Abstract
Introduction
Data on the prevalence and regional distribution of the metabolic syndrome in Germany are lacking, in particular for primary care.
Methods
In October 2005 anthropometric measurements were taken from 35 869 consecutive patients aged 18 to 99 years, in 1511 primary care practices. Waist circumference, blood pressure, lifestyle, and past medical history were assessed and blood tests taken (HDL-, LDL- and total cholesterol, triglycerides, glucose). Crude and age-standardized prevalence were calculated.
Results
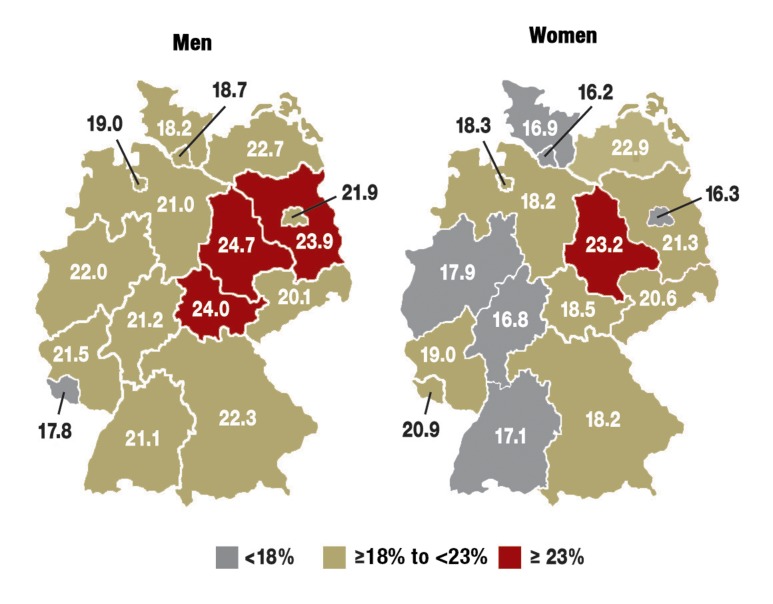
Women in the eastern part of Germany showed a higher age-standardized prevalence of the metabolic syndrome than women in the western part (21.1%; 95% CI: 19.9 to 22.4 respectively 17.7%; 95% CI: 17.2 to 18.3). In men the prevalences were 22.7% (95% CI: 20.9 to 24.4) and 21.4% (95% CI: 20.6 to 22.1) respectively. Patients from Saxony-Anhalt, Brandenburg, and Mecklenburg-Western Pomerania showed the highest prevalence, while women in Hamburg, Berlin, and Hesse and men in Schleswig-Holstein, Saarland, and Hamburg showed the lowest prevalence. Cardiovascular disease prevalence was comparable, while diabetes prevalence was higher in patients from eastern Germany (17% vs.13% in men; 12% vs. 9% in women).
Discussion
The prevalence of the metabolic syndrome in German primary care is high. Prevention efforts should focus in particular on differences in gender, socioeconomic status, and region.
Keywords: metabolic syndrome, diabetes mellitus, cardiovascular risk factors, prevalence, primary care, Germany
Regional differences in cardiovascular mortality were described in the MONICA study (Monitoring of Trends and Determinants of Cardiovascular Disease). This study was performed from 1984 to 1995 in 21 countries throughout the world (1). When the different MONICA centers in Europe are compared, marked differences are found, with a gradient from the northeast to the southwest. Finns have the highest prevalence values. Their risk of myocardial infarction is about fivefold greater than for Spaniards. Comparative analyses based on national mortality statistics between 1990 and 1992 essentially agree with these conclusions (2).
The 1996 data from the German Federal Statistical Office indicate that there are major differences in overall mortality among the 16 German federal states. Mortality from coronary infarction for men and women exhibited a comparable northeast to southwest gradient (3). The principle possible causes include differences in the classical risk factors, in socioeconomic conditions, in environmental influences, in medical care, and in genetic factors.
The metabolic syndrome includes a constellation of cardiovascular and metabolic states. It is accompanied by an increased risk of diabetes mellitus and cardiovascular morbidity and mortality (4). The diagnosis of metabolic syndrome is made when three or more of the following factors are present:
Hyperglycemia
Visceral obesity
Raised serum triglycerides
Reduced serum HDL
Arterial hypertension.
Results for the whole of Germany from the Federal Health Survey (Bundesgesundheitssurvey) for 1998 were based on the most frequently used definition of the NCEP/ATP III (2001) (5) and gave a prevalence of just over 20% (6). This was of the same order as the estimates of prevalence of the "German Metabolic and Cardiovascular Risk Project" (GEMCAS, previously with the acronym CROSS) for patients in primary care. GEMCAS was performed to determine the prevalence of the metabolic syndrome in Germany (7).
We have analyzed the GEMCAS data, with the aim of investigating regional differences in the prevalence of the metabolic syndrome for both genders. The individual criteria for the syndrome were also described separately.
Methods
Study design
The present analysis was based on the GEMCAS data. The GEMCAS was intended to collect epidemiological data throughout Germany for the prevalence of the metabolic syndrome in primary care. Detailed information on the method can be found in a separate publication (8). The study included randomly selected general practitioners from throughout Germany, as well as general physicians working in primary care and internal physicians, but no practices specializing in coronary heart disease or in diabetes. The practices were meant to include all patients, either with an appointment or appearing spontaneously during the course of a single morning, whatever the reason for the visit, and aged at least 18 years. The patients were enrolled consecutively into the study. The investigation included:
Determination of the body mass index (BMI)
Measurement of waist circumference
Measurement of blood pressure
Taking a venous blood sample, for the analysis of blood glucose and serum lipids in a central laboratory.
In addition, information on prior diseases and medication were obtained from the responsible physician. Information on lifestyle, nutritional habits, and sociodemographic characteristics were obtained from standardized questionnaires. The intention was to use a small number of questions to obtain a high completion rate and good data quality. The study was conducted according to the German GEP ("Good Epidemiological Practice") (9). One of the additional quality assurance measures included suburb and telephone monitoring throughout Germany (8).
The GEMCAS cohort was a population of persons cared for in primary care. As about 92% of all German adults have a general practitioner (10), this sample should provide a high degree of cover. In comparison to population cohorts like the Federal Health Survey or Microzensus, there were no evident differences with respect to BMI distribution, smoking or socioeconomic status (8). On the other hand, there were differences in age (more older people), gender (more women), and the prevalence of chronic diseases, such as diabetes (11).
Depending on the location of the doctor they visited, the patients were assigned to different federal states. In addition Brandenburg, Mecklenburg-Western Pomerania, Saxony, Saxony-Anhalt, and Thuringia were subsumed under East Germany and the other federal states under West Germany. See e-table 1 for the distribution of the participating doctors over the regions.
E-Table 1. Number of participating general practices in each state.
| Federal State | n |
| Baden-Württemburg | 186 |
| Bavaria | 248 |
| Berlin | 91 |
| Brandenburg | 36 |
| Bremen | 12 |
| Hamburg | 23 |
| Hesse | 87 |
| Mecklenburg-Western Pomerania | 37 |
| Lower Saxony | 141 |
| North Rhine-Westphalia | 313 |
| Rhineland-Palatinate | 64 |
| Saarland | 30 |
| Saxony | 89 |
| Saxony-Anhalt | 42 |
| Schleswig-Holstein | 58 |
| Thuringia | 54 |
| Total | 1511 |
Definition of the metabolic syndrome
The modified definition of the AHA/NHLBI (2004) was used for the diagnosis of metabolic syndrome (12). This definition includes the following criteria:
Visceral obesity with waist circumference of >102 cm in men and >88 cm in women
Raised blood pressure of >= 130 systolic and/or >= 85 mm Hg diastolic
Raised fasting glucose of 5.6 mmol/L (100 mg/dL) and/or random blood glucose of at least 11.1 mmol/L (200 mg/dL) and/or diabetes mellitus
Hypertriglyceridemia of at least 1.7 mmol/L (150 mg/dL)
Decreased HDL-cholesterol of <1.03 mmol/L (40 mg/dL) in men and <1.29 mmol/L (50 mg/dL) in women.
Drug treatment of hypertension or dyslipidemia is not considered here. These were first incorporated in the modified definition of 2005 (4). If three of the five criteria were fulfilled, the diagnosis of metabolic syndrome was made.
Statistical analysis
On the basis of an exploratory statistical analysis, the regional and gender-specific stratified prevalence values and the distributions of the individual criteria of the metabolic syndrome were determined. The prevalence values in the samples may be influenced by differences in the age structure. To avoid this, age standardization was performed for comparative purposes.
For the comparison between east and west, a weighted mean was calculated from the age- and/or gender-standardized prevalence values or mean values (reference: German population on 31 December 2004) (13). Age-standardized prevalence values and means were determined for each federal state. The comparison between west and east was based on weighted prevalence values and means. The weights then corresponded to the proportions of the population of each federal state in the overall population of West or East Germany. For continuous parameters, both a mean and a weighted mean were calculated. The weighting was performed analogously to the standardization described above. Odds ratios with 95% confidence intervals were performed with the help of log-binomial models.
Results
Study population
Between 10 and 21 October 2005, 35 869 patients were included in the study (response 84.6%). These patients came from 397 of the 438 districts and independently administered cities. Minimal information, such as age group and gender, was collected for additional patients, who either failed to fulfill the criteria for inclusion (n = 5516) or who were not prepared to participate (n = 6539) (8). The completeness of the documentation was very high (patient questionnaires, 87%; doctor’s documentation, 82%; laboratory findings, 93%). Table 1 shows the smoking status and the sociodemographic data for men and women in East and West Germany. The crude (non-age-standardized) data show that about 27% of the men in both east and west and 24% of women in the west and 20% in the east currently smoke. As regards employment status and education, the well known picture was found that East German women have on average more schooling and a higher proportion of employment than West German women. More men and more women were in employment in West Germany than in East Germany. The percentage of all unemployed persons – relative to the total number of persons capable of work – was about 10%, corresponding to the value in the official statistics for the same month.
Table 1. Sociodemographic data and smoking status of the study participants.
| Men | East Germany (n = 2578) | West Germany (n = 11 364) | ||||||
| Age mean ± SD | 54.1 ± 15.5 | 52.8 ± 15.5 | ||||||
| Crude | Standardized* | Crude | Standardized* | |||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Men | 39.0 | 38.8 | ||||||
| Size of settlement <20 000 people | 52.3 | 50.4–54.2 | 41.5 | 40.6–42.4 | ||||
| Smoking | ||||||||
| Non-smoker | 33.9 | 32.0–35.7 | 34.2 | 32.1–36.3 | 32.5 | 31.6–33.4 | 33.7 | 32.7–34.6 |
| Ex-smoker | 39.1 | 37.2–41.0 | 33.9 | 32.0–35.8 | 39.9 | 39.0–40.8 | 36.1 | 35.2–37.0 |
| Smoker | 27.1 | 25.4–28.8 | 31.9 | 29.9–33.4 | 27.6 | 26.8–28.4 | 30.3 | 29.3–31.2 |
| Employment status | ||||||||
| Employed | 45.8 | 43.9–47.8 | 51.7 | 49.8–53.5 | 53.6 | 52.7–54.5 | 56.7 | 56.0–57.5 |
| Unemployed | 11.0 | 9.8–12.2 | 12.2 | 10.7–13.9 | 6.3 | 5.8–6.7 | 6.3 | 5.8–6.8 |
| Not working | 43.2 | 41.3–45.1 | 36.2 | 34.8–37.6 | 40.1 | 39.2–41.0 | 37.0 | 36.3–37.6 |
| Number of years schooling | ||||||||
| < 10 | 6.1 | 5.2–7.1 | 7.2 | 5.9–8.4 | 9.5 | 9.0–10.0 | 9.9 | 9.3–10.5 |
| = 10 | 53.0 | 51.0–54.9 | 54.5 | 52.3–56.7 | 50.3 | 49.4–51.3 | 49.9 | 48.9–51.0 |
| > 10 | 40.9 | 39.0–42.8 | 38.3 | 36.2–40.5 | 40.2 | 39.3–41.1 | 40.2 | 39.2–41.2 |
| Women | East Germany (n = 4030) | West Germany (n = 17 897) | ||||||
| Age mean ± SD | 52.0 ± 15.8 | 50.6 ± 16.3 | ||||||
| Women | 61.0 | 60.6–61.7 | 61.0 | 59.8–62.2 | ||||
| Size of settlement <20 000 people | 51.8 | 50.2–53.3 | 42.0 | 41.3–42.7 | ||||
| Smoking | ||||||||
| Non-smoker | 62.4 | 60.9–64.0 | 60.5 | 58.9–62.1 | 52.3 | 51.6–53.0 | 53.0 | 52.3–53.8 |
| Ex-smoker | 17.5 | 16.3–18.7 | 17.0 | 15.8–18.3 | 23.4 | 22.8–24.0 | 22.3 | 21.6–22.9 |
| Smoker | 20.1 | 18.9–21.4 | 22.5 | 21.2–23.9 | 24.3 | 23.7–24.9 | 24.7 | 24.1–25.4 |
| Employment status | ||||||||
| Employed | 49.9 | 48.4–51.5 | 52.6 | 51.3–53.9 | 44.0 | 43.3–44.8 | 44.2 | 43.6–44.8 |
| Unemployed | 8.3 | 7.4–9.1 | 7.9 | 7.0–8.8 | 3.4 | 3.2–3.7 | 3.1 | 2.8–3.4 |
| Not working | 41.8 | 40.3–43.4 | 39.6 | 38.5–40.7 | 52.5 | 51.8–53.3 | 52.7 | 52.0–53.3 |
| Number of years schooling | ||||||||
| < 10 | 9.6 | 8.6–10.5 | 9.6 | 8.7–10.5 | 20.4 | 19.8–21.0 | 20.1 | 19.6–20.7 |
| = 10 | 56.7 | 55.1–58.2 | 55.6 | 54.0–57.3 | 56.1 | 55.4–56.8 | 56.1 | 55.4–56.9 |
| > 10 | 33.8 | 32.3–35.3 | 34.7 | 33.2–36.3 | 23.5 | 22.9–24.1 | 23.8 | 23.1–24.4 |
*Age standardization on the basis of the German population on 31 December 2004 (13) SD, standard deviation
Frequency of risk factors
e-table 2 shows the regional distribution of the individual risk factors which influence the metabolic syndrome. For the men, the only differences between West Germany and East Germany were in the higher HDL-cholesterol values in the East German men. In contrast, the risk profile was consistently worse in the East German than in the West German women.
E-Table 2. Distribution of cardiovascular risk factors and prevalence of cardiovascular diseases and diabetes mellitus.
| Men | East Germany (n = 2578) | West Germany (11 364) | ||||||
| Crude | Standardized*1 | Crude | Standardized*1 | |||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Waist circumference (cm) | 98.9 | 98.5–99.4 | 97.8 | 96.3–97.3 | 98.9 | 98.6–99.0 | 97.1 | 96.8–97.3 |
| Systole (mm Hg) | 134.4 | 133.7–135.0 | 132.5 | 131.8–133.2 | 133.7 | 133.1–133.8 | 131.9 | 131.6–132.3 |
| Diastole (mm Hg) | 81.4 | 81.1–81.8 | 81.0 | 80.5–81.4 | 81.4 | 81.2–81.6 | 80.8 | 80.6–81.0 |
| Glucose (mg/dL) | 100.7 | 99.4–102.1 | 97.9 | 96.6–99.1 | 99.3 | 98.7–100.1 | 96.4 | 95.8–97.1 |
| Triglyceride (mg/dL) | 182.7 | 177.0–188.4 | 176.7 | 170.8–182.5 | 178.2 | 175.5–181.8 | 171.7 | 168.8–174.5 |
| HDL-cholesterol (mg/dL) | 55.8 | 55.3–56.4 | 55.5 | 54.9–56.2 | 53.9 | 53.7–54.2 | 53.6 | 53.3–53.9 |
| LDL-cholesterol (mg/dL) | 129.5 | 128.1–131.0 | 127.2 | 125.6–128.7 | 127.8 | 127.1–128.4 | 125.7 | 125.0–126.4 |
| Weight (kg) | 85.7 | 85.2–86.3 | 84.9 | 84.2–85.5 | 86.3 | 86–86.6 | 85.6 | 85.3–85.9 |
| BMI (kg/m2) | 27.7 | 27.5–27.8 | 27.2 | 27.0–27.3 | 27.5 | 27.6–27.6 | 27.1 | 27.0–27.2 |
| CHD*2 | 12.8 | 11.5–14.1 | 10.1 | 9.0–11.2 | 13.1 | 12.5–13.7 | 11.1 | 10.6–11.6 |
| Diabetes*2 | 24.2 | 22.5–26.0 | 17.0 | 15.6–18.3 | 19.0 | 18.3–19.8 | 13.4 | 12.8–14.0 |
| Women | East Germany (n = 4030) | West Germany (17 897) | ||||||
| Crude | Standardized*1 | Crude | Standardized*1 | |||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Waist circumference (cm) | 88.4 | 88.0–88.8 | 86.8 | 86.4–87.2 | 86.4 | 86.2–86.6 | 85.6 | 85.4–85.8 |
| Systole (mm Hg) | 130.0 | 129.4–130.5 | 128.1 | 127.5–128.6 | 128.2 | 127.9–128.4 | 127.2 | 127.0–127.5 |
| Diastole (mm Hg) | 79.8 | 79.5–80.1 | 78.9 | 78.5–79.2 | 79.0 | 78.9–79.2 | 78.5 | 78.4–78.7 |
| Glucose (mg/dL) | 95.7 | 94.5–97.0 | 93.1 | 92.1–94.1 | 92.8 | 92.3–93.2 | 91.1 | 90.7–91.6 |
| Triglyceride (mg/dL) | 141.7 | 139.1–144.4 | 136.8 | 134.2–139.3 | 133.7 | 132.4–134.9 | 130.7 | 129.5–131.8 |
| HDL-cholesterol (mg/dL) | 67.1 | 66.6–67.7 | 67.1 | 66.5–67.3 | 67.3 | 67.0–67.5 | 67.2 | 66.9–67.4 |
| LDL-cholesterol (mg/dL) | 130.4 | 129.2–131.5 | 126.3 | 125.1–127.4 | 127.5 | 126.9–128.0 | 125.4 | 124.8–125.9 |
| Weight (kg) | 73.0 | 72.6–73.5 | 71.9 | 71.4–72.4 | 71.7 | 71.5–71.9 | 71.2 | 70.9–71.4 |
| BMI (kg/m2) | 27.2 | 27.0–27.4 | 26.4 | 26.5–26.8 | 26.4 | 26.3–26.5 | 26.2 | 26.1–26.3 |
| CHD*2 | 4.8 | 4.1–5.5 | 4.4 | 3.8–5.0 | 4.8 | 4.5–5.2 | 4.8 | 4.5–5.1 |
| Diabetes*2 | 15.3 | 14.2–16.5 | 12.3 | 11.3–13.2 | 11.5 | 11.0–12.0 | 9.2 | 8.8–9.6 |
*1 Standardized to the German population on 31 December 2004; *2 Myocardial infarction in the medical history, stroke and/or type 1 or type 2 diabetes mellitus; CI, confidence interval; CHD, coronary heart disease; BMI, body mass index
There were no regional differences for either men or women with respect to the prevalence values for cardiovascular diseases, such as myocardial infarction or stroke (e-table 2). In contrast, the prevalence of diabetes mellitus was clearly different in West and East Germany. The proportion of both male and female diabetics was markedly higher in East Germany than in West Germany (age-standardized prevalence values: men, 17.0% versus 13.4%; women, 12.3% versus 9.2%).
Prevalence of the metabolic syndrome
The age-standardized prevalence of the metabolic syndrome for the whole of Germany was 19.8% (men 22.7%, women 18.0%) (8). The metabolic syndrome was more frequent in East Germany than in West Germany (table 2). The highest crude prevalence values were 27% in the male patients in East Germany. After age standardization, the East German and West German men gave similar values (22.7% versus 21.1%, respectively). On the other hand, a clear difference remained for the East German women (21.4% versus 17.7%). With the sole exceptions of Saxony, Saarland, and Mecklenburg-Western Pomerania, higher age-standardized prevalence values were consistently found for men than for women (table 3).
Table 2. Crude and age-standardized prevalence estimates*1 for the metabolic syndrome and its individual criteria according to gender and region.
| East Germany (n = 6608) | West Germany (n = 29 261) | |||||||
| Men | Women | Men | Women | |||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Metabolic syndrome, crude | 27.0 | 25.3–28.8 | 23.3 | 22.0–24.7 | 24.7 | 23.8–25.5 | 18.4 | 17.8–19.0 |
| age-standardized | 22.7 | 20.9–24.4 | 21.1 | 19.9–22.4 | 21.4 | 20.6–22.1 | 17.7 | 17.2–18.3 |
| Single criteria | ||||||||
| Waist circumference, crude | 36.0 | 34.2–37.9 | 45.8 | 44.3–47.3 | 36.5 | 35.6–37.4 | 40.5 | 39.8–41.2 |
| age-standardized | 31.0 | 29.2–32.9 | 41.4 | 39.9–42.9 | 32.3 | 31.5–33.2 | 38.6 | 37.9–39.3 |
| Hypertriglyceridemia, crude | 26.2 | 24.3–28.1 | 14.5 | 13.3–15.7 | 23.4 | 22.6–24.3 | 12.5 | 12.0–13.0 |
| age-standardized | 23.6 | 21.6–25.5 | 13.3 | 12.2–14.4 | 21.7 | 20.8–22.6 | 12.1 | 11.6–12.6 |
| Raised HDL-cholesterol, crude | 10.0 | 8.9–11.2 | 14.2 | 13.1–15.3 | 12.8 | 12.1–13.4 | 13.8 | 13.3–14.3 |
| age-standardized | 10.0 | 8.7–11.3 | 14.6 | 13.4–15.8 | 13.0 | 12.3–13.6 | 13.8 | 13.3–14.3 |
| Hypertension, crude | 69.7 | 67.9–71.5 | 56.7 | 55.2–58.3 | 65.9 | 65.0–66.8 | 52.1 | 51.3–52.8 |
| age-standardized | 64.8 | 62.7–66.9 | 62.2 | 61.3–63.2 | 52.0 | 50.6–53.4 | 49.5 | 48.9–50.2 |
| Hyperglycemia, crude | 34.4 | 32.6–36.5 | 22.0 | 20.6–23.2 | 28.4 | 27.6–29.3 | 16.6 | 16.0–17.2 |
| age-standardized | 28.3 | 26.6–30.1 | 19.6 | 18.5–20.8 | 24.0 | 23.2–24.7 | 15.5 | 15.3–16.2 |
Limits for waist circumference: men >102 cm, women >88 cm;
limits for triglycerides:>=150 mg/dL;
limits for HDL-cholesterol: men <40 mg/dL, women <50 mg/dL;
limits for blood pressure:>=130/>=85 mm Hg;
limits for hyperglycemia: fasting glucose >=100 mg/dL and/or random blood glucose >=200 mg/dL and or diabetes mellitus.
*1 Standardized for the German population on 31 December 2004 (13);
(missing values: waist circumference, n = 233, triglycerides, n = 5466, HDL-cholesterol, n = 541, blood pressure, n = 134, blood sugar, n = 2667, metabolic syndrome, n = 2786).
Table 3. Sample prevalence and age-standardized prevalence of the metabolic syndrome (%, 95% confidence intervals) for men and women in the different federal states (age standardization on the basis of the German population on 31 December 2004).
| Federal State | Total | Men | Women | ||||||||||
| Crude | Standardized | Crude | Standardized | Crude | Standardized | ||||||||
| n | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Baden-Württemburg | 3983 | 20.9 | 19.7–22.2 | 18.6 | 17.5–19.8 | 21.5 | 19.4–23.6 | 21.1 | 19.1–23.0 | 15.6 | 14.2–17.2 | 17.1 | 15.7–18.6 |
| Bavaria | 5212 | 21.4 | 20.3–22.5 | 19.6 | 18.6–20.6 | 22.0 | 20.1–23.9 | 22.3 | 20.5–24.1 | 15.8 | 14.6–17.1 | 18.2 | 17.0–19.4 |
| Berlin | 1939 | 19.9 | 18.1–21.7 | 18.5 | 16.9–20.2 | 20.9 | 17.9–24.1 | 21.9 | 19.0–24.8 | 14.4 | 12.4–16.5 | 16.3 | 14.3–18.3 |
| Brandenburg | 893 | 27.5 | 24.6–30.6 | 22.0 | 19.6–24.8 | 24.1 | 19.4–29.2 | 23.9 | 19.0–28.8 | 20.7 | 17.4–24.4 | 21.3 | 18.2–24.3 |
| Bremen | 293 | 19.8 | 15.4–24.8 | 16.4 | 12.4–20.3 | 18.6 | 11.6–27.6 | 19.0 | 12.2–25.7 | 14.0 | 9.3–19.9 | 18.3 | 14.1–22.5 |
| Hamburg | 407 | 18.2 | 14.6–22.3 | 17.2 | 13.6–20.7 | 20.0 | 13.9–27.3 | 18.7 | 12.9–24.5 | 14.3 | 10.2–19.3 | 16.2 | 11.8–20.7 |
| Hesse | 1877 | 19.3 | 17.5–21.2 | 18.5 | 16.8–20.3 | 19.7 | 16.8–22.9 | 21.2 | 18.3–24.1 | 13.7 | 11.7–15.8 | 16.8 | 14.6–19.0 |
| Mecklenburg-Western Pomerania | 858 | 26.2 | 23.3–29.3 | 23.2 | 20.4–26.0 | 23.8 | 19.4–28.7 | 22.7 | 18.2–27.2 | 20.6 | 17.1–24.5 | 22.9 | 19.4–26.3 |
| Lower Saxony | 2869 | 20.4 | 19.0–21.9 | 19.2 | 17.8–20.6 | 20.3 | 17.9–22.8 | 21.0 | 18.6–23.3 | 16.0 | 14.3–17.8 | 18.2 | 16.4–19.9 |
| North Rhine-Westphalia | 7192 | 21.4 | 20.5–22.4 | 19.5 | 18.6–20.3 | 21.5 | 20.0–23.1 | 22.0 | 20.5–23.6 | 16.1 | 15.0–17.2 | 17.9 | 16.9–19.0 |
| Rhineland-Palatinate | 1397 | 22 | 19.9–24.3 | 19.9 | 18.0–21.8 | 22.7 | 19.1–26.5 | 21.5 | 18.3–24.8 | 16.2 | 13.8–18.9 | 19.0 | 16.6–21.4 |
| Saarland | 646 | 20.6 | 17.5–23.9 | 19.7 | 16.7–22.7 | 16.9 | 12.4–22.3 | 17.8 | 13.5–22.0 | 16.6 | 13.0–20.7 | 20.9 | 17.1–24.8 |
| Saxony | 2041 | 23.5 | 21.7–25.4 | 20.2 | 18.6–21.9 | 18.6 | 16.0–21.5 | 20.1 | 17.3–22.8 | 18.3 | 16.1–20.6 | 20.6 | 18.6–22.7 |
| Saxony-Anhalt | 1026 | 25.2 | 22.6–28.0 | 23.5 | 21.0–26.0 | 22.8 | 18.5–27.6 | 24.7 | 20.1–29.2 | 20.1 | 17.1–23.4 | 23.2 | 20.2–26.2 |
| Schleswig-Holstein | 1123 | 18.3 | 16.1–20.7 | 17.3 | 15.1–19.5 | 18.5 | 14.9–22.6 | 18.2 | 14.6–21.7 | 14.7 | 12.1–17.6 | 16.9 | 14.1–19.7 |
| Thuringia | 1327 | 23.5 | 21.3–25.9 | 20.7 | 18.5–22.8 | 24.6 | 20.9–28.5 | 24.0 | 20.3–27.7 | 17.1 | 14.6–20.0 | 18.5 | 15.8–21.2 |
Even though this relatively crude comparison between East and West Germany failed to find any major difference in the prevalence of the metabolic syndrome, the more exact regional analysis by federal state identified regional focuses (figure, table 3).
Figure.
Age-standardized prevalence estimates for the metabolic syndrome for men and women in the different federal states.
Estimation of the prevalence after adjustment
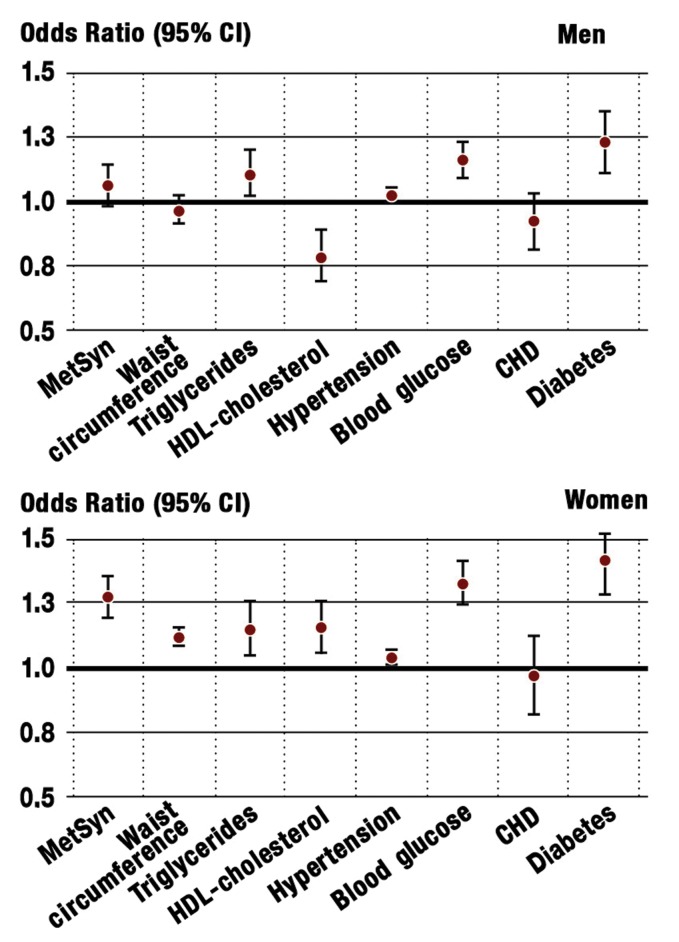
In addition to age and gender, the results may be influenced by other confounding factors, such as settlement size, degree of education and form of employment. To investigate these factors, adjusted odds ratios were estimated. In particular, this emphasized the marked age dependence of the metabolic syndrome (e-table3). It was also confirmed that the only differences between East German and West German men were in different lipid levels and blood sugar concentrations, as well as in the occurrence of diabetes mellitus (e-figure 1). Aside from the frequency of CHD, all factors were found more frequently in East German women than in West German women.
E-Table 3. Odds ratios (OR) of the individual criteria for the metabolic syndrome, CHD, and diabetes mellitus, adjusted for age, site of settlement, employment status, and education.
| Waist circumference | Triglyceride | HDL-cholesterol | Blood pressure | Blood glucose | CHD | Diabetes mellitus | ||||||||
| Men | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| East Germany | 0.96 | 0.91–1.02 | 1.10 | 1.02–1.20 | 0.78 | 0.69–0.89 | 1.02 | 1.00–1.05 | 1.16 | 1.09–1.23 | 0.92 | 0.81–1.03 | 1.23 | 1.11–1.35 |
| Berlin | 1.05 | 0.96–1.15 | 1.09 | 0.94–1.25 | 0.80 | 0.64–0.99 | 0.92 | 0.86–0.97 | 1.14 | 1.02–1.27 | 1.03 | 0.84–1.27 | 1.07 | 0.89–1.27 |
| Age 35–49 | 2.31 | 2.03–2.62 | 1.79 | 1.56–2.05 | 1.06 | 0.92–1.23 | 1.35 | 1.28–1.43 | 3.36 | 2.71–4.17 | 17.6 | 6.49–47.6 | 3.86 | 2.78–5.36 |
| Age 50–59 | 3.32 | 2.94–3.76 | 1.99 | 1.74–2.28 | 0.93 | 0.80–1.07 | 1.64 | 1.55–1.74 | 6.94 | 5.65–8.54 | 55.6 | 20.7–148.8 | 10.03 | 7.32–13.7 |
| Age 60–69 | 3.30 | 2.89–3.76 | 1.89 | 1.62–2.20 | 0.76 | 0.64–0.92 | 1.79 | 1.69–1.90 | 7.49 | 6.06–9.26 | 64.9 | 24.2–174.4 | 10.41 | 7.54–14.4 |
| Age 70–99 | 3.37 | 2.95–3.86 | 1.57 | 1.33–1.85 | 0.82 | 0.68–1.00 | 1.83 | 1.72–1.95 | 7.77 | 6.27–9.63 | 93.6 | 34.8–251.4 | 11.03 | 7.96–15.3 |
| Settlement < 20 ti | 1.09 | 1.04–1.14 | 1.03 | 0.96–1.11 | 0.98 | 0.89–1.07 | 1.02 | 1.00–1.04 | 0.99 | 0.94–1.04 | 0.94 | 0.85–1.04 | 0.97 | 0.89–1.05 |
| Unemployed | 1.18 | 1.08–1.28 | 1.12 | 0.99–1.27 | 1.15 | 0.97–1.36 | 1.02 | 0.97–1.07 | 1.37 | 1.24–1.51 | 1.65 | 1.31–2.08 | 1.76 | 1.51–2.05 |
| Not working | 1.17 | 1.10–1.26 | 0.97 | 0.88–1.07 | 1.09 | 0.95–1.25 | 0.98 | 0.94–1.01 | 1.26 | 1.16–1.36 | 2.09 | 1.78–2.45 | 1.56 | 1.38–1.77 |
| Schooling < 10 years | 1.09 | 1.02–1.17 | 1.08 | 0.96–1.21 | 1.25 | 1.08–1.44 | 0.98 | 0.94–1.02 | 1.11 | 1.03–1.20 | 1.18 | 1.02–1.36 | 1.26 | 1.12–1.42 |
| Schooling > 10 years | 0.84 | 0.80–0.88 | 0.89 | 0.83–0.95 | 0.83 | 0.75–0.91 | 0.95 | 0.93–0.98 | 0.74 | 0.70–0.79 | 0.89 | 0.80–0.98 | 0.70 | 0.64–0.76 |
| Women | ||||||||||||||
| East Germany | 1.12 | 1.09–1.16 | 1.15 | 1.05–1.26 | 1.16 | 1.06–1.26 | 1.04 | 1.01–1.07 | 1.33 | 1.25–1.42 | 0.97 | 0.82–1.13 | 1.42 | 1.29–1.56 |
| Berlin | 0.95 | 0.89–1.02 | 1.15 | 0.98–1.34 | 1.16 | 1.01–1.33 | 0.96 | 0.92–1.01 | 1.24 | 1.11–1.39 | 1.02 | 0.79–1.33 | 1.29 | 1.09–1.53 |
| Age 35–49 | 1.61 | 1.49–1.74 | 1.44 | 1.23–1.68 | 0.96 | 0.87–1.06 | 1.77 | 1.65–1.89 | 2.85 | 2.28–3.55 | 6.99 | 2.53–19.29 | 3.80 | 2.72–5.31 |
| Age 50–59 | 2.31 | 2.14–2.48 | 2.23 | 1.91–2.60 | 0.79 | 0.70–0.88 | 2.69 | 2.52–2.87 | 6.67 | 5.39–8.26 | 29.5 | 10.81–78.6 | 9.45 | 6.83–13.1 |
| Age 60–69 | 2.51 | 2.33–2.71 | 2.67 | 2.26–3.15 | 0.68 | 0.60–0.77 | 3.17 | 2.96–3.39 | 8.96 | 7.22–11.1 | 52.0 | 19.22–140.7 | 12.5 | 9.00–17.4 |
| Age 70–99 | 2.56 | 2.36–2.76 | 2.66 | 2.24–3.15 | 0.77 | 0.68–0.87 | 3.38 | 3.16–3.62 | 11.28 | 9.07–14.0 | 114.0 | 42.20–308.2 | 16.9 | 12.1–23.5 |
| Settlement < 20 ti | 1.04 | 1.01–1.07 | 1.01 | 0.94–1.09 | 0.96 | 0.90–1.03 | 1.03 | 1.00–1.05 | 1.02 | 0.97–1.08 | 0.92 | 0.81–1.04 | 1.04 | 0.96–1.13 |
| Unemployed | 1.40 | 1.32–1.49 | 1.91 | 1.63–2.24 | 1.69 | 1.47–1.94 | 1.11 | 1.04–1.17 | 1.70 | 1.48–1.96 | 2.18 | 1.49–3.17 | 2.01 | 1.64–2.45 |
| Not working | 1.17 | 1.12–1.22 | 1.33 | 1.21–1.47 | 1.34 | 1.23–1.45 | 1.04 | 1.01–1.08 | 1.29 | 1.18–1.42 | 1.57 | 1.25–1.97 | 1.52 | 1.35–1.73 |
| Schooling < 10 years | 1.21 | 1.17–1.25 | 1.17 | 1.07–1.28 | 1.54 | 1.42–1.67 | 1.05 | 1.03–1.08 | 1.38 | 1.30–1.46 | 1.12 | 0.98–1.28 | 1.51 | 1.39–1.66 |
| Schooling > 10 years | 0.77 | 0.73–0.80 | 0.81 | 0.73–0.89 | 0.71 | 0.65–0.78 | 0.90 | 0.87–0.93 | 0.78 | 0.71–0.86 | 0.78 | 0.63–0.95 | 0.73 | 0.64–0.83 |
Reference: patient in primary care within the West German states, age under 35, employed, practice in settlement of >20 000 inhabitants, =10 years of schooling;
CHD, coronary heart disease; CI, confidence interval; TI, thousand inhabitants
E-Figure.
Odds ratios of the metabolic syndrome (MetSyn), its individual criteria, coronary heart disease (CHD) and diabetes for men and women from East Germany, in comparison to men and women from West Germany; each adjusted for age, employment status, settlement size, number of years of schooling. Reference: patient in primary care within the West German states, age under 35, employed, practice in settlement of >20 000 inhabitants, =10 years of schooling.
Discussion
The results of the study show that the prevalence values for the classical cardiovascular risk factors and for the metabolic syndrome are greater in primary care in East Germany than in West Germany. The differences between East German and West German men were minor. In contrast, the risk profile tended to be less favorable for East German women than for West German women.
The nominal differences in cardiovascular risk factors are only moderate, although differences are seen in the greater waist circumference and in increased blood pressure and blood fat values. On the other hand, several studies have documented how even very small differences in (for example) blood pressure can influence cardiovascular prognosis (14, 15). In a meta-analysis of 61 cohort studies, the Prospective Studies Collaboration showed that a reduction in blood pressure of only 2 mm Hg could reduce the relative risk of mortality from ischemic heart disease by 7% and from stroke by 10%. The figures for the absolute reduction in risk were not reported (15). In analogous manner, only slight increases in BMI (or waist circumference) can lead to increased mortality (14, 16). Nevertheless, no causal connection can be established between increased risk factors and morbidity and mortality, as these are not longitudinal studies. They do confirm the associations in other large cohort studies and might encourage more attention for this risk constellation.
Both the crude and the age-standardized values for the prevalence of the metabolic syndrome in primary care were markedly higher in the East German states, particularly Brandenburg, Mecklenburg-Western Pomerania, and Saxony-Anhalt, than in the West German states. The only exception was Saxony. The lowest age-standardized prevalence values were found in women in Hamburg, Schleswig-Holstein, and Hesse (16% to 17%) and the highest values in Brandenburg, Mecklenburg-Western Pomerania, and Saxony-Anhalt (21% to 23%).
The values for men were generally higher, but presented a similar picture. As with women, there was a difference of about 6% between the lowest age-standardized prevalence values – in Schleswig-Holstein, Hamburg, and Bremen – (18% to 19%) and the highest values (24% to 25%), in Brandenburg, Thuringia, and Saxony-Anhalt. The exceptions to this generalization were the men in Saxony, with low prevalence, and the women in Saarland, with high prevalence. Independently of the age structure in the individual federal states, the prevalence figures for metabolic syndrome in primary care were highest for both men and women in Saxony-Anhalt.
The metabolic syndrome describes a typical constellation of overweight concentrated in the trunk (visceral obesity), arterial hypertension, abnormal glucose tolerance, and dyslipidemia. Taken together, these form an atherogenic network (17), which markedly increases the risk of development of type 2 diabetes mellitus and cardiovascular diseases (18, 19).
Although no difference in the prevalence values for cardiovascular diseases were observed (in contrast to the documented higher coronary mortality in East Germany in 1999), diabetes was markedly more common in East Germany than in West Germany, for both men and women. Although there is some controversy about the metabolic syndrome as a predictor of cardiovascular events (20), its significance for the development of diabetes is undisputed. Even if diabetics are excluded, 14% to 23% of the population in primary care was found to have the metabolic syndrome, particularly in Brandenburg, Thuringia, Mecklenburg-Western Pomerania, Saxony, and Saxony-Anhalt (data not shown).
Because of the cross-sectional design of this study, no temporal associations or causality could be identified for the prediction of CHD and diabetes. The results of the analysis are therefore coupled to the validity of this risk concept. These high prevalence values for both the individual risk factors and the symptom complex of the metabolic syndrome nevertheless give reason to fear that there will be at least no decrease in CHD mortality, particularly in East Germany. Further information will be provided by prospective cohort studies on cardiovascular diseases, such as KORA in the south (21), SHIP in the northeast (22), CARLA in central Germany (23), and the Heinz Nixdorf Recall Study in the West (24).
In spite of the high prevalence values found for the classical risk factors and for the metabolic syndrome, solutions should not concentrate broadly on intensified medical treatment of these factors. On the one hand, high risk patients must be comprehensively cared for, particularly regarding their frequent metabolic abnormalities and cardiovascular diseases. On the other hand, the high prevalence values are the consequence of taking low limiting values (20). In particular, the criteria for the metabolic syndrome are not the result of prospective studies. The most modern definition of the metabolic syndrome was the result of an international consensus and was published by the International Diabetes Federation in 2005 (25). Using this definition would increase the overall prevalence of the metabolic syndrome in the GEMCAS patient group to 30.7%, in comparison to 18.7% according to the NCEP/ATP III definition of 2001 (7).
It would not be expedient to treat all patients in primary care with the metabolic syndrome with drugs to counteract the spread and increase of the risk factors. Even though previous preventive approaches at lifestyle modification have been far from encouraging and have even been called into doubt, the current results suggest various approaches for more specific prevention. These should allow for regional and gender-specific needs and should especially consider the enormous socioeconomic differences in the population, which have long been underestimated.
Résumé
This is the first presentation of a comprehensive investigation of regional differences in the metabolic syndrome and its risk factors in primary care. The underlying data were recorded under realistic conditions of medical practice. Further studies are needed to research the causes for the regional and genderspecific differences in the prevalence of risk factors and to develop and evaluate sensible preventive strategies orientated towards specific target groups.
Acknowledgments
The authors wish to thank the participating medical practices and patients, employees of Labor 28 (Berlin), and the IMIBE medical documentation group of Essen University Hospital, in particular Ms Katja Frehse, for their valuable collaboration.
The study was supported by an "unrestricted educational research grant" from the company Sanofi Aventis Deutschland GmbH, Berlin.
Translated from the original German by Rodney A. Yeates, M.A., Ph.D.
Footnotes
Conflict of interest statement
Dr. Moebus has been paid lecture fees by the company Sanofi Aventis.
PD Dr. Bramlage has received financial support for research and lectures from various pharmaceutical companies (Sanofi-Aventis, Takeda, Daiichi Sankyo, Novartis, Berlin Chemie, Schwarz Pharma, Medac).
Prof. Hauner has received lecture fees from the companies Sanofi Aventis, Lilly, Novartis, and Merck. He has received support for research from Sanofi Aventis, Lilly, and Pfizer.
Prof. Jöckel is carrying out a series of externally funded projects and preparing expert reports in his department for Astra Zeneca, Takeda Pharma, and other pharmaceutical companies.
References
- 1.Tunstall-Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353:1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 2.Sans S, Kesteloot H, Kromhout D. The burden of cardiovascular diseases mortality in Europe. Task Force of the European Society of Cardiology on Cardiovascular Mortality and Morbidity Statistics in Europe. Eur Heart J. 1997;18:1231–1248. erratum Eur Heart J 1997; 18 1231-48. [PubMed] [Google Scholar]
- 3.Willich SN. Regionale Unterschiede der Herz-Kreislauf-Mortalität in Deutschland. Dtsch Arztebl. 1999;96(8):A 483–A 488. [Google Scholar]
- 4.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 5.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 6.Neuhauser HK, Ellert U. Prävalenz des metabolischen Syndroms in Deutschland: eine Sensitivitätsanalyse. gms german medical science. 2005 Meeting abstract, http://www.egms.de/en/meetings/gmds2005/05gmds183.shtml. [Google Scholar]
- 7.Moebus S, Hanisch J, Aidelsburger P, Bramlage P, Wasem J, Jöckel KH. Impact of 4 different definitions used for the assessment of the prevalence of the Metabolic Syndrome in primary healthcare: The German Metabolic and Cardiovascular Risk Project (GEMCAS) Cardiovascular Diabetology. 2007;6 doi: 10.1186/1475-2840-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moebus S, Hanisch J, Neuhaeuser M, Aidelsburger P, Wasem J, Joeckel K-H. Assessing the prevalence of the Metabolic Syndrome according to NCEP ATP III in Germany: feasibility and quality aspects of a two step approach in 1550 randomly selected primary health care practices. GMS Ger Med Sci. 2006;4 Doc07, http://www.egms.de/en/gms/2006-4/000036.shtml. [PMC free article] [PubMed] [Google Scholar]
- 9.Deutsche Arbeitsgemeinschaft für Epidemiologie. Leitlinien und Empfehlungen zur Sicherung von Guter Epidemiologischer Praxis (GEP) http://www.gesundheitsforschung-bmbf.de/_media/Empfehlungen_GEP.pdf. 2004. [DOI] [PubMed]
- 10.Kohler E, Ziese T. Telefonischer Gesundheitssurvey des Robert Koch-Instituts zu chronischen Krankheiten und ihren Bedingungen. Berlin: Robert Koch-Institut; 2004. [Google Scholar]
- 11.Hauner H, Hanisch J, Bramlage P, Steinhagen-Thiessen E, Schunkert H, Jöckel KH, Wasem J, Moebus S. Prevalence of undiagnosed type-2-diabetes mellitus and impaired fasting glucose in german primary care: data from the German Metabolic and Cardiovascular Risk Project (GEMCAS) Experimental and Clinical Endocrinology & Diabetes. 2008;1:18–25. doi: 10.1055/s-2007-985359. [DOI] [PubMed] [Google Scholar]
- 12.Grundy S, Brewer H, Cleeman J, Smith S, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association. Circulation. 2004;109:433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 13.Statistisches Bundesamt. Statistisches Jahrbuch für die Bundesrepublik Deutschland 2006. Wiesbaden: Statistisches Bundesamt; 2006. https//www-ec.destatis.de. [Google Scholar]
- 14.Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 15.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 16.Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in korean men and women. N Engl J Med. 2006;355:779–787. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 17.Hauner H. Gesundheitsrisiken von Übergewicht und Gewichtszunahme. Dtsch Arztebl. 1996;93(51-52):A 3405–A 3409. [Google Scholar]
- 18.Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA. Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol. 2002;156:1070–1077. doi: 10.1093/aje/kwf145. [DOI] [PubMed] [Google Scholar]
- 19.Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio Heart Study. Diabetes Care. 2003;26:3153–3159. doi: 10.2337/diacare.26.11.3153. [DOI] [PubMed] [Google Scholar]
- 20.Moebus S, Stang A. Das metabolische Syndrom - ein umstrittenes diagnostisches Konzept. Herz. 2007;32:529–540. doi: 10.1007/s00059-007-3025-9. [DOI] [PubMed] [Google Scholar]
- 21.Keil U, Liese AD, Hense HW, et al. Classical risk factors and their impact on incident non-fatal and fatal myocardial infarction and all-cause mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984-1992. Monitoring trends and determinants in cardiovascular diseases. Eur Heart J. 1998;19:1197–1207. doi: 10.1053/euhj.1998.1089. [DOI] [PubMed] [Google Scholar]
- 22.John U, Greiner B, Hensel E, Lüdermann J, Piek M, Sauer S, et al. Study of health in pomerania (SHIP): a health examination survey in an east German region: objectives and design. Soz Präventivmed. 2001;46:186–194. doi: 10.1007/BF01324255. [DOI] [PubMed] [Google Scholar]
- 23.Greiser K, Kluttig A, Schumann B, Kors J, Swenne C, Kuss O, et al. Cardiovascular disease, risk factors and heart rate variability in the elderly general population: Design and objectives of the CARdiovascular disease, Living and Aging in Halle (CARLA) Study. BMC Cardiovascular Disorders. 2005;5 doi: 10.1186/1471-2261-5-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmermund A, Möhlenkamp S, Stang A, Grönemeyer D, Seibel R, Hirche H, et al. Assessment of clinically silent atherosclerotic disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: rationale and design of the Heinz Nixdorf Recall Study. Risk factors, evaluation of coronary calcium and lifestyle. Am Heart J. 2002;144:212–218. doi: 10.1067/mhj.2002.123579. [DOI] [PubMed] [Google Scholar]
- 25.Alberti KG, Zimmet P, Shaw J IDF Epidemiology Task Force Consensus Group. The metabolic syndrome - a new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]