Abstract
Introduction
Intermittent paradoxical closure of the vocal cords can induce major attacks of dyspnea. Such attacks, called "vocal cord dysfunction" (VCD), are an important element in the differential diagnosis of intractable bronchial asthma.
Methods
Selective review of the literature.
Results
The etiology of VCD is unclear. Its clinical manifestations can mimic those of bronchial asthma. Standard asthma medication fails to improve the dyspnea of VCD, which is subjectively perceived as life-threatening. Consequently, patients with unrecognized VCD may be treated with very high doses of anti-asthmatic medication, including systemic corticosteroids, leading to major iatrogenic morbidity. No prospective studies are available on this subject to date. Experts estimate that 3% to 5% of persons diagnosed as having bronchial asthma actually suffer from VCD. Because of the brevity of the attacks, which usually last only 1–2 minutes, VCD is difficult to diagnose with the methods generally used to diagnose asthma. Evidence-based therapeutic approaches are still lacking, but speech therapy, including special breathing techniques with relaxation of the throat, seems to control the attacks of dyspnea in most patients.
Discussion
An improved knowledge of the clinical manifestations of VCD can help physicians diagnose it correctly. Early diagnosis can prevent prolonged erroneous treatment based on a false diagnosis of bronchial asthma and thereby obviate the iatrogenic side effects of long-term corticosteroid therapy, as well as the resulting economic losses.
Keywords: bronchial asthma, respiratory disease, dyspnea, asthma therapy, diagnosis
The expression "vocal cord dysfunction" (VCD) is not very precise. Other synonyms include "laryngeal asthma," "hysterical croup," and "psychogenic stridor." Laryngologists tend to assume that this term means vocal abnormalities, and this often causes confusion.
VCD is defined as intermittent, functional laryngeal obstruction causing dyspnea during inspiration or expiration (1–3). VCD may occur in isolation. Alternatively, it may be an additional cause of dyspnea in bronchial asthma and is responsible for the portion of the dyspnea which cannot be treated with drugs. It follows that VCD is not an exclusion diagnosis for bronchial asthma.
The present article is based on a selective literature search, using the key words "vocal cord dysfunction," "dyspnea," and "intractable asthma." The level of evidence of the definition of the condition, diagnosis, and treatment is that of expert opinions, as there have been no prospective randomized studies and no large epidemiological investigations. VCD is still little known and the therapies are all nonpharmacological. It often even happens that high doses of drugs are discontinued. No financial support has been available for studying the causes of VCD and for establishing evidence-based recommendations for treatment.
The clinical picture was mentioned as "hysteric croup" as early as 1842 (4). In 1977, the term "brittle asthma" was coined for intractable asthma, with two different clinical manifestations. Type B was characterized as intractable, persistent asthma, with dyspnea from one moment to the next, as well as unjustified insinuation of emotional asthma and chaotic peak flow variability–an apt description of VCD (5, 6). The term "vocal cord dysfunction" was established in 1983 (1, 2).
Epidemiology
There is no precise information on the prevalence of VCD in adults. VCD is apparently the cause of between 2.5% and 22% of cases of intensive emergency care for dyspnea (7). The author prospectively examined a group of pulmonology rehabilitation patients who had been admitted to hospital and concluded that the prevalence of VCD, as the exclusive or contributory cause of dyspnea, was between 3% and 5% (8).
Newman et al. performed a prospective evaluation of 167 patients with intractable asthma and concluded that VCD was the reason for treatment failure in 30% of cases. About one third of these patients exclusively exhibited VCD; about two thirds suffered from both VCD and asthma (3).
15% of US-American recruits exhibited VCD as a cause of stress-induced asthma (9). About 5% of US-American Olympia athletes, particularly those exposed to cold air, developed dyspnea as a result of laryngeal dysfunction or VCD (10).
The prevalence of VCD in children and adolescents admitted to hospital for bronchial asthma may be as high as 14% (11). About 75% of these patients suffered from both asthma and VCD (12).
If it is assumed that the prevalence of VCD among asthmatics is 3% to 5%, this corresponds to more than 250 000 patients for the whole of Germany, so that VCD patients can likely be found in every general practice (8).
Malfunction of the larynx and pathophysiology
The essential functions of the pharynx are phonation, thoracoabdominal stabilization, and protection of the lower respiratory tract (for example, during cough). Because of its complex neuromuscular structure and variety of motoric patterns, the larynx is the most functionally sensitive part of the respiratory tract. For this reason, laryngeal malfunction may be due to a variety of causes.
The cause of VCD has not been exactly clarified. Experts assume that there is no single pathophysiological cause of VCD, but that it is more likely to be the result of different factors. It was originally thought that the causes were only psychosomatic (13).
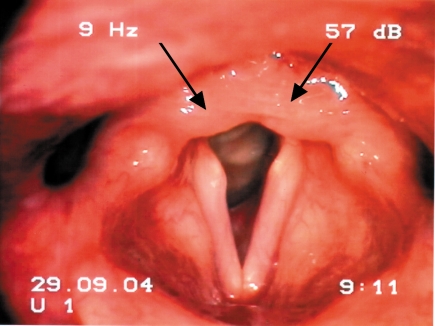
Psychosomatic VCD symptoms are regarded as a false alarm from the central respiratory control system. If the patient has a tendency to anxiety or panic, there may be a smooth transition to hyperventilation symptoms (11). Nevertheless, this complex condition cannot be explained by a single cause. Moreover, there are also purely organic pathological mechanisms, including "postnasal drip" (PND), gastroesophageal reflux (GER) (14) and, especially, laryngopharyngeal reflux (LPR) (15), with microaspiration, swallowing abnormalities, and long-term irritation on inhalation. Endoscopic demonstration of posterior laryngitis is suggestive, although not pathognomic (figure 1).
Figure 1.
Posterior laryngitis (arrows) due to reflux linked to irritation (laryngopharyngeal reflux, LPR)
VCD as hyperreactivity of the larynx
If there is above-threshold laryngopharyngeal irritation accompanied by the risk of aspiration–for example, from reflux–sudden adduction of the vocal cords is a sensible protective mechanism for the lung. Laryngospasm is complete closure of the larynx without stridor, independently of the respiratory cycle, and may be regarded as a full-blown form of a protective mechanism. Laryngospasm lasts at the most for seconds and is therefore distinct from the typical VCD symptoms.
Recurrent irritation of the laryngopharyngeal mucus membrane evidently leads to a reduction in the threshold trigger for protective reflexes (which would be abortive with laryngospasm). Even slight stimuli can then trigger a VCD attack (16).
Possible triggers include neurological diseases and injuries to the cervical spine. Acute laryngitis or recurrent damage can promote the initial manifestation or enhance prior symptoms (15). Patients with monolateral or bilateral pareses of the vocal cords often suffer not only typical VCD attacks, but also stress dyspnea on inspiration. This is connected with the relative constriction of the larynx due to inadequate opening of the vocal cords. This form of dyspnea stops at once when the exertion has ended (17).
"Vocal cord dysfunction" is not a homogenous clinical picture, but a complex and multifactorial disease, for which the causal pathological mechanisms have not yet been reliably clarified.
Clinical presentation
As there may be a multitude of trigger mechanisms and the intensity of VCD-linked dyspnea may be very changeable, the clinical symptoms may be confusingly variable.
Dyspnea mostly occurs as an attack during inspiration; this starts rapidly and is usually hyperacute. The dyspnea appears from one breath to the next. The symptoms are self-limiting and usually last for between 30 seconds and a few minutes. In a few cases, they may last longer (18). The constriction in the respiratory tract is mostly in the neck or upper trachea. The triggers differ between individuals. Frequent triggers include:
Inhaled irritants (perfume, disinfectants)
Dysphagia
Physical exertion
Psychological excitement.
VCD is typically stimulated by a dry cough. If patients complain of sudden dyspnea when they have been sleeping, reflux symptoms, particularly laryngopharyngeal reflux (LPR), can be considered. The symptoms may be caused by a combination of these factors.
The first manifestation is often felt to be potentially fatal (19). On the other hand, the VCD may also manifest itself submaximally, as "not being able to breath out properly." The smooth transition from active inspiration to passive expiration is no longer successful. The symptoms cannot be stimulated at will. Stridor is typical, as are dysphonia and aphonia during the attack of dyspnea. Sudden attacks of dyspnea without prior irritation of the mucus membrane are rare.
As the symptoms are often felt to be threatening, they may be accompanied by massive anxiety or panic, which may dominate the presentation.
VCD attacks strike the physician as emergencies. The patient is agitated and capable of little cooperation. His breathing is strident; he has to fight for breath.
Auscultation is not very reliable, as the laryngeal sounds may be transmitted over the thorax and may be misinterpreted as rhonchi. These respiratory emergencies are more marked by hyperventilation than by a reduction in oxygen saturation (18).
Emergency treatment has often been intubation and respiration (19). Even tracheotomy has occasionally been performed for recurrent VCD attacks (2).
VCD and asthma
It is difficult to differentiate VCD from bronchial asthma. Dyspnea may have a multitude of pathophysiological causes. Many patients are incapable of stating whether their difficulties are in inspiration or in expiration. This may be because their perception of breathing is limited or it may show that they have never had to answer this question before.
The clinical picture is complicated if the patients simultaneously suffer from bronchial asthma and VCD. The trigger mechanisms for the two diseases are similar. Diagnostic differentiation is made more difficult by the fact that the episodic nature and severity of VCD dyspnea, as well as the variability of the findings, fulfill the formal criteria for asthma, as given, for example, by the American Thoracic Society (20, 21) (table).
Table. Typical clinical manifestations and possible triggering factors for asthma and VCD.
| Asthma | VCD | |
| Development | Often rapidly(minutes) | Mostly hyperacute (seconds) |
| Duration | Individually variable | Seconds to a few minutes |
| Dyspnea during | Expiration | Inspiration (rarely expiration) |
| Localization | Thorax/lower respiratory tract | Neck/upper respiratory tract |
| Drugs | Highly effective | Ineffective |
| Triggers | Irritants, allergens, stress, exertion | Irritants, stress, exertion, (allergens?) |
| Cough | Trigger, accompanying | Trigger, accompanying |
Both diseases can be triggered by gastroesophageal reflux or a dry cough. It has been shown that reflux symptoms are absent in 20% to 60% of patients with gastric asthma (14).
In patients with asthma and VCD, a VCD attack can convert into an asthma attack, or conversely. Clinical classification of the symptoms is then difficult, even if both diagnoses have been made (22).
The threatening character of the dyspnea often discourages the doctor from critical enquiry or from decreasing drug dosages (15).
If asthma therapy for 6 months in accordance with the guidelines is unsatisfactory or inaffective, the asthma diagnosis should be critically re-evaluated by an established expert. If the presentation is not typical of asthma, the prior diagnosis must be questioned and the main symptom of dyspnea must be re-examined (box 1).
Box 1. Important questions in asthma which is apparently refractory to drug treatment.
Is the clinical course typical of asthma?
Is the patient’s compliance adequate, particularly in taking corticosteroids?
Are there persistent and/or destabilizing trigger factors, such as allergens?
Is there evidence for steroid resistance–which is extremely rare?
Is the asthma diagnosis certain? Is asthma the sole cause of the dyspnea?
Has the doctor made this diagnosis because he is desperate?
Diagnosis
Medical history
Even detailed differential diagnosis may fail to establish a reliable diagnosis (box 2). The medical history is an essential component and must include precise questions about the main symptom, dyspnea. As a subjective feeling, this cannot be exactly defined or measured. The correlations between dyspnea intensity and measured lung function are often weak. Graduation of the severity of the dyspnea rarely improves the clinical evaluation (18).
Box 2. Diagnostic procedure when VCD is suspected.
Specific, differentiated medical history
Pulmonary function:
| Are the findings normal during the symptom-free interval and is | MIF50 < MEF50? |
| During acute dyspnea, | is flow limited during inspiration or during expiration? |
Provocation laryngoscopy (endospirometry)
Ear, nose, and throat investigation: evidence for PND?
Reflux diagnosis: evidence for GER or LPR?
The quality of the dyspnea is of importance. Did the patient feel almost insuperable resistance? Was his chest constricted? Was he gasping for air? Where did he think the restriction was sited? Did the dyspnea develop at rest, with stress, or did it depend on body position? Did it occur when breathing in or out? Did irritants or coughing play a role? If the patient also suffers from bronchial asthma, it must be clarified whether the quality of the dyspnea has changed with time, so whether there are two different forms of dyspnea. The patient must also be asked about any dependence on the situation or the time of day. These aspects of dyspnea must be regarded in a differentiated manner, just as is usual when taking a pain history (box 3).
Box 3. Important questions for the VCD medical history.
Hyperacute dyspnea from one moment to the next?
Dyspnea during inspiration?
Localization of the feeling of constriction–upper respiratory tract or neck?
Short, self-limiting symptoms (under 2 minutes)?
Quality of dyspnea?
Is asthma medication effective, including systemic steroids?
Is the dyspnea triggered by irritatants?
Is the dyspnea triggered by coughing attacks?
Has the pulmonary function repeatedly been found to be normal?
Most patients are capable of describing their problems in such a way that the diagnosis of VCD suggests itself. When describing the dyspnea, the patient can provide useful evidence if he points towards the neck. The authors’ experience is that the patients can suggest the diagnosis themselves if they are provided with specific information. There have been many publications for laymen on this issue, particularly on TV, which have allowed VCD patients to recognize themselves so closely that this has helped to establish the diagnosis.
Pulmonary function
Although measurements of lung function are essential, they are rarely in accordance with the other findings or with the patient’s well-being, as the measured values do not agree with the description of the intensity of dyspnea. Typically, spirometry and body plethysmography find few if any abnormalities during the asymptomatic interval.
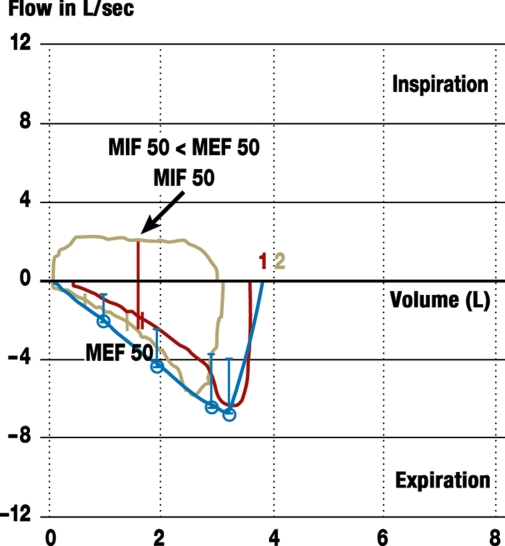
It is almost never possible to take a measurement at the time of the acute symptoms. It is therefore necessary to search for evidence of VCD in the pulmonary function tests. Functional abnormalities in the movements of the vocal cords may produce unusual changes in lung function. It is therefore necessary to analyze the flow-volume curve, both during inspiration and during expiration (figure 2).
Figure 2.
Flow-volume curve of a 24-year-old female patient with intractable attacks of dyspnea of unclear etiology; inspiration curve flattened; in addition, the maximal inspiration flow at 50% of the forced vital capacity (MIF 50) is less than the expiration flow (MEF 50)
The most helpful lung function tests are nonspecific inhalation provocation challenge tests, e.g., with metacholine. Provocation tests can provoke both bronchial and laryngeal hyperreactivity. It must therefore be clarified what has caused the reduction in the forced expiratory volume in the first second (FEV1). The time courses of the curves are just as important as the numerical values. The reduction in FEV1 from VCD is mostly linked to restricted inspiration, rather than expiration. Without evaluation of the time courses, a numerically positive provocation test may not be taken as proof of bronchial asthma.
Expiratory VCD is rare and difficult to demonstrate, as no endoscopic differentiation is possible between physiological adduction of the vocal cords during expiration–particularly in asthmatics–and expiratory malfunction of the vocal cords (16).
Endoscopy
The laryngoscopic imaging of a VCD attack is regarded as the diagnostic gold standard. The indications for laryngoscopy are unusual clinical courses which are either untypical of asthma or which cannot be fully explained by asthma. The investigation is performed transnasally, after anesthesia of the nasal mucus membrane, but without premedication. This excludes any pharmacological effect on larynx function.
Specific individually selected irritants are employed during endoscopy, including odor irritants, tactile stimulation, and ergometer stress (18). However, iatrogenic laryngospasm should certainly not be misinterpreted as VCD. It is rather the case that the triggered dyspnea must be compared with the known characteristics of the patient’s dyspnea.
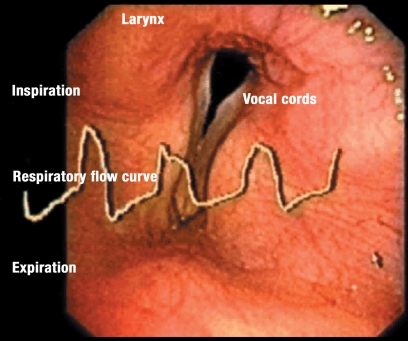
Endospirometry has been developed as a special procedure to confirm the diagnosis (23). In this approach, the endoscopic image and the spirometry curves are synchronously projected on a monitor (figure 3).
Figure 3.
Endospirometry of the larynx with synchronous presentation of the endoscopic image and pulmonary function curve, giving a reliable interpretation of restriction to respiratory flow and the movements of the vocal cord and their connection with dyspnea
VCD is never excluded if the laryngoscopy is normal, as VCD attacks cannot be stimulated on order, in spite of intensive provocation.
Differential diagnoses
Differential diagnoses to be considered include congenital, allergic, neural, neuromuscular, malignant, posttraumatic and acute inflammatory changes in the larynx and trachea (15).
It has been known since 1988 that VCD and the obstructive sleep-apnea syndrome may be associated (24).
A clear distinction should be made between VCD and voluntary strident and clearly ostentatious respiration.
Treatment
Asthma therapy according to guidelines–including high dose corticosteroids–has no effect on VCD symptoms (18). Currently available VCD therapy concepts have the status of experts’ recommendations. Respiration is immediately facilitated with acute heliox inhalation (20% oxygen + 80% helium) (25). Intravenous midazolam has an immediate effect in a few patients (19). VCD used to be treated in the USA by injecting botulinum toxin into the larynx musculature, even though this causes dysphonia or aphonia, and sometimes dysphagia. As there are now better alternatives, this approach is obsolete (26).
If the patient has previously been treated with oral steroids, it is important that the dose is consistently and carefully reduced after the VCD diagnosis. If there are any remaining asthma symptoms, these must be treated according to the guidelines. Pulmonary function is monitored over time and this can indicate the necessary dose of anti-obstructive drugs (20).
The most effective therapeutic approach is to provide the patient with information, if possible using a video to support the explanation. Once the patient has understood the symptoms, this resolves the apparent contradiction between the dyspnea–perceived as potentially fatal–and the comparatively harmless disorder. This helps to alleviate the patient’s fears, which usually considerably improves his overall condition, making it possible to start breathing therapy. The aim of the breathing strategies is to counteract the functionally paradoxical closure of the respiratory tract, with specific breathing techniques to maintain patency. These include emphasis on the diaphragm and special techniques to relax the throat ("throat relaxed breathing").
Complementary relaxation measures can be helpful and may even include psychotherapy. It is usually unnecessary to administer psychotropic drugs (18).
If there is irritation from a post nasal drip (PND), treatment of the infection can improve symptoms. Treatment with high doses of proton pump inhibitors for 10 to 12 weeks can alleviate the symptoms if there are signs of LPR (14).
Conclusion
VCD is an underestimated disease, which occasionally has a tragic clinical course. The specific medical history mostly rapidly leads to an effective diagnosis.
Although it may be relatively simple to make a preliminary diagnosis, it is sometimes difficult to prove this. Particularly for patients who have suffered for years from VCD, with simultaneous bronchial asthma, even experts may have problems in reaching conclusions. The symptoms can hardly ever be elicited voluntarily. As the attacks are so short, it is very difficult to study them diagnostically. Typical findings on pulmonary function are difficult to recognize or interpret. The diagnosis must sometimes be made from the evaluation of the overall time course, bearing in mind the patient’s history.
The dyspnea history is of central importance, as only the patient himself can describe all aspects of his dyspnea. Once the patient has some knowledge of the disease, he will lose his fear of suffocation and master breathing techniques to alleviate the symptoms. Concomitant diseases, such as post nasal drip (PND) or laryngopharyngeal reflux (LPR) must be treated by specialists.
The dosage of asthma drugs should be gradually reduced until asthma symptoms appear. If this does not happen, the drugs should be totally discontinued.
As this condition causes severe suffering, the patients are prepared to make every effort to clarify their situation. The diagnostic effort is often considerable, but is justified by the severe consequences for health and expenditure. In any case, patients with VCD and their symptoms must be taken seriously and not be prematurely diagnosed as suffering from psychosomatic problems.
As the pathophysiology of VCD is still incompletely understood, collaborative research between different disciplines is necessary to increase our knowledge of this condition.
Acknowledgments
Translated from the original German by Rodney A. Yeates, M.A., Ph.D.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Newman KB, Mason UG, Schmaling KB. Prospective study of vocal cord dysfunction. Eur Respir J. 1994 [Google Scholar]
- 2.Newman KB, Dubester SN. Vocal Cord Dysfunction: masquerader of asthma. Seminars in Respiratory and Crit Care Med. 1994;15:161–167. [Google Scholar]
- 3.Newman KB, Mason UG, Schmaling KB. Clinical features of Vocal Cord Dysfunction. Am J Respir Crit Care Med. 1995;152:1382–1386. doi: 10.1164/ajrccm.152.4.7551399. [DOI] [PubMed] [Google Scholar]
- 4.Dunglison R. The practice of Medicine. Philadelphia: Lea and Blanchard; 1842. pp. 257–258. [Google Scholar]
- 5.Warwick M Turner. On observing patterns of airflow obstruction in chronic asthma. Br J Dis Chest. 1977;71:73–86. doi: 10.1016/0007-0971(77)90086-9. [DOI] [PubMed] [Google Scholar]
- 6.Ayres JG, Miles JF, Barnes PJ. Brittle asthma. Thorax. 1998;53:315–321. doi: 10.1136/thx.53.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain S, et al. Incidence of vocal cord dysfunction in patients presenting to emergency room with acute asthma exacerbation. Chest. 1997;11 [Google Scholar]
- 8.Kenn K, Schmitz M. Prevalence of vocal cord dysfunction in patients with dyspnea. First prospective clinical study. Am J Respir Crit Care Med. 1997;155 [Google Scholar]
- 9.Morris MJ, Gerbach VX, Deal LE, Boyd SY, Morgan JA, Johnson JE. Evaluation of exertional dyspnea in the active duty patient: the diagnostic approach and the utility of clinical testing. Mil Med. 2002;167:281–288. [PubMed] [Google Scholar]
- 10.Rundell KW, Spiering BA. Inspiratory stridor in elite athletes. Chest. 2003;123:468–474. doi: 10.1378/chest.123.2.468. [DOI] [PubMed] [Google Scholar]
- 11.Gavin LA, Wamboldt M, Brugman S, Roesler TA, Wamboldt F. Psychological and family characteristics of adolescents with vocal cord dysfunction. J of Asthma. 1998;35:409–417. doi: 10.3109/02770909809048949. [DOI] [PubMed] [Google Scholar]
- 12.Brugman S. What’s this thing called vocal cord dysfunction. Pulmonary and Critical Care Update. in press. [Google Scholar]
- 13.Selner JC, Staudenmayer H, Koepke JW, Harvey R, Christopher K. Vocal cord dysfunction: The importance of psychological factors and provocation challenge testing. J Allergy Clin Immunol. 1987;79:726–733. doi: 10.1016/0091-6749(87)90203-x. [DOI] [PubMed] [Google Scholar]
- 14.Harding SM, Guzzo MR, Richter JE. Respiratory symptom correlation with esophageal acid events. Chest. 1999;115:654–659. doi: 10.1378/chest.115.3.654. [DOI] [PubMed] [Google Scholar]
- 15.Kenn K, Hess M. Vocal Cord Dysfunction - eine rein pneumologische Erkrankung? HNO. 2004;52:103–109. doi: 10.1007/s00106-003-0974-z. [DOI] [PubMed] [Google Scholar]
- 16.Bucca C, Rolla G, Brussino L, De Rose V, Bugiani M. Are asthma-like symptoms due to bronchial or extrathoracic airway dysfunction? Lancet. 1995;346:791–796. doi: 10.1016/s0140-6736(95)91617-2. [DOI] [PubMed] [Google Scholar]
- 17.Sittel C, Wassermann K, Mathen F, Eckel HE. Uni- und bilaterale Lähmung des Nervus laryngeus inferior (recurrens) Pneumologie. 2001;55:568–578. doi: 10.1055/s-2001-19004. [DOI] [PubMed] [Google Scholar]
- 18.Kenn K. Vocal Cord Dysfunction, (VCD), was wissen wir heute? Pneumologie. 2007;61:431–439. doi: 10.1055/s-2007-959199. [DOI] [PubMed] [Google Scholar]
- 19.Christopher KL, Wood RP, Eckert RC, Blager FB, Raney RA, Souhrada JF. Vocal cord dysfunction presenting as asthma. N Engl J Med. 1983;308:1566–1570. doi: 10.1056/NEJM198306303082605. [DOI] [PubMed] [Google Scholar]
- 20.Global Initiative for Asthma: Global strategy for asthma management and prevention. NIH Publication No 02-3659. Bethesda: National Institute of Health/National Heart, Lung and Blood Institute; 2005. [Google Scholar]
- 21.Thomas PS, Geddes DM, Barnes PJ. Pseudo-steroid resistant asthma. Thorax. 1999;54:352–356. doi: 10.1136/thx.54.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balkissoon R. Occupational upper airway disease. Clin Chest Med. 2002;23:717–725. doi: 10.1016/s0272-5231(02)00032-1. [DOI] [PubMed] [Google Scholar]
- 23.Kenn K, Freitag L. Endospirometry - development of a device to objectify vocal cord dysfunction and proposal for a classification system. Eur Respir J. 2006;28 [Google Scholar]
- 24.Rubinstein I, Slutsky A, Zamel N, Hoffstein V. Paradoxical glottic narrowing in patients with severe obstructive sleep apnea. J Clin Invest. 1988;81:1051–1055. doi: 10.1172/JCI113416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reisner C, Borish L. Heliox therapy for acute vocal cord dysfunction. Chest. 1995;108 doi: 10.1378/chest.108.5.1477. [DOI] [PubMed] [Google Scholar]
- 26.Garibaldi E, La Blance G, Hibbett A, Wall L. Exercise-induced paradoxical vocal cord dysfunction: diagnosis with videostroboscopic endoscopy and treatment with clostridium toxin. J Allergy Clin Immunol. 1993;91200 [Google Scholar]