Abstract
Introduction
Retinal venous and arterial occlusions are common causes of visual loss. Depending on the location and extent, symptoms may vary from very discrete impairments to complete loss of sight.
Methods
Selective literature review including the authors’ own research data with a particular focus on interdisciplinary aspects.
Results
Retinal vascular occlusions are not a uniform entity. Rather, they reflect the whole breadth of vascular disease. In arterial occlusion, embolic phenomena and Horton’s arteritis should be excluded, in addition to local ophthalmological investigations. In retinal venous occlusion, optimal treatment of arterial hypertension is universally useful, while investigations for thrombophilia are useful in patients under 50 years of age. The results of intravitreal injection of corticosteroids and vascular endothelial growth factor inhibitors appear encouraging in treatment of macular edema secondary to retinal vein occlusion.
Discussion
While local diagnostic and therapeutic measures are performed by ophthalmologists, there is an important role for interdisciplinary cooperation in the investigation and systemic treatment of these events.
Keywords: ophthalmology, visual impairment, retinal vascular occlusion, venous occlusion, arterial occlusion
Vascular occlusions of the retina and their sequelae in the eye are a common cause of visual impairment (1, 2). Fundamentally, arterial occlusions have to be distinguished from venous occlusions, but mixed forms exist. The prognosis mainly depends on the location, extent, duration, and intensity of retinal ischemia.
Retinal vascular occlusions mostly have systemic causes, whose diagnosis and treatment will influence not only the ophthalmological course but also the prognosis quo ad vitam. Interdisciplinary collaboration is of central importance in this setting. The general work-up for underlying cardiovascular disorders, special further investigations such as diagnostic tests for thrombophilia, or acute therapeutic measures such as selective intra-arterial thrombolysis regularly require close cooperation with other disciplines such as internal medicine, neurology, vascular surgery, or interventional radiology. As atherosclerosis has an important role in the development of retinal vascular occlusions, further cardiovascular clarification makes sense, while taking into account the patient’s age and risk factors.
Arterial occlusions
Fundamentally, a distinction has to be made between central retinal artery occlusion and branch retinal artery occlusion. As a rule, sudden, painless, lasting sight impairment occurs. In addition to the loss of, or reduction in, central visual acuity, patients also complain about visual field loss. Depending on which vessel is affected, the entire visual field (central retinal artery) or part of the visual field (branch retinal artery) may be affected. Amaurosis fugax represents a particular scenario, where transient sight impairment occurs subsequent to transient retinal ischemia (central retinal artery) or the head of the optic nerve (posterior ciliary artery) (3). A transition to manifest arterial occlusion is possible. In retinal arterial occlusion as well as in amaurosis fugax, medical and neurological investigations are obligatory. Men are affected twice as often as women by retinal arterial occlusion. The incidence of central retinal artery occlusions is higher than that of branch artery occlusions and is an estimated 0.85/100 000 population (4).
Pathogenesis
Distinction has to be made between arteritic and non-arteritic occlusions. Non-arteritic retinal arterial occlusions are most often caused by emboli (5). Further reasons include thrombosis, vascular narrowing, hemorrhage underneath an atherosclerotic plaque, dissecting aneurysm, vascular spasm, reduced perfusion in circulatory failure, and vasculitis (1). Atherosclerotic stenosis of the carotid artery and disorders of the cardiac wall and heart valves are the most important sources of arterio-arterial embolism (1). 20% of patients with central arterial occlusion have a hemodynamically relevant carotid stenosis (1), and 50% of those affected have changes on the echocardiogram, of whom only 10% will require treatment (6). In younger patients (<45 years of age), cardiac causes are more common. In the group of patients aged <30 years, migraine, trauma, and hormonal changes may contribute to pathogenesis. Among the rarer causes are vasculitis, vascular spasm, and several coagulation disorders.
Further causes of impaired perfusion of the retinal artery include a sudden loss in blood pressure – e.g., at night or due to shock – or reduced perfusion owing to increased intraocular pressure. Acute glaucoma, massive orbital edema, or ophthalmic surgical interventions with compression can result in arterial occlusion in patients with a predisposition.
Horton’s giant cell arteritis (Horton’s disease) is found in only 1% to 4% of cases of central retinal artery occlusion, but it is the most common systemic vasculitis in people older than 50, whose ocular manifestation can cause occlusion of the ophthalmic artery owing to granulomatous inflammation of the arterial wall. Giant cell arteritis also often leads to anterior ischemic optic neuropathy.
Diagnosis
A characteristic feature of central arterial occlusion is acute and painless visual loss in the affected eye. The sudden visual loss is noticed mostly during daytime, and most often in the first half of the day. On the one hand, this is because arterial occlusions can be the result of nocturnal arterial hypotension. Another possible cause is the nocturnal accumulation of occlusive events during the sleep phase.
An afferent pupillary defect – and therefore a conduction impairment in the optic nerve – can be found. Reactiveness to light in the ipsilateral pupil is slower than in the other eye. A typical feature is the "cherry red spot" of the macula lutea, visible on ophthalmoscopy, which is due to the contrast between the choroid that shows through in the area of the fovea centralis and the yellowish edematous retina. The visual field losses are massive. In cases of complete blindness, additional infarction of the choroid can be assumed. In occlusions of the branch artery, acute visual field loss develops in the affected area (figure 1). If the macula lutea is affected by the ischemia this will result in a loss of visual acuity. In a case of an isolated occlusion of a cilioretinal artery, which is present in about a quarter of the population, this may result in a loss of central visual acuity while the peripheral visual field remains.
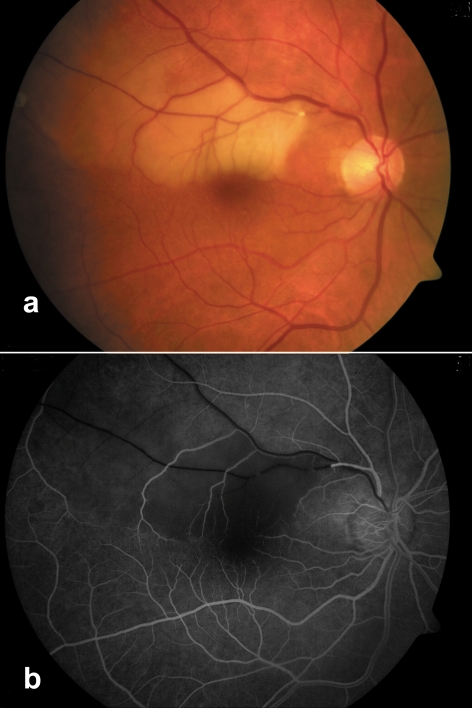
Figure 1.
Occlusion of the superior temporal artery of the retina with visible embolus on
a) funduscopy and
b) fluorescence angiography
Treatment
The therapeutic options that are currently available for arterial retinal occlusion are unsatisfactory. The spontaneous course after central arterial occlusion has been found to be an improvement in visual acuity by two lines in up to 8% of patients (5). Only 8% of patients achieved final visual acuity of 0.1 (20/200) or better without treatment.
Currently, no data exist from prospective randomized studies into the treatment of central arterial occlusion. A meta-analysis of case series thus far has shown that treatment can lead to an improvement in sight in about 15% of cases, compared with the spontaneous disease course. Owing to the lack of studies, no scientific proof for the superiority of any therapeutic option exists, and the options chosen in everyday clinical practice therefore include therapeutic approaches that have as few adverse effects as possible, such as ocular globe massage, lowering of intraocular pressure to improve retinal perfusion, isovolemic hemodilution, or administration of thrombocyte aggregation inhibitors. Often, several of these measures are combined.
Another therapeutic approach is intravenous and selective intra-arterial thrombolysis of the ophthalmic artery. A meta-analysis of the few case reports and case series published so far shows that thrombolysis for acute arterial retinal occlusion probably yields a notable visual improvement in 30% to 40% of cases. However, owing to the lack of prospective randomized studies, these results must be interpreted with extreme caution. From 2002 to 2007, a randomized multicenter study of the European Assessment Group for Lysis in the Eye (EAGLE) was conducted in Germany, Austria, and Switzerland, which compared the efficacy of local intra-arterial thrombolysis with conservative therapeutic approaches (7). Recruitment has been concluded, but the results from this study have not yet been published.
Although the time span during which therapy is actually beneficial after an occlusion event is not known, it is unanimously accepted that rapid administration of treatment is desirable. The therapeutic threshold is reported to be between 6 and 24 hours. Patients with new retinal arterial occlusion should therefore present to an ophthalmologist as soon as possible.
In temporal arteritis, the typical clinical symptoms and the investigation of acute phase reactions including erythrocyte sedimentation rate, C-reactive protein, and fibrinogen are diagnostic indicators; arterial biopsy confirms the diagnosis. Unfortunately, a negative biopsy result does not exclude temporal arteritis, so that in case of doubt therapy should be administered to prevent further vascular occlusions. If temporal arteritis is suspected, prednisolone should be given at a dosage of 1 mg/kg body weight; in patients with inflammation related visual deterioration, oral prednisolone should be given at a dosage of at least 100 mg/day. The steroid dose can be reduced in accordance with the development of the acute phase proteins. It has not been proved that intravenous administration of steroids is superior to oral administration (8).
Ocular sequelae of retinal arterial occlusion will require specific treatment. Panretinal laser coagulation is indicated in case of retinal neovascularization or neovascular secondary glaucoma.
Interdisciplinary work-up
The most common causes of retinal arterial occlusion – embolism and thrombosis – mostly arise as a consequence of systemic illness. The medical examination is therefore of particular importance, with risk stratification to reduce atherosclerotic factors such as hypertension, nicotine use, and hyperlipidemia. A cardiac source of embolism should be ruled out by echocardiogram – transesophageal echocardiogram if required. Long term blood pressure measurement and electrocardiographic control examinations also seem useful. In the context of collaborating with neurologists, Doppler echocardiography of the carotid arteries is highly recommended to exclude this source of embolism. Depending on the results of these investigations, a consultation with a vascular surgeon may be useful. To perform local intra-arterial thrombolysis, which is currently being investigated in the context of studies, cooperation with interventional radiologists is required. At this point, we wish to emphasize the important role of specialists in internal medicine in the treatment of potentially underlying Horton’s arteritis.
Patients with retinal arterial occlusions have a notably shortened life expectancy after the event (e1). In an older study, Lorenzen calculated a mean survival period of 5.5 years, compared with 15.4 years in the comparison group (e2). However, this seems to apply only when the patients’ arterial hypertension was not sufficiently treated with drugs after the initial occlusion (9). This example again highlights the importance of closer interdisciplinary cooperation in the treatment of patients with retinal vascular occlusion.
Venous occlusions
The term "venous occlusion" of the retina is preferable to "thrombosis" because the pathogenesis of venous retinal occlusions is still not fully clear. Dependent on the location of the retinal venous occlusion, events can be classified into central retinal vein occlusion, hemicentral retinal vein occlusion, branch retinal vein occlusion, and macular branch retinal vein occlusion (10). Clinically, the distinction between central vein occlusion and branch vein occlusion is sensible; the latter is more common. A subclassification into ischemic and non-ischemic occlusions is also widely accepted; the degree of ischemia is an indicator for the severity of disease. The distribution of ocular occlusions is shown in table 1. The likelihood of sequelae – e.g., neovascular secondary glaucoma – depends, among others, on this classification and the extent of the occlusion. The decisive factor that influences visual acuity is the development of macular edema as a result of a barrier disruption.
Table 1. Proportional distribution of the most important vascular occlusions in the posterior section of the eye.
| Retinal veins | Central vein | 29% | 64% |
| Branch vein | 35% | ||
| Retinal arteries | Central artery | 10% | 20% |
| Branch artery | 10% | ||
| Optic nerve arterial | Anterior ischemic optic neuropathy | 15% | 15% |
| Ocular globe | Ocular ischemia | 1% | 1% |
Data from a collection of the University Eye Hospital in Aachen. Table drawn up by Prof. Dr. Dr. S. Wolf, Inselspital Bern, Switzerland
The prevalence of venous retinal occlusion is estimated at 0.7% to 1.6% (2). The prevalence and five-year incidence is 0.6% for occlusions of the branch vein and 0.1% and 0.2% for occlusion of the central vein (11). The risk of central vein occlusion in the non-affected eye is 7% within four years (12). Compared with arterial retinal occlusions, much more is known about the treatment of venous retinal occlusions, although only few of the numerous existing studies were randomized.
Pathogenesis
The development of central retinal vein occlusions is a multifactorial event (13). An important component is the compression of the central vein, which runs jointly with the central artery through the central canal of the optic nerve. Artery and vein share an adventitia in this section, which means that if the arterial wall undergoes changes at particularly prone sites the thinner venous wall may be compressed. The result will be impaired blood flow which reacts sensitively to hemodynamic changes such as a fall in blood pressure and low central venous pressure. Atherosclerotic changes to the arterial wall will result in secondary changes to the venous wall because of the increased rigidity. This increases the compression of the central vein, resulting in impaired flow, and thus promotes thrombogenesis.
A further important factor for the development of venous retinal vascular occlusions is an increase in the viscosity of the blood, which is observed in disorders of the hematogenic system or in inflammatory changes. Thrombophilic coagulation disorders are obviously of major importance, especially in younger patients. Associations between thrombophilia and retinal vein occlusions have been described particularly for the resistance against activated protein C (APC resistance), the most common known coagulation disorder. An association between oral contraceptives and the development of central retinal vein occlusion has not been proved conclusively thus far. An ocular risk factor for the development of central retinal vein occlusion is raised intraocular pressure; the risk of central retinal vein occlusion in glaucoma patients is 5-fold to 10-fold increased (14).
Occlusions of the retinal branch vein arise at arteriovenous crossings in more than 99.9% of cases. Similar to the pathogenesis of central retinal vein occlusions, the main pathomechanism can be assumed to be compression of the vein by the artery in the area of the joint section of vascular wall. Atherosclerotic or hypertension related changes are seen as the main causes of compression (10).
Diagnosis
Retinal venous occlusions, especially occlusions of the retinal branch vein, may be asymptomatic – depending on their degree of severity and extent – or be accompanied by visual impairment. This impairment is not as pronounced and does not develop as rapidly as in arterial occlusions. The symptoms often develop over several days. Typically, vision impairment in retinal vein occlusion depends on the time of day and is more pronounced in the morning, which is explained by impaired drainage during rest and in a horizontal position. Occlusions of the retinal branch vein result in visual field defects that are often only noticed by affected patients if the macula is affected. Funduscopy confirms the diagnosis. In central retinal vein occlusion, the typical diagnostic findings are intraretinal, flame-shaped hemorrhages in the entire retinal area, and in retinal branch vein occlusion, these would be found in the affected area of the retina (figure 2). Fluorescence angiography will provide further insights into the degree of ischemia and – if present – the severity of macular edema. Modern, non-invasive procedures – e.g., optical coherence tomography (OCT) – are useful in qualifying the macular edema and in the follow-up (figure 3).
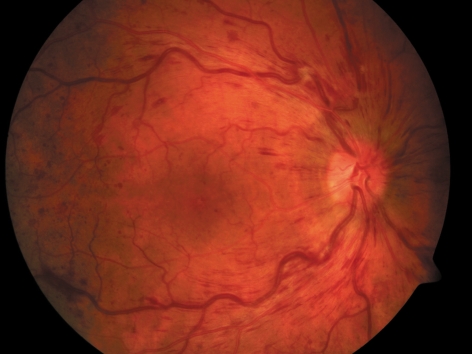
Figure 2.
Clinical image of central venous occlusion with intraretinal hemorrhages, cotton wool spots, congested veins, and macular edema
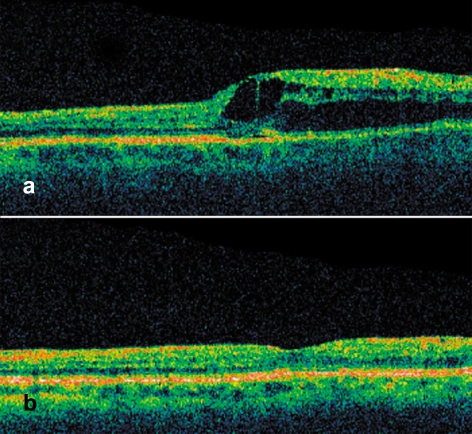
Figure 3.
Optical coherence tomography of macula lutea after branch vein occlusion.
a) Cystoid macular edema before and b) after treatment with intravitreous injection of bevacizumab
Treatment
In contrast to current recommendations for the treatment of thromboses in large vessels, the lack of sufficiently large, reliable studies makes it impossible to provide any recommendation about the use of anticoagulant drugs in the treatment of retinal venous occlusions (15, 16). Similarly, no evidence base exists to date for the administration of thrombocyte aggregation inhibitors (10). Blood viscosity can be reduced by giving pentoxifyllin. A randomized controlled study has shown an improvement in retinal venous blood flow as a result of a therapeutic dosage of 1600 mg pentoxifyllin/day (17). Isovolemic hemodilution is currently the only therapeutic option for retinal venous occlusions whose evidence base is provided by several studies. Simultaneous bloodletting (venesection) and infusion of plasma expanders aim to lower the haematocrite temporarily to 35% to 37% (13, 18, 19). The visual prognosis can thus be improved.
The data situation with respect to systemic thrombolysis is not clearly evidence based. The results of a prospective study published in 1976 – of treatment with streptokinase and systemic anticoagulants – have hinted at efficacy of thrombolysis in acute occlusions of the central retinal vein compared with the natural disease course (e3). This result is consistent with preliminary data of an as yet unpublished randomized controlled study of intravenous thrombolysis with recombinant tissue plasminogen activator (rt-PA) compared with hemodilution. However, the problem inherent in this therapeutic option is the risk of hemorrhage that is associated with systemic thrombolysis.
Current surgical therapeutic options, such as "radial optic neurotomy" in central venous occlusion or "arteriovenous dissection" in retinal branch vein occlusion require further scientific study. A promising new therapeutic option for macular edema as a common sequela of retinal venous occlusions is the injection of medical drugs into the vitreous space, the so-called intravitreal injection. Crystalline corticosteroids – such as triamcinolone – and inhibitors of the vascular endothelial growth factor (VEGF, e.g., bevacizumab), which is of central importance in the development of barrier disruptions and neovascularization in retinal vascular occlusions, have been used with encouraging results (figure 3) (20, 21). However, none of the substances mentioned has been approved for intravitreal administration in this particular indication; the main reason can be assumed to be a lack of interests on the part of the pharmaceutical industry in relevant licensing studies.
If neovascularizations occur as a result of retinal vascular occlusions, thermic laser coagulation of the retina is still the evidence based treatment method of choice. Serious late complications, such as vitreous hemorrhage or retinal detachment, often necessitate surgical intervention (pars plana vitrectomy).
Interdisciplinary work-up
A particular trait of venous occlusions of the retina is their association with atherosclerosis. This underlines the particular importance if interdiscpliniary clarification and treatment. General risk factors of atherosclerosis – such as arterial hypertension, diabetes mellitus, or hyperlipidemia – should be assessed in all patients (table 2). Color duplex sonography of the arteries supplying the brain is not required because patients with venous retinal occlusions have only the age related risk of the general population with regard to carotid stenosis. Long term blood pressure measurement, electrocradiography, and lipid status assessment are the standard investigations. However, it should be mentioned that an Australian study concludes, on the basis of 8384 patients, that venous retinal occlusions are associated with increased cardiovascular mortality only in those aged 70 or younger (hazard ratio 2.5) (22).
Table 2. Summary of tests outside the remit of ophthalmological diagnostics.
| Arterial occlusion | Venous occlusion | |
| Blood pressure control | 24 h | 24 h |
| Echocardiography | Yes | No |
| Electrocardiography | Yes | Yes |
| Color duplex sonography of the carotid artery | Yes | No |
| Doppler sonography of the temporal artery | In suspected Horton’s disease | No |
| General examination of the blood | Yes | Yes |
| Diagnostic tests for thrombophilia | Patients aged under 50 | Patients aged under 50 |
| Imaging (magnetic resonance imaging, magnetic resonance angiography, etc) | Only when suspected for a good reason | Not as a rule |
Investigations for thrombophilia can generally be recommended for younger patients (<50 years), especially in cases where no known vascular risk factors are present (23, 24). Several authors also recommend measuring homocysteine concentrations (25).
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Feltgen N, Schmidt D, Hansen L. Arterielle retinale Verschlüsse. Ophthalmologe. 2003;100:651–665. doi: 10.1007/s00347-003-0845-8. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol. 1996;114:1243–1247. doi: 10.1001/archopht.1996.01100140443012. [DOI] [PubMed] [Google Scholar]
- 3.Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005;24:493–519. doi: 10.1016/j.preteyeres.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Rumelt S, Dorenboim Y, Rehany U. Aggressive systematic treatment for central retinal artery occlusion. Am J Ophthalmol. 1999;128:733–738. doi: 10.1016/s0002-9394(99)00359-1. [DOI] [PubMed] [Google Scholar]
- 5.Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005;140:376–391. doi: 10.1016/j.ajo.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S, Naqvi A, Sharma SM, Cruess AF, Brown GC. Transthoracic echocardiographic findings in patients with acute retinal arterial obstruction. A retrospective review. Retinal Emboli of Cardiac Origin Group. Arch Ophthalmol. 1996;114:1189–1192. doi: 10.1001/archopht.1996.01100140389004. [DOI] [PubMed] [Google Scholar]
- 7.Feltgen N, Neubauer A, Jurklies B, et al. Multicenter study of the European Assessment Group for Lysis in the Eye (EAGLE) for the treatment of central retinal artery occlusion: design issues and implications. EAGLE Study report no. 1. Graefes Arch Clin Exp Ophthalmol. 2006;244:950–956. doi: 10.1007/s00417-005-0140-2. [DOI] [PubMed] [Google Scholar]
- 8.Ness T, Auw-Hadrich C, Schmidt D. Arteriitis temporalis (Riesenzellarteriitis). Klinik, Histologie und Therapie. Ophthalmologe. 2006;103:296–301. doi: 10.1007/s00347-006-1324-9. [DOI] [PubMed] [Google Scholar]
- 9.Eckardt C, Gotze O, Utermann D. Über die Lebenserwartung von Patienten mit Zirkulationsstörungen am hinteren Bulbusabschnitt. [Life expectancy of patients with circulatory disorders of the posterior eyeball segment] Ophthalmologica. 1983;187:34–42. doi: 10.1159/000309299. [DOI] [PubMed] [Google Scholar]
- 10.Dithmar S, Hansen LL, Holz FG. Venöse retinale Verschlüsse. Ophthalmologe. 2003;100:561–577. doi: 10.1007/s00347-003-0820-4. [DOI] [PubMed] [Google Scholar]
- 11.Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000;98:133–41. discussion 41-3. [PMC free article] [PubMed] [Google Scholar]
- 12.―Hayreh SS, Zimmerman MB, Podhajsky P. Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol. 1994;117:429–441. doi: 10.1016/s0002-9394(14)70001-7. [DOI] [PubMed] [Google Scholar]
- 13.Lang GE. Zentralvenenverschlüsse. Klin Monatsbl Augenheilkd. 2007;224:R 95–R 109. [Google Scholar]
- 14.David R, Zangwill L, Badarna M, Yassur Y. Über die Lebenserwartung von Patienten mit Zirkulationsstörungen am hinteren Bulbusabschnitt. Ophthalmologica. 1988;197:69–74. [Google Scholar]
- 15.Hansen LL. Behandlungsmöglichkeiten bei Zentralvenenverschlüssen. Ophthalmologe. 1994;91:131–145. [PubMed] [Google Scholar]
- 16.Mruthyunjaya P, Wirostko WJ, Chandrashekhar R, et al. Central retinal vein occlusion in patients treated with long-term warfarin sodium (Coumadin) for anticoagulation. Retina. 2006;26:285–291. doi: 10.1097/00006982-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 17.De Sanctis MT, Cesarone MR, Belcaro G, et al. Treatment of retinal vein thrombosis with pentoxifylline: a controlled, randomized trial. Angiology. 2002;53(Suppl 1):35–38. [PubMed] [Google Scholar]
- 18.Hansen LL, Danisevskis P, Arntz HR, Hovener G, Wiederholt M. A randomised prospective study on treatment of central retinal vein occlusion by isovolaemic haemodilution and photocoagulation. Br J Ophthalmol. 1985;69:108–116. doi: 10.1136/bjo.69.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen LL, Wiek J, Wiederholt M. A randomised prospective study of treatment of non-ischaemic central retinal vein occlusion by isovolaemic haemodilution. Br J Ophthalmol. 1989;73:895–899. doi: 10.1136/bjo.73.11.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jonas JB, Kreissig I, Degenring RF. Intravitreal triamcinolone acetonide as treatment of macular edema in central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2002;240:782–783. doi: 10.1007/s00417-002-0529-0. [DOI] [PubMed] [Google Scholar]
- 21.Stahl A, Agostini H, Hansen LL, Feltgen N. Bevacizumab in retinal vein occlusion-results of a prospective case series. Graefes Arch Clin Exp Ophthalmol. 2007;245:1429–1436. doi: 10.1007/s00417-007-0569-6. [DOI] [PubMed] [Google Scholar]
- 22.Cugati S, Wang JJ, Knudtson MD, et al. Retinal vein occlusion and vascular mortality: pooled data analysis of 2 population-based cohorts. Ophthalmology. 2007;114:520–524. doi: 10.1016/j.ophtha.2006.06.061. [DOI] [PubMed] [Google Scholar]
- 23.Kuhli C, Hattenbach LO, Scharrer I, Koch F, Ohrloff C. High prevalence of resistance to APC in young patients with retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2002;240:163–168. doi: 10.1007/s00417-001-0415-1. [DOI] [PubMed] [Google Scholar]
- 24.Kuhli C, Scharrer I, Koch F, Ohrloff C, Hattenbach LO. Factor XII deficiency: a thrombophilic risk factor for retinal vein occlusion. Am J Ophthalmol. 2004;137:459–464. doi: 10.1016/j.ajo.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 25.Fegan CD. Central retinal vein occlusion and thrombophilia. Eye. 2002;16:98–106. doi: 10.1038/sj.eye.6700040. [DOI] [PubMed] [Google Scholar]
- e1.Savino PJ, Glaser JS, Cassady J. Retinal stroke. Is the patient at risk? Arch. Ophthalmol. 1977;95:1185–1189. doi: 10.1001/archopht.1977.04450070083005. [DOI] [PubMed] [Google Scholar]
- e2.Lorentzen SE. Occlusion of the central retinal artery. A follow-up. Acta Ophthalmol (Copenh) 1969;47:690–703. doi: 10.1111/j.1755-3768.1969.tb08157.x. [DOI] [PubMed] [Google Scholar]
- e3.Kohner EM, Pettit JE, Hamilton AM, Bulpitt CJ, Dollery CT. Streptokinase in central retinal vein occlusion: a controlled clinical trial. BMJ. 1976;1:550–553. doi: 10.1136/bmj.1.6009.550. [DOI] [PMC free article] [PubMed] [Google Scholar]