Abstract
India provided one of the most challenging chapters of the worldwide smallpox eradication program. The campaign was converted from a project in which a handful of officials tried to impose their ideas on a complex health bureaucracy to one in which its components were constantly adapted to the requirements of a variety of social, political, and economic contexts. This change, achieved mainly through the active participation of workers drawn from local communities in the 1970s, proved to be a momentous policy adaptation that contributed to certification of smallpox eradication in 1980. However, this lesson appears to have been largely forgotten by those currently managing the Global Polio Eradication Initiative. We hope to show ways in which contemporary efforts to eliminate polio worldwide might profitably draw on historical information, which can indicate meaningful ways in which institutional adaptability is likely to help counter the political and social challenges being encountered in India.
THERE HAS BEEN AN unexpected upsurge in polio outbreaks in western Africa and southern Asia, which has stoked anxieties within the World Health Organization (WHO) headquarters in Geneva, Switzerland, and its South East Asia Regional Office in New Delhi, India (WHO SEARO).1 Responses to the upsurge have been complicated by political and social instability in some regions (such as Pakistan's North West Frontier Province), as well as continuing instances of bureaucratic and civilian hostility to polio vaccination within regions such as northern and eastern India; increased financial investment into polio eradication work has therefore only brought forth limited benefits.
As options and new strategies are being considered by members of the various United Nations (UN) organizations, national aid agencies, global funding bodies, and committees of experts, however, one important set of lessons appear to have been consistently ignored. These relate to the successful worldwide eradication of smallpox, which was certified in 1980 by the World Health Assembly (WHA), the international forum of WHO member states. As in the 1970s, the South Asian subcontinent—in particular, locations in the Indian states of Uttar Pradesh and Bihar—is providing significant hurdles for the successful completion of a major global disease eradication program involving the WHO.2
It is sometimes said that smallpox and polio are distinct diseases and that lessons cannot be carried over from one eradication program to the other. That is partially true—symptoms of infective polio and smallpox are quite different and therefore necessitate distinct means of identification and reporting; there are also very specific technological questions of vaccine production and deployment to consider when studying efforts to control the 2 diseases in a comparative frame. And yet, diseases and plans to eradicate them cannot be treated as entities that are purely defined by medical science. Significant elements of both are deeply influenced by a range of social and political conditions, as people in different walks in life often perceive causes of—and possible cures for—illness in widely varied ways. Public health officials are therefore forced to navigate complex administrative and societal terrains, where knowledge gleaned from scientific and medical journals can only be partially useful. From this perspective, one can argue that all immunization campaigns are deeply social and political phenomena, whose complexities require careful study and understanding by all stakeholders.
THE GLOBAL SMALLPOX PROGRAM AND INDIA
Discussions on the potential eradication of smallpox worldwide began in the WHA as early as 1950, and Brock Chisholm, the WHO's first director general, formally proposed global eradication in 1953. Noticeable progress on the issue was witnessed at the 11th WHA, which was held in Minneapolis, Minnesota, in 1958; there, Viktor Zhdanov, the Soviet deputy minister of health, argued that eradication of the variola virus was both theoretically possible and important to the world as a whole, including countries that had already expunged the disease within their territories. The so-called “Zhdanov resolution” received broad support at the gathering, leading the WHO's Executive Board to meet immediately afterward and announce preparations for a future smallpox eradication drive.3
Officials based in India, a major reservoir of smallpox cases, were brought into discussions soon after the passage of the 1958 resolution. These negotiations, which involved senior members of the WHO, the WHO SEARO, and the Indian federal government, did not go smoothly; there was disagreement about even the most basic issues, such as the exact definition of smallpox eradication. It did not help matters that Geneva-based WHO officials attempted to impose a fixed set of ideas and policies on national governments. Consequently, calls for smallpox eradication in the late 1950s and early 1960s received a frosty reception across the Indian political spectrum.4 Indian lack of interest began to change only in the mid-1960s, after reorganization of the WHO. Significantly, this reorganization placed an emphasis on employing people who were more willing than were their predecessors to engage with national politicians and public health officials in developing common ground.5 The results were impressive at one level in particular: India's federal authorities agreed to organize district-level pilot projects within each state; on paper at least, these projects would include large numbers of local health staff.6
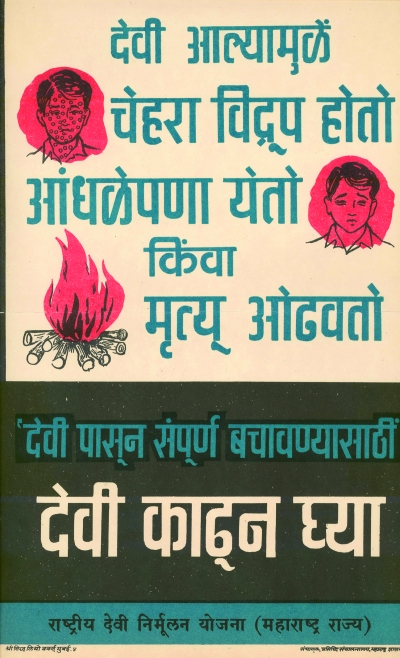
Poster advertising the dangers from smallpox and the benefits of vaccination, distributed by the government of Maharashtra state, India, 1970.
Source. Sanjoy Bhattacharya.
Almost immediately, however, insurmountable problems arose. To the frustration of several officials in Geneva, most pilot projects started late, failed to meet agreed timetables, and often produced defective data.7 The experience also brought home to them that they could not hope to micromanage the program from the top-down and from a great distance. Splits within the WHO followed. It was reported that senior WHO SEARO officials, including the regional director, openly expressed doubts about the possibility of ever eradicating smallpox; critics within the Indian federal and state governments, including members of the Office of the Indian Director General of Health Services, harbored doubts as well. By 1967, the problem deteriorated to the point that people within the WHO's Smallpox Eradication Unit, headed by Donald A. Henderson (an official with the US Centers for Disease Control and Prevention who had moved to Geneva to direct this body), feared that the Indian government would withdraw from the program.8
One of millions of children vaccinated for polio in India.
Source. Rajib Dasgupta.
The situation was finally rescued by a series of time-consuming and placatory diplomatic initiatives managed by Henderson. Through these efforts, Indian federal authorities agreed to keep the country in the global program; they also agreed to streamline the national health department, create a more dynamic smallpox unit within it, and commit greater resources to state-level smallpox eradication efforts from 1968 onwards.9 The WHO's Smallpox Eradication Units in Geneva and New Delhi began to work closely with the body set up by the Indian government.
Nicole Grasset, a French public health official employed by the WHO SEARO, was charged with coordinating work carried out by the 3 bodies, which met on a regular basis, collected information from the states and their districts, and developed policies together. The units set up mixed teams of international and Indian workers, which were given the responsibility of going into the states, searching for smallpox cases, and putting containment and vaccination schemes into place. Henderson and Grasset expected these workers to spend most of their time in India in the field, but they also arranged some time for relaxation in city-based residences and hotels.10
Those unwilling or unable to put up with the rigors of the posting were quietly relocated—to other government departments if they were Indian and out of the country if they were not. The policy was quite ruthlessly enforced such that, between 1971 and 1975, the Indian smallpox eradication program was managed by groups of well-organized workers who generally respected each other's abilities. The workers were also consistently encouraged to adapt policies to social, political, and economic conditions encountered in the field, and team managers were reminded to enlist the help of staff drawn from local communities. Crucially, they were provided access to the financial means to offer generous short-term employment contracts, and local workers were usually accorded the role of valued partners. Indeed, they helped the development of a raft of socially and politically acceptable—and thus effective—policies, most notably in states like Rajasthan, Uttar Pradesh, Bihar, Madhya Pradesh, and Bengal, where smallpox outbreaks occurred regularly and bureaucratic and civilian antagonism toward vaccination continued to be a problem in the early 1970s.11
These new arrangements were not always easily implemented. WHO SEARO retained a great degree of autonomy, and its director continued to harbor reservations about the smallpox eradication program. Over time, however, Henderson and his supporters within the WHO were able to counter this opposition through a variety of measures. For example, the team was able to negotiate the creation of a special fund with significant Swedish assistance, which the WHO's Smallpox Eradication Units were able to draw upon without time-consuming clearances from government officials. Henderson, Grasset, and Larry Brillian (an American official attached to WHO SEARO on a short-term contract) also worked hard to develop good working relations with parliamentary representatives, other politicians, and their financial backers.
Some of these connections proved invaluable at crucial junctures. The significant economic, material, and political support provided during the 1974 epidemic outbreaks in Bihar by J. R. D. Tata, head of India's powerful Tata industrial conglomerate and a funder of the ruling Indian National Congress party, is perhaps the best example of the fruits of these labors. Policy successes were fortified further through efforts to keep donors abreast of the true epidemiological situation and administrative problems in South Asia; such operational transparency was crucial to winning the trust of such organizations as the Swedish International Development Agency.12
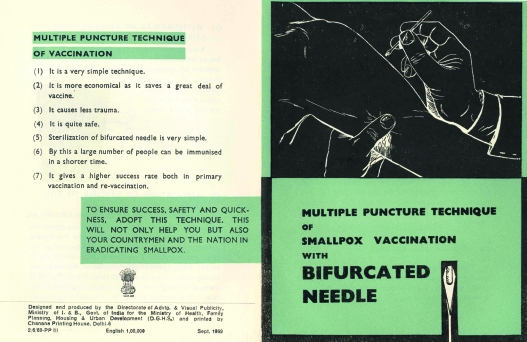
Viewed from this perspective, the question of eradicating smallpox in India was never purely a medical or biological matter, and it was not presented as such by those responsible for its eradi-cation. It was, by necessity, a substantially more intricate phenomenon, requiring careful preparation and implementation. The widespread adoptions of freeze-dried vaccine and the bifurcated needle were crucial because they made vaccination more reliable and less painful and enabled greater economy in vaccine usage. The adoption of new operational strategies, however, was equally important in the long run. International workers, for instance, often assumed the important role of accessing information from South Asian health workers of all ranks; this feedback was then used to good effect by touring epidemiologists employed by WHO in the field. The relationship between international personnel and Indian and Bangladeshi workers was a strikingly symbiotic one, especially in situations where the parties involved were open-minded and willing to listen to each other's ideas. The more democratic elements of WHO, of which there were many in the field in India in the 1970s, were able to ensure that the insightful views of junior and midlevel South Asian health and paramedical officials were not rejected outright by state- and federal-level administrators and their collaborators within the UN framework.13
Handbook distributed in 1969 by the Indian government describing the use of bifurcated needles and freeze-dried smallpox vaccine for immunization.
Source. Sanjoy Bhattacharya.
This exchange of ideas between international health personnel and local workers, and the many ways in which they strengthened smallpox eradication work, are frequently downplayed in retellings of the history of the smallpox eradication program. A number of factors appear to have contributed to the diminution of this version of events, and some of these go back several years. Although the certification of smallpox eradication was celebrated by WHO and its regional offices in 1980, these festivities, in hindsight, appear to have been perfunctory and hurried in nature. From a historian's perspective, there are links between these hurried celebrations and WHO's efforts at that time to advocate for a worldwide program of primary health care. Reportedly, festivities commemorating smallpox eradication, and colloquia intended to draw lessons from the campaign, were regarded as unnecessary distractions for the new programmatic mantra of primary health care.
National-level jealousies directed at personnel associated with the successful smallpox eradication work were also a problem, leading to a situation in which the complex factors that had led to the success of the program were downplayed. Senior government administrators who had continually insisted that smallpox was not eradicable also ensured that teams were quickly disbanded and that individual officials were isolated and frequently forced into unimportant jobs; in this manner, they were able to devalue the lessons that could have been drawn from the program.
Therefore, despite the creation of a WHO Expanded Program on Immunization post-–smallpox eradication, significant elements within WHO offices and the Indian government remained hostile to the initiation of other large-scale “vertical” disease eradication efforts. This often translated into simplistic descriptions of how variola had been wiped out, creating an almost self-perpetuating official narrative of negativity that sometimes denigrates the efforts of the many people who worked in collaboration to eradicate smallpox. This version of events is at times unquestioningly transmitted in some academic writing and policy documents, and it appears to have contributed to a situation where people responsible for designing new public health programs consider it unnecessary to study historical materials dealing with the global and national antismallpox campaigns.14
What can the Global Polio Eradication Initiative (GPEI) learn from the history of the worldwide eradication of smallpox? Might some of the strategies that proved useful in India in the 1970s also pay dividends for the managers of the troubled antipolio campaigns in that country? Success with polio eradication in India would, after all, make global polio eradication a more viable possibility. Although there have been some changes in political conditions, both internationally and nationally, we must be careful not to overstate the distinctions between the situation in the 1970s and today. We might otherwise be in danger of presenting oversimplified analyses based on a mistaken assumption that it is enough to study the attitudes and calculations of a handful of new players in international health before developing plans for a national campaign. A much wider range of official and civilian positions need careful examination, especially because they reflect significant individual variations; historical materials relating to the smallpox program can provide insights into political and social relations in India, a country of subcontinental proportions.
The relative lack of superpower rivalry, the strategic and economic dominance of the United States, and the World Bank's role in the restructuring of national health care structures have all influenced political debate at one level; this mix has been further complicated by the entry of private funding bodies such as the Bill and Melinda Gates Foundation with a global remit, as well as new collaborative aid arrangements involving private and public agencies, such as the GAVI Alliance (formerly the Global Alliance for Vaccines and Immunization) and the Global Fund to Fight Aids, Tuberculosis and Malaria. There have also been changes in the Indian political landscape. The increased incidence of relatively unstable coalition governments at federal and state levels; the greater confidence of political formations based on region, caste, or religion; and the radicalization of sections of Muslim and Hindu society have changed the terms of many debates locally.
Nevertheless, broad similarities remain at many levels. National governments continue to try to play a dominant role in proceedings within agencies such as the WHO, federal governments still enter into bilateral agreements independently of UN involvement, international and national agencies seek to raise funds for their activities from a variety of external and internal sources, different national political and community organizations tend to respond to international health programs in distinctive ways, and field workers continue to negotiate with elected governments and their representatives, as well as the members of the political opposition, as they seek to implement policies.
As in the 1970s, there are variations in attitude and ability within international, national, and local health programs; this, as in the past, stokes differences in opinion and results in different understandings of project goals and outcomes. In the GPEI, such disagreements are particularly noticeable in relation to the discussions about the involvement of “outside” agencies and the choice, efficacy, and safety of vaccines. These issues are considered in greater detail in the following section.
THE INDIAN POLIO ERADICATION PROGRAM
A 1983 meeting of public health experts in Bellagio, Italy, considered, for the first time, the idea of polio eradication as a component of the Expanded Program on Immunization.15 The following year, Rotary International formed a consultative committee to consider the goal's potential; the result was a declaration that efforts would be made to eradicate polio by 2005. This was followed by the 1985 Pan American Health Organization resolution to eradicate polio from the Western Hemisphere by 1990. In 1988, 166 member countries of the WHA signed up to the goal of global polio eradication by 2000. The initiative was projected as an “appropriate gift, together with the eradication of smallpox, from the twentieth to the twenty-first century.”16
The GPEI was thus born. Yet the unanimity characterizing the WHA 1988 resolution about the meaning of—and the strategies required for—polio eradication turned out to be illusory. At this assembly, eradication had been defined as the complete absence of the disease following concerted public health interventions; however, discussions and declarations from within and outside the confines of the WHO subsequently displayed a far less clear-cut approach to the issue.17 The Global Commission for the Certification of the Eradication of Poliomyelitis has defined “eradication” as the absence of circulation of all indigenous wild polioviruses for at least a three-year period during which surveillance activities have been maintained.18 Alternative assessments about the form and possibilities of polio eradication have persisted side by side since the launch of the GPEI. At one level, the 1988 WHA decision to recommend the oral polio vaccine (OPV) for widespread use increased the level of debate about how eradication could be best achieved. Vaccine-derived polio, field experience showed, was one of the adverse outcomes of OPV deployment. People therefore wondered if the elimination of wild polioviruses was a sufficient condition for the certification of eradication or whether the removal of cases of vaccine-derived disease was crucial as well.19
In India, OPV-based work was included in the national Expanded Program on Immunization in 1978 and 1979, which was subsequently upgraded to a Universal Immunization Program in 1985. The “Polio Plus” program was initiated in Tamil Nadu state in 1986 with a grant of US $2.6 million from Rotary International; this was followed by another US $20 million grant from the same source for financing the procurement of OPV, cold chain support (for transporting and storing vaccinations), surveillance activities, and social mobilization across the country. A staged approach to eradicate polio followed in 11 other states, with the stated aim of extending the program to other parts of the country after that.20
The expanded project took the shape of the so-called “Pulse Polio” initiative, which was started in Tamil Nadu, Kerala, and Delhi states in 1994. Also referred to as the “Supplementary Immunization Activities,” the strategy involved the mass immunization of a target population of children, aged up to 5 years, on prearranged immunization days irrespective of their earlier vaccination status. A countrywide Pulse Polio initiative was put into place in July 1995, after the state governments responded to concerted calls from federal authorities for its extension across the board. Unfortunately, the deadlines proposed at that time—for polio eradication by 2000 and certification of eradication by 2005—have joined the list of missed opportunities in the history of public health in India.21
What were the factors responsible for these targets being missed when in 1995 they appeared to have broad-based local political and scientific support? Most significantly, perhaps, the main tenet of eradication—the strengthening of ongoing routine immunization programs as part of the country's participation in the WHO-supported Expanded Program on Immunization project—was only partially followed. Instead, routine immunization coverage appears to have been weakened after the introduction of the Pulse Polio strategy, as has been noted by the country's Planning Commission; this influential federal body has recorded these adverse trends in its Tenth Five Year Plan document, after drawing on data gathered under the aegis of the National Family Health Survey.22 This situation is attributed to the deployment of the Pulse Polio initiative, which, it has been claimed, has caused official and civilian “fatigue” and created vast pools of unimmunized children.23
Oral polio vaccines in use in India.
Source. Rajib Dasgupta.
The complex causes of such difficulties was indicated in a study carried out recently in 2 endemic districts in Uttar Pradesh—Moradabad and Jyotiba Phule Nagar. This investigation found district-level program managers and medical officers complaining of lack of flexibility in local-level decision making; they reported that field workers were working under great pressure and that outbreaks of wild poliovirus had brought on the threat or imposition of penalties from the top, all of which was leading to demoralization and discontent among personnel of all ranks.24
These trends are by no means isolated; they appear also to exist in western Uttar Pradesh and some districts of Bihar, which are widely regarded as major hotspots of endemic polio.25 This situation has been variously attributed to such biological determinants as the “peculiar environmental and socio-demographic milieu of western UP [Uttar Pradesh] (high population density, high birth rate, poor sanitation, etc.) coupled with poor SIA [Supplementary Immunization Activities] performance with consequent low coverage,” as well as to such programmatic and social determinants as the “falsification of data and fierce resistance by the minority community.”26(p81) But other explanations have been suggested. It has been claimed that outpatient services provided by primary health care centers and other public health programs have been disrupted by polio-related activities, and these perceptions are widespread among government and civil society groupings. For this reason, “Why only polio?” is a question often posed by both local communities and junior public health officials.26
COUNTERMEASURES OF DOUBTFUL EFFICACY
The persistence of these problems has sometimes caused GPEI workers to adopt initiatives of doubtful long-term viability, such as encouraging local-level political and civilian leaders to distribute cash as an inducement to improve OPV uptake. There have also been reports of cases where polio vaccination was carried out forcibly by health administrators, with the support of the local police. Apart from creating hostility within affected communities, this policy has caused nervousness about the aims of the GPEI in territories where news of the use of compulsion has spread through word of mouth and the press. Indeed, the local media, especially Hindi and Urdu elements, have spread reports of vaccinal side effects, stoking concern among parents. This situation is at least partly attributable to the GPEI management's inability to develop a consistent media engagement policy within Indian states and their districts. The 17th India Expert Advisory Group, an interagency monitoring body, has called for development, implementation, and monitoring of a proactive editorial media strategy.27
This, perhaps, explains the continued suspicion toward GPEI programs within certain territorial pockets, most notably among economically and socially disadvantaged communities of all religious backgrounds. Indeed, the nature of the opposition is highly complex and cannot be explained by religious affiliation alone, as is sometimes done in discussions about supposedly undifferentiated “Muslim resistance.”28 Interviews conducted recently by R. D. among village headmen and primary health care officers in the East Khasi and Ri Bhoi districts of Meghalaya state in northeastern India indicate a complex interplay between rumors about GPEI work and resistance to OPV-based immunization; these trends appear to have been fueled partly by the Christian clergy and local media, whose members have drawn on larger socioeconomic concerns and raised objections to components of the antipolio campaign.29 Community groups have used the vaccination of children as an important bargaining point for obtaining local development projects; significantly, resistance to the Pulse Polio initiative is often most present in areas where civilian demands for roads, bridges, and public food distribution systems have not been met.30
All these problems have been accentuated by the inflexible verticality of the GPEI. Apparently demanded by a relatively small number of senior officials, this verticality has left relatively little space for community involvement. The current program is based largely on a top-down approach that does not adequately address local social, political, and economic conditions, or the variations that exist within Indian states and districts. A variety of analysts, including constituencies within the Indian medical community that had initially been supportive of the GPEI's aims, have therefore been recommending the introduction of far-ranging reforms; these include the identification of key people or groups at different levels of the civilian administration and society as well as consideration of needs based on age, gender, class, caste, religion, and education.
Some commentators have recommended the introduction of an injectable polio vaccine, arguing that the OPV is an inferior and dangerous product.31 The resulting debates have not been entirely straightforward. The supporters of OPV usage, for instance, highlight the relative economy of this form of immunization as well as national technological independence (because India mass produces OPV); there is the added “advantage” that children immunized with OPV can cross-infect, via the fecal–oral route, others with the vaccine virus and thus naturally immunize peers and family members.3
The main point, however, is that the Indian chapters of the GPEI are being censured from several perspectives and by a variety of potential stakeholders in the country.33 WHO offices are not completely oblivious to the dangers of this situation, even if some troublesome issues, such as the actual epidemiological situation, are not as frequently discussed as some observers would like. Indeed, deep-seated reforms were urged at the WHA meeting in 2007 (held May 14–23 in Geneva), especially regarding the establishment of mechanisms that would enhance political commitment and civilian participation in poliomyelitis eradication activities at all levels.34 It is incumbent on the GPEI managers, in India and elsewhere, to respond in meaningful ways to this call for operational openness.
CONCLUSIONS
We have presented a tale of 2 global eradication programs as they have unfolded in complex forms in India. We have offered comparisons in the hope that the smallpox story can prove useful to the managers of the polio campaign as it struggles to cope with fresh disease outbreaks, a resurgence of the wild poliovirus 3 strain, social opposition to reporting and vaccination, and, not least, operational disunity in the field. Although the biological natures of the diseases targeted by the 2 programs are quite distinct, we have tried to show that there is much more to consider in the design and the implementation of a global eradication effort. Lessons provided by the antismallpox campaign about the means of countering social, political, and economic challenges can be invaluable to GPEI managers and workers. These messages are of relevance to officials located at all levels of national and local government, the WHO and UNICEF administration, and agencies funding mass polio immunization campaigns. We also seek to underline the dangers of assuming that the problems currently facing the GPEI are merely technological and therefore capable of redress through laboratory-based solutions and new infusions of money.
There is another global disease eradication program whose history offers worrying insights into the long-term damage wreaked by the failure of a well-funded campaign—the unsuccessful effort to rid the world of malaria. Consistently dogged by technical difficulties, problems related to the use of DDT, and societal opposition, this program was also hamstrung by deep-seated administrative problems; these resulted mainly from the inflexible attitudes of a relatively small group of people in Geneva and New York who appeared to believe that they could ensure the development of a unitary strategy that could then be implemented worldwide. The plan proved disastrous, as federal and local governments within sovereign nations reacted badly to the dictates from distant locations; the disintegration of the malaria eradication program resulted. Some years ago, well-informed commentators warned of the pitfalls of ignoring the lessons provided by the failed malaria program and the successful smallpox campaign. Unfortunately, such warnings appear to have been ignored, to the great detriment of the global polio initiative.35
One can only hope that the global polio eradication program does not fail, even though some well-informed commentators have raised serious doubts about its chances of success. It is clear that the great challenges facing the national chapters of the GPEI, in India and elsewhere, will have to be tackled with greater sensitivity and care.36 The final phases of the smallpox program showed that careful preparation, operational flexibility, and the deployment of international staff willing to spend long stints in the field and work in close association with local health personnel are of great importance. In India specifically, broad-based support from the political and administrative establishment—in New Delhi, state and district capitals, and subdivisions and villages—would help increase the morale of local workers.
Once introduced, these reforms would have long-term benefits, even if polio was never eradicated and the long-term goal was converted to one of eliminating and controlling the spread of the disease. Indeed, operational clarity in the field would help in the development and running of a regularized polio vaccination program, as well as a host of immunization projects, which would help the long-term survival of valuable national and global Expanded Program on Immunization projects. This, in turn, would help reduce childhood mortality and increase the quality of children's lives worldwide.37
Acknowledgments
This study was funded by a grant awarded by the Medical Humanities division of the Wellcome Trust, UK, to S. Bhattacharya (grant 077551/Z/05/Z/AW/HH).
We are grateful to D. A. Henderson, Alan Schnur, Thomson Prentice, Dr William Aldis, Tony Woods, Elizabeth Shaw, Kai Khiun Liew, N. K. Arora, Sanjay Chaturvedi, Vivek Adhish, and Sangeeta Chawla for their advice and support.
Endnotes
- 1. See, for example, “Urgent Operational Improvements Critical to Stop Nigeria Outbreak, Says Expert Review Committee,” July 15, 2008, Global Polio Eradication Initiative Web site, available at http://www.polioeradication.org/content/general/LatestNews200807.asp#ERC, accessed July 22, 2008.
- 2.For a representative report on the challenges in India, see Sanjit Bagchi, “Polio Eradication Setback in India,”. Canadian Medical Association Journal. doi: 10.1503/cmaj.061716. 176(3) (2007): 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fenner F., Henderson D.A., Arita Z., Jezek, Ladnyi I.D., Smallpox and Its Eradication (Geneva: World Health Organization, 1988), 369–371 [Google Scholar]
- 4. See, for instance, memorandum from regional director, World Health Organization South East Asia Regional Office (WHO SEARO), to director, Division of Communicable Diseases, WHO headquarters (HQ), August 18, 1961, File SPX-1, Box 545, Smallpox Eradication Archives, WHO HQ (hereafter SEA/WHO)
- 5. See, for example, information provided in an enclosure to a letter from the British High Commissioner, India, to Commonwealth Relations Office, Government of Britain, November 5, 1962, File MH 55/2520, National Archives of Britain, Kew, UK.
- 6. “Proceedings of the Third Meeting of the Newly Constituted Advisory Committee of the National Smallpox Vaccination Eradication Programme Held in New Delhi on the 16th of November 1965,” File 416, Box 193, SEA/WHO.
- 7. For example, see memorandum from F.G.L. Gremlinka and J. Keka, consultants, WHO SEARO, to WHO HQ, February 7, 1967, File 416, Box 193, SEA/WHO. [Google Scholar]
- 8. Telegram from assistant director general, WHO HQ, to regional director, WHO SEARO, April 4, 1967, File 416, Box 193, SEA/WHO.
- 9. Memorandum from regional director, WHO SEARO, to D. A. Henderson, chief, Smallpox Eradication Unit (SEU), WHO HQ, January 5, 1968, File 416, Box 193, SEA/WHO.
- 10. See, for example, letter from Nicole Grasset, SEU, WHO SEARO, to D. A. Henderson, chief, SEU, WHO HQ, September 15, 1972, File 830, Box 194, SEA/WHO.
- 11. See, for instance, personal letter from Larry Brilliant, WHO SEARO, to D. A. Henderson, chief, SEU, WHO HQ, July 20, 1973, File 830, Box 194, SEA/WHO.
- 12. See letter from D.A. Henderson, chief, SEU, WHO HQ, to R. Lickfett, senior programme officer, Swedish International Development Agency, Stockholm, July 1, 1974, File 948, Box 17, SEA/WHO. An assessment of these themes is available in Sanjoy Bhattacharya, Expunging Variola: The Control and Eradication of Smallpox in India, 1947–77 (Hyderabad, India: Orient Longman, 2006) [Google Scholar]
- 13. This point is often made by international workers who recognize that they were receiving ideas from national and local workers, which were then made the basis of important, region-specific policy adaptations. Public lecture presented by Alan Schnur, WHO HQ, Geneva, at the Wellcome Trust Centre for the History of Medicine at University College London on December 5, 2007.
- 14. Interview with Mahendra Dutta, New Delhi, India, by Sanjoy Bhattacharya, May 7, 1999. See also Bhattacharya, Expunging Variola, 281–304.
- 15.John T. In: Sachdev H.P.S., Choudhury P., editors. (New Delhi: Jaypee Brothers Medical Publishers, 1996), 76–90. [Google Scholar]
- 16. WHO, 41st World Health Assembly, Geneva, May 2–13, 1988, WHA Resolution No. 41.28, “Global Eradication of Poliomyelitis by the Year 2000,” available at http://www.who.int/csr/ihr/polioresolution4128en.pdf, accessed December 20, 2007.
- 17.Dowdle W.R., “The Principles of Disease Elimination and Eradication,” Bulletin of the World Health Organization 76(2) (1998): 22–25 [PMC free article] [PubMed] [Google Scholar]
- 18. WHO, “Report of the Second Meeting of the Global Commission for the Certification of the Eradication of Poliomyelitis,” available at http://www.who.int/vaccines-documents/DocsPDF/www9813.pdf, accessed October 1, 2008.
- 19.Dowdle, “The Principles.”
- 20.Sathyamala C., Mittal O., Dasgupta R., Priya R., “Polio Eradication Initiative in India,” International Journal of Health Services 35(2) (2005): 361–383 [DOI] [PubMed] [Google Scholar]
- 21.Puliyel J.M., Gupta M.A., Mathew J.L., “Polio Eradication and the Future for Other Programmes: Situation Analysis for Strategic Planning in India,” Indian Journal of Medical Research 125 (2007): 1–4 [PubMed] [Google Scholar]
- 22.Planning Commission, Tenth Five Year Plan (2002–2007), Volume II, Sectoral Policies and Programmes, Family Welfare (New Delhi: Government of India, undated), 194–196; R. J. Yadav and K. Suresh, “Evaluation of IPPI Coverage Survey in Two Districts of Bihar,” Indian Pediatrics41 (2004): 961–963 [PubMed]
- 23.Thacker N., Shendurnikar N., “Current Status of Polio Eradication and Future Prospects,” Indian Journal of Pediatrics 71 (2004): 241–245 [DOI] [PubMed] [Google Scholar]
- 24.Dasgupta R., Chaturvedi S., Adhish V., et al. , “Social Determinants and Polio ‘Endgame’: A Qualitative Study in High Risk Districts of India,” Indian Pediatrics 45 (2008): 357–365 [PubMed] [Google Scholar]
- 25. See K. Sinha, ‘Study Finds Polio Drive Counter-Productive,” Times of India, June 1, 2008.
- 26.Thacker N., “Polio Eradication: Window of Opportunity!” Indian Pediatrics 44 (2007): 81–82; quotations from p. 81 [PubMed] [Google Scholar]
- 27. UNICEF, “India Communication Update No. 6, June 2007,” available at http://www.unicef.org, accessed November 2, 2007.
- 28. For a good example of the reporting of “Muslim” resistance to the Global Polio Eradication Initiative activities in India, see Amelia Gentleman, “A Scramble in India to Limit Polio,” International Herald Tribune, August 3, 2006, available at http://www.iht.com/articles/2006/08/01/news/polio.php, accessed October 15, 2006.
- 29. Interviews conducted by Rajib Dasgupta with medical officers and village headmen of Umsing Block, Ri Bhoi District and Mawryngkneng Block, East Khasi District, and with pediatricians at North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India, October 13–16, 2007.
- 30.Dasgupta R., Chaturvedi S., Adhish V., et al. , Social Determinants of the Polio Eradication Program—2006–2007 (New Delhi: International Clinical Epidemiology Network, 2007). [Google Scholar]
- 31.For explications in support of discontinuing the use of oral polio vaccine, see;, for instance, P. M. Bhargava, “The Politics of Polio,” The Hindu, June 11, 2008, available at http://www.hindu.com/2008/06/11/stories/2008061151410900.htm, accessed July 1, 2008); Y. Paul, “OPV Cannot Eradicate Polio From India: Do We Need Any Further Evidence?” Vaccine26 (2008): 2058–2061
- 32.Polio Eradication Committee, Indian Academy of Pediatrics, “Recommendations of 2nd National Consultative Meeting of IAP on Polio Eradication and Improvement of Routine Immunization,” Indian Pediatrics 45 (2008): 367–378 [PubMed] [Google Scholar]
- 33.For descriptions of the broad-based nature of the criticisms directed at the Global Polio Eradication Initiative, see R.K. Agarwal , “Polio Eradication in India: A Tale of Science, Ethics, Dogmas and Strategy!” Indian Pediatrics45 (2008): 349–351
- 34. WHO, “Address to the Sixtieth World Health Assembly, Dr Margaret Chan, DG of the WHO,” available at http://www.who.int/mediacentre/events/2007/wha60/en/index.html, accessed October 28, 2007.
- 35.Henderson D.A., “The Principles of Disease Elimination and Eradication,” Bulletin of the World Health Organization 76(2) (1998): 17–21 [PMC free article] [PubMed] [Google Scholar]
- 36.Arora N.K., Dasgupta R., Sushant L., “The Polio Eradication Initiative in India: Need for Evidence Based Actions,” Indian Journal of Medical Research 126 (2007): 500–501 [PubMed] [Google Scholar]
- 37.Puliyel J.M., Gupta M.A., Mathew J.L., “Polio Eradication and the Future for Other Programmes,” Indian Journal of Medical Research 125 (2007): 1–4; audio recording of 2007 Pumphandle Lecture by D. A. Henderson, available at http://www.johnsnowsociety.org/lectures/lecture2007.html, accessed December 26, 2008