Abstract
Introduction
The ever-increasing level of air traffic means that any medical evaluation of its effects must be based on recent data.
Methods
Selective literature review of epidemiological studies from 2000 to 2007 regarding the illnesses, annoyance, and learning disorders resulting from aircraft noise.
Results
In residential areas, outdoor aircraft noise-induced equivalent noise levels of 60 dB(A) in the daytime and 45 dB(A) at night are associated with an increased incidence of hypertension. There is a dose-response relationship between aircraft noise and the occurrence of arterial hypertension. The prescription frequency of blood pressure-lowering medications is associated dose-dependently with aircraft noise from a level of about 45 dB(A). Around 25% of the population are greatly annoyed by exposure to noise of 55 dB(A) during the daytime. Exposure to 50 dB(A) in the daytime (outside) is associated with relevant learning difficulties in schoolchildren.
Discussion
Based on recent epidemiological studies, outdoor noise limits of 60 dB(A) in the daytime and 50 dB(A) at night can be recommended on grounds of health protection. Hence, maximum values of 55 dB(A) for the day and 45 dB(A) for the night should be aimed for in order to protect the more sensitive segments of the population such as children, the elderly, and the chronically ill. These values are 5 to10 dB(A) lower than those specified by the German federal law on aircraft noise and in the report "synopsis" commissioned by the company that runs Frankfurt airport (Fraport).
Keywords: aircraft noise, noise exposure, hypertension, myocardial infarction, environmental pollution
Continually rising levels of air traffic are making it increasingly important to medically evaluate the effects of aircraft noise, with particular emphasis on organic diseases, annoyance, and functional disorders. Field studies under conditions of daily living are suitable instruments for this purpose. Laboratory tests are of only limited value because they fail to record phenomena such as habituation, sensitization, conditioning, and exhaustion. Sleep disorders in the form of awakening reactions (1) are also little suited for evaluation purposes since their avoidance is insufficient for the prevention of long-term health hazards (2).
Epidemiological research into the effects of noise has made significant strides in recent years. The availability of new studies therefore mandates a reassessment of the current situation. Many of the epidemiological studies published up to the year 2000 exhibit methodological deficiencies. In many cases, extreme groups were considered in a simplifying approach or the study population was classified as "exposed to stress" and "not exposed to stress" on the basis of a noise level criterion. These studies reveal only a trend towards increased health risks from continuous noise levels of 65 dB(A) upwards (3). New results are available especially as regards hypertension, annoyance, and learning difficulties (box 1).
Box 1. How loud are continuous sound levels?
Continuous sound levels are energy values averaged over a long assessment period and are inaudible. Only momentary sound events are perceptible. If the sound energy remains constant over the assessment period, however, the continuous sound level has the same value as the momentary sound level. The continuous sound level, with additions or deductions for the time of day, for example, is a single figure value intended to gauge only the long term effects of a noise situation. In Germany the established practice is to differentiate between the continuous daytime sound level (6 a.m. to 10 p.m.) and the continuous nocturnal sound level (10 p.m. to 6 a.m.). The unit of measurement is the dB(A), which takes into account that human hearing has variable sensitivity for different frequencies. The fact that aircraft noise is perceived as a greater annoyance than road and rail noise, however, is not factored in. In residential areas around civil airports, the continuous aircraft related noise level now reaches levels exceeding 65 dB(A). For example, about 200 000 residents in the area around Frankfurt Airport, some of whom live more than 20 km distant from the airport along the flight corridors, are exposed to a continuous daytime noise level of 55 dB(A) and above.
Method
A selective literature review of epidemiological studies from 2000 to March 2007 was performed in the DIMDI and PubMed databases using the search terms noise and epidemiol*** (German and English), supplemented by literature references from the authors’ own databases. Articles with the terms occupational, work, and tinnitus were excluded electronically. In a second step, articles obviously unrelated to the study topic, such as studies on the effects on hearing or language, were excluded. In the third step, 10 primary studies among 81 remaining publications were identified on the basis of study topic (for example day or night), design (information value), scope (avoidance of random errors), and the probability of systematic errors (bias) (table 1). Inclusion criteria were case numbers of above 1000 or more than 5000 individual measured values in the case of the time-series studies, address-based recording of aircraft noise exposure, and standardized recording of the effect endpoints or medical diagnoses of diseases elicited by questionnaire. Review articles and standard publications as well as studies with other effect endpoints were disregarded. The primary studies identified on this basis were evaluated in terms of diseases, noise annoyance, and learning difficulties.
Table 1. Overview of selected primary studies.
| First author (study name) | Year | Study design | Persons | Exposure (recording) | Endpoint and recording | Stratification and control variables | Results (selected endpoints) | Comments (limitation) |
| M. Rosenlund (8) | 2001 | Cross-sectional study | 2959 adults, 19 to 80 years | Aircraft noise (aircraft noise contours) | Elicited hypertension diagnoses | Age, gender, smoking, education, physical activity, fruit consumption, house type | OR 1.3 (95% CI: 0.8 to 2.2) for trend per 5 dB; OR 1.6 (95% CI: 1.0 to 2.5) for FBN >55 dB(A); prevalence reference group 14% (FBN < 55 db [a]) | Random sample, high response rate (few cases with high levels) |
| C. Eriksson (9) | 2007 | Cohort study (follow-up study) | 2037 men, 35 to 56 years | Aircraft noise (GIS technology) | Medical hypertension diagnoses based on BP measurements and medical history impaired glucose tolerance, noise annoyance | Age, smoking, BMI, physical inactivity, HL, SES, family history (diabetes), | RR 1.1 (95% CI: 1.01 to 1.2) for trend per 5 dB; RR 1.2 (95% CI: 1.03 to 1.4) for FBN >50 dB(A); incidence reference group 27% (FBN < 50 db [a]) | Random sample, 10 year follow-up period, BP 140/90 mmHg (men only) |
| L. Jarup (HYENA) (10) | 2007 | Cross-sectional study | 4861 adults, 45 to 70 years | Aircraft noise separately for day and night (road traffic noise) | Hypertension diagnoses based on BP measurements and medical treatment | Country, age, gender, BMI, alcohol, physical activity, education | For increase in night-time Leq by 10 dB OR 1.14 (95% CI: 1.01 to 1.29); prevalence in the countries 49% to 57% | Aircraft noise recorded for day and night BP 140/90 mmHg (low response rate); few cases with high levels |
| E. Öhrström (LERUM study) (11) | 2005 | Cross-sectional study | 1953 adults, 18 to 75 years | Road, rail, aircraft noise (GIS technology) | Elicited medication consumption and hypertension diagnoses | Age, gender, smoking, BMI, education, marital status, occupational noise | Hypertension: OR 1.1 at 50–55 dB(A) to OR 4.0 (95% CI: 1.3 to 13) at 60 to 70 dB(A) (Leq, 24 h) Medications: OR 1.6 at 50 to 55 dB(A) to 0R 5.3 (95% CI: 1.5 to 19) at 60 to 70 dB(A) (Leq, 24 h) | Medication consumption and hypertension diagnoses elicited simultaneously, random sample, high response rate |
| E.A.M. Franssen (12) | 2004 | Cross-sectional study | 11 812 adults over 18 years | Aircraft noise (ZIP codes) | Medication consumption (cardiovascular, sleep) | Age, gender, smoking, education, urbanization, ethnicity | Trend per 10 dB Lden from 50 dB(A): cardiovascular medications OR 1.30 (95% CI: 1.06 to 1.6) hypnotic agents (non-prescription) OR 2.34 (95% CI: 1.63 to 3.35) | Large sample size (increased exposure uncertainty, low response rate) |
| E. Greiser (Cologne/Bonn Airport Study (13) | 2006 | Cross-sectional study | 809 379 insured persons of all ages | Nocturnal aircraft noise (GIS technology) | Medication prescriptions (cardiovascular drugs and others) | Age, gender, social welfare incidence, nursing home density, interaction term of aircraft noise and social welfare incidence, night-time road and rail traffic noise (95% CI: 1.014 to 1.030) | Trend per 1 dB from 39 dB(A) (Leq, 3 to 5 h), highest social welfare quartile: antihypertensives, women: OR 1.049 (95% CI: 1.042 to 1.056); men: OR 1.020 (95% CI: 1.014 to 1.026); cardiac drugs, women OR 1.049 (1.042 to 1.056); men 1.022 | More than 800 000 insured persons, 43.2% of study population, no response bias, no recall bias (no person-related control variables) |
| Y. Aydin (14) | 2007 | Time-series study (3 months) | 53 adults, 14 to 76 years | Day-to-day changes in aircraft noise | 8266 measurements of blood pressure, heart rate, and perception of aircraft noise | Age, gender, BMI, smoking, medications, night-time window position (parallelized groups) | Mean BP in West group (50 dB [A] for 75% of time) approx. 10/8 mmHg significantly higher than East group (50 dB [A] for 25% of time); low-noise periods no longer distinguishable from loud periods in West group | Small groups but >8000 individual measurements, acute aircraft noise effects, cross- correlation analyses (volunteers) |
| W. Babisch (NaRoMI study) (4) | 2004 | Case control study | 4115 adults, 20 to 69 years | Road traffic noise, most highly exposed façade (RLS 90) | Myocardial infarction patients (hospital admission) family history (MI), cholesterol | Age, gender, smoking, education, BMI, occupational status, marital status, shift work, NS, diabetes mellitus, HBP, versus < 65 db(a) | Infarction risk (men, Leq, day, residence period >10 years): OR 1.17 at 60 to 65 dB(A) to OR 1.8 (95% CI: 1.02 to 3.21) >70 dB(A). OR 1.4 (1.0 to 2.0) >65 dB(A) | All MI admissions in 3 years in 32 Berlin hospitals (continuous noise level only 6 a.m. to 10 p.m.) |
| S. A. Stansfeld (RANCH study) (15) | 2005 | Cross- sectional study (3 nation study) | 2844 children, 9 to 10 years | Aircraft noise (GIS technology, aircraft noise contours) | Reading comprehension, memory performance, annoyance window type/glazing | Age, gender, nationality, SES, mother’s education, longstanding childhood diseases, native language, parental assistance with school work, school (non-linear) p = 0.018 | With increasing aircraft noise: decrease in reading comprehension (n = 2010) Beta = –0.008; p = 0.0097 Decreased recognition (n = 1998) Beta = –0.018; p = 0.0141 increase in annoyance | International study at 89 schools, standardized method inventory (very small age range) |
| D. Schreckenberg (RDF study) (18) | 2006 | Cross- sectional study | 2312 adults over 18 years | Aircraft noise (GIS technology) | Annoyance (ICBEN scales), quality of life | Age, gender, SES, various acoustic parameters | Dose-response relationship to continuous noise level; in level class 50 to 52.5 dB(A) (and 47.5 to 50 real distribution) 25% of population exposed to "serious annoyance" | Random sample, external quality control, standardized survey of annoyance (no adjustment) |
BMI, body mass index; HL, hearing loss; HBP, high blood pressure; MI, myocardial infarction; NS, noise sensitivity; BP, blood pressure; FBN, continuous day-night aircraft noise level;
Lden, noise index; SES, socioeconomic status; GIS, geo-information system; RLS 90, German Guideline for Protection against Road Traffic Noise; OR, odds ratio; RR, relative risk; CI, confidence interval
As regards myocardial infarction, one road traffic noise study is also mentioned (4) because no aircraft noise studies are available on this topic. One study from 1995 (16) is devoted to learning difficulties; there are no new longitudinal observations on this subject (table 1).
Results
The most informative new studies relate to hypertension, annoyance, and learning difficulties. As far as may be deduced from the findings, absolute changes in risk were reported. A study of road traffic noise annoyance and a meta-analysis showed a significant noise-related increase in myocardial infarctions from continuous daytime noise levels of 60 dB(A) upwards (4, 5). No studies exploring a relationship with aircraft noise are available. This association is therefore not examined more closely. There is no doubt, however, that every increase in arterial hypertension can lead to more infarctions and strokes.
Hypertensive disease
In pathophysiological terms, the development of noise-related hypertension is regarded as the consequence of impaired recovery processes. Noise-related stress persisting over long periods can lead to the exhaustion of compensatory mechanisms and a decrease in the body’s regulatory capacity. In many cases, therefore, health effects of chronic noise-related stress only begin to appear after 5 to 15 years (6). Chronic arterial hypertension affects a large segment of the population and is a major risk factor for myocardial infarction and stroke. At least every third adult has blood pressure values above the optimal range and an increase from "optimal" to still normal blood pressure values doubles the risk of stroke or myocardial infarction (7).
In 2001, Rosenlund evaluated aircraft noise exposure for 2959 adults based on an address-specific search and found an association between the increase in raised blood pressure and a continuous 24 h aircraft noise level (FBN) above 55 dB(A) and at maximum levels above 72 dB(A) (8).
Eriksson et al. studied 2037 men in the 40 to 60 year age group over a 10 year period (9, e1). The continuous noise levels (FBN) were determined for exact addresses using a geo-information system (GIS technology). The presence of hypertension was documented by repeated medical examinations including blood pressure measurements and a questionnaire about cardiovascular treatments and risk factors. Exposure to aircraft noise above 50 dB(A) (FBN) was associated with a significant 20% increase in the risk of hypertension (table 2).
Table 2. Relationship between aircraft noise annoyance and number of hypertension sufferers (HT).
| Noise annoyance*1 | n | HT | HT (%) | RR*2 | 95% CI |
|---|---|---|---|---|---|
| per 5 dB*3 | 2020 | 626 | 31 | 1.10 | 1.01–1.19 |
| <50 db (a) | 1610 | 478 | 29.7 | 1 | – |
| ≥ 50 dB (A) | 410 | 148 | 36.1 | 1.19 | 1.03–1.37 |
Medical examinations including blood pressure measurements plus a questionnaire about cardiovascular treatments and risk factors.
The relative risk (RR) and the 95% confidence interval (95% CI) are reported for adjusted data (acc. to 9).
A relative risk is statistically significant if the respective confidence interval (95% CI) does not include the value 1.
For FBN the continuous evening (7 to 10 p.m.) noise level is supplemented with 5 dB and the continuous night-time noise level (10 p.m. to 7 a.m.) is supplemented with 10 dB. Study period: 10 years; incidence in the reference group (<50 dB [A]) 26.7%;
*1 24 h continuous noise level (FBN); *2 adjusted for age and body mass index; n, persons with complete data on noise exposure and the control variables;
*3 The relationship is applicable from FBN 50 dB[A]
The special significance of nocturnal noise exposure for the development of hypertension is demonstrated by the HYENA study (10, e2), which studied 4861 adults aged 45 to 70 years living in the close vicinity of 6 European airports. The continuous noise levels were determined to an accuracy of 1 dB for exact addresses, separately for the day and night. The presence of hypertension was determined by repeated blood pressure measurements and a questionnaire about cardiovascular treatments. The prevalence of hypertension adjusted for age and gender was between 49% and 57% in the countries concerned. A 10 dB increase in the continuous night-time noise level was found to be significantly associated with a 14% increase in the probability of being diagnosed with hypertension. The first significant level class was 40 to 44 dB(A). The chance of becoming ill also increased slightly with continuous daytime noise levels, but was not statistically significant.
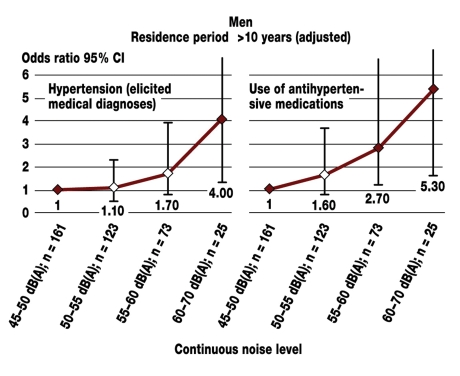
A Swedish study (11, e3) demonstrated a close association between noise level, hypertension, and use of blood pressure lowering medications (figure 1). 1953 volunteers aged between 18 and 75 years from a random sample were studied. The feedback rate was 71%. All volunteers were exposed to a traffic induced continuous noise level (road, rail, air traffic) of at least 45 dB(A) over 24 h. The noise exposure was determined for exact addresses (GIS technology) and compared with medical diagnoses of hypertension elicited by a questionnaire (figure 1).
Figure 1.
Odds ratio for hypertension and use of antihypertensive medications in men with a residence period of at least 10 years as a function of exposure to road, aircraft, and rail traffic noise. Adjusted for age, gender, smoking, body mass index, marital status, school education, and occupational noise exposure.
An odds ratio is statistically significant here when the corresponding 95% confidence interval (T bar) does not include the value 1. Significant odds ratios are recorded in the study for medication use from 55 to 60 dB(A) (LAeq, 24 h), (LAeq, 24 h = 24 hour continuous noise level) according to (11).
Increased medication consumption associated with aircraft noise exposure was also revealed by a Dutch study with 11 812 participants. In this case, however, exposure was only recorded approximately by means of zip codes (12). In this case the clearest increase in consumption was associated with evening noise, which could be due to the legal restrictions on night flight activity in Amsterdam.
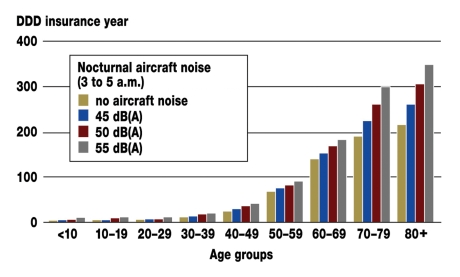
The largest study of medication use was performed in the vicinity of Cologne/Bonn Airport (Germany). Individual prescription data of 809 379 persons insured with statutory health insurance companies were linked to address-specific aircraft and road traffic noise exposure data (GIS technology) (13, e4). The study revealed significant relationships between the intensity of aircraft noise and the number of antihypertensive medications prescribed per patient. The increase in prescription prevalence correlated most clearly with night-time aircraft noise between 3 and 5 a.m., since the highest nocturnal aircraft noise exposure occurs at Cologne/Bonn Airport during this period. For this time window, antihypertensive medications for women were already prescribed 27% significantly more often at a continuous aircraft noise level of 40 to 45 dB(A) and 66% significantly more often at 46 to 61 dB(A). For men, the significant increase in prescription prevalence was 24% at continuous noise levels of 46 to 61 dB(A).
Significant exposure dose-effect associations were detected, i.e. the more noise, the more medications were prescribed (figure 2).
Figure 2.
Prescription of antihypertensive medications in relation to increasing night-time noise exposure in women compared to women without aircraft noise in quiet residential areas with a nocturnal road and rail traffic noise level of <35 dB(A). Adjusted for frequency of social welfare, density of nursing home places, interaction of social welfare and aircraft noise, possibility of applying for noise protection measures. The prevalence in the total population of women is 24% (men 19.3%). An increase in prescriptions is already apparent from 45 dB(A) upwards. (DDD= defined daily doses) (13) (DDD insurance year is a numerical value for average medication prescribing in the insurance year).
As regards the prodromal stages of chronic hypertensive disease, a time-series study performed in the vicinity of Frankfurt Airport in Germany showed that a relationship between the day-to-day variations in aircraft noise and morning blood pressure is also present in the physiological range. Two groups exposed to a continuous nocturnal outdoor air traffic noise level of 50 dB(A) were compared for three months: the West group was exposed for 75% of the time, the East group for 25% of the time. The evaluation of altogether 8266 blood pressure measurements in 53 persons showed that blood pressure was statistically significantly higher by a mean 10/8 mmHg in the West group compared to the East group. The West group was also found to have a reduced relaxation ability insofar as the "less noisy" periods were no longer perceived as such as a consequence of the noise related stress (14).
There are no epidemiological studies with results that contradict an increase in hypertension due to aircraft noise.
Learning difficulties
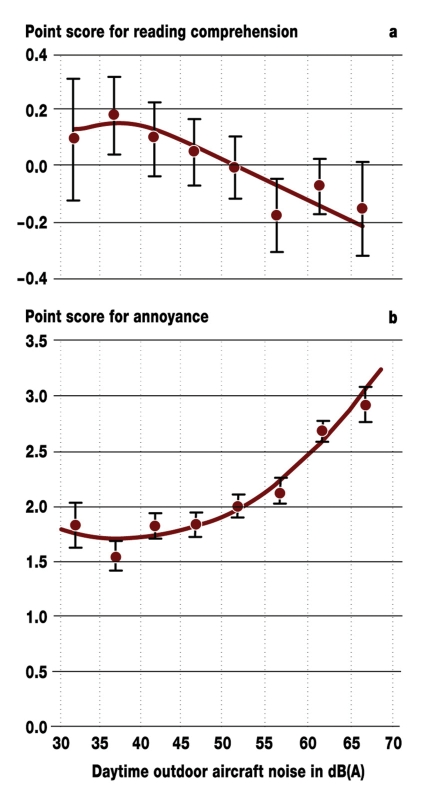
Noise can impair human mental performance without detectable organic damage. Stansfeld et al. studied 2844 children aged 9 to 10 years in 89 schools. These children showed a significant relationship between the deterioration in silent reading comprehension and certain memory performances and increasing aircraft noise exposure at schools (15). Reading comprehension showed a linear decrease with increasing noise (figure 3 a), while the subjective annoyance showed a logarithmic increase (figure 3 b).
Figure 3.
Association of aircraft noise and reading comprehension.
a) With increasing aircraft noise there is a linear decrease in silent reading comprehension.
b) The extent of subjective annoyance increases logarithmically.
The relationships are significant after factoring in the socioeconomic data. From (15)
An earlier longitudinal study in 9- to 13-year-olds in Munich, Germany, produced similar results (16, e5, e6), while a study in 11-year-olds from 2002 (e7) showed that socioeconomic factors could be responsible for the learning impairments. In the Stansfeld study, the relationships demonstrated remained statistically significant after adjustment for mother’s education, socioeconomic status, longstanding illness, and extent of classroom insulation against noise (15). Children had a one- to two-month reading delay per 5 dB(A) increase in aircraft noise (15, e8–e10). There are no studies that contradict these findings.
Annoyance
Aircraft noise annoyance is evaluated in Europe mainly by means of meta-analyses of the kind submitted by Miedema et al. (17, e11). The studies on which they are based, however, are more than 25 years old in relation to the year 2007.
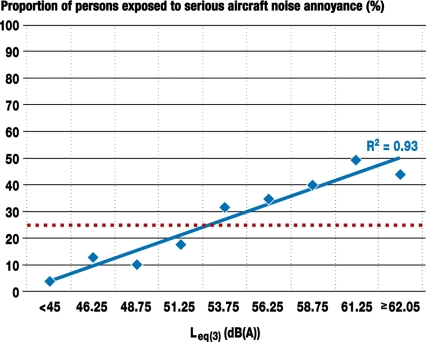
The air traffic investigated in these studies and the types of aircraft operating at that time are hardly comparable with the present day situation at passenger airports. A new study performed in the vicinity of Frankfurt Airport revealed that 64% of the survey sample felt themselves exposed to moderate to extreme aircraft noise annoyance, compared to only 23% in the rest of the state of Hesse. The survey sample classified aircraft noise as the most objectionable source of noise (18, 19, e12): the higher the aircraft noise level, the greater was the annoyance (figure 4).
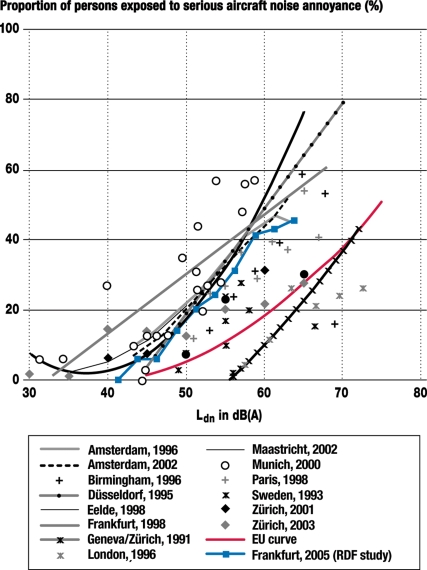
Figure 4.
Proportion of persons exposed to serious aircraft noise annoyance as a factor of continuous daytime noise level (Leq, 16 h) calculated by the 100% rule (19). According to the 100% rule, an envelope is formed from the noise values for East and West operation in the six busiest air traffic months (in Frankfurt usually May to October). This is a representation of the worst case situation of a mean East and a mean West situation, irrespective of the frequency of occurrence. The volunteers answered the question: "Overall, how seriously have you felt disturbed or annoyed by the aircraft noise over the last 12 months?" Persons who reported a value in the upper 28% of the survey scale from "not at all" to "extremely" were defined as exposed to serious annoyance. The intersection point of the continuous line with the dotted line marks the corresponding level range within which 25% of those surveyed classified themselves as exposed to serious annoyance. The range of the level classes was 1.25 dB(A). R² is the square of the correlation coefficient r and is a measure of the closeness of the correlation, with 1 being the highest achievable value (18).
At a continuous daytime outdoor noise level of 53 dB(A), 25% of local residents considered themselves exposed to a serious noise annoyance. In the relevant legislation, this percentage is defined as the beginning of considerable annoyance (e13). A comparison of the 25% annoyance curve of Frankfurt with that of other European airports shows that the Frankfurt values are in the mid-range of more recent studies. It may therefore be assumed that the noise associated with the anticipated extension is not greatly overestimated (figure 5). The aircraft noise was perceived as a particular nuisance in the night and in the off-peak hours, i.e., in the morning and evening. In addition, aircraft noise was perceived as a much greater annoyance at the weekends than during the week (19) (figure 5).
Figure 5.
Dose-response data of 11 studies on the proportion of exposure to serious aircraft noise annoyance (18, e17). Studies were selected which were based on Ldn levels. Ldn is a continuous 24 h noise level at which the continuous night-time noise level (10 p.m. to 6 a.m.) is supplemented with 10 dB.
The boundary to considerable annoyance is now established at much lower continuous aircraft noise levels than in previous studies. Guski et al. already mentioned in 2004 that between 1960 and 1995 the continuous noise level decreased by about 8 dB(A) with the same level of annoyance (20). Today the boundary at which 25% of the average population feel seriously affected is approximately another 8 dB(A) lower. High mobility figures, sensitization by years of stress and the refined study methodologies are under discussion as reasons for this decrease.
Nocturnal noise
In the HYENA study, an increase in blood pressure requiring treatment was significantly associated with a continuous nocturnal aircraft noise level of 40 to 44 dB(A), compared to an exposure below 35 dB(A). In the Eriksson study (9) in the 40 to 60 year age group of volunteers, a risk increase was associated with a nocturnal aircraft noise level from about 40 dB(A) upwards, assuming an 8% night air traffic and 20% evening air traffic distribution. The Cologne medication study yielded similar threshold values. In this case, a significant increase in prescriptions for antihypertensive medications was already associated with nocturnal exposure, between 3 and 5 a.m., in the range of 40 to 45 dB(A) in women and of 46 to 61 dB(A) in men. Health is therefore impaired at the latest by a continuous nocturnal aircraft noise level of 50 dB(A). From this level onwards, organic diseases and functional disorders with a positive exposure-effect relationship are to be expected. As with other injurious environmental factors, a certain distance from this level must be maintained. In 2001, a night-time level of 45 dB(A) was recommended as a prophylactic value by the great majority of German noise researchers (21). Recent epidemiological studies confirm this estimate.
Whereas a nocturnal health hazard was formerly evaluated on the basis of awakening reactions, principal emphasis is now placed on the increased incidence of cardiovascular diseases associated with night-time noise (2). Assessing the hazard solely on the basis of awakening reactions is not acceptable because long-term health impairments cannot be ruled out when using this approach (2).
Daytime noise
Associations are also detectable for daytime noise annoyance. Increased use of antihypertensive medications was significant in the level class Leq, 16 h at approx. 57.5 to 61.5 dB(A) during the daytime (11). Impairment of cognitive abilities of schoolchildren was exposure related and began at continuous outdoor aircraft noise levels above 45 dB(A) (16). Aircraft noise levels causing serious annoyance for 25% of the average population are classified in Germany as the upper limit of acceptable noise annoyance. In the Frankfurt study on noise annoyance, the boundary to considerable annoyance was defined as a continuous daytime noise level of 53 dB(A). The risk of health impairments therefore begins at the latest at continuous daytime noise levels of 60 dB(A). In terms of sensitivity, off-peak times during the day are to be classified as between the daytime and night-time value.
Discussion
The guide values determined are consistent with the findings and recommendations of German and international noise research (2, 21). The authors consider a publication bias unlikely because the large studies are usually already known while they are in progress and before results have been determined. Major deviations are revealed by the "synopsis" report commissioned by the company that runs Frankfurt Airport (22, 23). Since this summarizing assessment is frequently considered judicially to represent the current state of knowledge, a comparison with recent epidemiological findings is provided in table 3.
Table 3. Comparison of Frankfurt "synopsis" report and epidemiological findings.
| Synopsis 2001/2007 | Epidemiological findings 2000–2007 | ||
|---|---|---|---|
| Protection goal: health | |||
| Critical tolerance value 6 a.m. to 10 p.m. outdoors | 70 dB(A) | 65 dB(A) | In men with residence period >10 years significantly increased infarction risk with continuous daytime levels of road traffic noise >65 compared to <65 db(a) (4) |
| Critical tolerance value 10 p.m. to 6 a.m. outside | – | 50 dB(A) | Upper limit of first significant level class at 44 dB(A) according to (10). During the night period of 3 to 5 h, significant increase in prescription of blood pressure lowering medications in women from 40 to 45 dB(A), in men from 46 to 61 dB(A) upwards (13) |
| Preventive guide value 6 a.m. to 10 p.m. outdoors | 65 dB(A) | 60 dB(A) | Beginning of increased risk of myocardial infarction at 60 dB(A) road traffic noise (5). At 55 dB(A) (FBN) aircraft noise, significant increase in incidence of hypertension (8); at 50 dB(A) (FBN) aircraft noise for vulnerable group (9) |
| Preventive guide value 10 p.m. to 6 a.m. outside | – | 45 dB(A) | Lower limit of first significant level class at 40 dB(A) (10). At 50 dB(A) blood pressure increase depending on exposure period (14). In the night period of 3 to 5 h, significant increase in prescription of blood pressure lowering medications in women from 40 to 45 dB(A) upwards (13). |
| Protection goal: prevention of considerable annoyance | |||
| Critical tolerance value 6 a.m. to 10 p.m. outdoors | 65 dB(A) | 55 dB(A) | Upper limit of level class with 25% of persons exposed to serious annoyance (19) |
| Preventive guide value 6 a.m. to 10 p.m. outdoors | 62 dB(A) | 52.5 dB(A) | Lower limit of level class with 25% of persons exposed to serious annoyance (19) |
| Protection goal: prevention of learning impairments | |||
| Critical tolerance value school attendance hours | – | 55 dB(A) outdoors | Upper limit of level class with significantly increased annoyance compared to 35 to 40 dB(A). Marked impairment of reading comprehension (16). |
| Preventive guide value school attendance hours | 40 dB(A) indoors equivalent to 55 dB(A) outdoors | 50 dB(A) outdoors | Lower limit of level class with significantly increased annoyance compared to 35 to 40 dB(A). Latest onset of reading comprehension (16). |
FBN, continuous 24 h noise level
The "synopsis" report is based on the following definitions, among others:
A critical tolerance value states that health hazards or impairments can no longer be ruled out.
A preventive guide value defines when health hazards are largely ruled out (table 3).
In their publication of 2007, the authors of the Frankfurt "synopsis" see no reason to depart from the previous conclusions (23).
The higher values of still acceptable noise exposure can be explained to a great extent by the fact that the less suitable and in most cases old laboratory studies and the occurrence of night-time awakening reactions continue to be regarded as authoritative in the report. According to the new epidemiological studies, continuous daytime outdoor noise levels of 60 dB(A) and night-time levels of 50 dB(A) should not be exceeded in residential areas in order to extensively rule out damage to health. Vulnerable groups, especially children, the elderly, and the chronically ill may already be affected at levels below those tolerated by average persons. On medical criteria, a prophylactic outdoor value of 55 dB(A) (daytime) and 45 dB(A) (night-time) is therefore considered desirable. At about 55 dB(A) during the day it is to be assumed that 25% of persons will feel exposed to a serious noise annoyance.
Annoyance for awake persons can only be prevented by reducing aircraft noise (18, 19). The same presumably applies for the prevention of organic diseases and learning difficulties. Passive noise protection measures such as soundproof windows are not sufficient. Sleeping with closed, soundproof windows must also be regarded as hygienically questionable (24). Air change rates tend towards zero with closed windows. The DIN 1946-2 and DIN 1946-6 standards specify 0.15 percent by volume (1500 ppm) as the upper limit for CO2 concentrations in living spaces (e14–e16). This value is already exceeded after the first hours of sleep when windows are closed (box 2).
Box 2. Noise protection areas.
The German Aircraft Noise Protection Act in the version of 30 October 2007 defines noise protection zones (NPZ) on the basis of continuous sound levels and maximum night-time level criteria. For new or substantially altered airports, the daytime protection areas begin at a continuous sound level of 60 dB(A). This represents NPZ 1. At night, the protection zone begins at a continuous sound level of 53 dB(A), from 2011 of 50 dB(A). From this level onwards, claims for damages for passive noise protection are possible. It is not yet clear what consequences the recently adopted Aircraft Noise Act has for persons living in the airport vicinity in terms of entitlement to active noise protection. Ekardt and Seidel take the view that the limits defined in the Act are only minimum standards that do not rule out the introduction of stricter requirements for planning purposes (25). Based on these considerations and considering that the protection of health is guaranteed by the Basic Law, these results are of major relevance. The Aircraft Noise Act is to a great extent based on the state of scientific knowledge existing in the year 1999 when the first draft of the Amending Act was prepared.
Health hazards caused by aircraft noise can be most reliably identified from epidemiological field studies. The investigations conducted in recent years show distinctly lower guide values for health hazards, learning difficulties, and annoyance than previous assumptions on which the German Aircraft Noise Act is also based. Against this background, a warning must be issued from the medical viewpoint regarding a further increase in the widespread disease of hypertension associated with exposure to noise.
Acknowledgments
Translated from the original German by mt-g.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Basner M, Samel A, Isermann U. Aircraft noise effects on sleep: application of the results of a large polysomnographic field study. J Acoust Soc Am. 2006;119:2772–2784. doi: 10.1121/1.2184247. [DOI] [PubMed] [Google Scholar]
- 2.WHO Night Noise Guideline -Team of experts. Short term effects of transportation noise on sleep with specific attention to mechanism and possible health impact. Report on the second meeting on night noise guidelines. World Health Organization Regional Office for Europe. 2004 [Google Scholar]
- 3.Babisch W. Traffic noise and cardiovascular disease: epidemiological review and synthesis. Noise Health. 2000;2:9–32. [PubMed] [Google Scholar]
- 4.Babisch W, Beule B, Schust M, Kersten N, Ising H. Traffic noise and risk of myocardial infarction. Epidemiology. 2005;16:33–40. doi: 10.1097/01.ede.0000147104.84424.24. [DOI] [PubMed] [Google Scholar]
- 5.Babisch W. Transportation noise and cardiovascular risk. Review and synthesis of epidemiological studies - dose-effect curve and risk estimation. WaBoLu-Hefte 01/06, Umweltbundesamt Berlin. 2006 doi: 10.4103/1463-1741.32464. [DOI] [PubMed] [Google Scholar]
- 6.Graff C, Bockmüphl F, Tietze V, Nitschkoff S, Kriwizkaja G. Lärmbelastung, akustischer Reiz und neurovegetative Störungen. Stuttgart: Georg-Thieme Verlag; 1968. Lärmbelastung und arterielle (essentielle) Hypertoniekrankheit beim Menschen; pp. 112–126. [Google Scholar]
- 7.Zipes DP, Libby P, Bonow RO, Braunwald E. Heart disease. 7th ed. Philadelphia: Elsevier Saunders; 2005. [Google Scholar]
- 8.Rosenlund M, Berglund N, Pershagen G, Järup L, Bluhm G. Increased prevalence of hypertension in a population exposed to aircraft noise. Occup Environ Med. 2001;58:769–773. doi: 10.1136/oem.58.12.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eriksson C, Rosenlund M, Pershagen G, Hilding A, Ostenson C-G, Bluhm G. Aircraft noise and incidence of hypertension. Epidemiology. 2007;18:716–772. doi: 10.1097/EDE.0b013e3181567e77. [DOI] [PubMed] [Google Scholar]
- 10.Jarup L, Babisch W, Houthuijs D, et al. Hypertension and exposure to noise near airports - the HYENA study. Environmental health perspectives. 2008;116:329–333. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Öhrström E, Barregård L. Undersökning av hälsoeffekter av buller fran vägtrafik, tag och flyg i Lerums kommun (Untersuchung von Gesundheitsbeeinträchtigungen hervorgerufen durch Straßenverkehrs-, Zug- und Fluglärm in der Gemeinde Lerum) Technical Report, Västra Götalandsregionens Miljömedicinska Centrum & Sahlgrenska akademin. Gothenburg, Sweden. 2005 May 30; [Google Scholar]
- 12.Franssen EAM, van Wiechen CMAG, Nagelkerke NJD, Lebret E. Aircraft noise around a large international airport and its impact on general health and medication use. Occup Environ Med. 2004;61:405–413. doi: 10.1136/oem.2002.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greiser E, Greiser C, Janhsen K. Night-time aircraft noise increases prevalence of prescriptions of antihypertensive and cardiovascular drugs irrespective of social class - the Cologne-Bonn Airport study. J Public Health. 2007;15:327–337. [Google Scholar]
- 14.Aydin Y, Kaltenbach M. Noise perception, heart rate and blood pressure in relation to aircraft noise in the vicinity of Frankfurt airport. Clin Res Cardiol. 2007;96:347–358. doi: 10.1007/s00392-007-0507-y. [DOI] [PubMed] [Google Scholar]
- 15.Stansfeld SA, Berglund B, Clarc C, et al. Aircraft and road traffic noise and children’s cognition and health: a cross-national study. The Lancet. 2005;365:1942–1949. doi: 10.1016/S0140-6736(05)66660-3. [DOI] [PubMed] [Google Scholar]
- 16.Bullinger M, Gray WE, Hygge S, Evans G. Chronic noise and psychological stress. Psyschological Science. 1995;6:333–338. [Google Scholar]
- 17.Miedema HME, Vos H. Exposure-response relationships for transportation noise. J Acoust Soc Am. 1998;104:3432–3445. doi: 10.1121/1.423927. [DOI] [PubMed] [Google Scholar]
- 18.Schreckenberg D, Meis M. Belästigung durch Fluglärm im Umfeld des Frankfurter Flughafens. Gutachten im Rahmen des Regionalen Dialogforum Flughafen Frankfurt. ZEUS GmbH, Zentrum für angewandte Psychologie, Umwelt- und Sozialforschung, Bochum; Hörzentrum Oldenburg GmbH, Oldenburg. 2006. Jun 30, [Google Scholar]
- 19.Schreckenberg D. Stellungnahme zum Antrag der Landesregierung betreffend Verordnung über die Änderung des Landesentwicklungsplans (LEP) Hessen 2000 - Erweiterung Flughafen Frankfurt/Main (Drucksache 16/6057) Bochum: ZEUS GmbH, Zentrum für angewandte Psychologie, Umwelt- und Sozialforschung. 2007 [Google Scholar]
- 20.Guski R, Ising H, Jansen G, et al. Stellungnahme des Interdisziplinären Arbeitskreises für Lärmwirkungsfragen beim Umweltbundesamt. Berlin: 2004. Fluglärm 2004. [Google Scholar]
- 21.Bartels KH, Ising H. Nachtfluglärmproblematik. Schriftenreihe des Vereins für Wasser-, Boden- und Lufthygiene Berlin. Eigenverlag WaBoLu. 2001;Band 111 [PubMed] [Google Scholar]
- 22.Griefahn B, Jansen G, Scheuch K, Spreng M. Synopse im Auftrag der Fraport AG 2001. Same authors: Fluglärmkriterien für ein Schutzkonzept bei wesentlichen Änderungen oder Neuanlagen von Flughäfen/Flugplätzen. Zeitschrift für Lärmbekämpfung. 2002;49:171–175. [Google Scholar]
- 23.Scheuch K, Spreng M, Jansen G. Fluglärmkonzept der so genannten Synopse auf dem Prüfstand neuer Erkenntnisse der Lärmwirkungsforschung sowie gesetzlicher Rahmenbedingungen. Lärmbekämpfung. 2007;2:135–142. [Google Scholar]
- 24.Klinke R, Klinke O. Schlafen bei geschlossenen Fenstern - ein angemessener Schutz vor Fluglärm? Hessisches Ärzteblatt. 2005;66:242–243. [Google Scholar]
- 25.Ekardt F, Seidel J. Fluglärm zwischen neuerer Rechtsprechung, aktueller Bundesgesetzgebung und dem Europarecht, Neue Zeitschrift für Verwaltungsrecht. 2007;423:421–424. [Google Scholar]
- e1.Bluhm GL, Nordling EK. Community noise and blood pressure - a review of recent Swedish studies on aircraft - and road traffic noise. Proceedings of the Internoise. 2006 Honolulu, Hawaii, USA. [Google Scholar]
- e2.Jarup L, Dudley M-L, Babisch W, et al. Hypertension and exposure to noise near airports (HYENA): study design and noise exposure assessment. Environmental Health Perspectives. 2005;113:1473–1478. doi: 10.1289/ehp.8037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e3.Öhrström E, Barregård L, Andersson E, Skånberg A, Svensson H, Ängerheim P. Annoyance due to single and combined sound exposure from railway and road traffic. J Acoust Soc Am. 2007;122:2642–2652. doi: 10.1121/1.2785809. [DOI] [PubMed] [Google Scholar]
- e4.Greiser E, Janhsen K, Greiser C. Beeinträchtigung durch Fluglärm: Arzneimittelverbrauch als Indikator für gesundheitliche Beeinträchtigungen. Forschungsbericht im Auftrag des Umweltbundesamtes. 2006 Nov [Google Scholar]
- e5.Evans W, Bullinger M, Hygge S. Chronic noise exposure and physiological response: A prosepective study of children living under environmental stress. Psychological Science. 1998;9:75–77. [Google Scholar]
- e6.Hygge S, Evans GW, Bullinger M. A prospective study of some effects of aicraft noise on cognitive performance in school children. Psychological Science. 2002;13:469–474. doi: 10.1111/1467-9280.00483. [DOI] [PubMed] [Google Scholar]
- e7.Haines MM, Stansfeld SA, Head J, Job RFS. Multi-level modelling of aircraft noise on performance tests in schools around Heathrow, London Airport. International Journal of Epidemiology and Community Health. 2002;56:139–144. doi: 10.1136/jech.56.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e8.Clark C, Martin R, van Kempen E, et al. Exposure-effect relations between aircraft and road traffic noise exposure at school and reading comprehension: the RANCH project. American journal of epidemiology. 2006;163:27–37. doi: 10.1093/aje/kwj001. [DOI] [PubMed] [Google Scholar]
- e9.Haines MM, Stansfeld SA, Brentnall S, Head J, Berry B, Jiggins M, Hygge S. The West London Schools Study: The effects of chronic aircraft noise exposure on child health. Psychological Medicine. 2001;31:1385–1396. doi: 10.1017/s003329170100469x. [DOI] [PubMed] [Google Scholar]
- e10.Haines MM, Stansfeld SA, Job SFR, Berglund B, Head J. Chronic aircraft noise exposure, stress responses, mental health and cognitive performance in school children. Psychological Medicine. 2001;31:265–277. doi: 10.1017/s0033291701003282. [DOI] [PubMed] [Google Scholar]
- e11.Miedema HME. Relationships between exposure to single or multiple transportation noise sources and noise annoyance. WHO - Technical meeting on exposure-response relationships of noise on health, Paper 5038933-2002/5. 2002 [Google Scholar]
- e12.Zeus GmbH. Lärmbelästigung in Hessen 2006 - Ergebnisse einer repräsentativen landesweiten Telefonbefragung. Im Auftrag des Hessischen Ministeriums für Umwelt, ländlichen Raum und Verbraucherschutz. 2006. ( http://www.hlug.de/medien/laerm/dokumente/Laemumfrage_Hessen_2006_061123.pdf, 24.09.07) [Google Scholar]
- e13.BVerwG, Bundesverwaltungsgericht. Urteilsbegründung Planfeststellung Flughafen Schönefeld. BverwG 4 A 1075.04. [Google Scholar]
- e14.DIN 1946-2. Raumlufttechnik - Gesundheitstechnische Anforderungen (VDI-Lüftungsregeln) Berlin: Beuth Verlag; 1994. Januar. [Google Scholar]
- e15.DIN 1946-6. Raumlufttechnik - Teil 6: Lüftung von Wohnungen; Anforderungen, Ausführung, Abnahme (VDI-Lüftungsregeln). Berlin: Beuth Verlag; 1998. Oktober. [Google Scholar]
- e16.DIN 1946-6, Norm-Entwurf. Raumlufttechnik - Teil 6: Lüftung von Wohnungen; Allgemeine Anforderungen, Anforderungen zur Bemessung, Ausführung und Kennzeichnung, Übergabe/Übernahme (Abnahme) und Instandhaltung. Berlin: Beuth Verlag; 2006. Dezember. [Google Scholar]
- e17.Kempen v EEMM, Kamp v I. Annoyance from air traffic noise. Possible trends in exposure-response relationships. Report 01/2005 MGO EvK, RIVM, Bilthoven 2005. [Google Scholar]