou and the staff in the small-animal imaging facility at Crump Institute for Molecular Imaging for performing the mouse PET imaging, Dr. Michael Kreissl for taking serial blood samples, and Dr. N. Satyamurthy and his staff in the UCLA medical cyclotron facility for producing the tracer FLT used in this study. This work was partly supported by DOE cooperative agreement DE-FC03-02ER63420, and by NIH grants RO1-EB001943 and P50-CA086306.
References
- 1.Boothman DA, Davis TW, Sahijdak WM. Enhanced expression of thymidine kinase in human cells following ionizing radiation. Int J Radiat Oncol Biol Phys. 1994;30:391–398. doi: 10.1016/0360-3016(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 2.Been LB, Suurmeijer AJ, Cobben DC, Jager PL, Hoekstra HJ, Elsinga PH. [18F]FLT-PET in oncology: current status and opportunities. Eur J Nucl Med Mol Imaging. 2004;31:1659–1672. doi: 10.1007/s00259-004-1687-6. [DOI] [PubMed] [Google Scholar]
- 3.Kong XB, Zhu QY, Vidal PM, et al. Comparisons of anti-human immunodeficiency virus activities, cellular transport, and plasma and intracellular pharmacokinetics of 3¢-fluoro-3¢-deoxythymidine and 3¢-azido-3¢-deoxythymidine. Antimicrob Agents Chemother. 1992;36:808–818. doi: 10.1128/aac.36.4.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vesselle H, Grierson J, Muzi M, et al. In vivo validation of 3¢ deoxy-3¢-[(18)F]fluorothymidine ([(18)F]FLT) as a proliferation imaging tracer in humans: correlation of [(18)F]FLT uptake by positron emission tomography with Ki-67 immunohistochemistry and flow cytometry in human lung tumors. Clin Cancer Res. 2002;8:3315–3323. [PubMed] [Google Scholar]
- 5.Buck AK, Halter G, Schirrmeister H, et al. Imaging proliferation in lung tumors with PET: 18F-FLT versus 18F-FDG. J Nucl Med. 2003;44:1426–1431. [PubMed] [Google Scholar]
- 6.Buck AK, Schirrmeister H, Hetzel M, et al. 3-deoxy-3-[(18)F] fluorothymidine-positron emission tomography for noninvasive assessment of proliferation in pulmonary nodules. Cancer Res. 2002;62:3331–3334. [PubMed] [Google Scholar]
- 7.Mathews MB, Bernstein RM, Franza BR, Jr, Garrels JI. Identity of the proliferating cell nuclear antigen and cyclin. Nature. 1984;309:374–376. doi: 10.1038/309374a0. [DOI] [PubMed] [Google Scholar]
- 8.Shields AF, Grierson JR, Dohmen BM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med. 1998;4:1334–1336. doi: 10.1038/3337. [DOI] [PubMed] [Google Scholar]
- 9.Mankoff DA, Shields AF, Krohn KA. PET imaging of cellular proliferation. Radiol Clin North Am. 2005;43:153–167. doi: 10.1016/j.rcl.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Waldherr C, Mellinghoff IK, Tran C, et al. Monitoring antiproliferative responses to kinase inhibitor therapy in mice with 3¢-deoxy-3¢-18F-fluorothymidine PET. J Nucl Med. 2005;46:114–120. [PubMed] [Google Scholar]
- 11.Barthel H, Cleij MC, Collingridge DR, et al. 3¢-deoxy-3¢-[18F] fluorothymidine as a new marker for monitoring tumor response to antiproliferative therapy in vivo with positron emission tomography. Cancer Res. 2003;63:3791–3798. [PubMed] [Google Scholar]
- 12.Dittmann H, Dohmen BM, Kehlbach R, et al. Early changes in [18F]FLT uptake after chemotherapy: an experimental study. Eur J Nucl Med Mol Imaging. 2002;29:1462–1469. doi: 10.1007/s00259-002-0925-z. [DOI] [PubMed] [Google Scholar]
- 13.Oyama N, Ponde DE, Dence C, Kim J, Tai YC, Welch MJ. Monitoring of therapy in androgen-dependent prostate tumor model by measuring tumor proliferation. J Nucl Med. 2004;45:519–525. [PubMed] [Google Scholar]
- 14.Schoder H, Gonen M. Screening for cancer with PET and PET/CT:potential and limitations. J Nucl Med. 2007;48:4S–18S. [PubMed] [Google Scholar]
- 15.Cook G, Maisey MN, Fogelman I. Normal variants, artefacts and interpretative pitfalls in PET imaging with 18-fluoro-2-deoxyglucose and carbon-11 methionine. Eur J Nucl Med. 1999;26:1363–1378. doi: 10.1007/s002590050597. [DOI] [PubMed] [Google Scholar]
- 16.Molthoff CFM, Klabbers BM, Berkhof J, et al. Monitoring response to radiotherapy in human squamous cell cancer bearing nude mice: comparison of 2-deoxy-2-[18F]fluoro-D-glucose (FDG) and 3-[18F]fluoro-3-deoxythymidine (FLT) Mol Imaging Biol. 2007;9:340–347. doi: 10.1007/s11307-007-0104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kubota K, Ishiwata K, Kubota R, et al. Tracer feasibility for monitoring tumor radiotherapy: a quadruple tracer study with fluorine-18-fluorodeoxyglucose or fluorine-18-fluorodeoxyuridine, L-[methyl-14C]methionine, [6-3H]thymidine, and gallium-67. J Nucl Med. 1991;32:2118–2123. [PubMed] [Google Scholar]
- 18.Zasadny K, Wahl RL. Standardized uptake values of normal tissues at PET with 2-[fluorine-18]-fluoro-2-deoxy-D-glucose: variation with body weight and a method for correction. Radiology. 1993;189:847–850. doi: 10.1148/radiology.189.3.8234714. [DOI] [PubMed] [Google Scholar]
- 19.Keyes JJ. SUV: standard uptake or silly useless value? J Nucl Med. 1995;36:1836–1839. [PubMed] [Google Scholar]
- 20.Huang S. Anatomy of SUV. Nucl Med Biol. 2000;27:643–646. doi: 10.1016/s0969-8051(00)00155-4. [DOI] [PubMed] [Google Scholar]
- 21.Phelps ME. PET: molecular imaging and its biological applications. Springer; New York: 2004. [Google Scholar]
- 22.Muzi M, Vesselle H, Grierson JR, et al. Kinetic analysis of 3′-deoxy-3′-fluorothymidine PET studies: validation studies in patients with lung cancer. J Nucl Med. 2005;46:274–282. [PubMed] [Google Scholar]
- 23.Satyamurthy N, Amarasekera B, Alvord CW, Barrio JR, Phelps ME. Tantalum [18O]water target for the production of [18F]fluoride with high reactivity for the preparation of 2-deoxy-2-[18F]fluoro-D-glucose. Mol Imaging Biol. 2002;4:65–70. doi: 10.1016/s1095-0397(01)00068-1. [DOI] [PubMed] [Google Scholar]
- 24.Pollack A, Terry NH, White RA, Cao S, Meistrich ML, Milas L. Proliferation kinetics of recruited cells in a mouse mammary carcinoma. Cancer Res. 1994;54:811–817. [PubMed] [Google Scholar]
- 25.Loening AM, Gambhir SS. AMIDE: a free software tool for multimodality medical image analysis. Mol Imaging. 2003;2:131–137. doi: 10.1162/15353500200303133. [DOI] [PubMed] [Google Scholar]
- 26.Muzi M, Mankoff DA, Grierson JR, Wells JM, Vesselle H, Krohn KA. Kinetic modeling of 3¢-deoxy-3¢-fluorothymidine in somatic tumors: mathematical studies. J Nucl Med. 2005;46:371–380. [PubMed] [Google Scholar]
- 27.Huang SC, Phelps ME, Hoffman EJ, Sideris K, Selin CJ, Kuhl DE. Noninvasive determination of local cerebral metabolic rate of glucose in man. Am J Physiol. 1980;238:E69–E82. doi: 10.1152/ajpendo.1980.238.1.E69. [DOI] [PubMed] [Google Scholar]
- 28.Phelps ME, Huang SC, Hoffman EJ, Selin CE, Kuhl DE. Tomographic measurement of regional cerebral glucose metabolic rate in man with (F-18) fluorodeoxyglucose: validation of method. Ann Neurol. 1979;6:371–388. doi: 10.1002/ana.410060502. [DOI] [PubMed] [Google Scholar]
- 29.Sokoloff L, Reivich M, Kennedy C, et al. The [14C]deoxyglucose method for the measurement of local cerebral glucose utilization: theory, procedure, and normal values in the conscious and anesthetized albino rat. J Neurochem. 1977;28:897–916. doi: 10.1111/j.1471-4159.1977.tb10649.x. [DOI] [PubMed] [Google Scholar]
- 30.Mankoff DA, Shields AF, Graham MM, Link JM, Eary JF, Krohn KA. Kinetic analysis of 2-[carbon-11]thymidine PET imaging studies: compartmental model and mathematical analysis. J Nucl Med. 1998;39:1043–1055. [PubMed] [Google Scholar]
- 31.Lee JR, Madsen MT, Bushnel D, Menda Y. A threshold method to improve standardized uptake value reproducibility. Nucl Med Commun. 2000;21:685–690. doi: 10.1097/00006231-200007000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Rasey JS, Grierson JR, Wiens LW, Kolb PD, Schwartz JL. Validation of FLT uptake as a measure of thymidine kinase-1 activity in A549 carcinoma cells. J Nucl Med. 2002;43:1210–1217. [PubMed] [Google Scholar]
- 33.Ellims PH, Van der Weyden MB, Medley G. Thymidine kinase isoenzymes in human malignant lymphoma. Cancer Res. 1981;41:691–695. [PubMed] [Google Scholar]
- 34.Larson SM, Weiden PL, Grunbaum Z, et al. Positron imaging feasibility studies. I: characteristics of [3H]thymidine uptake in rodent and canine neoplasms: concise communication. J Nucl Med. 1981;22:869–874. [PubMed] [Google Scholar]
- 35.Jeong MH, Jin YH, Kang EY, Jo WS, Park HT, Lee JD, Yoo YJ, Jeong SJ. The modulation of radiation-induced cell death by genistein in K562 cells: activation of thymidine kinase 1. Cell Res. 2004;14:295–302. doi: 10.1038/sj.cr.7290230. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman EJ, Huang SC, Phelps ME. Quantitation in positron emission computed tomography. 1. Effect of object size. J Comput Assist Tomogr. 1979;3:299–308. doi: 10.1097/00004728-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Demaria S, Ng B, Devitt ML, et al. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. Int J Radiat Oncol Biol Phys. 2004;58:862–870. doi: 10.1016/j.ijrobp.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 38.Hamada N, Matsumoto H, Hara T, Kobayashi Y. Intercellular and intracellular signaling pathways mediating ionizing radiation-induced bystander effects. J Radiat Res (Tokyo) 2007;48:87–95. doi: 10.1269/jrr.06084. [DOI] [PubMed] [Google Scholar]
- 39.Patlak C, Blasberg RG. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. J Cereb Blood Flow Metab. 1983;3:1–7. doi: 10.1038/jcbfm.1983.1. [DOI] [PubMed] [Google Scholar]
- 40.Soret M, Bacharach SL, Buvat I. Partial-volume effect in PET tumor imaging. J Nucl Med. 2007;48:932–945. doi: 10.2967/jnumed.106.035774. [DOI] [PubMed] [Google Scholar]
- 41.Wu HM, Sui G, Lee CC, Prins ML, Ladno W, Lin HD, Yu AS, Phelps ME, Huang SC. In vivo quantitation of glucose metabolism in mice using microPET imaging and a microfluidic device. J Nucl Med. 2007;48:837–845. doi: 10.2967/jnumed.106.038182. [DOI] [PubMed] [Google Scholar]
- 42.Huang SC, Wu HM, Kreissl M, Stout D, Chatziioannou A, Truong D, Schelbert HR. Evaluation of partial volume effects in mouse cardiac MicroPET images using a 4D digital mouse phantom. Mol Imaging Biol. 2005;7:134. [Google Scholar]
- 43.Ferl GZ, Wu HM, Zhang X, Huang SC. Estimation of the 18F-FDG Input function in mice using dynamic microPET and minimal blood sample data. J Nucl Med. 2007;48:2037–2045. doi: 10.2967/jnumed.107.041061. [DOI] [PMC free article] [PubMed] [Google Scholar]