Abstract
Introduction
Clinical environmental medicine deals with environmental effects on human health in individual patients. Patients seek medical advice for problems of many different kinds that may be due to environmental exposures; such exposures must be considered carefully along with other potential causes. An environmental medical assessment should include thorough medical history-taking and physical examination, the formulation of a differential diagnosis, and (whenever indicated) human biomonitoring, site inspections, and ambient monitoring.
Methods
This review of clinically relevant environment-related health disturbances is based on a selective evaluation of the pertinent literature and of own experiences.
Results
Overall, relevant environmental exposures can be identified in up to 15% of patients who attribute their health complaints to environmental factors. (Clinical disorders are more common and more severe in these patients.) 40% to 75% are found to suffer from other physical and/or emotional conditions without any specific environmental aspect, i.e., without any apparent or verifiable exposure.
Discussion
Despite the relative rarity of verifiable environmentally related health disturbances, these must be clearly identified and delimited to avoid further harmful exposures. Environmental medical counseling should include risk assessment and behavior recommendations for all patients who attribute their medical problems to their environment. Physicians performing specific environmental-medical diagnostic procedures must be aware of their limitations in order to avoid performing tests whose results have no therapeutic consequences and are thus of no help to either the physician or the patient.
Keywords: environmental medicine; environmental pollution; monitoring, consultation; multiple chemical sensitivity
Environmental factors are increasingly being viewed as (contributory) causes of a great variety of health problems, e.g., diseases of the nervous system, airways, or skin, allergies, malignancies, other functional disturbances, non-specific malaise, and anxiety or panic states (1, e1). Clinical environmental medicine is thus confronted by many and varied problems with regard to the effects of environmental influences on individual health.
The most important reasons for the ever-widening discussion of the role of environmental influences in illness are as follows:
The growing number and amount of physical and chemical factors whose long-term effects on human health have not been sufficiently established
Public discussion of proved and potential health risks arising from environmental pollution
The resulting perception of a threat from environmental hazards
Therefore, the tendency to connect ill health with environmental factors.
All this necessitates painstaking assessment of potential environmental pollutants and other competing explanations for illness and malaise. Against this background, this article reviews adequate current diagnostic practices for clinically relevant environmentally related health problems. Furthermore, selected environmental medicine syndromes or constellations of symptoms are discussed in light of current knowledge.
Methods
Standard diagnostic procedures and evaluation strategies were examined in light of a selective analysis of the pertinent literature. The authors also drew on their own long experience of research and clinical practice.
On the basis of the findings, recommendations were then formulated with regard to procedures for investigation of environmental medicine problems and evaluation of the results of environmental medicine examinations.
Investigation procedure
The complexity of history-taking in environmental medicine is shown by the questions listed in box 1 (2). A standardized questionnaire should be used (3).
Box 1. Core questions in an environmental medicine inquiry (from 6, 17).
Where? (site of exposure)
Household (interior), household (surrounding area), kindergarten/school, vehicle (interior), workplace, etc.
Where from? (sources)
Building materials, clothing/jewelry, consumer products, contaminated site/dump, dental materials, electricity supply, furniture and fittings, heating system, industry/commerce, traffic, waste, water supply, etc.
How? (media, pathway)
Air (indoors), air (outdoors), foodstuffs, soil, water (bathing), water (drinking), other media
What? (agents)
Allergens, amalgam, asbestos/artificial mineral fibers, dioxins/furans, dust, electromagnetic fields, formaldehyde, fumes/gas/smoke, indoor air quality, metals/heavy metals, molds, noise, odors, ozone, PCB, plant protection products/pesticides, radioactivity, solvents, UV irradiation, wood preservatives, etc.
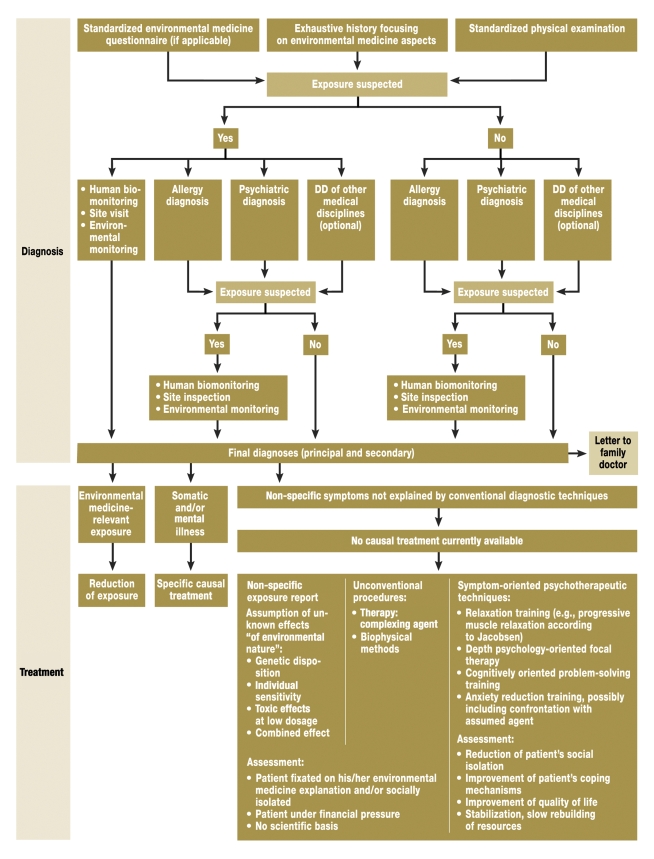
Subsequent specific diagnostic procedures are based on the patient’s symptoms and the possible environmental factors involved (tables 1 and 2, figure) (e2). The variety of possible environmental scenarios and combinations of symptoms does not permit a standardized investigation procedure.
Table 1. Most frequently encountered problems in environmental medicine practice (17): single noxae.
| Problem | Relevant substance | Routes/ssources of uptake | Environmental medicine anamnesis, physical findings | Indication for laboratory tests | Laboratory test/evaluation criteria | Environmental medicine relevance/evaluation |
| Amalgam intoxication | Mercury | Food and drink, dental fillings, ambient air | Number and condition of amalgam fillings | Not in those with fillings, only at patient’s express request | Mercury in urine/HBM values (e10) not indicated:
|
|
| Amalgam allergy | Mercury | Contact allergy | Local mucosal lesions, particularly whitish tartar | Symptoms in proximity to fillings | Epicutaneous test plus clinical findings |
|
| Acrodynia (Feer’s disease, pink disease) | Mercury | Ingestion (calomel, worm powder, tooth powder) or cutaneous uptake (bleaching creams) | Neurological, mental, dermatological symptoms, esp. in young children | Symptoms and/or current exposure | Mercury in urine/HBM values (e10) |
|
| Lead poisoning | Inorganic lead | Consumer products, household dust | Pallor, weakness, vacation souvenirs (e.g., pottery), alternative therapies (ayurveda), paints: white lead | Anemia | Lead in blood/HBM values |
|
| Inorganic lead | Drinking water | Age of house/ age of water supply system | – | Stagnant drinking water/TrinkWV values |
|
|
| Liver cirrhosis in infants | Copper | Drinking water | Preparation of baby foods with soft, acidic well water supplied via copper pipes | Current exposure and unexplained cirrhosis | Drinking water/TrinkWV values |
|
| Cancers | PCB | Food and drink, ubiquitous in environmental media; joint sealants etc. in interiors | – | At patient’s request | PCB congeners in blood/selection and reference values: UBA | |
| Wood preservative syndrome | PCP | Indoor air, treated wood products | – | If current indoor source demonstrated | PCP in urine/HBM values |
|
| Neural lesions | Pyrethroids and other biocidal agents | Indoor pest control, textiles, foodstuffs | Acute after pest control measures: mucosal irritation, rarely perioral tingling | Symptoms and current exposure | For example pyrethroid metabolites in urine/HBM values | Preventive reduction of exposure |
| Lung cancer | Radon | Geographical differences | Gneiss-granite area [see also radon atlas (24)], construction method | Preventive, at patient’s justified request | Precise information only via radon measurement (dosimetry) |
ArgeBau, Arbeitsgemeinschaft für Städtebau, Bau- und Wohnungswesen (Joint Working Group for Town Planning, Construction and Housing); DMPS, (RS)-2.3-dimercaptopropane-1-sulfonate; HBM, human biomonitoring; PCB, poly-chlorinated biphenyls; PCP, pentachlorophenol; TrinkWV, Trinkwasserverordnung (German Drinking Water Ordinance); UBA, Umweltbundesamt (German Federal Environment Agency)
Table 2. Frequently encountered problems in environmental medicine practice (17): constellations of symptoms.
| Problem | Relevant substance | Routes/sources of uptake | Environmental medicine anamnesis, physical findings | Indication for laboratory tests | Laboratory test/evaluation criteria | Environmental medicine relevance/evaluation |
| Indoor mucosal irritation | Formaldehyde | Ambient air, indoor air (e.g., tobacco smoke), consumer products: furnishings, foam rubber, materials, disinfectants, etc. | Irritation of mucosa and airways | Symptoms and current exposure | Indoor air/BfR safe level 0.124 mg/m3 HBM: not indicated owing to endogenous production paints, cleaning |
|
| Indoor mucosal irritation, central nervous disorders | Volatile organic compounds | Ambient air, solvents (e.g., from paints), new buildings, renovation | Irritation of mucosa and airways | Symptoms and current exposure | Indoor air/UBA reference and threshold values (16) |
|
| Allergy, infection, and/or intoxication from indoor mold | Mold spores and components | Airways, skin | Irritation of mucosa and airways, immune status: aspergillosis or asthma, dyspnea and/or pulmonary infiltrates | Symptoms and current visible exposure in inhabited rooms | Possibly indoor air and material samples, UBA (25) |
|
| Sick building syndrome (SBS) | No specific substance | Indoor air/mucosae | Irritation of ocular mucosae and upper and lower airways, non-specific symptoms | Symptoms and current exposure, other people also affected | Site inspection and standardized interview regarding interior perceptions and health problems | Symptoms are as a rule primarily related to factors from the following areas:
|
| Electrosensitivity | High-frequency electromagnetic fields, e.g., from cell phone masts | Field exposure, transdermal | No acute symptoms, no warming-up effect expected at exposure below threshold values | Interior space/Ordinance on Electromagnetic Fields*1 |
|
|
| Multiple chemical sensitivity | – | – | No typical constellation of symptoms known, neurovegetative symptoms frequent | Typical symptoms and history of specific exposure |
|
*1 26th Ordinance for Enforcement of the German Federal Immission Protection Law (Ordinance on Electromagnetic Fields – 26.BImSchV) of 16.12.1996 (BGBI. I S. 1966 ff.); BfR, Bundesinstitut für Risikobewertung (German Federal Institute for Risk Assessment); BfS, Bundesamt für Strahlenschutz (German Federal Office for Radiation Protection); UBA, Umweltbundesamt (German Federal Environment Agency)
Figure.
Diagnostic procedure and treatment options in environmental medicine (after Wiesmüller 2002 [18] and Herr et al. [e18]). Principal diagnoses explain all of the patient’s symptoms, while secondary diagnoses explain only some of the symptoms. DD, differential diagnosis
Table 1 lists a number of health problems that can be caused by various single environmental noxae, together with recommendations on how one should proceed. Many environmental medicine issues can be clarified by specific diagnostic tests and treatment can be instituted if appropriate. In patients with multiple non-specific symptoms the diagnostic approach should be interdisciplinary, with equal importance attached to organic and psychic aspects (4, e3).
On the one hand, most patients who assume their illness is caused by environmental factors can actually be assigned other clinical diagnoses. Examples are respiratory diseases (ICD J; ca. 55%), skin diseases (ICD L; ca. 30%), and gastrointestinal diseases (ICD K; ca. 20%). Evidence of an environmental cause is found in only up to 15% of patients (4).
On the other hand, in many cases these organic disorders are accompanied by somatization disorders (ICD F). The perceived environment-related illness thus forms part of the disorder. The reported proportion of patients with mental disorders ranges from 40% to 75% (4–8). In daily clinical practice, this means that the physical symptoms described cannot be explained adequately, if at all, by the organic disease; somatization is in many cases the central problem. Most patients are not satisfied with this explanation of the cause of their symptoms. On the basis of such a diagnosis, however, the spectrum of treatment offered can include psychotherapy (figure). Following interdisciplinary clinical diagnosis, more than one third of patients pursue this option (4).
Alongside the general clinical investigations such as lung function tests, sonography, and laboratory tests, specific environmental-medical diagnostic techniques can be employed. The most important procedures are investigations of bodily fluids and tissues (human biomonitoring), site inspections, and analyses in environmental media (environmental monitoring). Uncertainty and, in some cases, the lack of established diagnostic procedures can lead to the employment of tests of dubious validity. This danger exists, for example, when organic pathology is demonstrated due to subtoxic levels of exposure to harmful substances. Diagnostic techniques that are not accepted in other clinical disciplines have no place in environmental medicine.
Human biomonitoring
Human biomonitoring measures the concentrations of harmful substances in bodily fluids and tissues (10). The indication for human biomonitoring is decided on the basis of information provided by the patient, previous findings, if any, and the findings of a site inspection. Human biomonitoring can also help to convince the patient of a differential-diagnostic explanation of his/her symptoms and prevent or terminate "doctor hopping."
Because the results can be influenced by many different factors, the planning, execution, and analysis of human biomonitoring must be preceded by careful consideration of quality assurance and evaluability (box 2) (11, e4). One study of 99 patients showed that about 20% of the preliminary tests in human biomonitoring investigations were made in unsuitable media (box 3) (e5).
Box 2. Human biomonitoring (HBM): quality assurance and meaning of the values HBM-I and HBM-II.
The HBM values are laid down by the Human Biomonitoring Commission of the German Federal Environment Agency. In contrast to reference values, which reflect the average exposure of a population group to a given harmful substance, regardless of its relevance to health, the HBM values serve to judge the health risks of contaminants in biological materials (blood, urine, etc.). However, HBM values have been established only for a small number of selected substances. The HBM-I value (alert level) is the concentration below which a substance is thought to be harmless. Above the HBM-II value a detrimental effect on health is possible and urgent action is required to reduce the burden (11).
Quality assurance in HBM
Who performed/should perform the measurements?
What was/should be measured?
When was/should it be measured?
Where was/should it be measured?
Why was/should it be measured?
How was/should it be measured?
How can the findings be interpreted?
Meaning of the HBM values
At low concentrations:
Impairment of health: currently considered harmless
Action required: none
At concentrations above the HBM-I value (alert level):
Impairment of health: cannot be excluded with sufficient confidence
-
Action required:
Check the values (analysis, time course)
Search for specific sources
Where appropriate, reduction of burden (if attainable at reasonable cost)
At concentrations above the HBM-II value (intervention/action level):
Impairment of health: possible
-
Action required:
Environmental medicine counseling
Urgent measures to reduce the burden
Box 3. Example: Mucosal irritation by volatile substances in the household.
A 34-year-old woman (dental assistant, trade school teacher for 12 years) attended the environmental medicine clinic and stated her suspicion that she was suffering from multiple chemical sensitivity (MCS). She reported that her symptoms had begun with irritation of the eyes and the nasal/respiratory tract ("feels like breathing fire") after she moved into an apartment in a newly erected building seven months earlier and became worse after a carpet was laid. Currently the symptoms were also occurring in recently cleaned rooms. She said the staff at a university dermatology hospital had suspected MCS. After her stay in hospital she had moved out but had still paid for the apartment to be monitored. She had informed herself about MCS and feared her symptoms would become chronic and more wide-ranging.
Preliminary findings:
Human biomonitoring (HBM): Tested for pyrethroids, formaldehyde, and pentachlorophenol on 10th day after admission to the hospital: no abnormal findings.
Household monitoring: Increased concentrations of volatile substances, alkanes, and formaldehyde demonstrated in indoor air.
Evaluation by environmental medicine service: Because biological half-lives were not taken into account, the HBM findings could not be used to determine whether the patient was exposed to relevant amounts of harmful substances in her apartment. On the other hand, the household monitoring revealed concentrations of volatile compounds (alkanes and formaldehyde from the floor covering) potentially sufficient to affect health, although the apartment had been completed only six months previously.
Diagnosis: Mucosal irritation of eyes and airways by volatile substances in a new apartment.
Recommendation: After completion of the renovations advised on the basis of the household monitoring, the patient should try moving back into the apartment and report any reoccurrence of symptoms to the environmental medicine service; no evidence of MCS.
Course: The patient moved back into the new apartment and experienced no reoccurrence of the symptoms outlined above for over two years.
Remarks: Inappropriate and uncritically conducted human biomonitoring increases the risk of unsubstantiated, premature suspected diagnoses that can greatly unsettle the patient; in addition, genuinely existing noxae may be overlooked.
The mere demonstration of the presence of a substance, however, cannot be equated with a toxic effect or disease. For example, pentachlorophenol (PCP), which was used in Germany up to the end of the 1980s, is still regularly demonstrated in the course of human biomonitoring. Nevertheless, it can be classified as a health risk only in those individuals in whom toxicologically established threshold values are exceeded.
Ideally the human toxicological relevance of the results should be classified by means of the human biomonitoring values HBM-I and HBM-II (12). If the HBM-I value is found to be exceeded, a follow-up examination and possibly a search for the source of contamination are indicated. No immediate danger to health is assumed. If the HBM-II value is exceeded, however, urgent steps must be taken to identify the source and reduce or end the exposure. Details on derivation of the HBM values can be found in box 2.
If toxicologically derived thresholds other than the HBM values, such as the German BAT value (biological tolerance value for occupational exposures) or reference values, are used for evaluation, the physician should check for what population and following what toxicological concept they were derived. Examples of population groups are employees, men, women, children, or representative samples of the general population. Toxicological concepts consider whether healthy persons have suffered occupational exposure for a limited period of time or whether healthy and particularly sensitive individuals have experienced lifelong exposure. Since physicians inexperienced in environmental medicine may find it difficult to determine which is the case, it is recommended to engage the help of experts, e.g., a more experienced colleague or the local environmental medicine service.
According to the current state of knowledge in environmental medicine, investigations of susceptibility monitoring, e.g., on genetic sequence variations (polymorphisms) of enzyme systems that metabolize foreign substances (13) or lymphocyte transformation tests (LTT) for demonstration of allergic reactions to environmental agents (14), are not applicable to the evaluation of individual health complaints. The findings on genetic polymorphisms yield no further-reaching information, and the informative power of the LTT is inadequate as yet.
Site inspection and environmental monitoring
The source and precise nature of the harmful substance can be identified by a site inspection and environmental monitoring. In most cases, the patient’s private space, his/her household and the immediate surroundings are investigated and analyses in environmental media (environmental monitoring) are performed if appropriate.
Physicians inexperienced in environmental medicine will have difficulty carrying out environmental monitoring. For example, a university environmental medicine service evaluated the preliminary findings in 99 patients. The physicians who first treated these patients requested a total of 545 single-substance analyses, but their colleagues in the environmental medicine service considered only 62 (11%) of these analyses necessary (e5).
The physician who has grounds to suspect that a patient is being harmed by environmental factors should recommend investigation by qualified personnel, followed by joint evaluation of the findings with an expert. Suitably qualified staff can be contacted via regional health offices, regional offices for environmental protection, or regional university environmental medicine services and helplines.
The findings of interior environmental monitoring should be evaluated in light of the recommendations of the ad hoc committee of the Interior Air Hygiene Commission (IRK, Innenraumlufthygienekommission) of the German Federal Health Office and the Interior Air Subcommittee of the Environmental Hygiene Committee of the Joint Working Group of the State Health Authorities (AOLG, Arbeitsgemeinschaft der Obersten Landesgesundheitsbehörden) (15). Particularly for the concentrations of volatile organic compounds there is an evaluation scheme based on a cumulative index of total volatile organic compounds (TVOC) (16). This enables preliminary estimation of the exposure in daily clinical practice.
Analyses of water, soil, air and foodstuffs may be the responsibility of the environmental or health authorities. It is thus advisable to contact the authorities, e.g., the local Health Office, in advance. Environmental monitoring is not generally covered by health insurance. Unless the above-mentioned authorities are responsible, the patient him-/herself must bear the costs of the environmental medicine inspection of the household and of the environmental monitoring (17).
Counseling on the relation of symptoms to environmental factors
According to data from university environmental medicine institutes and public environmental medicine services, the proportion of patients with symptoms caused by environmental factors varies from 0% to 15% (table 1). In contrast, environmental medicine physicians not attached to such institutions report figures ranging from 36% to 45% (1, 4). It should be noted that these publications related to case series. One possible reason for the discrepancy might be that clearly environment-related health problems are diagnosed by independent physicians, while more complex cases are concentrated at university facilities. Another feasible explanation is that the budget difficulties experienced by non-hospital physicians prevent them performing the exhaustive differential diagnostic work-up required for environment-related disorders.
Risk communication, oriented on the patient’s anxieties and subjective illness models, represents a particular challenge for the environmental medicine practitioner (e6). Environmental medicine counseling includes recommendations and suggestions that can often be made before detailed investigation of the individual case. This embraces, for example, advice on the risks from amalgam in dental fillings, radiation from cell phones and masts, and fine-particle air pollution. Also included is explanation of the scope and limitations of investigations, together with their suitability and utility, and of their consequences (figure, tables 1 and 2) (18).
Should it emerge during the process of diagnosis that the patient’s symptoms are due to chemical substances or products (e7), the physician is legally obliged to make a report to the Poison and Product Documentation Centre of the German Federal Institute for Risk Assessment (BfR, Bundesinstitut für Risikobewertung). An example would be colic, pallor, and fatigue indicating lead poisoning from drinking tea out of a glazed ceramic beaker brought back from a foreign vacation.
Constellations of symptoms in environmental medicine
In environmental medicine there are various syndromes or constellations of symptoms that describe patients’ complaints but whose causes are inconsistently and inadequately explained. Examples are multiple chemical sensitivity (MCS), electrosensitivity (ES), and sick building syndrome (SBS). Under conditions of general daily population exposure, the supposed environment-associated health disorders are observed only in isolated cases. Reliable German data on the occurrence of these symptom complexes are almost non-existent. A representative, population-based survey on MCS conducted by the Allensbach polling institute in 2032 adults in Germany revealed a frequency of 9% for self-reported MCS (sMCS) and 0.5% for MCS diagnosed by a physician (19). SBS is described in more detail in the next section, while table 1 gives some information on the other syndromes and constellations of symptoms.
Sick building syndrome
The term "sick building syndrome" is employed when people using a particular building report non-specific health complaints involving especially the eyes, the respiratory tract, the skin, and the central nervous system. The most widespread and most frequently used classification of SBS is that published in 1998 by Mølhave (20), reproduced in box 4. Physical, chemical, biological, personal, and psychosocial factors may all have a causative role. SBS can be assumed to comprise a multifactorial event in which various simultaneously occurring factors combine in different ways to result in the syndrome.
Box 4.
Operationalized classification of sick building syndrome (SBS) according to Mølhave (20)
The symptoms most frequently reported by users of buildings where SBS is suspected can be classified in the following five categories:
Irritation of eyes, nose, and/or throat
Skin irritation
Symptoms associated with the nervous system
Non-specific hypersensitivity
Sensations of smell and taste
The symptoms occur only in a particular building.
In the absence of a binding definition and of representative epidemiological studies, there are no reliable figures on the prevalence of SBS. A preliminary study in 613 people carried out in the framework of the joint project "ProKlimA," started in Germany in 1994, showed that 30% to 40% of employees report non-specific malaise (e8). Petrovitch estimated that at least 1 million people in Germany had SBS of some degree (e9).
It must be assumed that the loss of productivity arising from SBS has appreciably negative consequences on the economy. In the USA, for example, the economic consequences of SBS are estimated at US$ 10 to 70 billion for commercial buildings (21). This is made up of the costs of medical care, absence from work (150 million working days), and loss of productivity (22). There are no comparable data for Germany.
Important data were yielded by the German ProKlimA study, which enabled the evaluation of environmental factors in buildings in the context of SBS through a comprehensive workplace-related survey of exposure. This study showed by means of multiple logistic regression analyses that the occurrence of SBS symptoms (self-reported sensory and physical symptoms, non-specific malaise) are associated in particular with the characteristics of those interviewed (gender, age, allergic diseases) and of their work (work requirements, job satisfaction). Only in a few isolated cases in the sample population did typical interior environmental influences such as room air quality and indoor climate have a measurable effect on the symptoms. Personal views and expectations of people using the room, however, were found to have a clear association with their symptoms (23). Specific techniques for objective demonstration of SBS-associated symptoms in daily clinical practice are either lacking or are not routinely applicable. A physician who suspects a patient may have SBS should initiate an investigation by qualified environmental medicine personnel. The findings should then be discussed together with the experts who conducted the investigation (see above, "Site inspection and environmental monitoring"). Strategies for dealing with SBS have been developed, based on international experience (23).
Conclusions
Both environmental medicine clinicians and family doctors have to deal with potential health risks from physical, chemical and biological factors in various environmental media and in the daily life environment. They are often the first port of call for an increasing number of patients seeking advice on mostly non-specific physical, mental, and/or psychosocial complaints and symptoms that only rarely can be connected with clearly identifiable environmental factors to which a name can be attached. In view of the resulting uncertainties, the following points should always be considered:
Exposure to a relevant environmental agent can be identified in no more than 15% of patients whose symptoms are suspected to be of environmental origin.
Somatization disorders can be diagnosed in 40% to 75% of patients with environment-related complaints.
Human biomonitoring and the site inspection with environmental monitoring must be carried out by experts.
To date, genetic or immunological tests are of no great use in clinical environmental medicine.
In contrast to health-relevant environmental pollution by specific substances, to date there is no scientific consensus on environmental medical syndromes such as SBS or MCS.
Acknowledgments
The authors thank Dr. Heinzow for detailed expert advice and the "Methods and Quality Assurance in Environmental Medicine" commission of the Robert Koch Institute for valuable comments on the manuscript.
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Nowak and Prof. Herr have participated in studies that benefited from external funding via the Robert Koch Institute and have received fees for lectures.
The remaining authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Hornberg C, Malsch AKF, Weißbach W, Wiesmüller GA. Umweltbezogene Gesundheitsstörungen, Erfahrungen und Perspektiven umweltmedizinischer Patientenversorgung. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2004;47:780–794. doi: 10.1007/s00103-004-0875-7. [DOI] [PubMed] [Google Scholar]
- 2.Fülgraff G. Risikobegriff und Risikokommunikation in der Umweltmedizin. Gesundheitswesen. 1998;60(Suppl. 1):4–10. [PubMed] [Google Scholar]
- 3.Eis D. Methoden und Qualitätssicherung in der Umweltmedizin. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2000;43:336–342. [Google Scholar]
- 4.Herr C, Kopka I, Mach J, et al. Interdisciplinary diagnostics in environmental medicine - outcome and follow up in patients with chronic unexplained health complaints. Int J Hyg Environ Health. 2004;207:31–44. doi: 10.1078/1438-4639-00263. [DOI] [PubMed] [Google Scholar]
- 5.Black DW, Okiishi C, Schlosser S. A nine-year follow-up of people diagnosed with multiple chemical sensitivities. Psychosomatics. 2000;41:253–261. doi: 10.1176/appi.psy.41.3.253. [DOI] [PubMed] [Google Scholar]
- 6.Bornschein S, Hausteiner C, Zilker T, Bickel H, Forstl H. Psychiatric and somatic morbidity of patients with suspected multiple chemical sensitivity syndrome (MCS) Nervenarzt. 2000;71:737–744. doi: 10.1007/s001150050658. [DOI] [PubMed] [Google Scholar]
- 7.Umweltbundesamt. Multizentrische Studien zum MCS-Syndrom (Multiple Chemische Sensitivität) 2005. 2007. Sep 5, [Google Scholar]
- 8.Hausteiner C, Bornschein S, Zilker T, Henningsen P, Forstl H. Dysfunctional cognitions in idiopathic environmental intolerances (IEI) - an integrative psychiatric perspective. Toxicol Lett. 2007;171:1–9. doi: 10.1016/j.toxlet.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Wüthrich B, Frei PC, Bircher A, et al. Bioresonanz - diagnostischer und therapeutischer Unsinn. Acta Dermatologica. 2006;32:73–77. [Google Scholar]
- 10.Umweltbundesamt. Human-Biomonitoring: Definitionen, Möglichkeiten und Voraussetzungen. Berichte. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 1996;39:213–214. [Google Scholar]
- 11.Umweltbundesamt. Konzept der Referenz- und Human-Biomonitoring-Werte (HBM) in der Umweltmedizin. Berichte. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 1996;39:221–224. doi: 10.1007/s00103-009-0902-9. [DOI] [PubMed] [Google Scholar]
- 12.Umweltbundesamt. Kommission Human-Biomonitoring (HBM) 2007. Jun 18, [Google Scholar]
- 13.Robert-Koch-Institut. Genetische Polymorphismen (Sequenzvariationen) von Fremdstoff-metabolisierenden Enzymen und ihre Bedeutung in der Umweltmedizin. Mitteilung der RKI-Kommission. „Methoden und Qualitätssicherung in der Umweltmedizin“. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2004;47:1115–1123. doi: 10.1007/s00103-004-0931-3. [DOI] [PubMed] [Google Scholar]
- 14.Robert-Koch-Institut. KMuQidU: Diagnostische Relevanz des Lymphozytentransformationstestes in der Umweltmedizin. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2002;45:745–749. [Google Scholar]
- 15.Umweltbundesamt. Kommission Innenraumlufthygiene (IRK) 2007. Jun 18, [Google Scholar]
- 16.Umweltbundesamt. Beurteilung von Innenraumluftkontaminationen mittels Referenz- und Richtwerten. Handreichung der Ad-hoc-Arbeitsgruppe der Innenraumlufthygiene-Kommission des Umweltbundesamtes und der Obersten Landesgesundheitsbehörden. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2007;50:990–1005. doi: 10.1007/s00103-007-0290-y. [DOI] [PubMed] [Google Scholar]
- 17.Otterbach I, Bergold M, Beyer M, Eikmann T, Herr C. Individuelle Gesundheitsleistungen (IGeL) in der Umweltmedizin - Teil 1. Umweltmed Forsch Prax. 2006;11:173–183. [Google Scholar]
- 18.Wiesmüller GA. Möglichkeiten und Grenzen der Diagnostik in der Umweltmedizin. In: Dott W, editor. Publikationsreihe des interdisziplinären Umwelt-Forums der RWTH Aachen. Akademische Edition Umweltforschung. Band 21. Aachen: Shaker Verlag; 2002. [Google Scholar]
- 19.Hausteiner C, Bornschein S, Hansen J, Förstl H, Zilkler T. Multiple Chemical Sensitivity und subjektive Chemikalienempfindlichkeit in Deutschland - Ergebnisse einer bevölkerungsbasierten Befragung. Umweltmed Forsch Prax. 2004;9:281–286. [Google Scholar]
- 20.Mølhave L. The sick buildings and other buildings with indoor climate problems. Environ Internat. 1989;15:65–74. [Google Scholar]
- 21.Mendell M, Fisk W, Kreiss K, et al. Improving the health of workers in indoor environments: Priority research needs for a national occupational research Agenda. Am J Public Health. 2002;92:1430–1440. doi: 10.2105/ajph.92.9.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bas GSD, Weißbach W, Hornberg C, Dott W, Wiesmüller GA. Socio-economic relevance of sick building syndrome - a literature study. In: Yang ZB, Don X, Zhao R, editors. Proceedings of Indoor Air ’05. Beijing, China: Tsinghua University Press; 2005. pp. 402–406. [Google Scholar]
- 23.Bischof W, Wiesmüller GA. Das Sick Building Syndrome (SBS) und die Ergebnisse der ProKlimA-Studie. Umweltmed Forsch Prax. 2007;12:23–42. [Google Scholar]
- 24.Bayerisches-Landesamt-für-Umwelt. Infozentrum. UmweltWissen 2007; 2007. Jul 13, Radon. [Google Scholar]
- 25.Umweltbundesamt. Leitfaden zur Vorbeugung, Untersuchung, Bewertung und Sanierung von Schimmelpilzwachstum in Innenräumen („Schimmelpilz-Leitfaden“) 2008. May 14, [Google Scholar]
- e1.Wiesmüller G, Ebel H, Schulze-Röbbecke R, Kunert H. 1st Aachen Symposium „Environment and Psyche“ (Editorial) Zentralbl Hyg Umweltmed. 1999;202:79–84. [PubMed] [Google Scholar]
- e2.Neuhann H-F, Wiesmüller GA, Hornberg C, Schlipköter H-W. Wichmann H-E, Schlipköter H-W, Fülgraff G, editors. III-2.4 Aufgaben und Strukturen umweltmedizinischer Beratungsstellen in Deutschland. Handbuch der Umweltmedizin. 2002;Band 25 Landsberg/Lech ecomed Medizin. [Google Scholar]
- e3.Eikmann T. Zentrum für Klinische Umweltmedizin: Interdisziplinäres Versorgungskonzept. Dtsch Arztbl. 1997;94(5):A 214. [Google Scholar]
- e4.Umweltbundesamt. Qualitätssicherung beim Human-Biomonitoring. Berichte. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 1996;39:216–221. [Google Scholar]
- e5.Herr C, Kopka I, Mach J, Eikmann T. Beurteilung des Einsatzes von Human- und Ambientemonitoring. In: Nowak D, Praml G, editors. Perspektiven der Klinischen Arbeits- und Umweltmedizin: Stäube - Feinstäube - Ultrafeinstäube. Fulda: Rindt-Druck; 2002. pp. 288–291. [Google Scholar]
- e6.Robert-Koch-Institut. Kommission: „Methoden und Qualitätssicherung in der Umweltmedizin“. 2007. Jul 13, [Google Scholar]
- e7.Kirchgatterer A, Rammer M, Knoflach P. Gewichtsverlust, Bauchschmerzen und Anämie als Folgen einer Urlaubsreise. Dtsch med Wochenschr. 2005;130:2253–2256. doi: 10.1055/s-2005-918557. [DOI] [PubMed] [Google Scholar]
- e8.Bullinger M. Stand des laufenden BMBF-Vorhabens „Untersuchung zu positiven und negativen Wirkungen raumlufttechnischer Anlagen auf Gesundheit, Leistungsfähigkeit und Befindlichkeit“. In: Dompke M, Kruppa B, Mayer E, editors. Sick Building Syndrome II. Forschungsstand und -umsetzung. Bonn: Verlag TGC GmbH; 1996. pp. 132–155. [Google Scholar]
- e9.Petrovitch A. Sick-Building-Syndrome: Umweltmed Forsch Prax. 1996;3:143–150. [Google Scholar]
- e10.Biomonitoring-(HBM)-Werte. Bekanntmachung. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 1999;42:522–532. [Google Scholar]
- e11.von Muhlendahl KE. Dental amalgam and feer disease. European Journal of Pediatrics. 1995;154:585–586. doi: 10.1007/BF02074842. [DOI] [PubMed] [Google Scholar]
- e12.Umweltbundesamt. Epidemiologische Untersuchung zum Risiko frühkindlicher Lebererkrankungen durch Aufnahme kupferhaltigen Trinkwassers mit der Säuglingsnahrung. Forschungsbericht 2003. Berlin: Umweltbundesamt; 2003. [Google Scholar]
- e13.Kommission der Europäischen Gemeinschaften. Strategie der Gemeinschaft für Dioxine, Furane und polychlorierte Biphenyle. KOM. 2001;593 endg. - Amtsblatt C 322 vom 17.11.2001 http://europa.eu.int/ [Google Scholar]
- e14.Projektgruppe „Schadstoffe“ der Fachkommission Baunormung der ARGEBAU. Richtlinie für die Bewertung und Sanierung PCB-belasteter Baustoffe und Bauteile in Gebäuden (PCB-Richtlinie) 1994, korrigiert. 2001. [Google Scholar]
- e15.Otto M, von Mühlendahl KE. ALLUM - das Informationsangebot zu Allergie, Umwelt und Gesundheit. Radon. 2006. www.allum.de/noxe/radon.html. [Google Scholar]
- e16.Bayrisches-Landesamt-für-Umwelt. Radon. Infozentrum UmweltWissen. 2007. [Google Scholar]
- e17.Sechsundzwanzigste Verordnung zur Durchführung des Bundes-Immissionsschutzgesetzes (Verordnung über elektromagnetische Felder-26. BImSchV) 1996. Dec 16, (BGBl. I S.1966ff.) [Google Scholar]
- e18.Herr C, Gieler U, Eikmann T. Therapie Teil 2. Therapeutische Maßnahmen aus Sicht des HZKUM. 05.02, 1-14. In: Beyer A, Eis D, editors. Praktische Umweltmedizin. Springer Loseblattsystem. Berlin, Heidelberg, New York: Springer; 2000. [Google Scholar]