Abstract
Introduction
Vertigo is not a separate disease process, but a multisensory and sensorimotor syndrome with various etiologies and pathogeneses. It is among the commonest symptoms presented to doctors, with a lifetime prevalence of around 20% to 30%. Patients have often consulted multiple physicians before a diagnosis is made and therapy initiated.
Methods
Selective literature research and review of the guidelines of the German Neurological Society.
Results
A careful history remains the cornerstone of diagnosis. Once the correct diagnosis is made, specific and effective treatments are available for most peripheral, central, and psychogenic forms of dizziness. Treatment may include medication, physiotherapy, and psychotherapy; a few limited cases may require surgical treatment. The treatment of choice for acute vestibular neuritis is the administration of corticosteroids. Menière’s disease is treated with high-dose, long-term betahistine. A new approach to the management of downbeat and upbeat nystagmus, and of episodic ataxia type 2, involves the use of aminopyridines as potassium-channel blockers. Close multidisciplinary cooperation is essential in dizziness, and further multicenter studies are needed.
Keywords: presenting complaint, vestibular disorder, vertigo, dizziness, Menière’s disease, migraine
The term "dizziness" refers either to an unpleasant disturbance of spatial orientation or to the erroneous perception of movement, which is more specifically called "vertigo." Vertigo involves a perceived movement either of one’s own body, such as swaying or rotation, or of the environment, or both. Alongside headache, dizziness and vertigo are among the more common symptoms with which patients present to physicians in general, not just to neurologists. Their lifetime prevalence is approximately 20% to 30% (1). Experience has shown that the affected persons often make an odyssey of visits to physicians belonging to various specialties, beginning with their family physicians and proceeding through ENT specialists, neurologists, ophthalmologists, internists, and orthopedists, before the correct diagnosis is made and the appropriate treatment is begun. In other words, these patients often fall into the cracks between medical specialties.
A patient’s complaint of "dizziness" necessitates the taking of a thorough history precisely because of the many different meanings this term can have. Ancillary testing is of secondary importance. The relative frequencies of various syndromes presenting with dizziness and vertigo are listed in table 1. The important criteria for distinguishing among them are as follows (2):
Table 1. The relative frequencies of different dizziness and vertigo syndromes.
| Diagnosis | Number of patients | Percent |
| Benign paroxysmal positioning vertigo | 1336 | 18.6 |
| Phobic postural vertigo | 1127 | 15.6 |
| Central vestibular vertigo | 893 | 12.4 |
| Basilar/vestibular migraine | 738 | 10.2 |
| Menière’s disease | 677 | 9.4 |
| Vestibular neuritis | 531 | 7.4 |
| Bilateral vestibulopathy | 367 | 5.1 |
| Vestibular paroxysmia | 284 | 3.9 |
| Psychogenic dizziness | 228 | 3.2 |
| Perilymph fistula | 44 | 0.6 |
| Dizziness syndromes of unclear etiology | 239 | 3.3 |
| Other | 741 | 10.3 |
| Overall | 7205 |
The type of dizziness/vertigo: rotatory vertigo resembles the sensation of being on a merry-go-round (in vestibular neuritis and other disorders), while postural vertigo resembles the sensation of riding in a boat (e.g., in bilateral vestibulopathy). Many patients use the term "dizziness" for lightheadedness without any sensation of movement (e.g., in drug intoxication).
The duration of dizziness/vertigo: attacks may last for seconds or minutes (as in vestibular paroxysm) or hours (as in Menière’s disease or vestibular migraine). Persistent vertigo lasting days or weeks is seen in vestibular neuritis, among other conditions. Attacks of postural vertigo lasting minutes to hours can be produced, for example, by brainstem transient ischemic attacks.
Precipitating and exacerbating factors of dizziness and vertigo: the symptoms arise at rest in some conditions (e.g., vestibular neuritis); they can also arise when the patient walks (as in bilateral vestibulopathy) or be induced by turning the head to the right or left (as in vestibular paroxysm). Other possible precipitating factors include turning in bed (as in benign paroxysmal positioning vertigo [BPPV]), coughing, pressing, and loud tones of a particular frequency (Tullio’s phenomenon, seen in perilymph fistula), as well as certain social or environmental conditions (e.g., phobic postural vertigo).
The accompanying symptoms, if present, may arise from the inner ear – e.g., attacks of intense tinnitus, hearing impairment, and a pressure sensation in the ear, which are typical of Menière’s disease. Diplopia, sensory disturbances, dysphagia, dysarthria, and paralysis of arms and legs are symptoms of central origin that usually arise in the brainstem. Headache or a history of migraine may point to the diagnosis of vestibular migraine but can also be caused by brainstem ischemia or posterior fossa hemorrhage.
General principles of treatment
The treatment of dizziness and vertigo (2) may include medication, physical therapy, and psychotherapy; a few limited cases may require surgical treatment. Before the treatment is begun, the patient should be told that the prognosis is generally good: many of these conditions have a favorable spontaneous course, both because peripheral vestibular dysfunction tends to improve and because there is central vestibular compensation for asymmetrical peripheral vestibular tone. Moreover, most of these conditions can be treated successfully.
In this review article, the authors summarize the diagnosis and treatment of dizziness, vertigo, and dysequilibrium. The information presented here was drawn from a selective review of the literature and from the guidelines of the German Neurological Society.
The common types of dizziness and vertigo and their treatment
Peripheral vestibular vertigo
A functional classification of peripheral vestibular disorders divides them into three main types, which can be distinguished on the basis of their typical symptoms and signs (table 2):
Table 2. The presenting manifestations and causes of peripheral vestibular types of vertigo.
| Type of disorder | Presenting manifestations | Examples and causes |
|---|---|---|
| Chronic, bilateral peripheral vestibular dysfunction | Oscillopsia on head movement (loss of the vestibulo-ocular reflex) Unsteadiness of stance and gait, worsening in darkness and on uneven ground (because of the partial or total removal of visual or somatosensory cues) Impairment of spatial memory | Bilateral vestibulopathy due to (e.g.):
|
| Acute/subacute unilateral vestibular dysfunction (labyrinth and/or vestibular nerve) with asymmetrical vestibular tone | Rotatory vertigo (lasting a few days to weeks) Oscillopsia due to spontaneous nystagmus Tendency to fall to a particular side Nausea | Vestibular neuritis due to reactivation of a latent herpes simplex virus type 1 infection |
| Inappropriate unilateral paroxysmal excitation or loss of function of the peripheral vestibular system | Attacks of rotational or swaying vertigo that (depending on their cause) may or may not be externally precipitated, are of varying duration, and are accompanied by various other symptoms | Benign peripheral paroxysmal positioning vertigo due to canalolilthiasis Menière’s disease due to rupture of the endolymphatic membrane Vestibular paroxysm due to neurovascular contact |
Chronic, bilateral dysfunction of the vestibular nerve or the peripheral vestibular organs;
Acute, unilateral vestibular dysfunction;
Paroxysmal pathological excitation or inhibition of the vestibular nerve or vestibular organs.
In the following sections, we will present the characteristic history, clinical findings, and treatment of these three common types of peripheral vestibular vertigo.
Benign paroxysmal positioning vertigo (BPPV)
This is the most common type of vertigo; it mainly affects older patients (table 1) and has a lifetime prevalence of 2.4% (1). It is characterized by brief attacks of rotational vertigo, accompanied by vertical positioning nystagmus that rotates toward the lower of the two ears and beats toward the forehead. The attacks are precipitated by reclination of the head, or by lateral positioning of the head or body, with the affected ear downward. After a change in position of one of these types, rotational vertigo and nystagmus arise after a latency of a few seconds and then take a characteristic crescendo-decrescendo course, lasting a total of 30 to 60 seconds. The nystagmus corresponds to a so-called ampullofugal excitation of the affected posterior vertical semicircular canal of the affected (lower) ear.
More than 90% of cases are idiopathic; the remaining, symptomatic cases are most commonly due to head trauma, vestibular neuritis, or Menière’s disease (3). BPPV also arises with greater than usual frequency after prolonged bed rest necessitated by other diseases, or after surgery. BPPV of the horizontal semicircular canal is rare and is precipitated by rotation of the head in the recumbent position. BPPV is called "benign" because it usually resolves spontaneously within a few weeks or months; in some cases, however, it can last for years. If left untreated, it persists in about 30% of patients.
The canalolithiasis hypothesis explains all of the manifestations of positioning vertigo and nystagmus (4). According to this hypothesis, the condition is due to the presence of agglomerates of many otoconia that nearly fill the lumen of the semicircular canal and are freely mobile within it, instead of the small pieces of particulate matter that adhere firmly to the cupula (so-called cupulolithiasis).
BPPV is treated with positioning maneuvers: rapid repositioning of the head can move the otoconial agglomerate out of the semicircular canal so that it can no longer cause positioning vertigo. The treatments of choice are the Semont (5) and Epley maneuvers. For the Semont maneuver, see figure 1; the Epley maneuver involves rotation of the patient in the recumbent position with the head hanging down. Most patients can perform these maneuvers themselves after brief training. The two are equally effective, and the cure rate is more than 95% within a few days, as shown by multiple controlled studies and meta-analyses (6). The rate of recurrence of BPPV is about 15% to 30% per year. The symptoms eventually recur at some time after effective treatment in about 50% of patients (7) but can then be treated effectively a second time in the same manner.
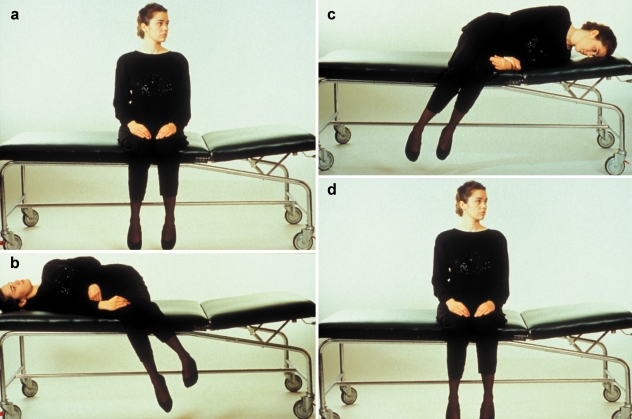
Figure 1.
Figure 1: The treatment of benign paroxysmal positioning vertigo (BPPV) with the Semont maneuver. The illustration shows the treatment of BPPV due to canalolithiasis of the right posterior semicircular canal.
a) In the initial, sitting position, the head is turned 45° to the side of the unaffected ("healthy") ear.
b) The patient is laid on the right side, i.e., on the side of the affected ear, while the head is kept in 45° of rotation to the other side. This induces movement of the particulate matter in the posterior semicircular canal by gravity, leading to rotatory nystagmus toward the lower ear that extinguishes after a brief interval. The patient should maintain this position for about one minute.
c) While the head is still kept in 45° of rotation toward the side of the healthy ear, the patient is rapidly swung over to the side of the unaffected ear, so that the nose now points downward. The particulate matter in the semicircular canal now moves toward the exit from the canal. This position, too, should be maintained for at least one minute.
d) The patient returns slowly to the initial, sitting position. The particulate matter settles in the utricular space, where it can no longer induce rotatory vertigo. This sequence (a-d) should be performed three times in a row three times per day, in the morning, at noon, and at night. Most patients are free of symptoms after doing this for three days.
Vestibular neuritis
The clinical syndrome of vestibular neuritis is characterized by the following (figure 2):
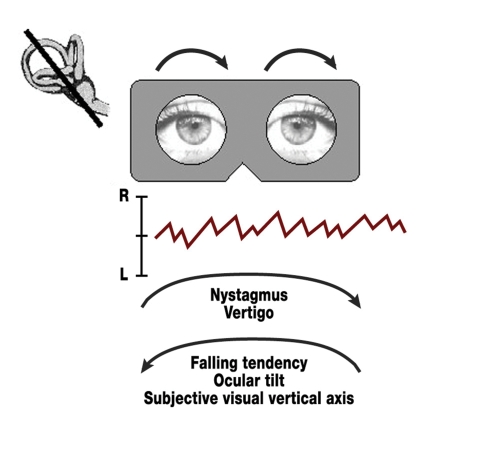
Figure 2.
The symptoms and clinical findings in right vestibular neuritis.
The rotatory vertigo often arises acutely and lasts from several days to a few weeks. Clinical examination is performed with Frenzel’s goggles that are lit from within and contain magnifying lenses (+16 diopters). These goggles prevent the suppression of spontaneous nystagmus by visual fixation and make the patient’s eye movements easier to observe. Spontaneous nystagmus away from the affected side is seen, along with a falling tendency, ocular tilt, and deviation of the subjective visual vertical axis toward the affected side.
Persistent rotational vertigo with a pathological inclination of the visual vertical axis toward the side of the affected labyrinth
Spontaneous, horizontally rotating nystagmus toward the unaffected side, producing apparent movement of the environment ("oscillopsia")
Gait deviation and falling tendency toward the affected side
Nausea and vomiting
Unilateral dysfunction of the horizontal semicircular canal, as revealed by the Halmagyi-Curthoys head impulse test (8) for the function of the vestibulo-ocular reflex, as well as by caloric testing.
A viral and/or autoimmune etiology for vestibular neuritis is probable but has not yet been proven. Autopsy studies have revealed inflammatory degeneration of the vestibular nerve, the presence of viral DNA from herpes simplex virus type I, and the so-called "latency-associated transcript" (LAT) in vestibular ganglion cells (9). The treatment is symptomatic, causal, and physiotherapeutic:
Symptomatic treatment: antivertiginous medications, such as 100 to 300 mg of dimenhydrinate, should be given only in the first three days and only if necessary to treat severe nausea and vomiting, because they delay the development of central compensation mechanisms.
"Causal" treatment: a four-armed, placebo-controlled trial was performed, based on the assumption that vestibular neuritis is caused by the reactivation of a latent herpes simplex virus type 1 infection. The trial revealed that monotherapy with a glucocorticoid-methylprednisolone at an initial dose of 100 mg daily, reduced in 20-mg steps every four days, significantly improved the recovery of peripheral vestibular function. The administration of valacyclovir alone had no effect, nor did its administration in combination with the glucocorticoid have any additional effect (10).
Physical therapy: a further principle of treatment is the promotion of central compensation by physical therapy. Equilibrium training significantly lessens the time required for vestibulospinal compensation and postural regulation to develop (11). Voluntary eye movements and fixation are exercised in order to improve impaired visual fixation; furthermore, active head movements are exercised to realign the vestibular reflex, as well as balance tasks, goal-directed movements, and Q
Menière’s disease
This condition is probably due to labyrinthine endolymphatic hydrops with periodic rupturing of the membrane that separates the endolymphatic and perilymphatic spaces. These ruptures precipitate the paroxysmal attacks that last a few minutes to hours (12). The ultimate etiology is impaired resorption in the endolymphatic sac due to perisaccular fibrosis or to obliteration of the endolymphatic duct. Attacks are produced when rupture of the endolymphatic tube causes calcium-induced depolarization of the vestibulocochlear nerve. A classic Menière’s attack consists of rotatory vertigo, tinnitus, hearing impairment, and pressure sensation in one ear. The lifetime prevalence of this condition is approximately 0.5% (1). It usually begins on one side, and the frequency of attacks is highly variable. Menière’s disease becomes bilateral in 50% of cases (13) and is the second most common cause of bilateral vestibulopathy.
Its treatment is based on two principles:
Treatment of individual attacks: vertigo and nausea can be improved with antivertiginous medications just as in the treatment of other types of acute labyrinthine dysfunction. For example, 100 mg dimenhydrate suppositories can be used.
Attack prophylaxis: this type of treatment is aimed at improving the underlying endolymphatic hydrops. Despite the high prevalence of Menière’s disease and the large number of clinical studies that have been performed, there is still no treatment of this type that has been conclusively shown to be effective. The spectrum of recommendations ranges from a sodium-free diet to diuretics, transtympanic gentamicin instillation (20 to 40 mg given repeatedly, at intervals of several weeks, until symptoms improve), betahistine, and surgical procedures (12). A beneficial effect on the frequency of attacks has been reported for transtympanic gentamicin (6) and for the prolonged high-dose administration of betahistine hydrochloride (48 mg tid for 12 months). The latter dose of betahistine hydrochloride is currently recommended on the basis of a recently reported observational treatment study in 112 patients who were treated for at least 12 months at doses of 16, 24, or 48 mg tid (14). The highest dose led to a statistically significantly greater reduction of attack frequency and was well tolerated. These findings provided the motivation for a multicenter, controlled dose-finding study that is currently in progress (EudraCT number 2005-000752-32; BMBF177zfyGT).
Central vestibular syndromes
Central vestibular syndromes are mainly caused by lesions of the vestibular pathways, which arise in the vestibular nuclei in the caudal portion of the brainstem and proceed to the cerebellum, thalamus, and vestibular cortex, or by damage to the vestibulocerebellum. Pathological excitation is a rare cause, as occurs, for example, in the paroxysmal brainstem attacks with ataxia that can be produced by multiple sclerosis or vestibular epilepsy. The common causes of central vestibular vertigo include vestibular migraine and ischemic lesions in the brainstem. Furthermore, central vestibular disturbances arise in the setting of certain ocular motor disorders such as downbeat and upbeat nystagmus, as attacks in episodic ataxia type 2, and in vestibular migraine. These individual disorders, and the treatment of each, will be discussed in the following sections.
Downbeat and upbeat nystagmus
Two types of vertically beating central nystagmus are of special importance: downbeat nystagmus (DBN) and upbeat nystagmus (UBN), each named after the direction of the rapid, beating phase. DBN is the most common type of acquired, persistent nystagmus (15). Both types manifest themselves above all with swaying nystagmus and unsteadiness of gait and only secondarily with oscillopsia, i.e., apparent movement of the environment due to oscillation of the retinal image. In distinction to spontaneous nystagmus such as in vestibular neurits, DBN and UBN are types of fixation nystagmus, i.e., their intensity increases with visual fixation. Both DBN and UBN always indicate the presence of a central disturbance and possess special localizing significance. DBN is usually due to bilateral dysfunction of the flocculus (16); its three common causes are cerebellar atrophy, ischemia, and Arnold-Chiari malformation (15). UBN – which, unlike DBN, generally persists for no more than a few weeks – can be caused by paramedian medullary or pontomesenchephalic lesions, e.g., brainstem infarct or hemorrhage.
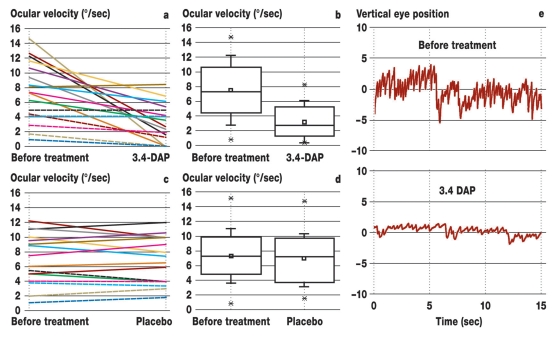
A randomized, placebo-controlled study of DBN has shown that the potassium-channel blockers 3,4-diaminopyridine (17) (figure 3) and 4-aminopyridine can significantly improve this type of nystagmus (18). The dosage is 5 to 10 mg tid; follow-up ECG is necessary. The effectiveness of this treatment has since been confirmed by multiple studies. 4-Aminopyridine seems to be effective against UBN as well, but this has been documented to date only in a single case study (20).
Figure 3.
Mean peak slow phase velocities (PSPV) of DBN measured by 2-D recordings of eye movements. The two graphs on the left show the original data of mean PSVP of each subject: (a) Control versus 3,4-DAP, (c) control versus placebo. The two graphs in the middle give the box plot charts with the mean, median, and the 50% percentile as well as the range for control versus 3,4-DAP (b) and control versus placebo (d). 3,4-DAP reduced mean PSPV of DBN from 7.2 ± 4.2 deg/s (mean ± SD) before treatment to 3.1 ± 2.5 deg/s 30 min after ingestion of the 3,4-DAP (n = 17, p < 0.001, two-way ANOVA). The inset (e) shows an original recording of the vertical eye position before (upper trace) and 30 min after ingestion of the drug (lower trace).
From: Strupp M, Schuler O, Krafczyk A, Jahn K, Schautzer F, Buttner U, Brandt T: Treatment of downbeat nystagmus with 3,4-diaminopyridine: a placebo-controlled study. Neurology 2003; 61: 165-70, with the kind permission of Lippincott Williams and Wilkins.
Episodic ataxia type 2
The familial episodic ataxias are rare genetic diseases of autosomal dominant transmission. There are at least two well-defined varieties. Type 2 (EA 2) is characterized by recurrent attacks of dizziness and ataxia that are precipitated by physical activity, stress, or alcohol and usually last for hours. In between attacks, more than 90% of patients have marked central ocular motor disturbances, often DBN. EA 2 is caused by mutations in the CACNA1A gene (PQ calcium channel gene). Most patients can be treated successfully with acetazolamide. If this treatment is ineffective, or if adverse effects such as kidney stones develop, patients with EA 2 can also be treated with 4-aminopyridine (5 mg tid) (21).
Aminopyridines are thus an effective treatment for DBN, UBN, and EA 2 which is well tolerated at the low dose that is generally used. These studies have also led to the development of a new principle of treatment; activation of cerebellar Purkinje cells through potassium-channel blockade enhances the cerebellar inhibitory influence on the vestibular and cerebellar nuclei.
Vestibular migraine or migraine with vestibular aura
Vestibular migraine is characterized by recurrent attacks that last minutes to hours and usually consist of rotatory vertigo (22, 23). It is the most common cause of spontaneously occurring attacks of vertigo (table 1). Its lifetime prevalence is 0.98% (1). In more than 60% of patients, these attacks are associated with headache and/or photophobia or phonophobia; the remaining patients have attacks of vertigo alone. Most patients also have migraine attacks with or without an aura; this fact makes the condition easier to diagnose. In some patients, the diagnosis can be made only on the basis of a positive response to the treatment of the individual attacks with medication and to pharmacological prophylaxis. The prophylactic treatment of vestibular migraine is analogous to that of migraine with aura and consists of the administration of beta-blockers, valproic acid, and topiramate. No randomized, controlled studies on the efficacy of medications for vestibular migraine have yet been published.
Phobic postural vertigo
Phobic postural vertigo is the second most common diagnosis in a specialized neurological ambulatory clinic for dizziness and vertigo. This disorder is not found in the diagnostic repertoire of most neurologists and ENT specialists. Patients with phobic postural vertigo usually complain of swaying vertigo, lightheadedness, and gait unsteadiness that are continually present but fluctuate in severity. These symptoms are often accompanied by anxiety and are situationally dependent. The precipitating factor may be the presence of a large crowd, or waiting in the check-out line at a store; often, avoidance behavior results (2). The symptoms typically improve when the patient participates in sports or has had a small amount of alcohol to drink. The affected patients often have an obsessive-compulsive personality, in the sense of "accentuated" personality traits, with a marked tendency toward introspection and a need to "have everything under control." The central problem in phobic postural vertigo is the patient’s attempt to establish conscious control over body equilibrium, which leads to a "spiral of self-observation." When this happens, the body’s own movements may be perceived as movements of the outside world. The main features of this disorder and its treatment are summarized in the box. The clinical neurological examination and ancillary tests reveal no relevant pathological findings.
Box. Phobic postural vertigo: the second most common cause of vertigo.
Clinical features
The patient has postural vertigo with unsteadiness of stance and gait; the neurological examination and ancillary tests are generally unremarkable
Fluctuating unsteadiness of stance and gait with attacks of fear of falling, but without an actual fall
Anxiety and autonomic disturbances sometimes occur during or just after the attacks
The attacks are precipitated or exacerbated by typical situations, e.g., crowds, empty spaces, driving
The symptoms often improve during sporting activity or after the consumption of a small amount of alcohol
Increasingly severe avoidance behavior is common
The patient’s personality is usually of an obsessive-compulsive or reactive-depressive type. At the onset of the disorder, there is often a vestibular disturbance (25%) or a situation giving rise to particular stress (70%).
Treatment
A thorough diagnostic assessment to allay the patient’s fear of having a serious organic disease
Psycho-educative therapy to inform the patient about the pathological mechanism and the precipitating factors and situations
Desensitization by self-exposure, i.e., the deliberate seeking out of situations that precipitate vertigo. Light sporting activities are also helpful.
If the symptoms persist, pharmacotherapy, e.g., with selective serotonin reuptake inhibitors, and/or cognitive behavioral therapy are indicated
Treatment markedly improves symptoms in about 70% of patients (25)
These patients can be treated with three or four of the following measures: A thorough diagnostic assessment serves to reassure the patient that the symptoms are not caused by an organic disorder. Psycho-educative explanation informs the patient about the underlying mechanism of excessive self-observation. Desensitization can be performed by repeated exposure to the precipitating situation(s) and by regular participation in sports; these activities strengthen the patient’s confidence in his or her own balancing ability. Finally, if the symptoms persist, pharmacotherapy with a selective serotonin reuptake inhibitor and/or cognitive behavioral therapy can be initiated (24). Combined therapy according to this approach leads to marked improvement in more than 70% of patients, even if the disorder has been present for many years (25).
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Professor Strupp has received lecture fees from the following companies in Germany: Solvay Pharmaceuticals (Hanover), Hennig-Pharma (Flörsheim), Schwarz Pharma (Monheim), and Serono (Unterschleissheim). Professor Brandt has received lecture fees from Solvay Pharmaceuticals (Hanover).
References
- 1.Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol. 2007;20:40–46. doi: 10.1097/WCO.0b013e328013f432. [DOI] [PubMed] [Google Scholar]
- 2.Brandt T, Dieterich M, Strupp M. Vertigo - Leitsymptom Schwindel. Darmstadt: Steinkopff; 2003. [Google Scholar]
- 3.Karlberg M, Hall K, Quickert N, Hinson J, Halmagyi GM. What inner ear diseases cause benign paroxysmal positional vertigo? Acta Otolaryngol. 2000;120:380–385. doi: 10.1080/000164800750000603. [DOI] [PubMed] [Google Scholar]
- 4.Brandt T, Steddin S. Current view of the mechanism of benign paroxysmal positioning vertigo: cupulolithiasis or canalolithiasis? J Vestib Res. 1993;3:373–382. [PubMed] [Google Scholar]
- 5.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290–293. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 6.Strupp M, Cnyrim C, Brandt T. Vertigo and dizziness: Treatment of benign paroxysmal positioning vertigo, vestibular neuritis and Menère’s disease. In: Candelise L, editor. Evidence-based Neurology - management of neurological disorders. Oxford: Blackwell Publishing; 2007. pp. 59–69. [Google Scholar]
- 7.Brandt T, Huppert D, Hecht J, Karch C, Strupp M. Benign paroxysmal positioning vertigo: a long-term follow-up (6-17 years) of 125 patients. Acta Otolaryngol. 2006;126:160–163. doi: 10.1080/00016480500280140. [DOI] [PubMed] [Google Scholar]
- 8.Halmagyi GM, Curthoys IS. A clinical sign of canal paresis. Arch Neurol. 1988;45:737–739. doi: 10.1001/archneur.1988.00520310043015. [DOI] [PubMed] [Google Scholar]
- 9.Theil D, Arbusow V, Derfuss T, et al. Prevalence of HSV-1 LAT in human trigeminal, geniculate, and vestibular ganglia and its implication for cranial nerve syndromes. Brain Pathol. 2001;11:408–413. doi: 10.1111/j.1750-3639.2001.tb00408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strupp M, Zingler VC, Arbusow V, et al. Methylprednisolone, valacyclovir, or the combination for vestibular neuritis. N Engl J Med. 2004;351:354–361. doi: 10.1056/NEJMoa033280. [DOI] [PubMed] [Google Scholar]
- 11.Strupp M, Arbusow V, Maag KP, Gall C, Brandt T. Vestibular exercises improve central vestibulospinal compensation after vestibular neuritis. Neurology. 1998;51:838–844. doi: 10.1212/wnl.51.3.838. [DOI] [PubMed] [Google Scholar]
- 12.Minor LB, Schessel DA, Carey JP. Meniere’s disease. Curr Opin Neurol. 2004;17:9–16. doi: 10.1097/00019052-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Takumida M, Kakigi A, Takeda T, Anniko M. Meniere’s disease: a long-term follow-up study of bilateral hearing levels. Acta Otolaryngol. 2006;126:921–925. doi: 10.1080/00016480500535204. [DOI] [PubMed] [Google Scholar]
- 14.Strupp M, Huppert D, Frenzel C, Wagner J, Zingler VC, Mansmann U, Brandt T. Long-term prophylactic treatment of attacks of vertigo in Menière’s disease-comparison of a high with a low dosage of betahistine in an open trial. Acta Otolaryngol (Stockh) 2008 doi: 10.1080/00016480701724912. In press. [DOI] [PubMed] [Google Scholar]
- 15.Wagner JN, Glaser M, Brandt T, Strupp M. Downbeat nystagmus: Aetiology and comorbidity in 117 patients. J Neurol Neurosurg Psychiatry. 2007 Sep 14; doi: 10.1136/jnnp.2007.126284. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 16.Kalla R, Deutschlander A, Hufner K, et al. Detection of floccular hypometabolism in downbeat nystagmus by fMRI. Neurology. 2006;66:281–283. doi: 10.1212/01.wnl.0000194242.28018.d9. [DOI] [PubMed] [Google Scholar]
- 17.Strupp M, Schuler O, Krafczyk S, et al. Treatment of downbeat nystagmus with 3,4-diaminopyridine: a placebo-controlled study. Neurology. 2003;61:165–170. doi: 10.1212/01.wnl.0000078893.41040.56. [DOI] [PubMed] [Google Scholar]
- 18.Kalla R, Glasauer S, Buttner U, Brandt T, Strupp M. 4-Aminopyridine restores vertical and horizontal neural integrator function in downbeat nystagmus. Brain. 2007;130:2441–2451. doi: 10.1093/brain/awm172. [DOI] [PubMed] [Google Scholar]
- 19.Sprenger A, Rambold H, Sander T, et al. Treatment of the gravity dependence of downbeat nystagmus with 3,4-diaminopyridine. Neurology. 2006;67:905–907. doi: 10.1212/01.wnl.0000233829.76150.6b. [DOI] [PubMed] [Google Scholar]
- 20.Glasauer S, Kalla R, Buttner U, Strupp M, Brandt T. 4-aminopyridine restores visual ocular motor function in upbeat nystagmus. J Neurol Neurosurg Psychiatry. 2005;76:451–453. doi: 10.1136/jnnp.2004.045716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strupp M, Kalla R, Dichgans M, Freilinger T, Glasauer S, Brandt T. Treatment of episodic ataxia type 2 with the potassium channel blocker 4-aminopyridine. Neurology. 2004;62:1623–1625. doi: 10.1212/01.wnl.0000125691.74109.53. [DOI] [PubMed] [Google Scholar]
- 22.Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology. 2001;56:436–441. doi: 10.1212/wnl.56.4.436. [DOI] [PubMed] [Google Scholar]
- 23.Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol. 1999;246:883–892. doi: 10.1007/s004150050478. [DOI] [PubMed] [Google Scholar]
- 24.Holmberg J, Karlberg M, Harlacher U, Magnusson M. One-year follow-up of cognitive behavioral therapy for phobic postural vertigo. J Neurol. 2007;254:1189–1192. doi: 10.1007/s00415-007-0499-6. [DOI] [PubMed] [Google Scholar]
- 25.Huppert D, Strupp M, Rettinger N, Hecht J, Brandt T. Phobic postural vertigo-a long-term follow-up (5 to 15 years) of 106 patients. J Neurol. 2005;252:564–569. doi: 10.1007/s00415-005-0699-x. [DOI] [PubMed] [Google Scholar]